Abstract
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by vascular thrombosis or pregnancy morbidity. Ocular involvement in APS includes a broad spectrum of manifestations involving anterior and posterior segment or the presence of neuroophthalmologic features. Nonarteritic anterior ischemic optic neuropathy (NAION) is a very rare finding, and in this report a case having NAION as the prevailing sign of APS is presented. A middle-aged women who presented with visual disturbances in her left eye (LE) and turned out to have the diagnosis of primary APS with the help of rheumatological investigations is discussed. She was treated with oral steroids for NAION in her LE. With systemic and rheumatological work-up, primary APS was diagnosed, and hydroxychloroquine, coumadin, and aspirin were started, after which she remained stable under control. Due to the important diagnostic and therapeutic implications of APS, it should be considered in the differential diagnosis of NAION, particularly when the etiology is uncertain.
Keywords: Antiphospholipid syndrome, nonarteritic ischemic optic neuropathy, optic neuropathy
Nonarteritic anterior ischemic optic neuropathy (NAION) has been reported in association with a number of systemic conditions. However, it has rarely been reported with antiphospholipid syndrome (APS).[1] APS is an autoimmune disorder characterized by vascular (arterial, venous, or small vessel) thrombosis or pregnancy morbidity. Diagnosis of APS is based on having at least one clinical (vascular occlusion and/or pregnancy complications) finding and one laboratory criterion (repeated positivity for lupus anticoagulants and/or antibodies targeted against cardiolipin or β (2)-glycoprotein in 3 months) at the same time.[2] Ocular involvement in APS includes a broad spectrum of manifestations from the anterior and posterior segment, or the presence of neuroophthalmologic features. Neuroophthalmologic features are transient visual loss, ischemic optic neuropathy (ON), and progressive optic nerve atrophy.[3]
NAION has rarely been reported as the prevailing sign of APS. We here described a case presenting with NAION in whom a primary APS was subsequently diagnosed.
Case Report
A 36 year old Caucasian woman was admitted because of headache and sudden unilateral visual loss in her left eye (LE). She was not a smoker or alcohol consumer. The patient did not have hypertension, hyperlipidemia, and diabetes mellitus. She had a history of abortion in the second trimester. Physical examination was normal.
Ophthalmological examination showed a left relative afferent pupillary defect (RAPD) and swelling of the left optic disc (OD) with accompanying pallor. Visual acuities (VA) were 20/20 and 6/20 in the right and LE, respectively. Color vision was impaired in the LE with Ishihara color plates. Visual field testing with automated perimetry (Humphrey Field Analyser Model 750i, HFA II, Carl Zeiss Meditec Inc. Dublin, CA, USA; 1994-2000 central 30-2 threshold test) showed a dense inferior arcuate defect [Fig. 1]. Examination of the right eye was normal. Initially, a diagnosis of ON was made and intravenous methylprednisolone was started and given 1 g/day for 3 consecutive days. Oral prednisolone 1 mg/ kg/ day was started on day 4 and continued for 1 week and stopped in 1 month by tapering the dose each week. VA increased to 0.7 on day 1, to 0.9 on day 2, and to 1.0 at week 1.
Figure 1.
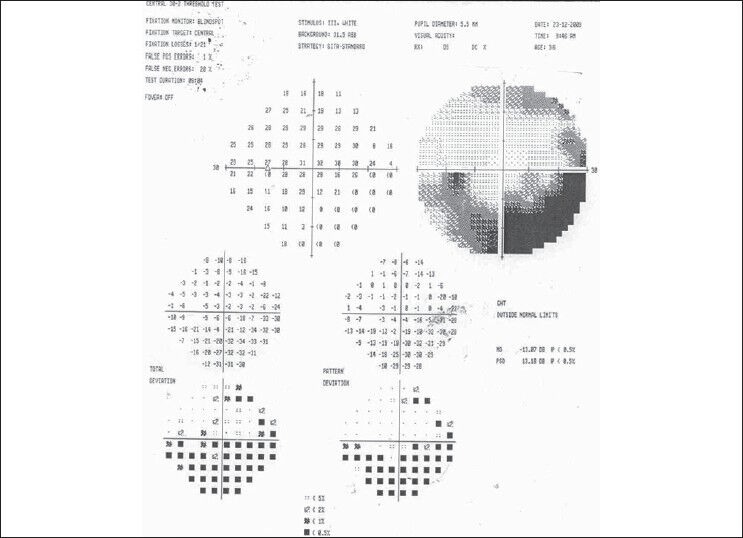
Visual field test demonstrates an inferior arcuate defect in the LE
At follow-up examination at the end of the first month, the visual acuity in the LE was 20/20 and pupillary light reflexes were normal. Cup/disc (c/d) ratio was analyzed with Optical Coherens Tomography (Optovue Fourier domain OCT, Optovue Inc, Freemont, CA, USA). Horizontal c/d ratio was 0.54 in RE and 0.40 in LE. Vertical c/d ratio was 0.32 in RE, and 0.41 in LE. OD edema in LE resolved leaving partial atrophy in the superior part of the optic disc and the visual field test revealed partial improvement of the inferior arcuate defect. Corticosteroid therapy was stopped. Two months later, she presented again with blurred vision in her LE. The VAs were 20/20 in both eyes, with no RAPD. The OD had a slight pallor superiorly [Fig. 2]. Fluorescein angiography showed a patchy background choroidal flourescence and a relative delay in arterio-venous filling in the superior temporal retinal vessels compared with the inferior temporal ones [Fig. 3]. No leakage from the disc or vessels was observed.
