Abstract
Background:
Palestinian refugees have been a displaced group of people since 1948, many of whom are living in refugee camps in the Middle East. They are entitled to free health care from the United Nations Relief and Work Agency (UNRWA). They show a higher prevalence of diabetes than the population in their host countries in the Middle East. This study examined the realities of care for diabetic patients in UNRWA health clinics in Damascus, Syria. The aim was three-fold: To investigate the level of diabetes care, to probe patients’ level of general understanding of their disease and its management, and to search for areas of potential improvement.
Methods:
Data on patient education and care was gathered over a 1 month period from August 4, 2008 to September 4, 2008 using questionnaires and direct observation of the workflow at the clinics. Clinic-led care was observed by the study team using checklists during patient visits. All of the clinic staff and sampled patients were interviewed. The main areas of care assessed were: Patient follow-up; examination of eyes and feet; availability of medications; and patient education. A total of 154 people with diabetes were sampled from three refugee camps situated around Damascus.
Results:
A total of 154 patients, three doctors and seven nurses composed the sample of the study. Foot examinations were almost always neglected by health staff and eye examinations were not offered by the UNRWA clinics. Interviews with patients showed that: 67% (95% confidence intervals [CI]: 0.59-0.70) had to buy their medication at their own expense at least once due to medication shortage in the UNRWA clinics, 48% (95% CI: 0.40-0.55) displayed poor knowledge regarding the cause and exacerbating factors of diabetes, 65% (95% CI: 0.56-0.72) had not heard of insulin, and 43% (95% CI: 0.35-0.51) did not know for how long they needed to take their medications.
Keywords: Diabetes mellitus, health clinic, healthcare management, resource management, under-served populations
INTRODUCTION
Palestinians have largely been a displaced group of people since 1948 with numbers in countries of the Middle East, other than Palestine, exceeding 5 million.[1] In Syria alone, the number has been estimated to be over 510,000 people.[2] The number of Palestinian refugees has continued to rise as refugee status extends to their children. Palestinian refugee camps are generally poor, overcrowded and lack adequate basic infrastructure.[3,4] A branch of the United Nations was established in 1949 to provide free health care, education, and relief to displaced Palestinians and was named the United Nations Relief and Work Agency (UNRWA). Palestinian refugee camps are found in Syria, Lebanon, Jordan, and the Palestinian Territories. There are two types of camps: Official camps set up by the UNRWA and unofficial camps set up by the host country. The UNRWA offers its services equally to refugees from both types of camps.
Diabetes is a major cause of premature morbidity and among Palestinian refugees, as in many other Middle Eastern populations. For example, the prevalence of diabetes mellitus (DM) among Palestinian refugees is estimated to be 12-15% and has doubled in the last 10 years. Obesity, a risk factor for type 2 diabetes, is a problem more prevalent in UNRWA refugee camps compared with original populations of the host countries.[6]
In 2008, 533 diabetic patients were registered at UNRWA clinics in Syria alone.[14] Some patients (e.g., those with type 1 diabetes) require uninterrupted access to insulin for survival, and others (e.g., many with type 2 diabetes) require insulin for adequate blood glucose control. Of the 26,113 Palestinian refugees in Syria with diabetes, 23.5% were being treated with insulin.[13] All patients with diabetes require access to education on how to manage the condition; medication, particularly for blood glucose and blood pressure lowering, frequent monitoring of blood glucose and blood pressure, regular monitoring of feet, eyes and kidneys function for potential complications, and access to care in order to both prevent and treat complications when they occur.[14] Compliance and adherence to medication is crucial in diabetics and poses a challenge to caregivers around the world. Factors shown to influence patient compliance include ease of access to facilities, cost of medication(s), patient's cultural or family factors, and patients’ perception and knowledge about their illness.[15,16]
Health care provision and uptake in the Palestinian refugee camps has been investigated in Jordan, Lebanon, and the Palestinian territories,[3,4,5,6,7,8,9,10,11] but not in Syria. The published studies to date have included the assessment of diabetes risk factors and aspects of diabetes care. However, none of these studies directly sought the attitudes of refugees with diabetes, which are very important when considering issues of compliance. Our study aimed to fill these gaps by examining diabetes care for Palestinian refugees in Syria, and in particular to involve users of the services in this assessment.
