Abstract
Currently, pharmaceutical preparations are serious contributors to liver disease; hepatotoxicity ranking as the most frequent cause for acute liver failure and post-commercialization regulatory decisions. The diagnosis of hepatotoxicity remains a difficult task because of the lack of reliable markers for use in general clinical practice. To incriminate any given drug in an episode of liver dysfunction is a step-by-step process that requires a high degree of suspicion, compatible chronology, awareness of the drug’s hepatotoxic potential, the exclusion of alternative causes of liver damage and the ability to detect the presence of subtle data that favors a toxic etiology. This process is time-consuming and the final result is frequently inaccurate. Diagnostic algorithms may add consistency to the diagnostic process by translating the suspicion into a quantitative score. Such scales are useful since they provide a framework that emphasizes the features that merit attention in cases of suspected hepatic adverse reaction as well. Current efforts in collecting bona fide cases of drug-induced hepatotoxicity will make refinements of existing scales feasible. It is now relatively easy to accommodate relevant data within the scoring system and to delete low-impact items. Efforts should also be directed toward the development of an abridged instrument for use in evaluating suspected drug-induced hepatotoxicity at the very beginning of the diagnosis and treatment process when clinical decisions need to be made. The instrument chosen would enable a confident diagnosis to be made on admission of the patient and treatment to be fine-tuned as further information is collected.
Keywords: Drug-induced hepatotoxicity, Causality assessment, Diagnostic algorithms, Clinical scales
INTRODUCTION
Idiosyncratic liver disease caused by drugs or toxins is a major challenge of modern hepatology, and is a somewhat neglected field as well. The reasons for this are varied. Firstly, hepatotoxicity is rarely encountered in standard clinical practice because of its relatively low incidence compared to other hepatic diseases and the difficulties in confidently diagnosing the condition. Secondly, there have not been substantial advances in recent decades in the understanding of its pathogenesis, which is mostly due to the lack of validated animal models for investigating idiosyncratic hepatotoxicity. As such, susceptibility factors that can predispose individuals to adverse hepatic reactions to drugs have not been conclusively identified, nor has there been any development of reliable and standardized markers for the identification and measurement of toxic liver damage[1]. Co-operative efforts are being encouraged so as to prospectively collect bona fide cases from which quality data and biological samples could be obtained for genome-wide studies[2,3].
Hepatotoxicity has a considerable impact on health because many of the hepatic reactions induced by pharmaceutical preparations can be very severe. A survey from the Acute Liver Failure Study Group (ALFSG) of the patients admitted in 17 US hospitals showed that prescribed drugs (including acetaminophen) accounted for > 50% of cases of acute liver failure[4]. Indeed, drug-induced hepatotoxicity is still the main reason for cessation of further drug development and, as well, for post-approval drug regulatory decisions including removal of several culprit drugs from the market[5]. Recent examples in the USA and Europe are troglitazone, bromfenac, trovafloxacin, ebrotidine, nimesulide, nefazodone and ximelagatran[6-8].
CLINICAL PRESENTATION OF DRUG-INDUCED HEPATOTOXICITY
In standard clinical practice, drug-induced hepatotoxicity may present in several ways (clinical and pathological) that simulate known forms of acute and chronic liver diseases; the severity ranging from sub-clinical elevations in liver enzyme concentrations to acute liver failure. Gastroenterologists need to bear hepatotoxicity in mind when conducting a differential diagnosis in every patient who presents with liver dysfunction. Mainly, drugs tend to induce acute hepatitis, cholestasis or a mixed condition. A clinical picture resembling acute viral hepatitis with jaundice, malaise, anorexia, nausea and abdominal pain is the principal presentation but, because every liver cell may be the target of drug-induced toxicity, many other expressions of hepatotoxicity may be evident including chronic hepatitis, cirrhosis, sinusoidal obstruction syndrome or neoplasm[9].
Liver histology (although not very specific and at best resulting in “compatible with”) is the ideal tool to date for defining the pattern of hepatotoxicity. However, since a liver biopsy specimen is often not available, the pattern of drug-related liver injury is, from a practical standpoint, classified according to laboratory data. This mainly includes the activity of serum alanine aminotransferase (ALT) and alkaline phosphatase (AP) with the increase in activity being expressed with respect to the upper limit of normal (ULN) and the ratio of the measured activities[10]. This classification is somewhat arbitrary and insufficient in classifying all types of drug-induced liver damage (e.g. vascular lesions and chronic damage, in general), however, the system does have some prognostic value.
Acute hepatocellular (e.g., cytotoxic, cytolytic) liver injury is defined by ALT > 2-fold that of ULN (2N) or an ALT/AP ratio ≥ 5[10]. Patients with this particular type of liver damage have non-specific clinical features, and jaundice is not always evident. Sometimes there are clues of drug allergy, such as fever, rash or peripheral eosinophilia. Serum levels of aminotransferase are markedly increased. Liver histology shows variable degrees of cell necrosis and inflammation, mainly in zone 3 of the hepatic accini together with an abundance of eosinophils in the infiltrate, which is consistent with a toxic etiology[9,11-14]. These expressions of hepatotoxicity are observed with many drugs (Table 1). Patients with acute hepatocellular injury related to drugs are at risk of acute liver failure. The observation by Hyman Zimmerman, known as “Hy’s rule”[9], predicts a mean mortality (or its surrogate marker, liver transplantation) of 10% for jaundiced patients with acute toxic hepatocellular damage (providing total bilirubin is not elevated as a result of other causes such as biliary obstruction or Gilbert syndrome). Two recent studies[3,15] have validated this observation using multivariate analysis, and they indicated that, apart from total bilirubin and the hepatocellular-type of injury, other variables such older age, female gender and AST levels were independently associated with a poor outcome[3,15].
Table 1.
Medications, herbal products and illicit drugs related to the hepatocellular-type of damage
| Compound | Other injury | Comments |
| Acarbose | FHF | |
| Allopurinol | Granuloma | Hypersensitivity |
| Amiodarone | Phospholipidosis, cirrhosis | |
| Amoxicillin, Ampicillin | ||
| Anti-HIV: (Didanosine, Zidovudine, protease inhibitors) | ||
| NSAIDs (AAS, Ibuprofen, Diclofenac, Piroxicam, Indometacin) | Nimesulide; withdrawn | |
| Asparaginase | Steatosis | |
| Bentazepam | Chronic hepatitis | |
| Chlormethizole | Cholestatic hepatitis | FHF |
| Cocaine, Ecstasy and amphetamine derivatives | FHF | |
| Diphenytoin | Hypersensitivity | |
| Disulfiram | FHF | |
| Ebrotidine | Cirrhosis | FHF |
| Fluoxetine, Paroxetine | Chronic hepatitis | |
| Flutamide | FHF | |
| Halothane | ||
| Hypolipemics; Lovastatin, Pravastatin, Simvastatin, Atorvastatin | ||
| Isoniazid | Granuloma, chronic hepatitis | FHF |
| Ketoconazole, Mebendazole, Albendazole, Pentamidine | FHF | |
| Mesalazine | Chronic hepatitis | Autoimmune features |
| Methotrexate | Steatosis, fibrosis, cirrhosis | |
| Minocycline | Chronic hepatitis, steatosis | Autoimmune features |
| Nitrofurantoin | Chronic hepatitis | |
| Nefazodone | FHF, withdrawn | |
| Omeprazole | ||
| Penicillin G | Prolonged cholestasis | |
| Pyrazinamide | ||
| Herbal remedies | FHF | |
| Germander (Teucrium chamaedrys), senna | ||
| Pennyroyal oil, kava-kava | ||
| Camellia sinnensis (green tea); Chinese herbal medicines | ||
| Risperidone | ||
| Ritodrine | ||
| Sulfasalazine | Hypersensitivity | |
| Telithromycin | ||
| Terbinafine | Cholestatic hepatitis | FHF |
| Tetracycline | Micro-steatosis | FHF |
| Tolcapone | FHF, withdrawn | |
| Topiramate | ||
| Trazodone | Chronic hepatitis | |
| Trovafloxacin | FHF, withdrawn in Europe | |
| Valproic acid | Micro-steatosis | |
| Venlafaxine | ||
| Verapamil | Granuloma | |
| Vitamin A | Fibrosis, cirrhosis | |
| Ximelagatran | FHF, discontinued |
Features of hypersensitivity include fever, rash and eosinophilia; FHF: Fulminant hepatic failure.