Figure 2.

Fundus photograph of the LE. Note the optic disk pallor in the superior half
Figure 3.
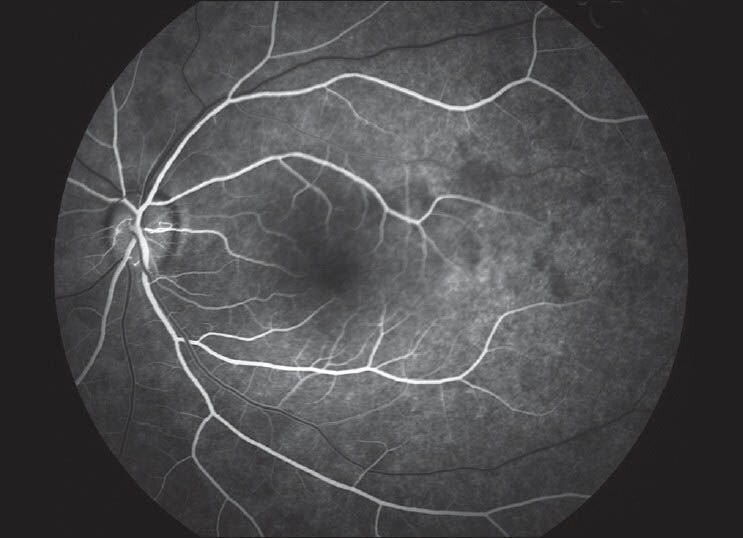
Fundus fluorescein angiography of the LE. Fluorescein angiography showed a patchy background choroidal flourescence and a relative delay in arterio-venous filling in the superior temporal retinal vessels compared with the inferior temporal ones in the early phase. No early hyperfluorescence of the disc or vessels was observed
Extensive investigations for hypertension, hyperlipidemia, diabetes mellitus, atherosclerosis, cardiac diseases connective tissue, and autoimmune disorders were performed. As there was no clinical signs or findings of infectious disease, no extensive work-up was performed. Renal and liver tests, glucose, and lipid profile were all normal. Factor V Leiden and prothrombin gene mutations were absent. SLE and other connective tissue disorders were excluded with intensive investigations. APS was detected in the immunological examination [lupus anticoagulant 62.9 s (normal 31-44); anticardiolipin antibodies IgG, 18.86 (normal 0-10), IgM 30.90 (normal 0-7)]. Primary APS was diagnosed based on the above clinical and laboratory findings and treatment with oral anticoagulant (coumadin 5 mg/day), antiagregan (coraspin 100 mg/day), and antiinflammatory drug (hydroxychloroquine 200 mg/day) was started immediately. We tested lupus anticoagulant and anticardiolipin antibodies IgG and IgM 3 months later, and they were still at high levels, which confirmed the diagnosis.
The patient remained asymptomatic under treatment. One year later, the patient had 20/20 vision in both eyes and did not have any new thrombotic events. She is still under the above-mentioned treatment with excellent treatment efficacy regarding the INR values and without side effects.
Discussion
The systemic features of the APS syndrome are characterized by large variability depending on the affected organs. However, studies on the frequency and clinical presentation of the ocular manifestation as the presenting sign of APS in patients suffering from unexplained ocular disease are missing.[4] Herein, we present a case of NAION as the first manifestation of APS, which is very rarely described.
Ocular involvement associated with APS include vaso-occlusive retinopathy and ON.[5] Prevalence of ocular vaso-occlusive disease has been estimated in 29% of patients with primary APS, but ON is a very rare manifestation of primary APS and only a few isolated cases have been reported in the literature.[6] Tsironi et al.[4] reported a case series with ocular disorders as the prevailing manifestations of APS. The first patient had bilateral retinal occlusive disease and the second and third patient had unilateral NAION with macular edema.[4] Our case was also unilateral, which responsed to CS therapy with recurrence of blurred vision after its cessation. Reino et al.[1] reviewed cases of ON in APS from the recent literature. ON was associated with systemic thrombotic manifestations, most commonly with neurological disorders followed by cardiac disease, arterial and venous thrombosis, miscarriage, and livedo reticularis.[1] However, in our case there was no systemic thrombotic events. The only important finding was her history of abortion. The most probable pathogenesis of ON is an abnormal microcirculation secondary to thrombosis of the small arterial vessels that arise from the choroidal circulation and supply the anterior portion of optic nerve caused by antiphospholipid antibodies, similar to other clinical manifestations of the primary APS.[7] Giorgi and Gabrieli[2] suggested that a monolateral ON in patients with significant levels of aPL could be considered as a focal lesion due to microthrombotic events involving the ciliary vasculature.
