Abstract
Schwann cells (SCs) in the peripheral nerves myelinate axons during postnatal development to allow saltatory conduction of nerve impulses. Well-organized structures of myelin sheathes are maintained throughout life unless nerves are insulted. After peripheral nerve injury, unidentified signals from injured nerves drive SC dedifferentiation into an immature state. Dedifferentiated SCs participate in axonal regeneration by producing neurotrophic factors and removing degenerating nerve debris. In this review, we focus on the role of mitogen activated protein kinase family proteins (MAP kinases) in SC dedifferentiation. In addition, we will highlight neuregulin 1 and the transcription factor c-jun as upstream and downstream signals for MAP kinases in SC responses to nerve injury.
Keywords: Schwann cell, dedifferentiation, plasticity, nerve injury, mitogen activated protein kinase family proteins, c-jun
INTRODUCTION TO SCHWANN CELL DEDIFFERENTIATION AND PLASTICITY
The peripheral nerves consist of sensory nerves that transmit somatic and visceral afferent information to the brain via the spinal cord and motor nerves that convey efferent outputs of the brain to effector organs such as skeletal muscles and glands. The nerve conduction velocities (NCV) of mammalian peripheral nerves range from 10 m/s to 150 m/s, depending on the type of information being transmitted. Mechanistically, two important factors determine the velocity of nerve conduction, axonal diameter and the presence of myelin sheath [1]. For example, the NCV of large myelinated nerves controlling skeletal muscle contraction or transmitting proprioceptive sensory information is far faster than that of unmyelinated or small myelinated nerves that transmit pain signals [1]. Peripheral nerve myelination is achieved by the plasma membrane of Schwann cells (SCs), the sole glial cells of peripheral nerves, wrapping around axons during perinatal and early postnatal development. In fact, the myelin sheath is a notable outcome of the differentiation of SCs [2, 3, 4]. Once the myelin sheath is formed and matured postnatally, the integrity of the myelin sheath is maintained throughout life unless the nerve is physically or chemically damaged. For sustaining the structure and function of the myelin sheath during adulthood, SCs need to express continuously high levels of myelin proteins such as myelin protein zero (MPZ) and myelin basic protein (MBP) in adulthood [5].
When exposed to harmful situations such as nerve injury, SCs stop expressing myelin genes and begin to actively degrade and remove their myelin sheath [6]. Unidentified signals from damaged axons or physicochemical insults to the myelin sheath induce these SC responses [6]. The demyelinating action of SCs following nerve damage is accompanied by cellular dedifferentiation, which generally refers to a process by which fully differentiated cells revert to an immature phenotype [4, 6, 7]. In dedifferentiated states, SCs express proteins such as p75 neurotrophin receptor (p75), glial fibrillary acidic protein and neuronal cell adhesion molecule, which are found in immature SCs but not in adult myelinating SCs [6, 8]. In addition, dedifferentiated SCs proliferate in response to nerve injury [9, 10, 11]. Although these are features of immature SCs, dedifferentiated SCs exhibit several unique features that are not observed in immature SCs. For example, dedifferentiated SCs express macrophage-2 antigens [12] and produce enormous amounts of lysosomes, which correlate with the increased phagocytic activity of SCs [13, 14, 15]. Dedifferentiated SCs also produce a large number of cytokines that regulate chemotaxis and infiltration of blood monocytes into lesion sites [16, 17, 18]. Furthermore, these injury-induced SC responses include the induction of several growth factors for axonal regeneration and neuronal survival [19, 20]. Therefore, the overall responses of SCs following nerve injury represent a sophisticated SC plasticity that cannot simply be described as dedifferentiation (Fig. 1).
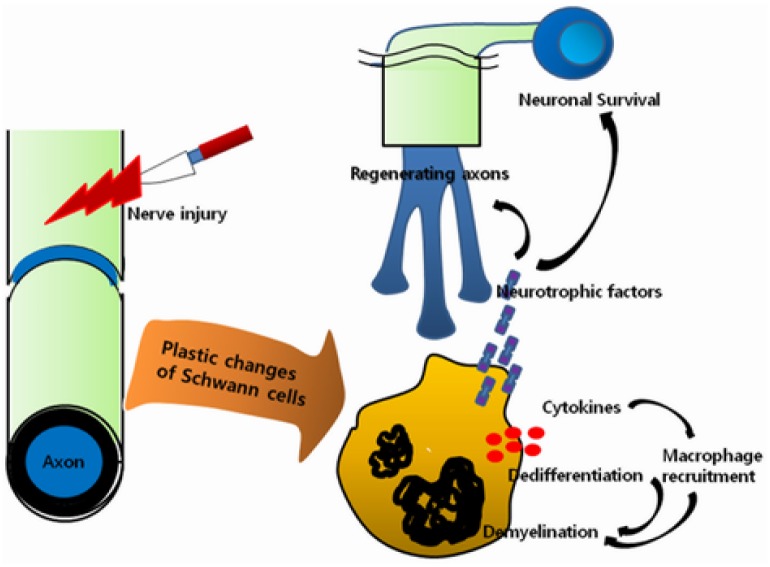
Fig. 1.
