Abstract
Objective
Assess utility of functional status in classifying patients by discharge setting following inpatient rehabilitation for hip fracture.
Design
Retrospective cohort study.
Setting
1,257 inpatient rehabilitation facilities in the United States.
Patients
Medicare beneficiaries (N=117,168) receiving inpatient rehabilitation for hip fracture in 2007-2009.
Methods
Receiver operating characteristic (ROC) curve analyses to assess the overall discriminatory ability of functional status scores (FIM total, FIM cognition, and FIM motor) and to identify the functioning threshold that best differentiates patients by discharge setting.
Main Outcome Measurements
Discharge setting (community versus institutional).
Results
Approximately 68% of patients were discharged to the community following inpatient rehabilitation for hip fracture. ROC curve analyses indicate discharge FIM motor ratings (area under the curve: 0.84) alone are as effective as a multivariable model (area under the curve: 0.85) including sociodemographic and clinical factors in discriminating patients discharged to the community from those discharged to an institution. Discharge FIM motor rating of 58 yielded the best balance in sensitivity and specificity for classifying discharge setting.
Conclusions
Discharge FIM motor ratings demonstrated good discriminatory ability for classifying discharge setting. A FIM motor rating of 58 may serve as a clinical tool to guide treatment plans and/or as additional information in complex discharge planning decisions for patients with hip fracture.
Keywords: hip fracture, outcome assessment, rehabilitation
Hip fracture is one of the most serious medical events geriatric patients experience.1-3 With rising life expectancy around the globe, it is estimated that the incidence of hip fractures will increase from 1.7 million in 1990 to 6.3 million by 2050.2 The complications of hip fracture include chronic pain, disability, diminished quality of life, caregiver burden, and premature death. Many patients with hip fracture require inpatient rehabilitation because they are unable to care for themselves and live independently at hospital discharge.
The goal of inpatient rehabilitation for patients with hip fracture is to regain their pre-injury level of functioning. Successful inpatient rehabilitation is commonly marked by discharge to the community. Several factors are associated with discharge to community,4-7 including demographics, family/social support, and patient preferences, which are beyond the control of rehabilitation facilities. Functional status, however, is strongly associated with discharge disposition and the primary modifiable variable for the multidisciplinary rehabilitation teams. The Functional Independence Measure (FIM) instrument is the standard functional measure in inpatient medical rehabilitation settings. The FIM instrument covers two broad functional domains: motor and cognition.
The goals of this study were: 1) identify which discharge functional score (FIM total, FIM motor, or FIM cognition) best discriminates community vs. institutional discharges, 2) compare the discriminatory ability of functional status alone with an adjusted model including sociodemographic and other clinical factors, and 3) determine the optimal cut-point in functional scores that best differentiates patients returning to the community from those discharged to an institution. An effective cutoff score could be a practical clinical tool to help clinicians in setting goals and individualized treatment plans and also serve as a benchmark for use in discharge planning decisions.
METHODS
Data Source and Study Population
We used the 100% inpatient rehabilitation facility-patient assessment instrument (IRF-PAI) files from the Centers for Medicare and Medicaid Services (CMS). Medicare beneficiaries with hip fracture who were discharged in 2007-2009 were included in the analyses. The cohort was identified by impairment group codes 08.11 (post unilateral hip fracture) and 08.12 (post bilateral hip fractures). Inclusion criteria were age 65 years or older, living in the community prior to injury, admission for initial rehabilitation, duration from injury to IRF admission ≤ 45 days, length of rehabilitation stay between 3 and 45 days, and discharged from the IRF alive. N = 118,668 over the 3-year study period. The 45-day limits capture 95-99% of patients and were chosen to limit the analyses to those experiencing typical delays and stays. Cases were excluded if missing information on marital status or discharge setting (n = 1,500). The final sample contained 117,168 cases from 1,257 inpatient rehabilitation units and hospitals. This study was approved by the University’s Institutional Review Board.
Study Variables
Sociodemographic variables included age (years), sex, race/ethnicity (black, Hispanic, white, other; recoded as white versus minority for entry in multivariable model), and marital status (married versus not married). Clinical factors included fracture type (unilateral vs. bilateral), duration from fracture onset to rehabilitation admission (days), length of stay (days), and the sum of comorbid conditions. The IRF-PAI file allows for reporting up to ten comorbid conditions. We summed the total number of ICD-9 codes across the ten comorbid variables for each patient (range 0-10).