Acute cholestatic injury, defined as an increase in serum AP > 2N or by an ALT/AP ≤ 2 is classified into two subtypes: pure, “bland” or canalicular cholestasis; and acute cholestatic or hepatocanalicular hepatitis. Patients with acute cholestasis usually present with jaundice and itching. The canalicular pattern is characterized by an increase in conjugated bilirubin, AP and γ-glutamyl transpeptidase (γ-GT) with minimal, if any, impairment in serum transaminases. Liver biopsy shows hepatocyte cholestasis and dilated biliary canaliculi with bile plugs, but with little or no inflammation and necrosis[14]. Anabolic and contraceptive steroids typically produce this expression of hepatotoxicity.
Symptoms in the hepatocanalicular type of damage include abdominal pain and fever and, as such, resemble acute biliary obstruction. However, the associated hypersensitivity features that sometimes occur are an important clue toward the diagnosis of hepatotoxicity. Liver biopsy reveals variable degrees of portal inflammation and hepatocyte necrosis, in addition to marked cholestasis of centrilobular predominance[9,11,14]. Older age has been found to increase the likelihood of drug-induced hepatotoxicity being expressed as cholestatic damage[3,16]. Typical examples of drugs that cause this variety of liver damage are amoxicillin-clavulanate, macrolide antibiotics and phenothiazine neuroleptics, but many others have a similar capacity (Table 2).
Table 2.
Medications associated with the cholestatic-type damage
| Compound | Other injury | Comment |
| Cholestasis without hepatitis (canalicular/bland/pure jaundice) | ||
| Estrogens, contraceptive steroids and anabolic-steroids (Budd-Chiari, adenoma, carcinoma, peliosis hepatitis, adenoma, carcinoma) | ||
| Cholestatis with hepatitis (hepatocanalicular jaundice) | ||
| Amoxicillin-clavulanic acid | Chronic cholestasis | VBDS |
| Atorvastatin | Chronic cholestasis | |
| Azathioprine | Chronic cholestasis | |
| Benoxaprofen (withdrawn) | ||
| Bupropion | Chronic cholestasis | |
| Captopril, enalapril, fosinopril | ||
| Carbamazepine | Chronic cholestasis | VBDS |
| Carbimazole | ||
| Cloxacillin, dicloxacillin, flucloxacillin | ||
| Clindamycin | Chronic cholestasis | |
| Ciprofloxacin, norfloxacin | ||
| Cyproheptadine | Chronic cholestasis | VBDS |
| Diazepam, nitrazepam | ||
| Erythromycins | Chronic cholestasis | VBDS |
| Gold compounds, penicillamine | ||
| Herbal remedies: | ||
| Chaparral leaf (Larrea tridentate); Glycyrrhizin, greater celandine (Chelidonium majus) | ||
| Irbesartan | Chronic cholestasis | |
| Lipid lowering agents (“statins”) | ||
| Macrolide antibiotics | ||
| Mianserin | ||
| Mirtazapine | Chronic cholestasis | |
| Phenotiazines (chlorpromazine) | Chronic cholestasis | |
| Robecoxib, celecoxib | ||
| Rosiglitazone, oioglitazone | ||
| Roxithromycin | Chronic cholestasis | |
| Sulfamethoxazole-trimethoprim | Chronic cholestasis | VBDS |
| Sulfonamides | Chronic cholestasis | |
| Sulfonylureas (Glibenclamide, Chlorpropamide) | ||
| Sulindac, piroxicam, diclofenac, ibuprofen | ||
| Terbinafine | Chronic cholestasis | VBDS |
| Tamoxifen | Hepatocellular, peliosis Chronic cholestasis | |
| Tetracycline | Chronic cholestasis | |
| Ticlopidine & Clopidogrel | Chronic cholestasis | |
| Thiabendazole | VBDS | |
| Tricyclic antidepressants (Amitriptyline, Imipramine) | Chronic cholestasis | VBDS |
| Sclerosing cholangitis-like | Floxuridine (intra-arterial) | |
| Cholangiodestructive (primary biliary cirrhosis) | Chlorpromazine, ajmaline | |
VBDS: Vanishing bile duct syndrome.
In mixed hepatic injury the clinical and biological picture is intermediate between the hepatocellular and cholestatic patterns, and features of either type may predominate. By definition, the ALT/AP ratio is between 2 and 5. Allergy reactions are often present, as well as a granulomatous reaction in the liver biopsy specimen. When faced with a mixed hepatitis clinical picture, the gastroenterologists should always seek a culprit medication since this type of injury is far more characteristic of drug-induced hepatotoxicity than of viral hepatitis[9]. Almost all drugs that produce cholestatic injury are also capable of inducing a mixed pattern.
Although drug-induced cholestatic and mixed lesions progress to acute liver failure less frequently than hepatocellular types, their resolution is generally slower. For example, a long-term follow-up of a large cohort in a Registry demonstrated a significantly higher trend towards becoming chronic in cholestatic/mixed cases compared to hepatocelullar-type disease[17].
DIAGNOSIS IN THE CLINICAL SETTING
A straightforward diagnosis of hepatotoxicity in clinical practice is seldom possible. An exception is when symptoms of hepatitis rapidly ensue following the obvious exposure to an over-dosage of intrinsic hepatotoxins, such as acetaminophen. In these circumstances, blood concentrations of the compound could be used to confirm the suspicion. In a few other instances the diagnosis can be easily established if liver damage becomes apparent after re-exposure to a drug that had been suspected as being the cause of previous hepatitis. This topic of re-challenge is discussed in more detail later.
Direct evidence for idiosyncratic hepatotoxicity is rarely available. This includes, for a few drugs, the detection of serum circulating autoantibodies to specific forms of cythocrome P450 (Table 3). Most of these drugs have been withdrawn from the market. This circumstance, in addition to uncertainty regarding sensitivity and specificity of the autoantibody test, makes such a situation irrelevant in current clinical practice[18].
Table 3.
Autoantibodies specific to drug-induced hepatotoxicity
| Autoantibody | Example |
| Anti-mitochondrial (anti-M6) autoantibody | Iproniazid |
| Anti-liver kidney microsomal 2 antibody (anti-LKM2) | Tienilic acid |
| Anti CYP 1A2 | Dihydralazine |
| Anti CYP 2E1 | Halothane |
| Anti-liver microsomal autoantibody | Carbamazepine |
| Anti-microsomal epoxide hydrolase | Germander |
CYP: Cytochrome P450.