Plastic changes of SCs following nerve injury. The figure depicts multiple aspects of SC plasticity following a physical damage to nerves. SC dedifferentiation refers to phenotype changes of mature SCs into an immature state. However, dedifferentiated SCs in injured nerves exhibit several unique features that are not observed in immature SCs, those are secretion of neurotrophic factors and cytokines and activation of lysosomal demyelination system. Expression of neurotrophic factors is essential for the survival of injured neurons and axonal regeneration, whereas cytokine expression is implicated in the chemotactic infiltration of monocytes into a lesion site.
Given the critical role of these plastic changes in SCs in myelin removal and axonal regeneration after nerve injury, studies on the molecular mechanisms on SC plasticity will shed light on the mechanisms of nerve repair and aid in the development of therapeutic strategies for axonal regeneration. As dedifferentiated SCs exhibit shutdown of myelin gene expression, induction of immature SC markers, activation of myelin degrading systems, cellular proliferation and expression of neurotrophic factors, SC plasticity must be regulated by complex molecular mechanisms. A growing body of recent researches has shown that mitogen activated protein kinase family proteins (MAP kinases) are important regulators for SC plastic changes. Interestingly, extracellular signal regulated kinase (ERK), c-jun N-terminal kinase (JNK) and p38 MAP kinase are all activated in SCs following nerve injury and play a specific or overlapping role in SC dedifferentiation [21, 22, 23, 24, 25]. In this review, we focus on the role of these three MAP kinases in SC plasticity. In addition, our discussion will be centered on neuregulin 1 (NRG1) and the transcription factor c-jun as upstream and downstream signals for MAP kinases in SC plasticity.
THE RAF/ERK PATHWAY IN SCHWANN CELL PLASTICITY
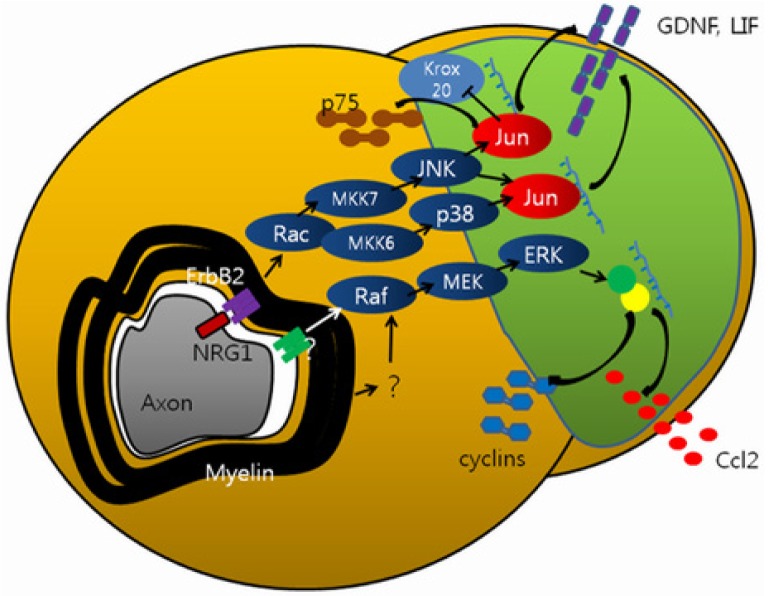
The potential role of the Raf-ERK pathway in SC dedifferentiation was first reported by Harrisingh et al. [25]. To determine the role of the Raf-ERK pathway, the researchers employed SCs overexpressing Raf kinase. In cultured SCs, increased intracellular cAMP levels induced the differentiation of SCs, as demonstrated by the expression of several myelin genes including krox20, MPZ and MBP [26]. Conversely, over-expression of Raf kinase suppressed cAMP-induced SC differentiation [25]. A recent study reported the effect of overexpression of tamoxifen-inducible Raf kinase in SCs in vivo [27]. The forced activation of the Raf-ERK pathway in SCs for 3 days by tamoxifen treatment of these genetically modified mice led SCs to express several dedifferentiation markers, such as p75, and to downregulate myelin gene expression, even in the absence of nerve injury. Importantly, longer treatment with tamoxifen induced demyelination with infiltration of macrophages and SC mitosis in uninjured naïve nerves [27]. In consistency with the importance of the Raf-ERK pathway in SC dedifferentiation, high levels of ERK activation in injured nerves are maintained for a long time in vivo [21, 25], and the inhibition of the ERK pathway with specific inhibitors suppressed SC mitosis, cytokine expression and demyelination [27]. On the other hand, the inhibition of the ERK pathway did not significantly prevent the induction of p75, a marker of SC dedifferentiation, and the shutdown of myelin gene expression [27]. Therefore, it seems that the Raf-ERK pathway participates in SC plasticity in a selective manner. This idea has been supported by Shin et al. who revealed that the inhibition of the ERK pathway suppressed the expression of cell cycle proteins and cytokines but did not affect the induction of SC dedifferentiation markers including p75 and neurotrophic factors such as glia cell-derived neurotrophic factor (GDNF) [28] (Fig. 2). Therefore, these findings support the idea that different aspects of SC plasticity are controlled by multiple independent mechanisms. In line with this hypothesis, SC mitosis is known to be independently regulated by SC dedifferentiation in cultured SCs [29].