The specific objectives of this study were:
To determine the level of care available to patients with diabetes in UNRWA camps
To investigate patients’ level of understanding about their condition
To identify areas for potential improvement in diabetes care.
METHODS
Study setting and ethical approval
This study included the staff of and a sample of patients in three UNRWA health clinics in the Palestinian refugee camps of Jaramana, Sbeineh and Qabr Essit in Damascus [Figure 1]. A population of 61,425 people was served by the three camps at the time of data collection in 2008.[17]
Figure 1.
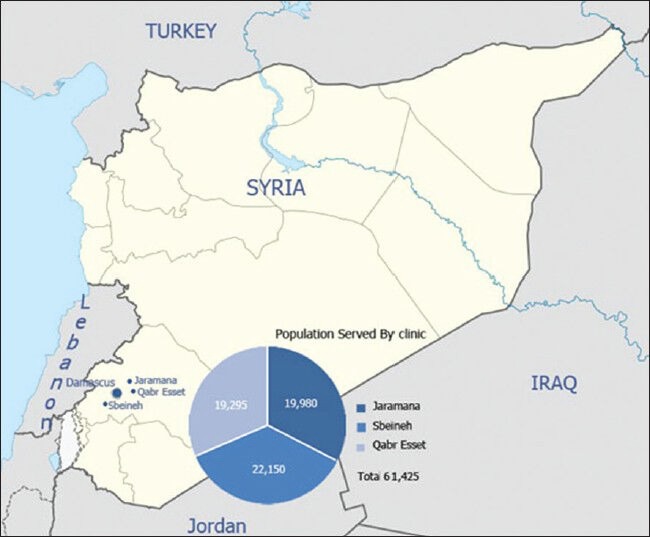
United Nations Relief and Work Agency clinics and population served by them
Ethical approval for the study was gained from UNRWA office (Damascus) and verbal consent was obtained from each clinic staff member and from all patients interviewed. Verbal consent included offering the interviewed subjects the choice of taking part in this study voluntarily and the option of stop at any point during the interview. The interviewed subjects were also made known about their rights at the point of taking consent, including confidentiality of the supplied information and personal data. All patients and members of staff were made aware that they were completely free to decline to participate in the study or to withdraw from it at any time.
Data collection
Data were collected from the three refugee camps in a 1 month period from August 4, 2008 to September 4, 2008. Questionnaires, patient observations, and patient health records were used for data collection. The data collection methods were based on instruments used for the evaluation of diabetes care in other low income settings. The instruments were adapted for use in this study through discussion among the study team, were pilot-tested and then finalized. Data collection was undertaken by a small team of medical students from Damascus University who were trained in the use of the data collection tools.
A total of 154 diabetic patients were identified from appointment lists of the diabetes clinics and were all invited to participate. Of these, 40 were from Jaramana, 55 from Qabr Essit and 59 from Sbeineh. Every Palestinian refugee with DM (type 1 or type 2) visiting the clinic was eligible for inclusion, regardless of comorbidities, age or gender. All of those approached agreed to be interviewed. Each patient was accompanied by one of the investigators throughout the clinic visit, starting with the nurse encounter, to the doctor's, and finally to the pharmacist's. In addition, a one-on-one interview with each patient was done to explore their knowledge and understanding of their disease and its management, patient risk factors, and medications taken by the patient. The health workers, including three doctors and seven nurses from the three clinics, were interviewed using a semi-structured interview schedule designed to investigate the challenges they perceived in providing diabetes care.
Throughout the month period, direct observation of the clinical practice of the nurses, doctors and pharmacists was carried out using checklists; including length of encounter, information and advice shared, examinations and tests ordered, and other services offered. Clinic inspections were also conducted using checklists, which looked specifically at resources, equipment, facilities, staff, and available medications.
