Abstract
Glandular odontogenic cyst (GOC) is an uncommon developmental odontogenic cyst of jaws with a relative frequency between 0.012 and 1.3%. GOC is very rare and only 111 cases have been documented in the English literature so far. Generally, this cyst is encountered in the anterior areas of the mandible and is more common with a wide age range, the mean age being 49.5 years and has a tendency to recur. GOC is often misdiagnosed because of its overlapping histopathological features with that of other odontogenic cysts such as lateral periodontal cyst (LPC) or botryoid cyst and central low-grade Mucoepidermoid carcinoma. Histopathological diagnosis and differential diagnosis of GOC is challenging for pathologist. Here, we present a case of GOC in a 40 year old male patient in left mandibular region that crossed the midline.
Keywords: Cilia, glandular odontogenic cyst, mucous cell, sialo-odontogenic cyst
INTRODUCTION
Glandular odontogenic cyst (GOC) was first documented as ‘sialo-odontogenic cyst’ by Padayachee and Van Wyk in 1987; who published two cases that resembled both the botryoid odontogenic cyst and the central mucoepidermoid tumor of jaws. After careful analysis, they concluded both lesions as separate entities.[1] Gardner et al., in 1988 characterized histopathological features and biological behavior of GOC and established it as a distinct entity and proposed term ‘GOC’.[2] High et al., (1996) proposed the term ‘polymorphous odontogenic cyst’ for this cyst because of its aggressive growth pattern.[3]
The GOC represents one of three possibilities. (1) A true cyst of glandular origin from either entrapped salivary gland primodia or undifferentiated primitive epithelial rests that differentiates into glandular epithelium. (2) An odontogenic primodial origin cyst in which the epithelial lining undergoes prosoplasia (metaplasia from a less specific differentiation to a more specific differentiation) into glandular epithelium. (3) Low-grade mucoepidermoid carcinoma that forms an initial single cystic space instead of the usual multicystic spaces.[4]
The most common mode of presentation is a slow growing intraosseous lesion in the anterior mandible (nearly 87.2%) and most of these are seen crossing the midline.[5] This cyst occurs in wide age range but is common in middle-aged adults with a mean age of 49.5 years.[5] Small cysts may be asymptomatic; however, large cysts often produce clinical expansion, which sometimes can be associated with pain or paresthesia. Radiographically, the lesion may appear as a unilocular or, more commonly, multilocular radiolucency. The margins of the radiolucency are usually well defined with a sclerotic rim.[6]
Characteristic histopathologic features are variable thickness of nonkeratinized stratified epithelium, with superficial layer of epithelium consisting of columnar or cuboidal cells, occasionally seen with cilia and numerous goblet cells. The epithelium has glandular or pseudoglandular structure, with intra-epithelial crypt or microcyst formation.[7]
GOC is very rare, so here we present a unique case of a GOC and clinico-histopathological features of this rare cyst.
CASE REPORT
A 40 year old male patient reported with chief complaint of painful swelling in lower left front tooth region since 5 months. Extraorally, the swelling was not obvious and did not produce any facial asymmetry.
Intraoral examination revealed a single buccal swelling in the left mandibular region extending from 34 to 36, approximately 2 × 1 cm2 in size [Figure 1]. The swelling extended supero-inferiorly from attached gingiva to the entire depth of the buccal vestibule. Overlying mucosa was smooth and erythematous. On palpation, the swelling was firm, non-tender, non-mobile and non pulsatile. Submandibular lymph nodes on left side were palpable and tender. A provisional diagnosis of ameloblastoma and differential diagnosis of odontogenic keratocyst was given. Radiographic examination revealed a multilocular radiolucent area with sclerotic border extending from 36 to 43 region [Figure 2].
Figure 1.

Intraoral photograph showing buccal left mandibular swelling
Figure 2.