Fig. 2.
MAP kinase signaling in SC plasticity. NRG1-ErbB2 signaling regulates SC plasticity via c-jun expression which is mediated by JNK and p38 kinase pathways. c-jun increases the expression of GDNF and LIF but suppresses the crucial transcription factor for myelination, Krox20, thereby inducing SC dedifferentiation. The Raf-ERK pathway is involved in the expression of cell cycle proteins and chemotactic factors such as Ccl2.
Previously, Parkinson et al proposed a hypothesis called the 'reciprocal c-jun/krox20 regulation' hypothesis of SC dedifferentiation, that is, c-jun induction suppresses krox20 expression, whereas krox20 overexpression antagonizes c-jun expression in cultured SCs [23, 30]. The essential role of c-jun induction in SC plasticity was demonstrated by delayed demyelination in SC-specific conditional c-jun knockout mice following nerve injury [23]. Because AP-1 proteins such as c-jun are important mediators of ERK-induced cell proliferation and cytokine expression in a variety of cells [31, 32, 33, 34, 35], c-jun expression may be an underlying mechanism of ERK-induced SC dedifferentiation. In a SC-dorsal root ganglion (DRG) neuron co-culture model, demyelination and dedifferentiation of myelinating SC can be triggered by NRG1 treatment [25, 36]. Inhibition of the ERK pathway suppressed both demyelination and c-jun expression induced by NRG1 in co-culture [37]. In contrast to these findings, in cultured primary SC and explant cultures, the induction of c-jun was prevented by JNK inhibition but not by ERK inhibition [28, 29]. It should also be noted that injury-induced SC mitosis and cytokine expression (ERK-dependent processes) were not suppressed in SC-specific c-jun conditional knock mice [19]. Thus, the role of the ERK pathway in injury-induced c-jun expression in vivo has not yet been determined. ERK could affect cell proliferation by regulating cell cycle regulating proteins through Forkhead fox [38, 39] and ETS domain-containing protein-1 [40, 41]. Further studies on the regulation of these proteins in SCs would provide important insights into ERK-mediated SC plasticity.
THE RAC/JNK PATHWAY AND C-JUN IN SCHWANN CELL PLASTICITY
JNK plays diverse roles in cultured SC, including regulating mitosis and migration [29, 42]. However, the role of JNK in SC plasticity in injured nerves was first proposed by Parkinson et al. who showed that the forceful activation of a protein upstream of JNK, MAP kinase kinase (MKK) 7, induces c-jun expression and concurrently downregulates myelin gene expression in cultured SCs [23]. JNK-mediated induction of c-jun has recently been demonstrated in dedifferentiating SCs deprived of cAMP [29]. In consistency with this finding, it was reported that JNK but not ERK is upstream of c-jun using sciatic nerve explant cultures, an ex vivo model of SC dedifferentiation [28]. In addition, they showed MKK7 activation in the injured nerves, further suggesting a role of the MKK7-JNK-cjun pathway in SC dedifferentiation in vivo (Fig. 2).
It has been recently reported that the induction of neurotrophic factors such as GDNF in dedifferentiated SCs is essential for neuronal survival and peripheral nerve regeneration [20]. The Jessen and Mirsky group referred to this critical function of SCs in axonal regeneration as "SC transdifferentiation into a repair cell"[19]. This SC change appears to be principally driven by c-jun because SCs lacking c-jun failed to induce the expression of neurotrophic factors including GDNF, artemin and brain derived neurotrophic factor, thereby resulting in neuronal cell death in DRGs following nerve injury [20]. Therefore, the MKK7-JNK-c-jun pathway in SCs might regulate axonal regeneration by providing a favorable milieu for neuronal survival and axonal regrowth. The role of the Raf-ERK pathway in changing SCs into repair cells (and in axonal regeneration) has not been extensively examined, but such a role seems unlikely because inhibition of the ERK pathway did not significantly reduce the induction of neurotrophic factors such as GDNF in SCs in an explant culture model [28].