Another tool that has been used in the search for evidence of drug allergy is the lymphocyte-stimulation test. This comprises counting of lymphocyte proliferation following exposure of peripheral blood mononuclear cells (monocytes) from the patient to the suspected drug in vitro. Using radiolabel led thymidine incorporation in the presence of a prostaglandin inhibitor (such as indometacin), prevents the suppressive influence of activated monocytes on T-cells[19,20]. However, a positive response merely indicates sensitization towards a certain drug and cannot actually be related to effector mechanisms (symptoms) while, on the contrary, a negative test does not exclude drug allergy[21]. Finally, these in vitro tests are difficult to standardize, are poorly reproducible between laboratories, and have not gained general clinical acceptance[20,21].
Hence, in the absence of an acceptable and convenient gold standard, the diagnosis is subjective and is made with varying levels of confidence based on a combination of factors including temporal associations and with respect to latency, the rate of improvement after cessation of the drug, and the definitive exclusion of alternative possible causes[22]. Confounding features include multiple drugs prescribed for many patients, lack of information on doses consumed as well as stop and start dates[23]. A careful “step-by-step” approach should proceed according to the outline in Figure 1[24].
Figure 1.
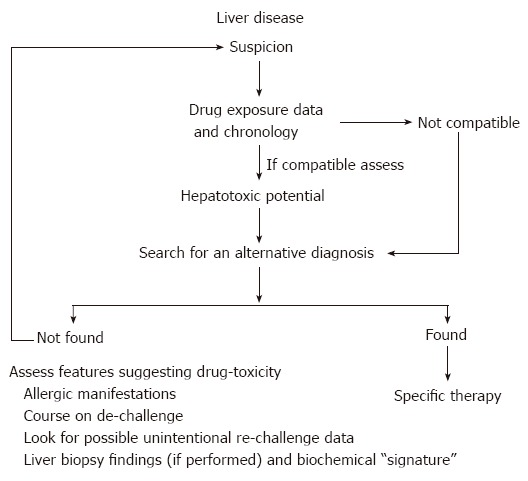
Approaching a suspicion of drug-induced hepatotoxicity.
Screening for drug exposure and assessment of its hepatotoxic potential
A thorough drug and chemical history is essential, including prescribed and over-the-counter medications as well as consumption of illicit (recreational) drugs. Soliciting medication containers or a written medication plan, when available, assists the patient’s recall and reduces errors[3]. In unconscious or confused patients or in those who are able to collaborate with the physician, the relatives or care-givers should be consulted.
The question that needs to be addressed is whether the treatment had commenced well before symptom presentation or in the early phase of hepatitis. This is because the suspected drug could actually have been prescribed to alleviate the first symptoms of hepatitis, such as gastrointestinal complaints or malaise. If this is not the case, duration of therapy with the suspected drug must be screened. Liver tests, if performed before starting the drug, can be very valuable in the patient’s assessment. The latency period of different drugs varies widely. However, there is a relatively consistent “signature” for each drug which is linked to the mechanism of damage involved. Details can usually be elicited from the patient. For instance, intrinsic hepatotoxins induce overt liver damage within a few hours of exposure. In most idiosyncratic cases, the latency period is roughly between 1 wk and 3 mo. In general, allergic hepatic reactions are likely to occur within 1 to 5 wk of taking the drug.
A delay of > 3 mo is typically seen with compounds that act by non-allergic mechanisms; i.e. “metabolic idiosyncrasy”. While drug-induced acute hepatitis seldom occurs after > 12 mo of exposure, these long latency-periods are still possible in unusual forms of chronic liver damage (such as steato-hepatitis, fibrosis and chronic hepatitis) in which the expression of hepatotoxicity is symptom-less and which allows the contra-indicated treatment to continue[25-31], or simply because the type of lesion requires prolonged exposure to become manifest (e.g. vascular lesions and tumors)[32,33].
In some instances the role of a drug is difficult to recognize because of a considerable delay (up to 3 or 4 wk) between the interruption of therapy and clinical presentation of the condition. Examples include amoxicillin-clavulanate[34], midecamycin[35] and trovafloxacin[36]. The reasons for this are unclear and could be that such an unusual time-course might combine a late immune response to the drug if its retention in the body is protracted[37].
There is no clear rule in identifying the culprit drug if the patient is taking various medications simultaneously. Attention should be paid to the latest drug introduced into the patient’s regimen since this is the one that is likely to have stimulated the reaction. However, when a known hepatotoxic drug antedates the latest medication introduced then it seems reasonable to ascribe the clinical picture to the combination of the drugs because of the possibility of pharmaco-kinetic interaction[3,38].
With respect to the hepatotoxic potential of screened drugs, their potentials for causing liver damage are not the same, and almost all marketed medications have been incriminated in incidences of hepatotoxicity[39]. For instance, some drugs like isoniazid, diclofenac, and amoxicillin-clavulanate are well-known hepatotoxic agents[3] while others such as digoxin rank very low on the list of hepatotoxins[9]. The main causative group of drugs, in a large cohort of hepatotoxicity cases collected in the Spanish Registry, was antibiotics followed by non-steroidal anti-inflammatory drugs (NSAIDs)[3]. Further, among the drugs most-frequently associated with idiosyncratic acute liver failure reported by the ALFSG, were antibiotics (particularly isoniazid), non-steroidal analgesics, anti-seizure medications and herbal preparations[40].
Valuable information can be accessed from databases of hepatotoxic drugs, such as HEPATOX from France[39], lists in reference textbooks[9,11,41] or more up-to-date resources such as MEDLINE-PubMed database of the National Library of Medicine where MESHing the name of the drug together with the terms “hepatotoxicity,” “hepatitis,” “drug-induced hepatotoxicity,” or simply “liver” can provide useful details.
If the patient has been taking a newly marketed drug, the data on its hepatotoxic potential, if known, would only be available in pre-approval clinical trials (usually involving 1500-2500 patients). This size of trial would not have the power to detect significant (clinically overt) liver disease since finding hepatotoxicity with an incidence of 1:10 000 (the approximate incidence of most idiosyncratic reactions) would require 30 000 patients to be treated in the trial (“rule of threes”)[42]. Nevertheless, the appearance of less prominent signals of liver damage in pre-approval studies should be carefully noted. These include the incidence of asymptomatic ALT and bilirubin elevations. An ALT ≥ 8N or a ≥ 1.5 fold increase in direct bilirubin, especially if it is accompanied by a raised ALT, deserves special attention since this rarely occurs in ostensibly normal populations.
Exclusion of other causes of liver damage
Diagnostic evaluation of any patient with acute liver disease of unknown origin should comprise a careful history to exclude alcohol abuse, recent episodes of hypotension, epidemiological risk factors of infectious hepatitis, specific serology and molecular biology studies for common viruses involved in viral hepatitis, as well as screening for autoimmune hepatitis. All patients should also have an abdominal ultrasound examination to exclude mechanical biliary obstruction.
The appropriateness of additional investigation would depend on the presence of particular symptoms or analytical features (Table 4). Patients with the cholestatic or mixed pattern of hepatic injury may require complementary imaging by magnetic resonance cholangiography or endoscopic retrograde cholangiography, despite normal abdominal ultrasound findings, so as to exclude benign or malignant obstruction of the biliary tract.
Table 4.