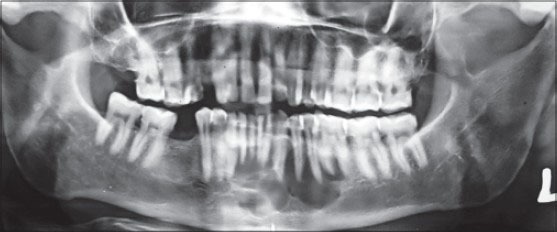
Multilocular radiolucency extending from 36 to 43
Numerous hard and soft tissue specimens were received. Hard tissue consisted of 34, 35 and 36 with soft tissue bits attached to apical region of these hard tissue specimens. Soft tissue showed cystic cavity surrounded by fibrous capsule and was soft in consistency and creamish white in color [Figure 3].
Figure 3.

Gross specimen: Multiple soft tissue bits with extracted teeth
The cyst was lined by a nonkeratinized stratified squamous epithelium of variable thickness, with flat epithelial connective tissue interface [Figure 4]. The superficial layer of the epithelial lining consisted of cuboidal and in some areas columnar cells with cilia or filiform-like extensions of the cytoplasm and the epithelium showed spherule arrangement at some places [Figure 5]. Small microcysts lined by single layer of cuboidal or columnar cell were present within the epithelium [Figure 6] which contained periodic acid Schiff [PAS] positive secretory product. Numerous PAS-positive goblet cells were present, mainly in the superficial part of the epithelium [Figure 7].
Figure 4.
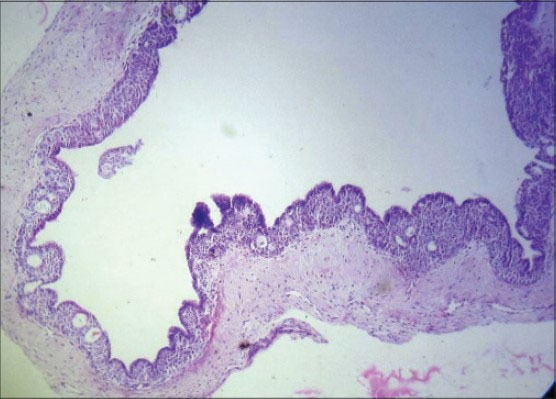
Photomicrograph showing cystic lining exhibiting variable thickness of epithelium, some areas of papillary projection and numerous microcysts formation (H&E stain, ×40)
Figure 5.
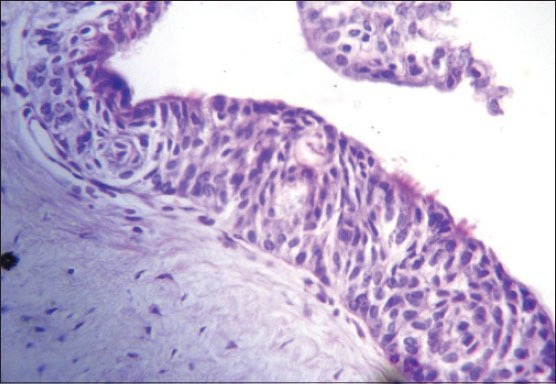
Photomicrograph revealing cystic epithelium exhibiting spherule formation with few superficial ciliated cuboidal cells (H&E stain, ×200)
Figure 6.
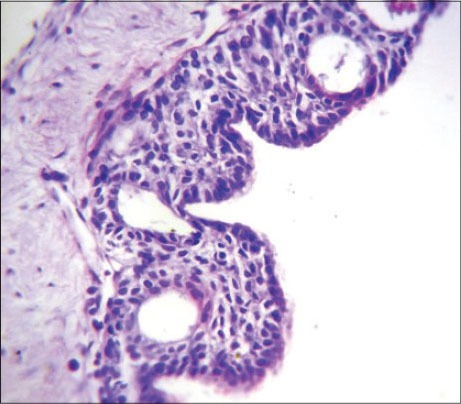
Photomicrograph showing numerous microcysts lined by eosinophilic cuboidal cells (H&E stain, ×400)
Figure 7.