Small RhoGTPases regulate many signaling pathways, including MAP kinases, in a variety of cells [43]. Previously, the Rac-JNK pathway has been implicated in SC transformation into tumor cells [44]. Jung et al. recently reported that Rac, but not cdc42, was activated in SCs of injured nerves [45], and it has been revealed that Rac contributed to both demyelination and c-jun induction [28, 45, 46]. Furthermore, microarray experiments showed that many Rac-dependent genes overlapped with c-jun-dependent genes in dedifferentiated SCs [19, 28]. For example, injury-induced induction of p75 and neurotrophic factors such as GDNF in SCs was dependent on Rac and c-jun, suggesting a role for the Rac-c-jun pathway in the control of SC plasticity (Fig. 2). Interestingly, Rac was not found to be upstream of the ERK pathway, and consistent with this finding, most ERK-dependent genes in dedifferentiating SCs were not dependent on Rac [28]. These data indicate differential regulation and distinct roles of the Rac-c-jun and Raf-ERK pathways in SC plasticity (Fig. 2).
P38 MAP KINASE IN SCHWANN CELL DEDIFFERENTIATION
P38 MAP kinase was rapidly activated in the distal part of injured nerves, and the inhibition of p38 MAP kinase suppressed the induction of several genes, including the cytokine leukemia inhibitory factor (LIF), in nerve explants [24, 47]. Interestingly, LIF expressed by SCs is known to play a role in regenerative axon growth of injured DRG neurons [48]. Therefore, p38 MAP kinase may be involved in the transformation of SCs into repair cells through c-jun induction. It has recently been reported that the inhibition of p38 MAP kinase suppressed injury-induced sciatic nerve demyelination in a co-culture model and in vivo [49]. Furthermore, the transfection of active MKK6, an upstream of p38 MAP kinase, into SCs prevented cAMP-induced SC differentiation and induced c-jun expression [49]. These findings suggest that there may be cross-talk between the p38 MAP kinase and Rac-JNK pathways associated with c-jun induction in SC plasticity (Fig. 2).
NRG MAY BE AN UPSTREAM OF MAP KINASE ACTIVATION IN SCHWANN CELL PLASTICITY
Given the ability of three MAP kinases to regulate SC plasticity independently or cooperatively, factors upstream of these MAP kinases might initiate SC responses to nerve injury. The glial growth factor NRG1, which is expressed at the axonal surface, is critical for SC precursor generation and myelination during peripheral nerve development [1, 2, 50]. Paradoxically, there is increasing evidence that NRG1 participates in SC responses to nerve injury during adulthood [36, 51]. Consistent with the demyelinating function of NRG1 in a SC-DRG co-culture model, activation of ErbB2, the receptor for NRG1, occurs within a minute of nerve injury in SCs. In addition, inhibition of ErbB2 with specific inhibitors suppressed demyelination in vivo and in ex vivo sciatic nerve explant cultures [28, 52]. Thus, it is likely that the different roles of NRG1 in SC physiology are related to the state of SC differentiation.
In SC-DRG co-cultures, NRG1 induces the activation of three MAP kinases and c-jun expression, and the inhibition of each MAP kinase prevented NRG1-induced demyelination [25, 49]. However, Shin et al recently suggested that NRG1-ErbB2 signaling is specific to the Rac-JNK pathway in dedifferentiating SCs [28]. They found significant reduction in the activation of the Rac-c-jun pathway (Fig. 2), but not ERK activation, when they inhibited ErbB2 using a specific inhibitor in nerve explant cultures, indicating that NRG1 contributes to SCs changes into repair cells through the activation of the Rac-JNK pathway. In agreement with this, mice lacking axonal NRG1 showed a delayed axonal regeneration following crush injury [53] but injury-induced SC proliferation was not altered in ErbB2 null mice [54]. In addition, exogenous NRG1 clearly promoted regeneration following nerve injury [55]. The mechanism by which NRG1 enhanced the repair of injured nerves may be related to its actions on SC plasticity.
On the other hand, multiple other factors may participate in MAP kinase activation in injured nerves. Calcium entry into SCs or lipid metabolites generated during demyelination could trigger MAP kinase activation [56, 57, 58]. In particular, phosphatidic acids, which are known to activate MAP kinases in a variety of experimental conditions [59], could induce demyelination through ERK activation [60]. The importance of phosphatidic acids in c-jun induction and SC plasticity following nerve injury remains to be determined.
CONCLUSIONS AND FUTURE PERSPECTIVES
In this review, we described the role of MAP kinase activation in SC responses to nerve injury, and associated signaling mechanisms. The molecular mechanisms of SC plasticity provide important mechanistic insights into peripheral neuropathies as well as peripheral nerve regeneration. Many demyelinating neuropathies are associated with SC dedifferentiation [6, 61], and the NRG-ERK pathway has been suggested to be involved in Leprotic demyelination [62]. Further studies are required to determine how each MAP kinase contributes to the diverse phenotypic changes in SCs following nerve injury and in neuropathies.
ACKNOWLEDGEMENTS
This research was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP) (2013041811).
