Abstract
Context:
Antibiotics are the mainstay of treatment for bacterial infections in patients of all ages. Athletes who maximally train are at risk for illness and various infections. Routinely used antibiotics have been linked to tendon injuries, cardiac arrhythmias, diarrhea, photosensitivity, cartilage issues, and decreased performance.
Evidence Acquisition:
Relevant articles published from 1989 to 2012 obtained through searching MEDLINE and OVID. Also, the Food and Drug Administration website was utilized.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
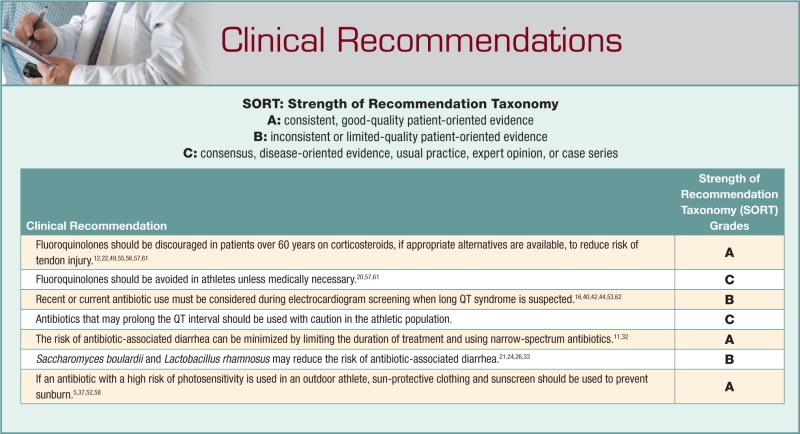
The team physician should consider alternative medications in place of the “drug of choice” when adverse drug effects are a concern for an athlete’s health or performance. If alternative medications cannot be selected, secondary preventative measures, including sunscreen or probiotics, may be needed.
Conclusion:
Physicians choose medications based on a variety of factors to help ensure infection resolution while limiting potential side effects. Extra precautions are indicated when treating athletes with certain antibiotics.
Keywords: antibiotics, tendon injuries, antibiotic-associated diarrhea, photosensitivity, long QT
Team physicians treat musculoskeletal problems as well as medical conditions, including bacterial infections. Several considerations are appropriate when treating with antibiotics, including the specific pathogen, susceptibility, dosing frequency, mode of administration, and allergies. Special considerations should also be given to athletic participation and exercise patterns.
Athletes use oral antibiotics twice as frequently as age-matched controls (2.7% vs 1.3%),1,2 perhaps because physicians are quicker to prescribe antibiotics in hopes of helping the athlete return to play as soon as possible. Antibiotics can have unintended side effects. Tailoring a treatment plan for effective antibiotics that limit an athlete’s risk is paramount to the athlete’s safety and ability to continue exercise
Tendon Injuries
Fluoroquinolones are broad-spectrum antibiotics that have bactericidal activity against a large number of both Gram-negative and Gram-positive bacteria. Because of their broad-spectrum coverage, by 2002, fluoroquinolones became the most commonly prescribed class of antibiotics for adults in the United States.28 However, as fluoroquinolone use became more widespread, adverse reactions related to these drugs have become apparent.10 The association between tendon injuries and fluoroquinolones has been receiving increased attention, most notably with the Achilles tendon.55,57 In 2008, the Food and Drug Administration reviewed the evidence and issued a black box warning regarding the increased risk for tendonitis and tendon rupture.22 The literature reports that patients taking fluoroquinolones have a 3 to 6 times increased risk of developing tendinitis or rupturing their Achilles tendon or an absolute risk of 7.74 per 100,000 days at risk and 3.2 per 1000 patient years.49,56
One proposed mechanism of tendon injury in the central avascular portion of the Achilles tendon “watershed area” is the accumulation of free radicals during the inflammatory process secondary to antibiotic use.46 These substances are toxic to tendon cells and can lead to necrosis.12 With frequent use, there also appears to be histologic changes, including abnormal arrangement of tendon fibers, cystic changes, fibrotic changes, hypercellularity, edema, and neovascularization leading to a remodeling process that ultimately weakens the tendon matrix.12
Age and concomitant steroid use have been associated with Achilles tendon ruptures in patients using fluoroquinolones.12,22,57,61 In a case-crossover study performed by Wise et al, patients over the age of 60 who used corticosteroids were at the highest risk of developing Achilles tendinopathy and/or rupture as compared with the general population.49,55,56,61 This risk should be discussed with athletes, and alternative antibiotics might be considered if appropriate.20,57,61