Clinical work-up to identify other possible causes of liver disease
| Test | Condition | Commentary |
| Viral serology | Viral hepatitis | Less frequent in older patients, especially Hepatitis A, search for epidemiologic risk factors, outcome may be similar to that of DILI following de-challenge. |
| IgM anti-HAV | ||
| IgM anti-HBc | ||
| Anti-HCV, RNA-HCV (RT-PCR) | ||
| IgM-CMV | ||
| IgM-EBV | ||
| Herpes virus | ||
| Bacterial serology: Salmonella, Campylobacter, Listeria, Coxiella | Bacterial hepatitis | If persistent fever and/or diarrhea |
| Serology for syphilis | Secondary syphilis | Multiple sexual partners. Disproportionately high serum AP levels. |
| Autoimmunity (ANA, ANCA, AMA, ASMA, anti-LKM-1) | Autoimmune hepatitis, Primary biliary cirrhosis | Women, ambiguous course following de-challenge. Other autoimmunity features. |
| AST/ALT ratio > 2 | Alcoholic hepatitis | Alcohol abuse. Moderate increase in transaminases despite severity at presentation |
| Ceruloplasmine, urine cooper | Wilson’s disease | Patients < 40 yr |
| Alfa-1 antitrypsin | Deficit of α-1 antitrypsin | Pulmonary disease |
| Transferrin saturation | Hemochromatosis | In anicteric hepatocellular damage. Middle-aged men and older women. |
| Brilliant eco texture of the Liver. | Non-alcoholic steatohepatitis | In anicteric hepatocellular damage. Obesity, Metabolic syndrome. |
| Transaminase levels markedly high | Ischemic hepatitis | Disproportionately high AST levels. Hypotension, shock, recent surgery, heart failure, antecedent vascular disease, elderly |
| Dilated bile ducts by image procedures (AU, CT, MRCP and ERCP) | Biliary obstruction | Colic abdominal pain, cholestatic/mixed pattern. |
ALT: alanine aminotransferase; AP: alkaline phosphatase; AST: aspartate aminotransferase; AU: abdominal ultrasound examination; Anti-HAV: Hepatitis A antibody; Anti-HBc: Hepatitis B core antibody; Anti-HCV: Hepatitis C antibody; anti-LKM-1: Liver-kidney microsomal antibody type 1; AMA: antimitochondrial antibody; ANA: antinuclear antibody; ANCA: perinuclear antineutrophil cytoplasmic antibody; ASMA: antismooth muscle antibody; BPC: Biliary primary cirrhosis; CMV: cytomegalovirus; CT: computed tomography; EBV: Epstein-Barr virus; ERCP: Endoscopic retrograde cholangiography; MRCP: Magnetic resonance cholangiography.
Features suggesting toxic liver damage
Once alternative causes of liver damage have been ruled out, the suspicion of drug-induced hepatotoxicity can be confirmed by a careful scrutiny of co-existing features of drug-allergy, by noting the course following drug cessation and following a re-challenge dose, as well as through biopsy findings or biochemical patterns compatible with toxic liver damage[24]. Drug-allergy manifestations are associated with widely variable hepatotoxicity rates depending, mainly, on the drug class. Features that suggest drug-allergy include, skin rash, fever, peripheral eosinophilia, short latency period (1 mo or less) and rapid symptoms recurrence on re-challenge. Hematological features including granulocytopenia, thrombopenia or hemolytic anemia as well as renal and pancreatic involvement may also accompany some instances of drug-induced immuno-allergic hepatic injury[43,44]. In rare cases the extreme skin involvement of Steven-Johnson syndrome or the Lyell syndrome are strong clues to drug hypersensitivity[9]. However, because these manifestations occur in a minority of cases of hepatotoxicity, their absence is not necessarily a helpful sign. In our Spanish Registry[3], some of the hallmarks of hypersensitivity (e.g., fever, rash, eosinophilia, cytopenia) were present only in 106 of 446 cases (23%) with idiosyncratic hepatotoxicity.
In some instances, typical hypersensitivity symptoms are absent. However, clues pointing toward an immuno-allergic reaction might come from the presence of more subtle features, such as detectable serum autoantibodies and antinuclear and anti-smooth-muscle antibodies[12,31]. It is very likely that immunologic and metabolic idiosyncrasies operate concurrently in many cases of drug-induced hepatic injury[9,18].
The value of hypersensitivity features as indirect evidence of drug-allergy is currently under debate. In a large cohort of patients with drug-induced idiosyncratic liver disease, a link between HLA-DRB1*15 and-DQB1*06 alleles and the cholestatic/mixed injury (but not hepatocellular injury) was established. The frequency of DRB1*07 and DQB1*02 alleles was also reduced in the cholestatic/mixed injury group[45]. Conversely, there were no differences in HLA-class II allele distributions between hepatotoxicity patients who had and those who had not any hypersensitivity features. This would suggest that the majority of cholestatic/mixed cases might have an allergy pre-disposition that was genetic, irrespective of whether they have accompanying signs of drug-allergy. This is less certain in hepatocellular cases with hypersensitivity features[46].
Rapid improvements in biochemical values following withdrawal of drug therapy raises the possibility of a toxic etiology, even though this outcome may be seen in viral hepatitis as well. For hepatocellular injury, the involvement of a drug has been defined as being “highly likely” if there is a decrease of at least 50% in the levels of liver enzymes in the first 8 d following cessation of the therapy[9]. Although less conclusive, expert consensus still considers drug involvement “suggestive” (and positively weighted on the clinical scale) if such a decrease occurs within 30 d following cessation of the therapy[10].
Gastroenterologists assessing suspected drug hepatotoxicity should be aware that other atypical outcomes make laboratory scrutiny following drug withdrawal less categorical. In general, cholestatic reactions subside more slowly, with abnormal enzyme levels persisting for long periods of more than one year in some instances[47,48].
Particularly confusing is the clinical evolution of some severe cases in which the injury may progress over several days despite drug cessation, or even progressing to fulminant hepatic failure[49,50]. Conversely, the phenomenon of “adaptation” to injury can occur with some drugs (e.g. statins). This can be responsible for the spontaneous improvement in liver function tests, despite the drug treatment being continued[42].
Currently, the only way to confidently confirm idiosyncratic drug-induced hepatotoxicity is by demonstrating a recrudescence of liver injury following re-challenge with the suspected agent. Strictly, a positive response following re-exposure can be defined as a doubling of ALT and AP values for hepatocellular and cholestatic reactions, respectively. From a practical standpoint, however, it is hard to demonstrate this in most circumstances in which unintentional re-exposure occurs. Conversely, with careful inquiry a history of inadvertent re-challenge may be sometimes elicited because jaundice had not accompanied the index episode and the symptoms were non-specific at the time (e.g., malaise, gastrointestinal complaints) and were thus easily overlooked. In such cases, what was believed to be the first instance of hepatitis was, in reality, a re-challenge episode[24].
Intentional re-challenge implies several practical problems. Firstly, re-challenge is strictly contra-indicated in drug-induced hepatocellular hepatitis with associated hypersensitivity features because there is the risk of inducing a more severe, or even fulminant, clinical picture. Secondly, the amount of drug required to provoke the reaction is not known. Arbitrarily, a single dose needs to be chosen. Arguably, however, several doses may be necessary to reproduce liver damage in “metabolic” (non-allergic) drug-induced hepatotoxicity. This false negative response to re-challenge has been demonstrated for isoniazid[9] and, probably, applies to many other drugs operating under similar mechanisms. Finally, and most importantly, re-exposure of the patient to the suspected drug cannot be ethically supported purely for diagnostic purposes. Re-exposure should be attempted only when the drug being used is deemed essential for disease treatment, such as in the treatment of tuberculosis with isoniazid. Written informed consent needs to be obtained from the patient. Nevertheless, taking into consideration the consequences of misdiagnosing hepatotoxicity in pre-approval clinical trials[12], we believe that testing clinical or sub-clinical hepatitis in the trial setting might be an additional indication for re-challenge[24].