Functional status was evaluated using items from the FIM instrument, which is administered within 3 days of admission to and 3 days of discharge from inpatient rehabilitation. The FIM instrument includes 18 items that assess patient abilities across 6 subscales: self care, sphincter control, transfers, mobility, communication, and social cognition. Scores for each item range from 1 (total assistance) to 7 (complete independence). The reliability and validity of the FIM data have previously been substantiated.8 FIM total represents the summation of all 18 items (range: 18–126). FIM motor is the summation of 13 items (range: 13-91) covering the self care, sphincter control, transfers, and mobility subscales. FIM cognition is the summation of 5 items (range 5-35) covering the communication and social cognition subscales. Stineman et al.9 used multitrait scaling analyses to evaluate the psychometric properties of FIM items and determined that the unweighted summed scores (motor, cognitive, and/or total) are appropriate outcome measures. Internal consistency (Cronbach’s alpha) for our data ranged from 0.85 for FIM motor to 0.95 for FIM cognition.
Discharge setting in the IRF-PAI includes 13 options, including death. The 12 settings were coded into two broad settings for presentation and analysis: community (home, board and care, transitional living, and assisted living) and institution (acute care, long-term care, skilled nursing, nursing home, rehabilitation, alternate care, subacute setting, and other).
Data Analysis
Descriptive summaries of patient demographic, clinical, and functional characteristics were stratified by discharge setting. Univariate associations between discharge setting and various patient characteristics were tested using independent t-tests and chi-square tests or Fisher’s exact test as appropriate. Backwards stepwise logistic regression was used to create a parsimonious model estimating each patient’s predicted probability of community discharge. Alpha was set at 0.05 for remaining in the model. Variables included in the model were age, sex, race/ethnicity, marital status, fracture type, comorbidity sum, duration to admit, length of stay, and discharge FIM cognition and motor ratings.
Four separate receiver operating characteristic (ROC) curves were constructed to differentiate patients discharged to the community versus to an institution. The four continuous variables were FIM cognition, FIM motor, FIM total, and predicted probability from the multivariable logistic regression model. Area under the curve (AUC) was used to rank the overall discriminatory ability of each continuous measure.10 We used two techniques to identify the cut-point in FIM motor ratings that best differentiated a community discharge from an institutional discharge. The “closest-to-(0,1)” procedure identified the point on the ROC curve that was closest to perfect discrimination. The “Youden Index” procedure identified the point on the ROC curve that was furthest from chance discrimination.10, 11 Lastly, we calculated test diagnostics (sensitivity, specificity, positive predictive value, and negative predictive value) for a series of FIM motor cut-points centered around the one identified in the ROC curve analysis. SPSS v21 software was used for all analyses.
RESULTS
Approximately 68% of the patients were discharged to the community. Table 1 displays patient demographic and clinical characteristics stratified by discharge setting. Compared to those discharged to an institution, patients discharged to the community were younger, more likely to be female, non-white, and married. They also had fewer comorbid conditions, experienced shorter lengths of stay, and demonstrated greater independence in both motor and cognitive functioning at admission and discharge.
Table 1.