Cardiac Arrhythmias
Cardiac effects from antibiotics may have significant consequences regarding participation and safety. Macrolides are a popular class of antibiotics used for a variety of mild to moderate bacterial infections. Macrolides and fluoroquinolones may be associated with increased risk of ventricular arrhythmia and cardiac arrest.62 There is a small increase in cardiovascular deaths with azithromycin use.40 A review by the Food and Drug Administration has resulted in additional warnings for azithromycin.16 Prolongation of the QT interval by macrolides (erythromycin and clarithromycin) has been well established. These changes have also been seen in patients taking fluoroquinolones, especially moxifloxacin.40,42,44,53 A prolonged QT interval is linked to torsades de pointes, which can progress to a potentially fatal ventricular arrhythmia.66
Prolongation of the QTc (corrected QT interval) on electrocardiogram can be important in the consideration for participation in competitive sports. Criteria for participation with congenital long QT syndrome were outlined at the 36th Bethesda Conference65 and by the European Society of Cardiology in its 2005 guidelines.30 The conference currently defines the upper limit to >470 ms in men and >480 ms in women,65 while the European Society of Cardiology recommends further evaluation in men with QTc intervals >440 ms and women with >460 ms.30 Drug-induced prolongation of the QTc can carry substantial risk.66 While the mean increase in the QT interval with fluoroquinolones is approximately 3 to 6 ms and is thought to have little clinical significance, it may place patients at an increased risk for ventricular arrhythmias,47 especially those with long QT syndrome. Since electrocardiogram testing is used in organized competitive sports, even mild prolongation of the QTc could confuse evaluation, delay participation, and cause limitations or possibly disqualification. Antibiotic use close to or at the time of testing should be addressed during history. A prolonged QT interval may resolve over time and not necessitate extensive cardiac evaluation.25,40
Most athletes will not undergo formal evaluation before participation in athletics and may have other risk factors that put them at risk for arrhythmia with concomitant use of antibiotics (Table 1).62
Table 1.
Risk factors for arrhythmia with concomitant use of antibiotics62
| Organic heart disease |
| Congenital long QT syndrome |
| Ischemic heart disease |
| Congestive heart failure |
| Dilated cardiomyopathy |
| Hypertrophic cardiomyopathy |
| Myocarditis |
| Metabolic abnormalities |
| Hypokalemia |
| Hypocalcemia |
| Hypomagnesaemia |
| Bradycardia |
| Atrioventricular and sinoatrial blocks |
| Drug-related factors |
| Actions on cytochrome P450 enzymes |
| Polypharmacy |
| Female preponderance |
| Hepatic impairment |
Antibiotic-Associated Diarrhea
Antibiotic-associated diarrhea (AAD) is a common adverse reaction with many antibacterials, with rates ranging from 5% to 39%.31,51 Diarrhea can start acutely or up to 3 to 4 weeks after the initiation of antibiotic therapy. Antibiotics disrupt the normal intestinal microflora, leading to proliferation of pathogenic microorganisms (eg, Clostridium difficile) or impairment of the metabolic function of the microflora.11,34,38 Broad-spectrum antibiotics, especially those that affect Enterobacteriaceae and anaerobic bacteria (eg, aminopenicillins, cephalosporins, clindamycin), are likely to have a significant effect on the normal flora, as well as antibiotics with a high intraluminal concentration in the intestinal tract.11,23 Risk factors for AAD include duration, repeated use, and combination of antibacterial therapies.11,34 The dosage and route of antibiotics are usually not risk factors; exceptions are erythromycin and beta-lactams11,60 (Table 2). The prevalence of AAD in children is 11%, with amoxicillin-clavulanate (23%), erythromycin (16%), cephalosporins (9%), macrolides (9%), trimethoprim-sulfamethoxazole (6%), and penicillin G and V (3%).54
Table 2.