A common misconception among clinical gastroenterologists is the need to have a liver biopsy specimen to establish a diagnosis of drug-induced hepatotoxicity with confidence. Rather, since there are no histological findings specific for toxic damage, liver biopsy should not be performed routinely for this indication[14,51]. Indeed, a liver biopsy specimen, which is often taken several days after the clinical presentation of the symptoms when the pathological features are beginning to wane, may generate perplexity and confusion in cases in which chronological sequence criteria are critical and when exclusion of alternative causes appear to incriminate the drug.
Currently, a reasonable approach for performing a liver biopsy in patients with suspected drug-induced hepatotoxicity is restricted[13] to when the patient may have an underlying liver disease and, hence, it is difficult to ascribe the picture to the candidate drug or to a recrudescence of the disease (Table 5) or, alternatively, to characterize the pattern of injury with those drugs that had not been previously incriminated in hepatotoxicity[12,30,36]. We believe that a liver biopsy is also justified for identifying more severe or residual lesions (e.g. fibrosis), which could have prognostic significance. For instance, in some chronic variants of hepatotoxicity, clinical and laboratory features reflect the severity of the liver injury[30,31] poorly and a liver biopsy may clarify its true magnitude. Further, severe bile duct injury during cholestatic hepatitis has been shown to be predictive of clinical evolution into chronic cholestasis[52], and, in a retrospective study, the presence of fibrosis in the index liver biopsy had been related to the development of chronic liver disease[53].
Table 5.
Rationale for performing liver biopsy in a case suspected of having drug-induced hepatotoxicity
| Clinical setting | Presentation |
| Any clinical context | Putative drugs not previously incriminated in liver toxicity |
| Acute or chronic liver disease | Female, autoantibody sero-positive |
| High serum gammaglobulin and immunoglobulin G levels at presentation | |
| Incomplete or ambiguous de-challenge | |
| Chronic alcoholism | Acute deterioration during aversive therapy (disulfiram, carbimide calcium) |
| Any acute liver deterioration in a patient with cirrhosis or chronic hepatitis C. | e.g. worsening of liver function in a patient with primary biliary cirrhosis receiving rifampicin or a chronic hepatitis C patient receiving ibuprofen |
| Chronic impairment in liver tests in non-jaundiced patients. | Especially if constitutional symptoms and/or clinical signs of portal hypertension are disclosed. |
| Young patients with sero-negative acute hepatitis or chronic liver disease. | Moderate decrease in ceruloplasmin levels or slight increases in urinary copper excretion. |
Since a liver biopsy is not available in most cases, focus on the biochemical expression of hepatic damage may help in incriminating a specific medication. Each drug appears to have its own “signature” in relation to a more-or-less specific pattern of liver injury[7,42]. Although this is true for some drugs (e.g., estrogens induce cholestatic injury and seldom any present with any other pattern of damage), for most other drugs such consistency is not so clear. For instance, amoxicillin-clavulanate tends to produce cholestatic or mixed damage, although hepatocellular damage has been reported frequently as well[16,54]. Hepatocellular and cholestatic or mixed injury have been noted with nimesulide[55] or troglitazone[56,57], among others. Hence it is important for gastroenterologists to view a suspicion of drug-induced hepatotoxicity with caution and with awareness that any given drug can produce diverse types of injury[58].
CAUSALITY ASSESSMENT METHODS: IN SEARCH OF GREATER OBJECTIVITY
Clinical judgment is a necessary first step in the identification of any hepatic disease suspected of being caused by a drug or toxin. Diagnostic precision and objectivity are essential from the perspective of the practicing clinician who must decide whether to continue, or to stop, a therapy even though it may be the most appropriate for the disease under treatment and which might induce new events in the future if not correctly identified. Except for the very rare circumstances in which an unintentional positive re-challenge may confirm the putative involvement of a drug, the evidence that is usually collected is often circumstantial, based on subjective impressions from previous experiences, and can lead to inaccurate diagnosis[59]. The process is time-consuming and delays clinical judgment; at least until other possible causes of liver disease have been excluded.
An approach that does not follow objective guidelines that complement standard clinical practice, results in causation categories that may be defined as drug-related (e.g. acetaminophen overdose, instances of positive re-challenge), not drug related (an alternative explanation found) or when the role of a medication may appear conditional[22]. This last judgment in which subjectivity prevails does, indeed, represent the bulk of situations in standard clinical practice. In addition, this judgment depends closely on the attending physician’s skill and attitude towards the disease under consideration. Hence, agreement among physicians who evaluate a given case of drug-suspected hepatotoxicity may differ considerably. Variations in data consistency, completeness, and subjective weighting of causality arguments would, presumably, contribute to these differences.
Algorithms or clinical scales
Over the last three decades, several groups have developed methods to improve the consistency, accuracy and objectiveness in causality assessment of adverse drug reactions. The qualities required for any scoring system are, usually, reproducibility and validity[60]. Reproducibility ensures an identical result when the scales are applied irrespective of the user. Validity refers to the capacity to distinguish between cases when the drug is responsible, and cases when the drug it is not responsible.
There are two possible categories of approach: the probabilistic approach[61] based on Bayesian statistics, which is rarely used in routine clinical practice because the approach requires precisely-quantified data to model the probability distributions for each parameter. The alternative approach is the widely used algorithm or clinical scale[62]. The key features of an adverse reaction are identified and integrated into an objective rating scale based on the sum of weighted numerical values assigned to individual axes of a decision strategy. The scores are translated into categories of suspicion. The different causality assessment methods developed can produce different numerical scales that may or may not be super-imposable and with non-identical categories of suspicion. This complicates any comparisons among the different scales[62].
The Naranjo Adverse Drug Reaction Probability Scale (1981) proposed for adverse reactions to drugs (not restricted to hepatotoxicity) offers the advantage of simplicity and wide applicability[63]. This scale involves ten “yes”, “no” or “not known or inapplicable” answers to questions concerning several disease-related areas: temporal relationship, competing causes, de-challenge/re-challenge results, and knowledge of the drug’s reactions. In addition, universally-accepted criteria are introduced: placebo challenge, drug concentrations and objective measurement of adverse drug reaction. An adverse drug reaction is described as a probability category based on the total score. The categories are: definite (≥ 9 points scored), likely (5 to 8 points), possible (1 to 4 points), and doubtful (≤ 0 points). The scale has been validated and has resulted in improved reproducibility of patient evaluations. The main source of inter-observer disagreement has been the question of alternative causes and reflects, perhaps, the complexity of the clinical situation and differences in clinical training among observers. Despite the lack of specificity with respect to hepatotoxicity, use of the Naranjo scale is a requirement by some journals when adverse drug-related events are reported[63,64] and, as well, in reporting to national drug monitoring bodies.