RESULTS
Participants’ characteristics
A total of 154 patients composed our patient sample [Table 1]. Ten patients (6.5%) had type 1 diabetes without hypertension, 46 (29.8%) had type 2 diabetes without hypertension, and 98 (63.6%) had both diabetes and hypertension. About 71% were women and 29% men, with ages ranging from 13 to 79 years.
Table 1.
Participants characteristics
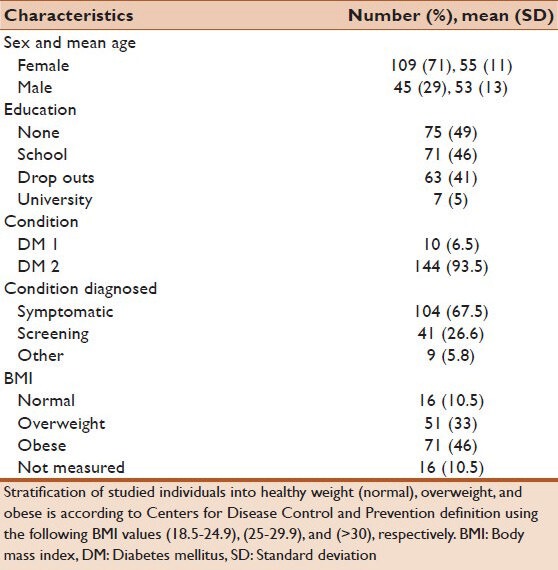
Of the 138 patients for whom height and weight was available, and thus body mass index was calculable, 88% were classified as overweight or obese. Diabetes control was assessed by fasting plasma glucose, with the target for control being <7 mmol/L (126 mg/dl). 74.2% of patients had a fasting plasma glucose level exceeding this normal value, and 62.5% exceeded 9 mmol/L.
Diabetes care
Outpatient follow-up
The main role of the doctor was to sign prescriptions. There was no history taking or examination during follow-up appointments. About 94% of patients spent 5 min or less with the doctor, with a median of 3 min (interquartile range [IQR] 2-4) for each patient. Only 13 patients (8%) had minimal form of examination. Nurses saw each patient for a median of 6 min (IQR 5-9) with 80% of the patients spending 10 min or less in the nurses’ room. Measurement of blood pressure and weight, alongside with urinalysis, were done routinely, but patients’ feet were examined in only 8% of the encounters.
Eye examination
Eye examinations were not performed in UNRWA clinics, and patients were asked to visit an ophthalmologist at their own expense. About 57% of patients reported that they had had their eyes checked at least once since their DM was diagnosed.
Medications
Clinic inspections highlighted shortages in drug stocks. However, pharmacy staff indicated that drugs for diabetes and hypertension were considered a priority by the clinic administration and were more available than other medications. Of the 93 patients responses regarding drug availability, 47.3% had encountered problems accessing prescribed medications and 67.7% (95% confidence intervals [CI]: 0.59-0.70) had to buy medications at their own expense at least once since their diagnosis.
Patient education
Knowledge about diabetes
When asked “which factors exacerbate your diabetes?,” more than half of the sampled population correctly recognized that diet had a role in their diabetes, associating an elevated blood glucose level with the intake of foods such as sugar, bread, rice, potatoes and sweet tea. About a third of the people surveyed associated salt, rheumatism, anger, tiredness, sadness and stress with their diabetes. Ninety-six patients (62%) included sadness or stress in the answer they gave, whilst 12% did not know what could exacerbate their diabetes.
Knowledge about treatment
When asked “Is it important to treat diabetes?” 148 patients (96%) believed that it was important to treat diabetes. However, 25 (16%) had either no information about the importance and purpose of treatment or revealed misunderstandings, for example, that the purpose of medication was “to be able to eat everything.” Whilst most had some idea of the importance of diabetes management, 112 (73%) could only mention one or two reasons support the importance of complying with medications.