Rates of antibiotic-associated diarrhea from multiple studies
Two ways to minimize the risk of AAD is to limit the duration of treatment to a minimum and use a narrow-spectrum antibiotic.32 Another method may be the use of probiotics. Some studies showed that Saccharomyces boulardii can prevent AAD,26 while others showed no difference.27 One study showed that probiotics did not help with acute diarrhea but rather helped prevent delayed-onset diarrhea.21 A sensitivity analysis found that only 2 probiotic strains could prevent AAD: S boulardii and Lactobacillus rhamnosus.33 A Cochrane review showed that probiotics are effective in preventing AAD in children (relative risk, 0.49); the number needed to treat to prevent 1 case of AAD was 10.24
Photosensitivity
Common photosensitizers in the athlete population include tetracyclines, fluoroquinolones, and sulfonamides.37,59 Photosensitivity can be either phototoxic after a single dose or photoallergic, which is immunologically mediated and requires re-exposure.15,37 Many drugs can cause both reactions. Clinical presentation resembles an exaggerated sunburn with clear delineation of sun-exposed areas.37 Photosensitivity can increase the risk of skin cancer from sunburn.4,15,37
Tetracyclines are commonly prescribed for acne vulgaris and other common infections that occur in high school and college athletes. Doxycycline has the highest incidence of photosensitivity (20%), while minocycline rarely causes photosensitivity.58 The effect can be seen within 2 weeks of the onset of treatment and is dose dependent.63 Doxycycline is also known to cause photo-onycholysis, with onset in as few as 8 days64; these changes generally resolve spontaneously after 3 to 4 months.39 Although minocycline generates less photosensitivity than other tetracyclines, it can cause reversible or irreversible hyperpigmentation in 2% to 15% of cases.18,48
Fluoroquinolones are also photosensitizers.52 There are a variety of mechanisms, including free radical formation and reactive oxygen species.52 Fortunately, the worst offenders (nalidixic acid and similar generation quinolones) in this class are less commonly used or unavailable in the United States.58 Ciprofloxacin is often used for a variety of conditions, including urinary tract infection. The incidence of photosensitivity with ciprofloxacin is 1% to 4%,50 while levofloxacin carries a lower risk of 0.2%.14,29,58
Sulfonamides, especially sulfamethoxazole, can cause a number of cutaneous reactions, including photosensitivity and the more severe Stevens-Johnson syndrome.37,52,58 The incidence of cutaneous reactions is between 1:1000 and 1:100,000 and can occur within 3 days of treatment.52
If an athlete is participating in outdoor events, it is best to avoid photosensitizing antibiotics. If use cannot be avoided, use of sun-protective clothing and broad-spectrum sunscreen should be emphasized.