References
- 1.Sherman DL, Brophy PJ. Mechanisms of axon ensheathment and myelin growth. Nat Rev Neurosci. 2005;6:683–690. doi: 10.1038/nrn1743. [DOI] [PubMed] [Google Scholar]
- 2.Taveggia C, Feltri ML, Wrabetz L. Signals to promote myelin formation and repair. Nat Rev Neurol. 2010;6:276–287. doi: 10.1038/nrneurol.2010.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jessen KR, Mirsky R. The origin and development of glial cells in peripheral nerves. Nat Rev Neurosci. 2005;6:671–682. doi: 10.1038/nrn1746. [DOI] [PubMed] [Google Scholar]
- 4.Mirsky R, Woodhoo A, Parkinson DB, Arthur-Farraj P, Bhaskaran A, Jessen KR. Novel signals controlling embryonic Schwann cell development, myelination and dedifferentiation. J Peripher Nerv Syst. 2008;13:122–135. doi: 10.1111/j.1529-8027.2008.00168.x. [DOI] [PubMed] [Google Scholar]
- 5.Decker L, Desmarquet-Trin-Dinh C, Taillebourg E, Ghislain J, Vallat JM, Charnay P. Peripheral myelin maintenance is a dynamic process requiring constant Krox20 expression. J Neurosci. 2006;26:9771–9779. doi: 10.1523/JNEUROSCI.0716-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jessen KR, Mirsky R. Negative regulation of myelination: relevance for development, injury and demyelinating disease. Glia. 2008;56:1552–1565. doi: 10.1002/glia.20761. [DOI] [PubMed] [Google Scholar]
- 7.Jopling C, Boue S, Izpisua Belmonte JC. Dedifferentiation, transdifferentiation and reprogramming: three routes to regeneration. Nat Rev Mol Cell Biol. 2011;12:79–89. doi: 10.1038/nrm3043. [DOI] [PubMed] [Google Scholar]
- 8.Lee HK, Shin YK, Jung J, Seo SY, Baek SY, Park HT. Proteasome inhibition suppresses Schwann cell dedifferentiation in vitro and in vivo. Glia. 2009;57:1825–1834. doi: 10.1002/glia.20894. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez-Valle C, Bunge RP, Bunge MB. Schwann cells degrade myelin and proliferate in the absence of macrophages: evidence from in vitro studies of Wallerian degeneration. J Neurocytol. 1995;24:667–679. doi: 10.1007/BF01179817. [DOI] [PubMed] [Google Scholar]
- 10.Kim HA, Pomeroy SL, Whoriskey W, Pawlitzky I, Benowitz LI, Sicinski P, Stiles CD, Roberts TM. A developmentally regulated switch directs regenerative growth of Schwann cells through cyclin D1. Neuron. 2000;26:405–416. doi: 10.1016/s0896-6273(00)81173-3. [DOI] [PubMed] [Google Scholar]
- 11.Yang DP, Zhang DP, Mak KS, Bonder DE, Pomeroy SL, Kim HA. Schwann cell proliferation during Wallerian degeneration is not necessary for regeneration and remyelination of the peripheral nerves: axon-dependent removal of newly generated Schwann cells by apoptosis. Mol Cell Neurosci. 2008;38:80–88. doi: 10.1016/j.mcn.2008.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reichert F, Saada A, Rotshenker S. Peripheral nerve injury induces Schwann cells to express two macrophage phenotypes: phagocytosis and the galactose-specific lectin MAC-2. J Neurosci. 1994;14:3231–3245. doi: 10.1523/JNEUROSCI.14-05-03231.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holtzman E, Novikoff AB. Lysomes in the rat sciatic nerve following crush. J Cell Biol. 1965;27:651–669. doi: 10.1083/jcb.27.3.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jung J, Cai W, Jang SY, Shin YK, Suh DJ, Kim JK, Park HT. Transient lysosomal activation is essential for p75 nerve growth factor receptor expression in myelinated Schwann cells during Wallerian degeneration. Anat Cell Biol. 2011;44:41–49. doi: 10.5115/acb.2011.44.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venezie RD, Toews AD, Morell P. Macrophage recruitment in different models of nerve injury: lysozyme as a marker for active phagocytosis. J Neurosci Res. 1995;40:99–107. doi: 10.1002/jnr.490400111. [DOI] [PubMed] [Google Scholar]
- 16.Martini R, Fischer S, López-Vales R, David S. Interactions between Schwann cells and macrophages in injury and inherited demyelinating disease. Glia. 2008;56:1566–1577. doi: 10.1002/glia.20766. [DOI] [PubMed] [Google Scholar]