When asked “have you got information about your medication?” 134 (87%) patients said that they felt they had been given enough information about their medication, yet 100 people (65%) had never been told that daily insulin injections may become necessary in the course of their disease. A total of 67 patients (44%) did not know how long they would have to take their medication for, or gave wrong information such as “until they get better.” Patients’ knowledge about their management is summarized in Figure 2.
Figure 2.
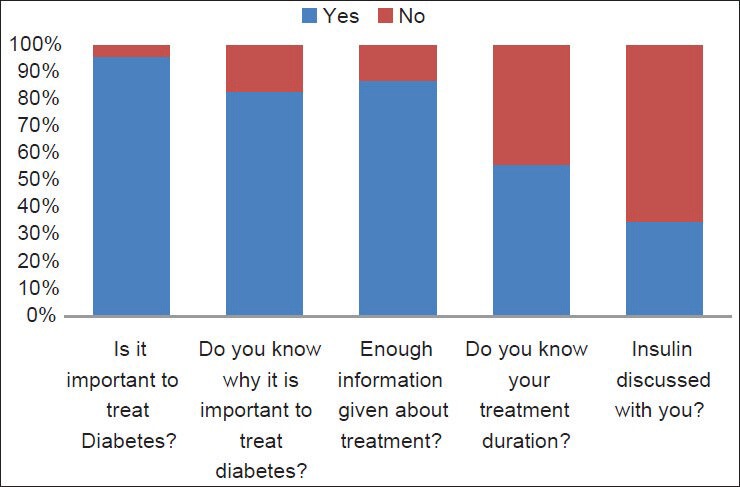
Patients knowledge about management
Staff interviews
When interviewing UNRWA clinic staff, many identified patient education as an area that was in need of improvement. They also felt that academic educational level was important in diabetes care, with lesser educated patients being the most difficult to manage.
DISCUSSION
The majority of patients studied were obese with poor glucose control (46% obese, 65% with blood glucose over 9 mmol/L). Hypertension was also very prevalent, which, in association with diabetes, increases the risk of complications and morbidity.[14]
As medical care at UNRWA clinics is free, the number of patient visits was high, thus leading to little time for each patient encounter.
Access to drugs appeared to be a problem for diabetics in UNRWA clinics. Drugs were sometimes prescribed but not available in clinic due to delays from the central depot. If drugs were unavailable, patients were advised to purchase them and/or starting the medication was delayed. This is particularly important in those taking more than one oral hypoglycaemic agent and those on insulin. Lack of access to medication can result in a life threatening hyperglycaemia causing dehydration, coma and eventually death in the short term, and a myriad number of complications on the long run.
Patients’ knowledge of their condition was limited, as demonstrated by the majority being unable to correctly identify risk factors for diabetes. Patients were generally unaware of the importance of good glucose control and disease management. The need to educate patients to develop a healthy diet, increase exercise, stop smoking and take medication was mostly neglected by time-constrained health staff.
Examination of patients was very limited and the vast majority of patients were unable to get their eyes checked at their own expense, as often recommended by the clinic staff. Although nurses have regular 3 monthly training sessions, they are not advised on how to increase patient awareness. Various advertising strategies, such as posters, highlight the importance of adequate glucose control, foot examination and regular self-examination, but research suggests that if this is not reinforced by health staff, there is little chance that it will be incorporated into the patient's own health regimen.[15]
LIMITATIONS
Due to the limited space available in the UNRWA clinics, we were unable to speak to each patient and staff member in a private room. Adequate confidentiality is therefore identified as a limitation as we recognize that this may impact on our results. Although effort was made to not reveal the exact checklist used to the medical staff until after completion of the study, we were unable to completely blind the medical practitioners to the study and therefore, we acknowledge that clinic staff behavior may have changed as a result of having researchers sit in the clinics.
RECOMMENDATIONS
A patient education program that involves all health care providers including nurses, doctors and pharmacists could benefit the patient population.[18,19] This may reduce the workload of the health clinics in the long term.