In 1992, under the auspices of the Council for International Organizations of Medical Sciences, a working group developed and implemented a standardized method for drug causality assessment and the scales are named after the organizers of the consensus meeting: CIOMS or RUCAM (Roussel Uclaf Causality Assessment Method)[65,66]. This method provides a standardized scoring system in which the limits and contents of most criteria were decided by consensus among experts on the basis of organ-oriented characteristics. The time-to-onset and duration are evaluated separately for hepatocellular versus cholestatic/mixed reactions since the latter can occur long after the cessation and may be resolved much more slowly (Table 6). The CIOMS/RUCAM scale provides a scoring system for 6 axes in the decision strategy. The categories of suspicion are “definite or highly probable” (score > 8), “probable” (score 6-8), “possible” (score 3-5), “unlikely” (score 1-2) and “excluded” (score ≤ 0). One of the advantages of this system that is of note is that there are very few questions that require a subjective response. The scale can assign a definitive diagnosis of drug-induced hepatotoxicity in patients even without re-challenge. Also, it performs well with newly-marketed drugs or for a previously-unreported liver injury associated with an older drug. The major drawback is its complexity. It requires training in its administration and is less efficient when a user is unfamiliar with the format. The scale may seem cumbersome and while reading across the page, care needs to be taken to not misunderstand the questions; otherwise careless errors can be made. Recently, experts have criticized the weighting attributed to certain of the risk factors (e.g., age of the patient > 55 years, alcohol consumption, pregnancy) which, at best, would be significant only for a limited number of drugs[23,42].
Table 6.
Comparison of the scores for individual axes of the CIOMS and Maria & Victorino diagnostic scales
| CIOMS criteria | Score | Maria & Victorino criteria | Score |
| Chronology criterion | Chronology criterion | ||
| From drug intake until event onset | +2 to +1 | From drug intake until event onset | +1 to +3 |
| From drug withdrawal until event onset | +1 to 0 | From drug withdrawal until event onset | -3 to +3 |
| Time-course of the reaction | -2 to +3 | Time-course of the reaction | 0 to +3 |
| Risk factors | Exclusion of alternative causes | -3 to +3 | |
| Age | +1 to 0 | ||
| Alcohol | +1 to 0 | Extra-hepatic manifestations | 0 to +3 |
| Concomitant therapy | -3 to 0 | Literature data | -3 to +2 |
| Exclusion of non-drug-related causes | -3 to +2 | Re-challenge | 0 to +3 |
| Literature data | 0 to +2 | ||
| Re-challenge | -2 to +3 |
More recently, Maria and Victorino from Portugal developed a simplified scoring system to overcome the above-mentioned problems. Called the Clinical Diagnostic Scale[67] (also termed the M&V scale) it uses several features of the CIOMS/RUCAM scale while omitting and adding others (Table 6). Five components were selected for inclusion in the scale: temporal relationship between drug intake and the onset of clinical symptoms, exclusion of alternative causes, presence of extra-hepatic manifestations (e.g., rash, fever, arthralgia, eosinophilia > 6% and cytopenia), intentional or accidental re-exposure to the drug, and previous reports in the literature. The sum of the points for each parameter can vary from -6 to +20. Concordance with the five classic degrees of probability of adverse drug reactions is established on the basis of the tabulated score as follows: “definite” (score > 17), “probable” (score 14-17), “possible” (score 10-13), “unlikely” (score 6-9) and “excluded” (score < 6). The authors highlighted some limitations of the scale: The instrument performs poorly in atypical cases of drugs with unusually-long latency periods or chronic outcome. There is room for improvement in the exclusion of alternative causes of liver injury by more clearly specifying the clinical conditions to be excluded, as well as including detailed criteria for exclusion. The main advantage of the M&V scale is its ease of application in standard clinical practice.
Comparison of assessment methods in hepatotoxicity
The merits of the CIOMS and the M&V scales and their degree of concordance were compared in a population of 215 patients included in a registry of hepatotoxicity[68]. Causality in this population had been verified previously by 3 experts as being drug-induced (185) or as non-drug (30 cases). Complete agreement between the M&V scale and the CIOMS scale was obtained in only 42 cases (18%). Discrepancies in the assessment of causality occurred in 186 ratings; in each of these cases the CIOMS scale ascribed a higher level of certainty than the M&V scale. The M&V system classified only about one third of the cases as “probable” or “definite”, and tended to underestimate the probability of causality. Indeed, the performance of the M&V scale was poor in reactions with long latency periods (more than 15 d; for example amoxicillin/clavulanic acid), clinical progression to chronic status following withdrawal (cholestatic pattern), or death.
The concordance of assessment was low because the two methods assigned different weightings to the assessment criteria and, as such, the reasons for discordance could be clearly identified. For example, a time-lapse of > 15 d between drug withdrawal and event onset can be rectified by subtracting 3 points from the score on the M&V scale. A time-lapse of > 6 mo between drug withdrawal and normalization of laboratory values (in cholestatic or mixed type of injury) or 2 mo (in hepatocellular damage) precluded a “definite” or “probable” diagnosis being reached. Unknown reactions to drugs marketed for > 5 years preclude a “certainty” diagnosis. Conversely, the best correlation between the two scales was found for drug-induced liver injury that included a probable immuno-allergic mechanism. This is because the M&V scale includes questions that apply only to cases with extra-hepatic features. It would appear, therefore, that the CIOMS instrument shows better agreement with “common sense” clinical judgment. Aside from its clinical validity, the usefulness of the CIOMS scale is that it provides a framework that emphasizes topics that need to be addressed in cases of suspected hepatic adverse reaction in order to improve the consistency of judgment[68].
The Clinical Diagnostic Scale (CDS or M&V) was further evaluated in the causality assessment of 135 hepatotoxic adverse drug reaction reports[69]. Initially, the CIOMS criteria were used to classify reactions as “drug-related”, “drug-unrelated” and “indeterminate.” Reports classified as drug-related (49 reactions) scored higher on the clinical scale, with a median score of 12 (range 8-15). Of those, no reactions were classified as “definite”, 20 were classified as “probable” and 23 as “possible”. It is important to note that 6 patients were classified as “unlikely”. The authors suggested that a cut-off score > 9 (falling into the category of “possible”) be used in clinical decision-making. It is of further note that “possible” is a fairly low category adjacent to “unlikely” and this makes the cut-off score somewhat unreliable for decision-making. In addition, the authors did not assess or compare the merits of the two systems in any detail[70]. Six patients whose hepatotoxicity was considered drug-related on the basis of the consensus classification (four of these patients having a positive re-challenge) scored < 10 (“unlikely”). Two patients had flucloxacillin-induced cholestasis that first appeared > 15 d following drug withdrawal, and in two other patients the reactions were fatal and therefore precluded an accurate assignment of cause. Two other patients with a long latency period scored only 1 point each for the onset-of-reaction score. These examples confirm the limitations of the clinical scale, as highlighted by the authors themselves and which are in accordance with the conclusions reached by Lucena et al[68].
These comparative studies clearly show that the CIOMS scale, although far from being a perfect instrument, provides a uniform basis from which to develop a more precise approach in determining the causes of drug-induced hepatotoxicity. Indeed, medical journals should insist on the application of the scale as a quality control prior to accepting reports of hepatotoxicity. Nevertheless, rules for assigning causality in drug-induced liver injury are no substitute for clinical judgment. For instance, when more than one drug could be the culprit, a “blind” application of the scale can lead to a somewhat misleading causality assessment if only chronological criteria are taken into account[38]. To avoid this, attention should be paid to major drug metabolic mechanisms in relation to potential pharmacokinetic interactions with the drug[71].