- 17.Tofaris GK, Patterson PH, Jessen KR, Mirsky R. Denervated Schwann cells attract macrophages by secretion of leukemia inhibitory factor (LIF) and monocyte chemoattractant protein-1 in a process regulated by interleukin-6 and LIF. J Neurosci. 2002;22:6696–6703. doi: 10.1523/JNEUROSCI.22-15-06696.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jang SY, Shin YK, Lee HY, Park JY, Suh DJ, Kim JK, Bae YS, Park HT. Local production of serum amyloid a is implicated in the induction of macrophage chemoattractants in Schwann cells during wallerian degeneration of peripheral nerves. Glia. 2012;60:1619–1628. doi: 10.1002/glia.22382. [DOI] [PubMed] [Google Scholar]
- 19.Arthur-Farraj PJ, Latouche M, Wilton DK, Quintes S, Chabrol E, Banerjee A, Woodhoo A, Jenkins B, Rahman M, Turmaine M, Wicher GK, Mitter R, Greensmith L, Behrens A, Raivich G, Mirsky R, Jessen KR. c-Jun reprograms Schwann cells of injured nerves to generate a repair cell essential for regeneration. Neuron. 2012;75:633–647. doi: 10.1016/j.neuron.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fontana X, Hristova M, Da Costa C, Patodia S, Thei L, Makwana M, Spencer-Dene B, Latouche M, Mirsky R, Jessen KR, Klein R, Raivich G, Behrens A. c-Jun in Schwann cells promotes axonal regeneration and motoneuron survival via paracrine signaling. J Cell Biol. 2012;198:127–141. doi: 10.1083/jcb.201205025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheu JY, Kulhanek DJ, Eckenstein FP. Differential patterns of ERK and STAT3 phosphorylation after sciatic nerve transection in the rat. Exp Neurol. 2000;166:392–402. doi: 10.1006/exnr.2000.7508. [DOI] [PubMed] [Google Scholar]
- 22.Agthong S, Kaewsema A, Tanomsridejchai N, Chentanez V. Activation of MAPK ERK in peripheral nerve after injury. BMC Neurosci. 2006;7:45. doi: 10.1186/1471-2202-7-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parkinson DB, Bhaskaran A, Arthur-Farraj P, Noon LA, Woodhoo A, Lloyd AC, Feltri ML, Wrabetz L, Behrens A, Mirsky R, Jessen KR. c-Jun is a negative regulator of myelination. J Cell Biol. 2008;181:625–637. doi: 10.1083/jcb.200803013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zrouri H, Le Goascogne C, Li WW, Pierre M, Courtin F. The role of MAP kinases in rapid gene induction after lesioning of the rat sciatic nerve. Eur J Neurosci. 2004;20:1811–1818. doi: 10.1111/j.1460-9568.2004.03641.x. [DOI] [PubMed] [Google Scholar]
- 25.Harrisingh MC, Perez-Nadales E, Parkinson DB, Malcolm DS, Mudge AW, Lloyd AC. The Ras/Raf/ERK signalling pathway drives Schwann cell dedifferentiation. EMBO J. 2004;23:3061–3071. doi: 10.1038/sj.emboj.7600309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morgan L, Jessen KR, Mirsky R. The effects of cAMP on differentiation of cultured Schwann cells: progression from an early phenotype (04+) to a myelin phenotype (P0+, GFAP-, N-CAM-, NGF-receptor-) depends on growth inhibition. J Cell Biol. 1991;112:457–467. doi: 10.1083/jcb.112.3.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Napoli I, Noon LA, Ribeiro S, Kerai AP, Parrinello S, Rosenberg LH, Collins MJ, Harrisingh MC, White IJ, Woodhoo A, Lloyd AC. A central role for the ERK-signaling pathway in controlling Schwann cell plasticity and peripheral nerve regeneration in vivo. Neuron. 2012;73:729–742. doi: 10.1016/j.neuron.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 28.Shin YK, Jang SY, Park JY, Park SY, Lee HJ, Suh DJ, Park HT. The Neuregulin-Rac-MKK7 pathway regulates antagonistic c-jun/Krox20 expression in Schwann cell dedifferentiation. Glia. 2013;61:892–904. doi: 10.1002/glia.22482. [DOI] [PubMed] [Google Scholar]
- 29.Monje PV, Soto J, Bacallao K, Wood PM. Schwann cell dedifferentiation is independent of mitogenic signaling and uncoupled to proliferation: role of cAMP and JNK in the maintenance of the differentiated state. J Biol Chem. 2010;285:31024–31036. doi: 10.1074/jbc.M110.116970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parkinson DB, Bhaskaran A, Droggiti A, Dickinson S, D'Antonio M, Mirsky R, Jessen KR. Krox-20 inhibits Jun-NH2-terminal kinase/c-Jun to control Schwann cell proliferation and death. J Cell Biol. 2004;164:385–394. doi: 10.1083/jcb.200307132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kurosawa M, Numazawa S, Tani Y, Yoshida T. ERK signaling mediates the induction of inflammatory cytokines by bufalin in human monocytic cells. Am J Physiol Cell Physiol. 2000;278:C500–C508. doi: 10.1152/ajpcell.2000.278.3.C500. [DOI] [PubMed] [Google Scholar]