Regular eye checks could be made available in UNRWA clinics to increase access for financially disadvantaged patients and improve treatment options.[20]
More time should be spent examining patients and addressing any concerns they have. In particular, feet should be checked and the presence or absence of peripheral neuropathy documented.
With employed staff currently working at near saturation, community volunteers or health assistants could be trained to screen for these conditions in the clinic or in community settings. This would be a practical and achievable method of increasing the capacity of the UNRWA centers and would also encourage and empower patient groups and the Palestinian refugee community to play a greater role in their health care.
The majority of patients (62%) referred to sadness and stress as a cause of their diabetes. Taking into account patients’ cultural beliefs and attitudes and trying to encourage health care providers to address them may help increase motivation and compliance.[21] Depression can be the cause of poor compliance with medications and should be addressed with appropriate care such as patient education, counseling or support groups.[22,23]
Women were more likely to attend the clinic than men, with 71% of patients being female. This distribution has similarly been observed in other studies of UNRWA clinics.[12] Further efforts could be made to reach the male population such as running education programs through local religious, cultural, or social organizations.
These recommendations could improve patient care but may weigh heavily on the limited resources, time and money available to UNRWA. If nothing else is achieved, patient education should be addressed as a priority.
Footnotes
Source of Support: Funding was received from Newcastle University as part of the Newcastle University Vacation Scholarship scheme.
Conflict of Interest: None declared.
REFERENCES
- 1.Habib RR, Basma SH, Yeretzian JS. Harboring illnesses: On the association between disease and living conditions in a Palestinian refugee camp in Lebanon. Int J Environ Health Res. 2006;16:99–111. doi: 10.1080/09603120500538341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Habib R, Seyfert K, Hojeij S. Health and living conditions of Palestinian refugees residing in camps and gatherings in Lebanon: A cross-sectional survey. The Lancet-Palestinian Health Alliance 2012. 2012. [Last accessed 2014 Apr 20]. Available from: http://www.download.thelancet.com/flatcontentassets/pdfs/palestine2012/palestine2012–1.pdf .
- 3.Zabaneh JE, Watt GC, O’Donnell CA. Living and health conditions of Palestinian refugees in an unofficial camp in the Lebanon: A cross-sectional survey. J Epidemiol Community Health. 2008;62:91–7. doi: 10.1136/jech.2006.054338. [DOI] [PubMed] [Google Scholar]
- 4.Mousa HS, Yousef S, Riccardo F, Zeidan W, Sabatinelli G. Hyperglycaemia, hypertension and their risk factors among Palestine refugees served by UNRWA. East Mediterr Health J. 2010;16:609–14. [PubMed] [Google Scholar]
- 5.Modol X, Pace-Shanklin SWV, Abu-Zayed IS. Efficiency analysis of the health-care facilities of the UN relief and works agency for Palestine refugees in the near east in Jordan: A retrospective, descriptive study. The Lancet-Palestinian Health Alliance 2012. 2012. [Last accessed 2014 April 20]. Available from: http://www.download.thelancet.com/flatcontentassets/pdfs/palestine2012/palestine2012–8.pdf .
- 6.Khader A, Farajallah L, Shahin Y, Hababeh M, Abu-Zayed I, Kochi A, et al. Cohort monitoring of persons with diabetes mellitus in a primary healthcare clinic for Palestine refugees in Jordan. Trop Med Int Health. 2012;17:1569–76. doi: 10.1111/j.1365-3156.2012.03097.x. [DOI] [PubMed] [Google Scholar]
- 7.Yusef JI. Management of diabetes mellitus and hypertension at UNRWA primary health care facilities in Lebanon. East Mediterr Health J. 2000;6:378–90. [PubMed] [Google Scholar]
- 8.Husseini A, Abu-Rmeileh NM, Mikki N, Ramahi TM, Ghosh HA, Barghuthi N, et al. Cardiovascular diseases, diabetes mellitus, and cancer in the occupied Palestinian territory. Lancet. 2009;373:1041–9. doi: 10.1016/S0140-6736(09)60109-4. [DOI] [PubMed] [Google Scholar]
- 9.Mikki N, Shoaibi A, Khatib R, Abdullatif H. Assessment of services for diabetes mellitus in clinics in Ramallah, West Bank, occupied Palestinian territory: An evaluation study. The Lancet-Palestinian Health Alliance 2012. 2012. [Last accessed 2014 Apr 20]. Available from: http://www.download.thelancet.com/flatcontentassets/pdfs/palestine2012/palestine2012–28.pdf .