FUTURE DIRECTIONS
Apart from the development of unequivocal diagnostic biomarkers in the near future, it would be feasible in the short term to develop some refinements to make the CIOM scale more realistic; more relevant data can be incorporated and low-impact items need to be deleted from the scoring system. This task will be helped by using large databases of bona fide cases of hepatotoxicity. The DILIN network is developing and testing such a causality assessment method by a complex computer-based process for gathering and distributing relevant information[72]. This analysis would useful to confirm or discard alcohol, age >55 years and pregnancy as general risk factors for hepatotoxicity, while evaluating the roles of other candidate susceptibility factors such as obesity (a condition that is associated with an increased expression of CYP2E1)[1]. Further, the age cut-off point does not consider the pediatric age range as a risk factor for toxicity of some drugs. Other known risk factors for individual drugs when present in the appropriate setting should be incorporated (e.g. HIV infection in sulfonamide use, co-infection with hepatitis B/hepatitis C virus and antiretroviral drugs, female gender for diclofenac).
In real practice, to make a definite diagnosis of drug-induced hepatotoxicity, clinicians pay much attention in assigning causality to a concordance between the actual biochemical profile of the patient and that which is provided by consensus guidelines relating to the suspected drug (for instance, cholestatic damage with amoxicillin-clavulanate use). As well, the presence of hypersensitivity features is considered by practicing physicians of crucial value in the attribution of culpability to a specific drug. Neither biochemical “signature” nor hypersensitivity features are weighted in the CIOMS scale[73] and these discrepancies await resolution.
Apart from these important questions, there is the need to validate a new instrument with an abridged scale that would provide a better approximation to the truth; i.e., the likelihood that a given case of hepatitis is due to a specific drug, at the very beginning of the patient evaluation process when key clinical decisions need to be made. The diagnosis needs to be made with confidence on admission of the patient and maintained while further confirmatory information is gathered. This would be the goal of a clinical assessment tool for the evaluation of drug-induced hepatotoxicity.
Footnotes
Supported partly by research grants from the Agencia Española del Medicamento and from the Fondo de Investigación Sanitaria (FIS 04-1688 and FIS 04-1759)
S- Editor Wang GP L- Editor Luzte M E- Editor Bi L
References
- 1.Bissell DM, Gores GJ, Laskin DL, Hoofnagle JH. Drug-induced liver injury: mechanisms and test systems. Hepatology. 2001;33:1009–1013. doi: 10.1053/jhep.2001.23505. [DOI] [PubMed] [Google Scholar]
- 2.Hoofnagle JH. Drug-induced liver injury network (DILIN) Hepatology. 2004;40:773. doi: 10.1002/hep.20445. [DOI] [PubMed] [Google Scholar]
- 3.Andrade RJ, Lucena MI, Fernández MC, Pelaez G, Pachkoria K, García-Ruiz E, García-Muñoz B, González-Grande R, Pizarro A, Durán JA, et al. Drug-induced liver injury: an analysis of 461 incidences submitted to the Spanish registry over a 10-year period. Gastroenterology. 2005;129:512–521. doi: 10.1016/j.gastro.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Ostapowicz G, Fontana RJ, Schiødt FV, Larson A, Davern TJ, Han SH, McCashland TM, Shakil AO, Hay JE, Hynan L, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–954. doi: 10.7326/0003-4819-137-12-200212170-00007. [DOI] [PubMed] [Google Scholar]
- 5.Bakke OM, Manocchia M, de Abajo F, Kaitin KI, Lasagna L. Drug safety discontinuations in the United Kingdom, the United States, and Spain from 1974 through 1993: a regulatory perspective. Clin Pharmacol Ther. 1995;58:108–117. doi: 10.1016/0009-9236(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 6.Shah RR. Drug-induced hepatotoxicity: pharmacokinetic perspectives and strategies for risk reduction. Adverse Drug React Toxicol Rev. 1999;18:181–233. [PubMed] [Google Scholar]
- 7.Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:474–485. doi: 10.1056/NEJMra021844. [DOI] [PubMed] [Google Scholar]
- 8.Mohapatra R, Tran M, Gore JM, Spencer FA. A review of the oral direct thrombin inhibitor ximelagatran: not yet the end of the warfarin era. Am Heart J. 2005;150:19–26. doi: 10.1016/j.ahj.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman HJ. Hepatotoxicity. The adverse effects of Drugs and Other Chemicals on the Liver. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 10.Bénichou C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. J Hepatol. 1990;11:272–276. doi: 10.1016/0168-8278(90)90124-a. [DOI] [PubMed] [Google Scholar]
- 11.Farrell GC. Drug Induced Liver Disease. London: Churchill-Livingstone; 1994. [Google Scholar]
- 12.Andrade RJ, Lucena MI, Martin-Vivaldi R, Fernandez MC, Nogueras F, Pelaez G, Gomez-Outes A, Garcia-Escaño MD, Bellot V, Hervás A, et al. Acute liver injury associated with the use of ebrotidine, a new H2-receptor antagonist. J Hepatol. 1999;31:641–646. doi: 10.1016/s0168-8278(99)80343-2. [DOI] [PubMed] [Google Scholar]
- 13.Larrey D. Drug-induced liver diseases. J Hepatol. 2000;32:77–88. doi: 10.1016/s0168-8278(00)80417-1. [DOI] [PubMed] [Google Scholar]
- 14.Goodman ZD. Drug hepatotoxicity. Clin Liver Dis. 2002;6:381–397. doi: 10.1016/s1089-3261(02)00011-9. [DOI] [PubMed] [Google Scholar]
- 15.Björnsson E, Olsson R. Outcome and prognostic markers in severe drug-induced liver disease. Hepatology. 2005;42:481–489. doi: 10.1002/hep.20800. [DOI] [PubMed] [Google Scholar]
- 16.Lucena MI, Andrade RJ, Fernández MC, Pachkoria K, Pelaez G, Durán JA, Villar M, Rodrigo L, Romero-Gomez M, Planas R, et al. Determinants of the clinical expression of amoxicillin-clavulanate hepatotoxicity: a prospective series from Spain. Hepatology. 2006;44:850–856. doi: 10.1002/hep.21324. [DOI] [PubMed] [Google Scholar]
- 17.Andrade RJ, Lucena MI, Kaplowitz N, García-Muņoz B, Borraz Y, Pachkoria K, García-Cortés M, Fernández MC, Pelaez G, Rodrigo L, et al. Outcome of acute idiosyncratic drug-induced liver injury: Long-term follow-up in a hepatotoxicity registry. Hepatology. 2006;44:1581–1588. doi: 10.1002/hep.21424. [DOI] [PubMed] [Google Scholar]
- 18.Kaplowitz N. Drug-induced liver disorders: introduction and overview. In: Kaplowitz N, Deleve LD, editors. Drug-induced liver disease. New York: Marcel Dekker Inc; 2003. pp. 1–14. [Google Scholar]