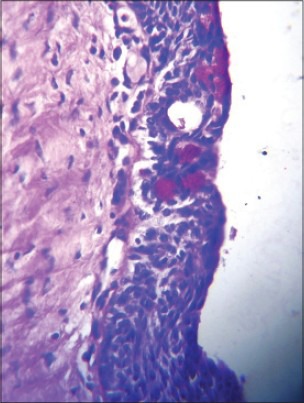
Photomicrograph showing PAS-positive mucous cells (PAS stain, ×400)
DISCUSSION
GOC is an uncommon jaw cyst of odontogenic origin. To the best of our knowledge, only 111 cases of GOC have been reported in the literature and Magnusson et al., observed that only 0.012% of the cysts seen on the oral cavity have fulfilled the criteria of GOC microscopically.[8,9] Literature review showed that GOC may mimic a wide clinicopathologic spectrum ranging from LPC to a destructive malignant neoplasm such as central mucoepidermoid carcinoma CMEC.
There is a slight male predilection and lesions occur mostly in middle-aged patients. The main clinical finding in this cyst is a painless local swelling; the clinical picture, however, is non-specific. The lesion may cause pain due to compression of a neurovascular bundle or secondary infection; inflammation, however, is uncommon. The anterior mandible is the most common site for occurrence of this cyst. In this case, lesion was found in the anterior mandibular area and was painful.[5]
Lack of consistency in the clinical manifestations and the intraosseous development of these lesions demonstrate the importance of radiographs for this lesion. Radiographic findings include a rounded or oval lesion, unilocular or multilocular lesion, usually with well-defined borders. The differential diagnosis includes botryoid cysts, keratocysts, residual cysts, central mucoepidermoid carcinoma (CMEC) and ameloblastoma.
The histopathological characteristic features of GOC given by Gardner et al. and Kaplan et al. proposed a list of microscopic criteria for GOC such as non-keratinized stratified squamous epithelium, epithelial whorls or spheres within the lining, eosinophilic cuboidal or columnar cells which are occasionally ciliated and presence of mucous cells with microcystic areas. The sub-epithelial connective tissue is usually free of inflammation. The present case had all the characteristic features of GOC.[2,10]
Histopathologically, GOC should be differentiated from lateral periodontal cyst (LPC) and CMEC as they exhibit considerable overlap of histological features. The lining of LPC exhibits focal thickenings and glycogen-rich epithelial cells, similar to those observed in GOC. However, the identification of ciliated epithelium and duct-like spaces with mucous cells specifically differentiate GOC from LPC and botryoid odontogenic cyst (BOC) and favors the diagnosis of GOC.[7] The differentiation of low-grade CMEC from GOC is more important and difficult. However, CMECs do not show superficial cuboidal cells, epithelial whorls, ciliated cells and intraepithelial microcyst or duct-like structures.[11] The central MEC and the GOC are distinct entities with different cytokeratin (CK) profiles and the differential expression of CKs 18 (CMEC) and 19 (GOC) could be useful adjunctive tools in differentiating these two entities.[7,12] Of interest is the discovery within the past few years that most MECs exhibit a t (11:19)(q21:p13) translocation resulting in the MECT1:MAML2 fusion protein. Recently, this translocation has also been reported in CMEC.[13]
The aggressive biologic behavior of GOC and its propensity for recurrence might be associated with cell kinetics in the lining epithelium. Tosios et al. (2000) investigated the expression of bcl-2 protein, Ki-67 antigen and p53 protein in GOCs. The authors concluded that the increased expression of the anti-apoptotic bcl-2 may be associated with deregulation of cell death in the lining epithelium of the GOCs, whereas Ki-67 and p53 status did not seem to play a significant part in cell proliferation.[14]