- 32.Jalali S, Li YS, Sotoudeh M, Yuan S, Li S, Chien S, Shyy JY. Shear stress activates p60src-Ras-MAPK signaling pathways in vascular endothelial cells. Arterioscler Thromb Vasc Biol. 1998;18:227–234. doi: 10.1161/01.atv.18.2.227. [DOI] [PubMed] [Google Scholar]
- 33.Kim JM, Jung HY, Lee JY, Youn J, Lee CH, Kim KH. Mitogen-activated protein kinase and activator protein-1 dependent signals are essential for Bacteroides fragilis enterotoxin-induced enteritis. Eur J Immunol. 2005;35:2648–2657. doi: 10.1002/eji.200526321. [DOI] [PubMed] [Google Scholar]
- 34.Alblas J, Slager-Davidov R, Steenbergh PH, Sussenbach JS, van der Burg B. The role of MAP kinase in TPA-mediated cell cycle arrest of human breast cancer cells. Oncogene. 1998;16:131–139. doi: 10.1038/sj.onc.1201485. [DOI] [PubMed] [Google Scholar]
- 35.Lee JH, Johnson PR, Roth M, Hunt NH, Black JL. ERK activation and mitogenesis in human airway smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2001;280:L1019–L1029. doi: 10.1152/ajplung.2001.280.5.L1019. [DOI] [PubMed] [Google Scholar]
- 36.Zanazzi G, Einheber S, Westreich R, Hannocks MJ, Bedell-Hogan D, Marchionni MA, Salzer JL. Glial growth factor/neuregulin inhibits Schwann cell myelination and induces demyelination. J Cell Biol. 2001;152:1289–1299. doi: 10.1083/jcb.152.6.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Syed N, Reddy K, Yang DP, Taveggia C, Salzer JL, Maurel P, Kim HA. Soluble neuregulin-1 has bifunctional, concentration-dependent effects on Schwann cell myelination. J Neurosci. 2010;30:6122–6131. doi: 10.1523/JNEUROSCI.1681-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Calvisi DF, Pinna F, Ladu S, Pellegrino R, Simile MM, Frau M, De Miglio MR, Tomasi ML, Sanna V, Muroni MR, Feo F, Pascale RM. Forkhead box M1B is a determinant of rat susceptibility to hepatocarcinogenesis and sustains ERK activity in human HCC. Gut. 2009;58:679–687. doi: 10.1136/gut.2008.152652. [DOI] [PubMed] [Google Scholar]
- 39.Asada S, Daitoku H, Matsuzaki H, Saito T, Sudo T, Mukai H, Iwashita S, Kako K, Kishi T, Kasuya Y, Fukamizu A. Mitogen-activated protein kinases, Erk and p38, phosphorylate and regulate Foxo1. Cell Signal. 2007;19:519–527. doi: 10.1016/j.cellsig.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 40.Apáti A, Jánossy J, Brózik A, Bauer PI, Magócsi M. Calcium induces cell survival and proliferation through the activation of the MAPK pathway in a human hormone-dependent leukemia cell line, TF-1. J Biol Chem. 2003;278:9235–9243. doi: 10.1074/jbc.m205528200. [DOI] [PubMed] [Google Scholar]
- 41.Smith ER, Smedberg JL, Rula ME, Xu XX. Regulation of Ras-MAPK pathway mitogenic activity by restricting nuclear entry of activated MAPK in endoderm differentiation of embryonic carcinoma and stem cells. J Cell Biol. 2004;164:689–699. doi: 10.1083/jcb.200312028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamauchi J, Chan JR, Shooter EM. Neurotrophin 3 activation of TrkC induces Schwann cell migration through the c-Jun N-terminal kinase pathway. Proc Natl Acad Sci U S A. 2003;100:14421–14426. doi: 10.1073/pnas.2336152100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shirai H, Autieri M, Eguchi S. Small GTP-binding proteins and mitogen-activated protein kinases as promising therapeutic targets of vascular remodeling. Curr Opin Nephrol Hypertens. 2007;16:111–115. doi: 10.1097/MNH.0b013e3280148e4f. [DOI] [PubMed] [Google Scholar]
- 44.Kaempchen K, Mielke K, Utermark T, Langmesser S, Hanemann CO. Upregulation of the Rac1/JNK signaling pathway in primary human schwannoma cells. Hum Mol Genet. 2003;12:1211–1221. doi: 10.1093/hmg/ddg146. [DOI] [PubMed] [Google Scholar]
- 45.Jung J, Cai W, Lee HK, Pellegatta M, Shin YK, Jang SY, Suh DJ, Wrabetz L, Feltri ML, Park HT. Actin polymerization is essential for myelin sheath fragmentation during Wallerian degeneration. J Neurosci. 2011;31:2009–2015. doi: 10.1523/JNEUROSCI.4537-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Park HT, Feltri ML. Rac1 GTPase controls myelination and demyelination. Bioarchitecture. 2011;1:110–113. doi: 10.4161/bioa.1.3.16985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Myers RR, Sekiguchi Y, Kikuchi S, Scott B, Medicherla S, Protter A, Campana WM. Inhibition of p38 MAP kinase activity enhances axonal regeneration. Exp Neurol. 2003;184:606–614. doi: 10.1016/S0014-4886(03)00297-8. [DOI] [PubMed] [Google Scholar]