Patient demographic, clinical, and functional status characteristics by discharge setting
| D/C Setting |
||||
|---|---|---|---|---|
| Total | Institution | Community | p-value | |
| N | 117,168 | 37,494 | 79,674 | |
| Age, years | 81.4 (7.2) | 83.5 (6.8) | 80.5 (7.2) | <.001 |
| Sex | <.001 | |||
| Female | 72.1% | 71.4% | 72.4% | |
| Male | 27.9% | 28.6% | 27.6% | |
| Race/ethnicity | <.001 | |||
| White | 90.7% | 91.2% | 90.4% | |
| Black | 3.2% | 3.4% | 3.2% | |
| Hispanic | 4.3% | 4.0% | 4.4% | |
| Other | 1.8% | 1.4% | 2.0% | |
| Marital status | <.001 | |||
| Not married | 60.9% | 70.6% | 56.3% | |
| Married | 39.1% | 29.4% | 43.7% | |
| Impairment | *0.061 | |||
| Unilateral fracture | 99.9% | 99.8% | 99.9% | |
| Bilateral fracture | .1% | .2% | .1% | |
| Comorbidity sum | 8.2 (2.3) | 8.5 (2.2) | 8.0 (2.4) | <.001 |
| Duration, days | 5.7 (3.8) | 6.1 (4.2) | 5.5 (3.6) | <.001 |
| Length of stay, days | 13.6 (4.9) | 14.1 (5.3) | 13.4 (4.7) | <.001 |
| FIM cognition: admit | 24.4 (7.1) | 21.9 (7.4) | 25.6 (6.6) | <.001 |
| FIM motor: admit | 35.1 (10.0) | 30.2 (8.9) | 37.4 (9.6) | <.001 |
| FIM total: admit | 59.5 (15.1) | 52.0 (14.2) | 63.0 (14.2) | <.001 |
| FIM cognition: d/c | 27.8 (6.2) | 24.9 (6.8) | 29.1 (5.3) | <.001 |
| FIM motor: d/c | 58.1 (14.7) | 46.4 (13.8) | 63.6 (11.6) | <.001 |
| FIM total: d/c | 85.9 (19.2) | 71.3 (18.4) | 92.7 (15.3) | <.001 |
Values are reported as mean (standard deviation) unless otherwise noted. D/C = discharge. P-values obtained from independent t-tests and chi-square or *Fisher’s exact tests as appropriate.
Areas under the ROC curves for FIM cognition (0.70), FIM motor (0.84), and FIM total (0.83), suggest that the FIM-motor yields the best overall discrimination of patients discharged to the community versus those discharged to an institution following inpatient rehabilitation for hip fracture. The results of logistic regression analysis indicated that age, sex, race, marital status, FIM-cognition and FIM-motor scores at discharge were significant factors associated with discharge destination (Table 2).
Table 2.
Results of backwards stepwise logistic regression model used to calculate the predicted probability of community discharge for each patient.
| OR | 95% CI | |
|---|---|---|
| Age, yrs | 0.98 | (0.98, 0.99) |
| Male | 0.94 | (0.91, 0.97) |
| Minority | 1.86 | (1.76, 1.97) |
| Not married | 0.51 | (0.49, 0.52) |
| Comorbidity sum | 0.99 | (0.98, 1.00) |
| D/C FIM cognition | 0.99 | (0.98, 0.99) |
| D/C FIM motor | 1.11 | (1.11, 1.11) |
Target group is community discharge. Duration to admit, length of stay, and impairment (unilateral vs. bilateral) did not reach statistical significance and were removed from the model.
ROC curves for the discharge FIM motor alone and the multivariable model are displayed in the figure. Areas under the two curves indicate no practical difference in discriminatory ability between discharge FIM motor alone and the full model. The figure also identifies the cut-point in the distribution of FIM motor ratings (58) that best differentiates community discharges from institutional discharges. Both methods (“closest-to-(0,1)” and “Youden index”) yielded the same cutoff value. Table 3 shows test diagnostics across 5-point intervals of FIM motor cut-points and illustrates that the threshold of 58 maximizes the balance between sensitivity (75%) and specificity (77%). For cut-points greater than 58, the reduction in sensitivity is greater than the gain in specificity. Conversely, for values below 58, the reduction in specificity is greater than the gain in sensitivity.
Figure.
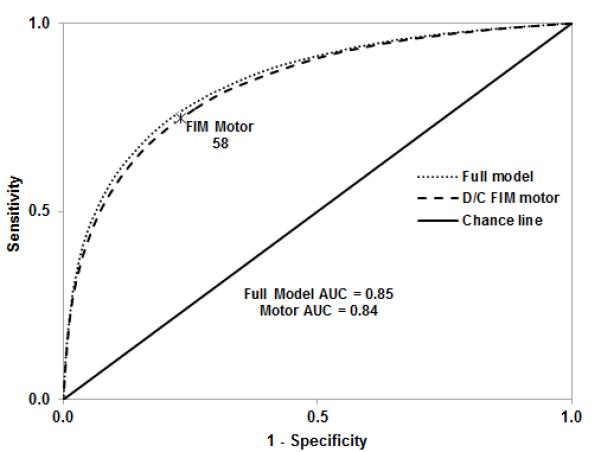
Receiver operating characteristic (ROC) curves for classifying patients who were discharged to the community versus an institution. The full model is based on the distribution of predicted probabilities obtained from the logistic model displayed in Table 2. D/C FIM motor is based on the distribution of discharge FIM motor ratings only. The asterisk (FIM Motor 58) indicates the optimum cut-point based on the minimum distance from perfect discrimination and the maximum vertical distance from the chance line.