Treatment by enucleation or curettage alone is associated with a high recurrence rate. Small unilocular lesions can be treated by enucleation. Surgical treatment of large lesions should include enucleation with peripheral ostectomy for unilocular cases and marginal resection or partial jaw resection in multilocular cases. Marsupialization followed by second phase surgery is an option for lesions approaching vital structures. Follow up should be continued for at least 3 years (up to 7 years in cases with features associated with increased risk of recurrence rate due to its intrinsic biological behavior, multilocularity of the cyst and incomplete removal of the lining following conservative treatment).[15]
CONCLUSION
Purpose of this case presentation is to increase existing knowledge of this rare entity as histopathological diagnosis and differential diagnosis of GOC is challenging for a pathologist. Adequate treatment of GOC is required because of its aggressive biologic behavior and propensity for recurrence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: Sialo-odontogenic cyst? J Oral Pathol. 1987;16:499–504. doi: 10.1111/j.1600-0714.1987.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 2.Gardner DG, Kessler HP, Morency R, Schaner DL. The glandular odontogenic cyst: An apparent entity. J Oral Pathol. 1988;17:359–66. doi: 10.1111/j.1600-0714.1988.tb01298.x. [DOI] [PubMed] [Google Scholar]
- 3.High AS, Main DM, Khoo SP, Pedlar J, Hume WJ. The polymorphous odontogenic cyst. J Oral Pathol Med. 1996;25:25–31. doi: 10.1111/j.1600-0714.1996.tb01219.x. [DOI] [PubMed] [Google Scholar]
- 4.Mark RE, Stern D. 2nd ed. New Delhi: Quintessence Publishing co, Inc; 2012. Oral and maxillofacial pathology. A rationale for diagnosis and treatment. [Google Scholar]
- 5.Shafer WG, Hine, Levy . 5th ed. India: Elsevier; 2005. Shafer's textbook of Oral Pathology. [Google Scholar]
- 6.Manor R, Anavi Y, Kaplan I, Caldren Radiological features of glandular odontogenic cyst. Dentomaxillofac Radiol. 2003;32:73–9. doi: 10.1259/dmfr/22912856. [DOI] [PubMed] [Google Scholar]
- 7.Shear M. 3rd ed. Mumbai: Varghese Publishing House; 1992. Cysts of the Oral Region. [Google Scholar]
- 8.Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: A challenge in diagnosis and treatment. Oral Dis. 2008;14:575–81. doi: 10.1111/j.1601-0825.2007.01428.x. [DOI] [PubMed] [Google Scholar]
- 9.Magnusson B, Goransson L, Odesjo B, Grondahl K, Hirsch JM. Glandular odontogenic cyst: Report of seven cases. Dentomaxillofac Radiol. 1997;26:26–31. doi: 10.1038/sj.dmfr.4600205. [DOI] [PubMed] [Google Scholar]
- 10.Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA. Glandular odontogenic cyst: Analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head and Neck Pathol. 2011;5:364–75. doi: 10.1007/s12105-011-0298-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prabhu S, Rekha K. Kumar. Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma. J Oral Maxillofac Pathol. 2010;14:12–5. doi: 10.4103/0973-029X.64303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen J, Fan M, Chen X, Wang S, Wang L, Li Y. Glandular odontogenic cyst in China: Report of 12 cases and immunohistochemical study. J Oral Pathol Med. 2006;35:175–82. doi: 10.1111/j.1600-0714.2006.00389.x. [DOI] [PubMed] [Google Scholar]
- 13.Seethala RR, Dacic S, Cieply K, Kelly LM, Nikiforova MN. A reappraisal of the MECT1/MAML2 translocation in salivary mucoepidermoid carcinomas. Am J Surg Pathol. 2011;34:1106–21. doi: 10.1097/PAS.0b013e3181de3021. [DOI] [PubMed] [Google Scholar]
- 14.Tosios KI, Kakarantza Angelopaulou E, Kapranos N. Immunohistochemical study of bcl-2 protein, ki67 antigen and p53 protein in epithelium of glandular odontogenic cysts and dentigenous cysts. J Oral Pathol Med. 2000;29:139–44. doi: 10.1034/j.1600-0714.2000.290306.x. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan I, Gal G, Anavi Y, Manor R, Caldron Glandular odontogenic cyst: Treatment and recurrence. J Oral Maxillofac Surg. 2005;63:435–41. doi: 10.1016/j.joms.2004.08.007. [DOI] [PubMed] [Google Scholar]