- 10.UNRWA. UNRWA, Homepage. 2013. [Last accessed on 2013 Oct 25]. Available from: http://www.unrwa.org/index.php .
- 11.UNRWA. UNRWA Statistics. 2013. [Last accessed on 2013 Oct 25]. Available from: http://www.unrwa.org/etemplate.php?id=253 .
- 12.UNRWA. The Annual Report of UNRWA-The Department of Health. 2012. [Last accessed on 2014 Apr 20]. Available from: http://www.unrwa.org/userfiles/file/publications/HealthReport2012.pdf .
- 13.Sabatinelli G, Pace-Shanklin S, Riccardo F, Shahin Y. Palestinian refugees outside the occupied Palestinian territory. Lancet. 2009;373:1063–5. doi: 10.1016/S0140-6736(09)60101-X. [DOI] [PubMed] [Google Scholar]
- 14.Srinivas G, Suresh E, Jagadeesan M, Amalraj E, Datta M. Treatment-seeking behavior and compliance of diabetic patients in a rural area of South India. Ann N Y Acad Sci. 2002;958:420–4. doi: 10.1111/j.1749-6632.2002.tb03017.x. [DOI] [PubMed] [Google Scholar]
- 15.Travis T. Patient perceptions of factors that affect adherence to dietary regimens for diabetes mellitus. Diabetes Educ. 1997;23:152–6. doi: 10.1177/014572179702300205. [DOI] [PubMed] [Google Scholar]
- 16.Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care. 2011;34:338–40. doi: 10.2337/dc10-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;1:CD001481. doi: 10.1002/14651858.CD001481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suppapitiporn S, Chindavijak B, Onsanit S. Effect of diabetes drug counseling by pharmacist, diabetic disease booklet and special medication containers on glycemic control of type 2 diabetes mellitus: A randomized controlled trial. J Med Assoc Thai. 2005;88(Suppl 4):S134–41. [PubMed] [Google Scholar]
- 19.Mumba M, Hall A, Lewallen S. Compliance with eye screening examinations among diabetic patients at a Tanzanian referral hospital. Ophthalmic Epidemiol. 2007;14:306–10. doi: 10.1080/09286580701272079. [DOI] [PubMed] [Google Scholar]
- 20.McCord EC, Brandenburg C. Beliefs and attitudes of persons with diabetes. Fam Med. 1995;27:267–71. [PubMed] [Google Scholar]
- 21.Katon W, Russo J, Lin EH, Heckbert SR, Karter AJ, Williams LH, et al. Diabetes and poor disease control: Is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009;71:965–72. doi: 10.1097/PSY.0b013e3181bd8f55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilbourne AM, Reynolds CF, 3rd, Good CB, Sereika SM, Justice AC, Fine MJ. How does depression influence diabetes medication adherence in older patients? Am J Geriatr Psychiatry. 2005;13:202–10. doi: 10.1176/appi.ajgp.13.3.202. [DOI] [PubMed] [Google Scholar]
- 23.Shahin Y. Monitoring of diabetes and hypertension services provided by the UN Relief and Works Agency for Palestine Refugees in the Near East. The Lancet-Palestinian Health Alliance 2012. 2012. [Last accessed 2014 Apr 20]. Available from: http://www.download.thelancet.com/flatcontentassets/pdfs/palestine2012/palestine2012–2.pdf .