Treatment of ON in primary APS is controversial and should be individually tailored. Anticoagulation therapy can prevent future events not only in eyes but also episodes in other vital organs.[5,8] As thrombosis with no evidence of vasculitis seems to be probably the most important mechanism of this ON, treatment with aspirin or anticoagulants must be tried, although in several occasions prednisolone has also been used. Corticosteroids have no established role in the treatment of APS but are used for rheumatic symptoms in patients with accompanying systemic autoimmune illness. However, high doses of corticosteroids are usually given empirically to patients with severe thrombocytopenia, hemolytic anemia, and catastrophic APS.
Our patient received systemic steroids because of the initial diagnosis of ON. As APS was diagnosed during rheumatologic work-up 2 months after the completion of the steroid therapy, anticoagulant therapy with antiinflammatory drug hydroxychloroquine was started. The protective effect of hydroxychloroquine on thrombosis in systemic lupus erythematosus patients has been shown in the literature. Furthermore, use of this drug has been considered as a new approach on prevention of the thrombosis in the APS.[9,10]
In conclusion, albeit rarely ON may be observed as a presenting manifestation in primary APS, it is advisable that patients with ON in whom the etiology is uncertain may be tested for the presence of antiphospholipid antibodies. Due to the important diagnostic and therapeutic implications of APS, the possibility of ocular features as the first clinical manifestation of APS, particularly in patients with no evident risk factors for ocular disease, should be kept in mind of ophthalmologists.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Reino S, Munoz-Rodriguez FJ, Cervera R, Espinosa G, Font J, Ingelmo M. Optic neuropathy in the primary antiphospholipid syndrome: Report of a case and review of the literature. Clin Rheumatol. 1997;16:629–31. doi: 10.1007/BF02247807. [DOI] [PubMed] [Google Scholar]
- 2.Giorgi D, Balacco Gabrieli C. Optic neuropathy in systemic lupus erythematosus and antiphospholipid syndrome (APS): Clinical features, pathogenesis, review of the literature and proposed ophthalmological criteria for APS diagnosis. Clin Rheumatol. 1999;18:124–31. doi: 10.1007/s100670050069. [DOI] [PubMed] [Google Scholar]
- 3.Miserocchi E, Baltatzis S, Foster CS. Ocular features associated with anticardiolipin antibodies: A descriptive study. Am J Ophthalmol. 2001;131:451–6. doi: 10.1016/s0002-9394(00)00884-9. [DOI] [PubMed] [Google Scholar]
- 4.Tsironi E, Gatzelis N, Kotoula MG, Zachou K, Pefkianaki M, Zacharaki F, et al. Ocular disorders as the prevailing manifestations of antiphospholipid sndrome: A case series. Cases J. 2009;2:159. doi: 10.1186/1757-1626-2-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine SR, Crofts JW, Lesser GR, Floberg J, Welch KM. Visual symptoms associated with the presence of a lupus anticoagulant. Ophthalmology. 1988;95:686–92. doi: 10.1016/s0161-6420(88)33139-8. [DOI] [PubMed] [Google Scholar]
- 6.Levine SR, Briley DP, Caull BM, Goodnight SH., Jr Neurological disease associated with antiphospholipid antibodies. Ann Neurol. 1989;25:221–7. doi: 10.1002/ana.410250303. [DOI] [PubMed] [Google Scholar]
- 7.Cervera R, Asherson RA, Lie JT. Clinicopathological correlations of the antiphospholipid syndrome. Semin Arthritis Rheum. 1995;24:262–72. doi: 10.1016/s0049-0172(95)80036-0. [DOI] [PubMed] [Google Scholar]
- 8.Galetta SL, Plock GL, Kushner MJ, Wyszynski RE, Brucker AJ. Ocular thrombosis associated with antiphospholipid antibodies. Ann Ophthalmol. 1991;23:207–12. [PubMed] [Google Scholar]
- 9.Pierangeli SS, Erkan D. Antiphospholipid syndrome treatment beyond anticoagulation: Are we there yet? Lupus. 2010;19:475–85. doi: 10.1177/0961203310361489. [DOI] [PubMed] [Google Scholar]
- 10.Szymezak J, Ankri A, Fischer AM, Darnige L. Hydroxychloroquine: A new approach of thrombosis in the antiphospholipid syndrome. Rev Med Interne. 2010;31:854–7. doi: 10.1016/j.revmed.2010.08.018. [DOI] [PubMed] [Google Scholar]