- 48.Teng FY, Tang BL. Axonal regeneration in adult CNS neurons-signaling molecules and pathways. J Neurochem. 2006;96:1501–1508. doi: 10.1111/j.1471-4159.2006.03663.x. [DOI] [PubMed] [Google Scholar]
- 49.Yang DP, Kim J, Syed N, Tung YJ, Bhaskaran A, Mindos T, Mirsky R, Jessen KR, Maurel P, Parkinson DB, Kim HA. p38 MAPK activation promotes denervated Schwann cell phenotype and functions as a negative regulator of Schwann cell differentiation and myelination. J Neurosci. 2012;32:7158–7168. doi: 10.1523/JNEUROSCI.5812-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Michailov GV, Sereda MW, Brinkmann BG, Fischer TM, Haug B, Birchmeier C, Role L, Lai C, Schwab MH, Nave KA. Axonal neuregulin-1 regulates myelin sheath thickness. Science. 2004;304:700–703. doi: 10.1126/science.1095862. [DOI] [PubMed] [Google Scholar]
- 51.Fricker FR, Bennett DL. The role of neuregulin-1 in the response to nerve injury. Future Neurol. 2011;6:809–822. doi: 10.2217/fnl.11.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guertin AD, Zhang DP, Mak KS, Alberta JA, Kim HA. Microanatomy of axon/glial signaling during Wallerian degeneration. J Neurosci. 2005;25:3478–3487. doi: 10.1523/JNEUROSCI.3766-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fricker FR, Lago N, Balarajah S, Tsantoulas C, Tanna S, Zhu N, Fageiry SK, Jenkins M, Garratt AN, Birchmeier C, Bennett DL. Axonally derived neuregulin-1 is required for remyelination and regeneration after nerve injury in adulthood. J Neurosci. 2011;31:3225–3233. doi: 10.1523/JNEUROSCI.2568-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Atanasoski S, Scherer SS, Sirkowski E, Leone D, Garratt AN, Birchmeier C, Suter U. ErbB2 signaling in Schwann cells is mostly dispensable for maintenance of myelinated peripheral nerves and proliferation of adult Schwann cells after injury. J Neurosci. 2006;26:2124–2131. doi: 10.1523/JNEUROSCI.4594-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen LE, Liu K, Seaber AV, Katragadda S, Kirk C, Urbaniak JR. Recombinant human glial growth factor 2 (rhGGF2) improves functional recovery of crushed peripheral nerve (a double-blind study) Neurochem Int. 1998;33:341–351. doi: 10.1016/s0197-0186(98)00037-0. [DOI] [PubMed] [Google Scholar]
- 56.Griffin JW, Stocks EA, Fahnestock K, Van Praagh A, Trapp BD. Schwann cell proliferation following lysolecithin-induced demyelination. J Neurocytol. 1990;19:367–384. doi: 10.1007/BF01188405. [DOI] [PubMed] [Google Scholar]
- 57.Fex Svenningsen A, Kanje M. Regulation of Schwann cell proliferation in cultured segments of the adult rat sciatic nerve. J Neurosci Res. 1998;52:530–537. doi: 10.1002/(SICI)1097-4547(19980601)52:5<530::AID-JNR5>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 58.Meador-Woodruff JH, Lewis BL, DeVries GH. Cyclic AMP and calcium as potential mediators of stimulation of cultured Schwann cell proliferation by axolemma-enriched and myelin-enriched membrane fractions. Biochem Biophys Res Commun. 1984;122:373–380. doi: 10.1016/0006-291x(84)90485-6. [DOI] [PubMed] [Google Scholar]
- 59.Kraft CA, Garrido JL, Fluharty E, Leiva-Vega L, Romero G. Role of phosphatidic acid in the coupling of the ERK cascade. J Biol Chem. 2008;283:36636–36645. doi: 10.1074/jbc.M804633200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nadra K, de Preux Charles AS, Médard JJ, Hendriks WT, Han GS, Grès S, Carman GM, Saulnier-Blache JS, Verheijen MH, Chrast R. Phosphatidic acid mediates demyelination in Lpin1 mutant mice. Genes Dev. 2008;22:1647–1661. doi: 10.1101/gad.1638008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hutton EJ, Carty L, Laurá M, Houlden H, Lunn MP, Brandner S, Mirsky R, Jessen K, Reilly MM. c-Jun expression in human neuropathies: a pilot study. J Peripher Nerv Syst. 2011;16:295–303. doi: 10.1111/j.1529-8027.2011.00360.x. [DOI] [PubMed] [Google Scholar]
- 62.Tapinos N, Ohnishi M, Rambukkana A. ErbB2 receptor tyrosine kinase signaling mediates early demyelination induced by leprosy bacilli. Nat Med. 2006;12:961–966. doi: 10.1038/nm1433. [DOI] [PubMed] [Google Scholar]