Table 3.
Test diagnostics for select FIM motor cutoff values in discriminating a community discharge (target category) from an institutional discharge.
| FIM Motor | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|
| ≥ 48 | 90.9% | 49.6% | 79.3% | 71.9% |
| ≥ 53 | 84.8% | 63.0% | 82.9% | 66.1% |
| ≥ 58 | 74.7% | 77.0% | 87.4% | 58.9% |
| ≥ 63 | 60.1% | 88.2% | 91.6% | 51.0% |
| ≥ 68 | 42.3% | 95.2% | 94.9% | 43.7% |
PPV = positive predictive value. NPV = negative predictive value.
DISCUSSION
This study examined patients with hip fracture in the 100% Medicare inpatient rehabilitation files from 2007-2009. Descriptive summaries indicated that hip fracture rehabilitation patients were primarily older, white, women, who were not married, had experienced unilateral hip fracture, and stayed in rehabilitation for approximately two weeks. Two-thirds of patients were discharged back to the community following inpatient rehabilitation. The key findings can be summarized as follows: FIM motor demonstrates good diagnostic qualities for differentiating patient discharge setting following inpatient rehabilitation for hip fracture, and a discharge FIM motor rating of 58 may be an important threshold for increased likelihood of community discharge.
FIM motor was noticeably more effective than FIM cognition and equally effective as FIM total in discriminating patients discharged to the community from those discharged to an institution after inpatient rehabilitation for hip fracture. Similar findings have been reported in patients with stroke.12 Hip fracture directly affects the motor domain, which leads to a greater distribution in physical independence scores compared to cognitive independence scores. In turn, discharge motor status is more likely than cognitive status to be a decisive factor in return to the community following rehabilitation for patients with hip fracture.
Kristensen7 reported that older age, male sex, and bilateral hip fracture were associated with a higher probability of being discharged to an institution. Our results indicate older age, male sex, white race, not married, higher cognition function, and lower motor function increased the likelihood of being discharged to an institution. We compared the discriminating ability of the discharge FIM motor alone, with a multivariable model that included these six statistically significant variables as well as fracture type and comorbidity sum. The discriminating ability of discharge FIM motor alone (AUC = 0.84) was similar to that of the fully-adjusted model (AUC = 0.85) suggesting that motor function is as effective at differentiating community from institutional discharges as the multivariable model with additional variables that are independently associated with discharge setting.
From a clinical perspective, a diagnostic tool based on a single standard measure is more practical and meaningful than values obtained from a composite model. If confirmed, our findings suggest information from the FIM motor alone may help clinicians to better plan individualized treatment plans designed to return patients with hip fracture to the community. This information may also be beneficial in the multifaceted discharge planning process.
We chose the cut point that best balanced sensitivity and specificity. With no rationale to emphasize either diagnostic criterion, the cut-point that maximizes the overall rate of correct classifications and minimizes the overall rate of misclassifications provides the most useful information.11 Table 3 demonstrates the tradeoffs in group classifications with shifts in the cut-point. Further study is needed to determine the clinical implications of false positives (i.e. classifying someone discharged to an institution as being discharged to the community) compared to false negatives (i.e. classifying someone discharged to the community as being discharged to an institution).
It is interesting to note that 58 is the midpoint between mean ratings of “minimal assistance” (4) and “supervision” (5) across the 13 motor items. Thus, the current findings substantiate the intuition that a person performing at or above the upper limit of the “Modified Dependence” range on individual functional items is more likely to be discharged to the community. While improving a person’s primary functional deficits is an obvious goal of any patient-centered rehabilitation program, our results simply provide a global, quantifiable target that may be useful for developing treatment plans and/or estimating timeframes.