Bone, Cartilage, and Teeth
Tetracycline and its derivatives cause intrinsic staining of the oral cavity and teeth of children during osteogenesis and odontogenesis.43 Hence, tetracyclines are contraindicated in pregnant women and in children under the age of 8 years because of their teratogenic effects on bone and tooth development in the fetus and because staining is more prevalent in growing children.13,19,43 Tetracyclines also cause hyperpigmentation of the skin, thyroid, nails, sclera, conjunctiva, and bone.43
The prevalence of tetracycline staining in the oral cavity is 3% to 6%.3,6 Staining can also occur on the long bones of the body.41 Minocycline treatment of severe acne, which is sometimes used for extended periods of treatment, can cause dental and hard palate staining.3,6 This cosmetic concern should be explained as a rare but potential side effect of treatment. Staining is caused by chelation of iron and the formation of insoluble deposits in skin, hair, and bone.3,8 This staining is reversible in bone, as humans remodel 10% of their skeleton annually.3,17 The staining of teeth, however, is permanent, as teeth do not remodel. In an animal study, fluoroquinolones caused articular cartilage damage during growth in lambs; there was no change in growth velocity.45 One study on human cadavers was inconclusive.36
Fatigue or Decreased Performance
Antibiotics may cause fatigue or affect an athlete’s performance.35 However, it is difficult to discriminate the effects of the antibiotic or the illness itself. A study comparing tetracycline, ampicillin, and trimethoprim-sulfamethoxazole to a placebo in 50 healthy male military trainees found that there were no differences in muscle enzyme activity, muscle strength, VO2 max, and subjective fatigue after 3 days of treatment.9 However, since most antibiotic treatment courses last longer than 3 days, it is possible that longer courses could cause a negative effect. Higher fatigue scores have been reported with a greater number of antibiotic courses and total use of antibiotics.7 In a side effect review of doxycycline and minocycline, somnolence was found in 1.2% with doxycycline, with weakness or fatigue with minocycline in 23%.48
Conclusion
There are no “perfect” antibiotics, and it may be impossible to avoid all side effects. AAD and tendon injuries may hinder performance, while prolongation of the QT interval may be more serious.
Acknowledgments
HB Fagan, MD
Deena Chisholm
Barbara Henry
Teresa Mazzella
Footnotes
The authors declared no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Alaranta A, Alarenta H, Helenius I. Use of prescription drugs in athletes. Sports Med. 2008;38:449-463 [DOI] [PubMed] [Google Scholar]
- 2. Alaranta A, Alaranta H, Heliövaara M, Airaksinen M, Helenius I. Ample use of physician-prescribed medications in Finnish elite athletes. Int J Sports Med. 2006;27:919-925 [DOI] [PubMed] [Google Scholar]
- 3. Ayangco L, Sheridan PJ. Minocycline-induced staining of torus palatinus and alveolar bone. J Periodontol. 2003;75:669-671 [DOI] [PubMed] [Google Scholar]
- 4. Baker CS. Photosensitivity. Med J Aust. 1996;165:96-101 [DOI] [PubMed] [Google Scholar]
- 5. Balk SJ; Council on Environmental Health; Section on Dermatology. Ultraviolet radiation: a hazard to children and adolescents. Pediatrics. 2011;127:e791-817 [DOI] [PubMed] [Google Scholar]
- 6. Berger RS, Mandel EB, Hayes TJ, Grimwood RR. Minocycline staining of the oral cavity. J Am Acad Dermatol. 1989;21:1300-1301 [DOI] [PubMed] [Google Scholar]
- 7. Bhattacharyya N, Kepnes LJ. Associations between fatigue and medication use in chronic rhinosinusitis. Ear Nose Throat J. 2006;85:510, 512, 514-515 [PubMed] [Google Scholar]
- 8. Bowles WH, Bokmeyer TJ. Staining of adult teeth by minocycline: binding of minocycline by specific proteins. J Esthet Dent. 1997;9:30-34 [DOI] [PubMed] [Google Scholar]
- 9. Burstein R, Hourvitz A, Epstein Y, et al. The relationship between short-term antibiotic treatments and fatigue in healthy individuals. Eur J Appl Physiol Occup Physiol. 1993;66:372-375 [DOI] [PubMed] [Google Scholar]
- 10. Carbon C. Comparison of side effects of levofloxacin versus other fluoroquinolones. Chemotherapy. 2001;47(suppl 3):9-14 [DOI] [PubMed] [Google Scholar]
- 11. Chassany O, Michaux A, Bergmann JF. Drug-induced diarrhoea. Drug Saf. 2000;22:53-72 [DOI] [PubMed] [Google Scholar]
- 12. Childs SG. Pathogenesis of tendon rupture secondary to fluoroquinolone therapy. Orthop Nurs. 2007;26:175-182 [DOI] [PubMed] [Google Scholar]
- 13. Conchie JM, Munroe JD, Anderson DO. The incidence of staining of permanent teeth by the tetracyclines. Can Med Assoc J. 1970;103:351-356 [PMC free article] [PubMed] [Google Scholar]
- 14. Davis R, Bryson HM. Levofloxacin: a review of its antibacterial activity, pharmacokinetics and therapeutics efficacy. Drugs. 1994;47:677-700 [DOI] [PubMed] [Google Scholar]
- 15. Epstein JH. Phototoxicity and photoallergy. Semin Cutan Med Surg. 1999;18:274-284 [DOI] [PubMed] [Google Scholar]
- 16. Food and Drug Administration. Drug safety communication: azithromycin (Zithromax or Zmax) and the risk of potentially fatal heart rhythms. http://www.fda.gov/drugs/drugsafety/ucm341822.htm Accessed July 1, 2013
- 17. Frost HM. Tetracycline-based histological analysis of bone remodeling. Calcif Tissue Res. 1969;3:211-237 [DOI] [PubMed] [Google Scholar]
- 18. Geria AN, Tajirian AL, Kihiczak G, Schwartz RA. Minocycline-induced skin pigmentation: an update. Acta Dermatovenerol Croat. 2009;17:123-126 [PubMed] [Google Scholar]
- 19. Grossman ER. Tetracycline and staining of the teeth. JAMA. 1986;255:2442-2443 [PubMed] [Google Scholar]
- 20. Hall MM, Finnoff JT, Smith J. Musculoskeletal complications of fluoroquinolones: guidelines and precautions for usage in the athletic population. PMR 2011;3:132-142 [DOI] [PubMed] [Google Scholar]
- 21. Hickson M, D’Souza AL, Muthu N, et al. Use of probiotic Lactobacillus preparation to prevent diarrhea associated with antibiotics: randomized double blind placebo controlled trial. BMJ. 2007;335:80-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Information for healthcare professionals: fluoroquinolone antimicrobial drugs [ciprofloxacin (marketed as Cipro and generic ciprofloxacin), ciprofloxacin extended-release (marketed as Cipro XR and Proquin XR), gemifloxacin (marketed as Factive), levofloxacin (marketed as Levaquin), moxifloxacin (marketed as Avelox), norfloxacin (marketed as Noroxin), and ofloxacin (marketed as Floxin)]. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm126085.htm Accessed March 5, 2013
- 23. Jaimes EC. Lincocinamides and the incidence of antibiotic-associated colitis. Clin Ther. 1991;13:270-280 [PubMed] [Google Scholar]
- 24. Johnston BC, Supina AL, Ospina M, Vohra S. Probiotics in the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev. 2007;2:CD004827. [DOI] [PubMed] [Google Scholar]
- 25. Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62:760-781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kotowska M, Albrecht P, Szajewska H. Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther. 2005;21:583-590 [DOI] [PubMed] [Google Scholar]
- 27. Lewis SJ, Potts LF, Barry RE. The lack of therapeutic effect of Saccharomyces boulardii in the prevention of antibiotic-associated diarhoea in elderly patients. J Infect. 1998;36:171-174 [DOI] [PubMed] [Google Scholar]