Study Limitations
This study has limitations. It is important to understand that sensitivity and specificity provide information on the diagnostic properties of the instrument only; they do not convey probability for an individual patient to experience an outcome. We did not have access to other variables that may also affect discharge destination; e.g., pre-fracture functional level, surgical procedure type, pain level, muscle strength, and the availability of care (informal or formal) if a person was discharged to the community. The effects of those variables on discharge destination and the discriminating ability of the FIM-motor scale merit further examination. In addition, we do not know if a patient discharged to the community was able to stay in the community once he or she experienced the challenges of living independently with new functional limitations.
This study also has strengths. The sample was obtained from the 100% Medicare inpatient rehabilitation hip fracture population from 2007-2009. To our knowledge, this is the first study using a large national sample to report a cut-off value for the FIM motor to differentiate patients discharged to the community from those discharged to institutions after inpatient rehabilitation for hip fracture.
CONCLUSIONS
Discharge FIM motor demonstrated good discriminatory ability for classifying discharge setting following inpatient rehabilitation for hip fracture. It was more effective than FIM cognition and equally effective as FIM total or a multivariable model that included patient demographic, clinical, and functional status measures. A discharge FIM motor rating of 58 demonstrated the best balance of sensitivity and specificity for classifying community and institutional discharges. Prospective research is needed to evaluate the clinical effectiveness of using a discharge FIM motor value of 58 as a practical tool to guide treatment plans and/or as additional information in discharge planning decisions for patients with hip fracture.
Acknowledgements
The authors wish to thank Fei Du, MS, for her biostatistics consult.
Grant support: This project was funded in part by the National Institutes of Health (NIH): R24 HD065702 – Graham, Karmarkar, Ottenbacher; K01 HD068513 – Reistetter; CTSA 8UL1TR000071 – Karmarkar, Reistetter, Ottenbacher; and the Agency for Health Research & Quality (AHRQ): R24 HS022134 – Graham, Reistetter, Ottenbacher.
Footnotes
Conflict of Interest / Disclosure: The authors report no conflicts of interest. No party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated.
REFERENCES
- 1.Hung WW, Egol KA, Zuckerman JD, Siu AL. Hip fracture management: tailoring care for the older patient. JAMA. 2012;307(20):2185–2194. doi: 10.1001/jama.2012.4842. [DOI] [PubMed] [Google Scholar]
- 2.Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian Journal of Orthopaedics. 2011;45(1):15–22. doi: 10.4103/0019-5413.73656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ottenbacher KJ, Smith PM, Illig SB, Peek MK, Fiedler RC, Granger CV. Hospital readmission of persons with hip fracture following medical rehabilitation. Arch Gerontol Geriatr. 2003;36(1):15–22. doi: 10.1016/s0167-4943(02)00052-3. [DOI] [PubMed] [Google Scholar]
- 5.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clinical Orthopaedics & Related Research. 2011;469(7):1913–1918. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilbert R, Todd C, May M, Yardley L, Ben-Shlomo Y. Socio-demographic factors predict the likelihood of not returning home after hospital admission following a fall. Journal of Public Health. 2010;32(1):117–124. doi: 10.1093/pubmed/fdp077. [DOI] [PubMed] [Google Scholar]
- 7.Kristensen MT. Factors affecting functional prognosis of patients with hip fracture. European journal of physical & rehabilitation medicine. 2011;47(2):257–264. [PubMed] [Google Scholar]
- 8.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the Functional Independence Measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 9.Stineman MG, Shea JA, Jette A, et al. The Functional Independence Measure: tests of scaling assumptions, structure, and reliability across 20 diverse impairment categories. Arch Phys Med Rehabil. 1996;77(11):1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- 10.Akobeng AK. Understanding diagnostic tests 3: Receiver operating characteristic curves. Acta Paediatrica. 2007;96(5):644–647. doi: 10.1111/j.1651-2227.2006.00178.x. [DOI] [PubMed] [Google Scholar]
- 11.Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006;163(7):670–675. doi: 10.1093/aje/kwj063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reistetter TA, Graham JE, Deutsch A, Granger CV, Markello S, Ottenbacher KJ. Utility of functional status for classifying community versus institutional discharges after inpatient rehabilitation for stroke. Arch Phys Med Rehabil. 2010;91(3):345–350. doi: 10.1016/j.apmr.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