- 28. Linder JA, Huang ES, Steinman MA, Gonzales R, Stafford S. Fluoroquinolone prescribing in the United States: 1995 to 2002. Am J Med. 2005;118:259-268 [DOI] [PubMed] [Google Scholar]
- 29. Liu HH. Safety profile of the fluoroquinolones: focus on levofloxacin. Drug Saf. 2010;33:353-369 [DOI] [PubMed] [Google Scholar]
- 30. Maron BJ, Zipes DP. Introduction: eligibility recommendations for competitive athletes with cardiovascular abnormalities—general considerations. J Am Coll Cardiol. 2005;45:1318-1321 [DOI] [PubMed] [Google Scholar]
- 31. McFarland LV. Epidemiology, risk factors and treatments for antibiotic-associated diarrhea. Dig Dis. 1998;16:292-307 [DOI] [PubMed] [Google Scholar]
- 32. McFarland LV. Evidence-based review of probiotics for antibiotic-associated diarrhea and Clostridium difficile infections. Anaerobe. 2009;15:274-280 [DOI] [PubMed] [Google Scholar]
- 33. McFarland LV. Meta-analysis of probiotics for prevention of antibiotic associated diarrhea and treatment of Clostridium difficile disease. Am J Gastroenterol. 2006;101:812-822 [DOI] [PubMed] [Google Scholar]
- 34. McFarland LV. Risk factors for antibiotic-associated diarrhea [in French]. Ann Med Interne (Paris). 1998;149:261-266 [PubMed] [Google Scholar]
- 35. McGrew CA. Acute infections. In: McKeag DB, Moeller JL, eds. ACSM’s Primary Care Sports Medicine. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:252 [Google Scholar]
- 36. Menschik M, Neumuüller J, Steiner CW, et al. Effects of ciprofloxacin and ofloxacin on adult human cartilage in vitro. Antimicrob Agents Chemother. 1997;41:2562-2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Moore DE. Drug-induced cutaneous photosensitivity: incidence, mechanism, prevention and management. Drug Saf. 2002;25:345-372 [DOI] [PubMed] [Google Scholar]
- 38. Nord CE, Heimdahl A, Kager L. Antimicrobial induced alterations of the human oropharyngeal and intestinal microflora. Scan J Infect Dis. 1896;49(suppl):64-72 [PubMed] [Google Scholar]
- 39. Rabar D, Combemale P, Peyron F. Doxycycline-induced photo-onycholysis. J Travel Med. 2004;11:386-387 [DOI] [PubMed] [Google Scholar]
- 40. Ray WA, Murray KT, Hall K, Arbogast PG, Stein CM. Azithromycin and the risk of cardiovascular death. N Engl J Med. 2012;366:1881-1890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Reed DN, Gregg FO, Corpe RS. Minocycline-induced black bone disease encountered during total knee arthroplasty. Orthopedics. 2012;35:e737-e739 [DOI] [PubMed] [Google Scholar]
- 42. Rubinstein E, Camm J. Cardiotoxicity of fluoroquinolones. J Antimicrob Chemother. 2002;49:593-596 [DOI] [PubMed] [Google Scholar]
- 43. Sanchez A, Rogers RS, 3rd, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol. 2004;43:709-715 [DOI] [PubMed] [Google Scholar]
- 44. Sanguinetti MC, Jiang C, Curran ME, Keating MT. A mechanistic link between an inherited and an acquired cardiac arrhythmia: HERG encodes the IKr potassium channel. Cell. 1995;81:299-307 [DOI] [PubMed] [Google Scholar]
- 45. Sansone J, Wilsman NJ, Leiferman EM, Conway J, Hutson P, Noonan KJ. The effect of fluoroquinolone antibiotics on growing cartilage in the lamb model. J Pediatr Orthop. 2009;29:189-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Seeger JD, West WA, Fife D, Noel GJ, Johnson LN, Walker AM. Achilles tendon rupture and its association with fluoroquinolone antibiotics and other potential risk factors in a managed care population. Pharmacoepidemiol Drug Saf. 2006;15:784-792 [DOI] [PubMed] [Google Scholar]
- 47. Shantsila E, Watson T, Lip GY. Drug-induced QT-interval prolongation and proarrhythmic risk in the treatment of atrial arrhythmias. Europace. 2007;9(suppl 4):iv37-iv44 [DOI] [PubMed] [Google Scholar]
- 48. Smith K, Leyden JJ. Safety of doxycycline and minocycline: a systemic review. Clin Ther. 2005;27:1329-1342 [DOI] [PubMed] [Google Scholar]
- 49. Sode J, Obel N, Hallas J, Lassen A. Use of fluoroquinolone and risk of Achilles tendon rupture: a population-based cohort study. Eur J Clin Parmacol. 2007;63:499-503 [DOI] [PubMed] [Google Scholar]
- 50. Stahlmann R. Safety profile of the quinolones. J Antimicrob Chemother. 1990;26(suppl D):31-44 [DOI] [PubMed] [Google Scholar]
- 51. Surawicz CM. Antibiotic-associated diarrhea and pseudomembranous colitis: are they less common with poorly absorbed antimicrobials? Chemotherapy. 2005;51(suppl 1):81-89 [DOI] [PubMed] [Google Scholar]
- 52. Svensson CK, Cowen EW, Gaspari AA. Cutaneous drug reactions. Pharmacol Rev. 2001;53:357-379 [PubMed] [Google Scholar]
- 53. Tsikouris JP, Peeters MJ, Cox CD, Meyerrose GE, Seifert CF. Effects of three flouroquinolones on QT analysis after standard treatment courses. Ann Noninvasive Electrocardiol. 2006;11:52-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Turck D, Bernet JP, Marx J, et al. Incidence and risk factors of oral antibiotic-associated diarrhea in an outpatient pediatric population. J Pediatr Gastroenterol Nutr. 2003;37:22-26 [DOI] [PubMed] [Google Scholar]
- 55. van der Linden PD, Sturkenboom MC, Herings RM, Leufkens HM, Rowlands S, Stricker BH. Increased risk of Achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids. Arch Intern Med. 2003;163:1801-1807 [DOI] [PubMed] [Google Scholar]
- 56. van der Linden PD, Sturkenboom MC, Herings RM, Leufkens HG, Stricker BH. Fluoroquinolones and risk of Achilles tendon disorders: case-control study. BMJ. 2002;324:1306-1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. van der Linden PD, van Puijenbrock EP, Feenstra J, et al. Tendon disorders attributed to fluoroquinolones: a study on 42 spontaneous reports in the period 1988 to 1998. Arthritis Rheum. 2001;45:235-239 [DOI] [PubMed] [Google Scholar]
- 58. Vassileva SG, Mateev G, Parish LC. Antimicrobial photosensitive reactions. Arch Intern Med. 1998;158:1993-2000 [DOI] [PubMed] [Google Scholar]
- 59. Wainwright NJ, Collins P, Ferguson J. Photosensitivity associated with antibacterial agents. Drug Saf. 1993;9:437-440 [DOI] [PubMed] [Google Scholar]
- 60. Weber FH, Jr, Richards RD, McCallum RW. Erythromycin: a motilin agonist and gastrointestinal prokinetic agent. Am J Gastroenterol. 1993;88:485-490 [PubMed] [Google Scholar]
- 61. Wise BL, Peloquin C, Choi H, Lane NE, Zhang Y. Impact of age, sex, obesity, and steroid use on quinolone-associated tendon disorders. Am J Med. 2012;125:1228.e23-1228.e28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. BMJ. 2003;89:1363-1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yap LM, Foley PA, Crouch RB, Baker CS. Drug-induced solar urticaria due to tetracycline. Australas J Dermatol. 2000;41:181-184 [DOI] [PubMed] [Google Scholar]
- 64. Yong CK, Prendiville J, Peacock D, Wong LT, Davidson AG. An unusual presentation of doxycycline-induced photosensitivity. Pediatrics. 2000;106:E13. [DOI] [PubMed] [Google Scholar]
- 65. Zambon A, Polo Friz H, Contiero P, Corrao G. Effect of macrolide and fluoroquinolone antibacterials on the risk of ventricular arrhythmia and cardiac arrest: an observational study in Italy using case-control, case-crossover and case-time-control designs. Drug Saf. 2009;32:159-167 [DOI] [PubMed] [Google Scholar]
- 66. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death—executive summary: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Eur Heart J. 2006;27:2099-2140 [DOI] [PubMed] [Google Scholar]