- 19.Maria VA, Victorino RM. Diagnostic value of specific T cell reactivity to drugs in 95 cases of drug induced liver injury. Gut. 1997;41:534–540. doi: 10.1136/gut.41.4.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maria VA, Victorino RM. Immunological investigation in hepatic drug reactions. Clin Exp Allergy. 1998;28 Suppl 4:71–77. [PubMed] [Google Scholar]
- 21.Berg PA, Becker EW. The lymphocyte transformation test--a debated method for the evaluation of drug allergic hepatic injury. J Hepatol. 1995;22:115–118. doi: 10.1016/0168-8278(95)80270-3. [DOI] [PubMed] [Google Scholar]
- 22.Kaplowitz N. Causality assessment versus guilt-by-association in drug hepatotoxicity. Hepatology. 2001;33:308–310. doi: 10.1053/jhep.2001.21083. [DOI] [PubMed] [Google Scholar]
- 23.Lee WM, Senior JR. Recognizing drug-induced liver injury: current problems, possible solutions. Toxicol Pathol. 2005;33:155–164. doi: 10.1080/01926230590522356. [DOI] [PubMed] [Google Scholar]
- 24.Andrade RJ, Camargo R, Lucena MI, González-Grande R. Causality assessment in drug-induced hepatotoxicity. Expert Opin Drug Saf. 2004;3:329–344. doi: 10.1517/14740338.3.4.329. [DOI] [PubMed] [Google Scholar]
- 25.Lewis JH, Ranard RC, Caruso A, Jackson LK, Mullick F, Ishak KG, Seeff LB, Zimmerman HJ. Amiodarone hepatotoxicity: prevalence and clinicopathologic correlations among 104 patients. Hepatology. 1989;9:679–685. doi: 10.1002/hep.1840090504. [DOI] [PubMed] [Google Scholar]
- 26.Oien KA, Moffat D, Curry GW, Dickson J, Habeshaw T, Mills PR, MacSween RN. Cirrhosis with steatohepatitis after adjuvant tamoxifen. Lancet. 1999;353:36–37. doi: 10.1016/S0140-6736(05)74872-8. [DOI] [PubMed] [Google Scholar]
- 27.Lewis JH, Schiff E. Methotrexate-induced chronic liver injury: guidelines for detection and prevention. The ACG Committee on FDA-related matters. American College of Gastroenterology. Am J Gastroenterol. 1988;83:1337–1345. [PubMed] [Google Scholar]
- 28.Sharp JR, Ishak KG, Zimmerman HJ. Chronic active hepatitis and severe hepatic necrosis associated with nitrofurantoin. Ann Intern Med. 1980;92:14–19. doi: 10.7326/0003-4819-92-1-14. [DOI] [PubMed] [Google Scholar]
- 29.Sturkenboom MC, Meier CR, Jick H, Stricker BH. Minocycline and lupuslike syndrome in acne patients. Arch Intern Med. 1999;159:493–497. doi: 10.1001/archinte.159.5.493. [DOI] [PubMed] [Google Scholar]
- 30.Andrade RJ, Lucena MI, Alcantara R, Fraile JM. Bentazepam-associated chronic liver disease. Lancet. 1994;343:860. doi: 10.1016/s0140-6736(94)92065-6. [DOI] [PubMed] [Google Scholar]
- 31.Andrade RJ, Lucena MI, Aguilar J, Lazo MD, Camargo R, Moreno P, García-Escaño MD, Marquez A, Alcántara R, Alcáin G. Chronic liver injury related to use of bentazepam: an unusual instance of benzodiazepine hepatotoxicity. Dig Dis Sci. 2000;45:1400–1404. doi: 10.1023/a:1005520523502. [DOI] [PubMed] [Google Scholar]
- 32.Ishak KG, Zimmerman HJ. Hepatotoxic effects of the anabolic/androgenic steroids. Semin Liver Dis. 1987;7:230–236. doi: 10.1055/s-2008-1040579. [DOI] [PubMed] [Google Scholar]
- 33.Ishak KG, Zimmerman HJ. Morphologic spectrum of drug-induced hepatic disease. Gastroenterol Clin North Am. 1995;24:759–786. [PubMed] [Google Scholar]
- 34.Andrade RJ, Lucena MI, Fernández MC, Vega JL, Camargo R. Hepatotoxicity in patients with cirrhosis, an often unrecognized problem: lessons from a fatal case related to amoxicillin/clavulanic acid. Dig Dis Sci. 2001;46:1416–1419. doi: 10.1023/a:1010627518254. [DOI] [PubMed] [Google Scholar]
- 35.Pérez Moreno JM, Saldaña González FJ, Puertas Montenegro M, Báez Perea J. Cholestatic hepatitis caused by midecamycin. Gastroenterol Hepatol. 1996;19:459–461. [PubMed] [Google Scholar]
- 36.Lucena MI, Andrade RJ, Rodrigo L, Salmerón J, Alvarez A, Lopez-Garrido MJ, Camargo R, Alcantára R. Trovafloxacin-induced acute hepatitis. Clin Infect Dis. 2000;30:400–401. doi: 10.1086/313680. [DOI] [PubMed] [Google Scholar]
- 37.Kaplowitz N. Drug-induced liver injury. Clin Infect Dis. 2004;38 Suppl 2:S44–S48. doi: 10.1086/381446. [DOI] [PubMed] [Google Scholar]
- 38.Lucena MI, Andrade RJ, Vicioso L, González FJ, Pachkoria K, García-Muñoz B. Prolonged cholestasis after raloxifene and fenofibrate interaction: A case report. World J Gastroenterol. 2006;12:5244–5246. doi: 10.3748/wjg.v12.i32.5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Biour M, Poupon R, Grangé JD, Chazouillères O. Drug-induced hepatotoxicity. The 13th updated edition of the bibliographic database of drug-related liver injuries and responsible drugs. Gastroenterol Clin Biol. 2000;24:1052–1091. [PubMed] [Google Scholar]
- 40.Lee WM. Acute liver failure in the United States. Semin Liver Dis. 2003;23:217–226. doi: 10.1055/s-2003-42641. [DOI] [PubMed] [Google Scholar]
- 41.Stricker BHCH. Drug-induced Hepatic Injury, 2nd ed. Amsterdam: Elsevier; 1992. [Google Scholar]
- 42.Kaplowitz N. Drug-induced liver disorders: implications for drug development and regulation. Drug Saf. 2001;24:483–490. doi: 10.2165/00002018-200124070-00001. [DOI] [PubMed] [Google Scholar]
- 43.Carrillo-Jimenez R, Nurnberger M. Celecoxib-induced acute pancreatitis and hepatitis: a case report. Arch Intern Med. 2000;160:553–554. doi: 10.1001/archinte.160.4.553. [DOI] [PubMed] [Google Scholar]
- 44.Schattner A, Sokolovskaya N, Cohen J. Fatal hepatitis and renal failure during treatment with nimesulide. J Intern Med. 2000;247:153–155. doi: 10.1046/j.1365-2796.2000.00612.x. [DOI] [PubMed] [Google Scholar]
- 45.Andrade RJ, Lucena MI, Alonso A, García-Cortes M, García-Ruiz E, Benitez R, Fernández MC, Pelaez G, Romero M, Corpas R, et al. HLA class II genotype influences the type of liver injury in drug-induced idiosyncratic liver disease. Hepatology. 2004;39:1603–1612. doi: 10.1002/hep.20215. [DOI] [PubMed] [Google Scholar]
- 46.Velayudham LS, Farrell GC. Drug-induced cholestasis. Expert Opin Drug Saf. 2003;2:287–304. doi: 10.1517/14740338.2.3.287. [DOI] [PubMed] [Google Scholar]
- 47.Andrade RJ, Guilarte J, Salmerón FJ, Lucena MI, Bellot V. Benzylpenicillin-induced prolonged cholestasis. Ann Pharmacother. 2001;35:783–784. doi: 10.1345/aph.10266. [DOI] [PubMed] [Google Scholar]
- 48.Andrade RJ, Lucena MI, Fernández MC, Vega JL, García-Cortés M, Casado M, Guerrero-Sanchez E, Pulido-Fernandez F. Cholestatic hepatitis related to use of irbesartan: a case report and a literature review of angiotensin II antagonist-associated hepatotoxicity. Eur J Gastroenterol Hepatol. 2002;14:887–890. doi: 10.1097/00042737-200208000-00014. [DOI] [PubMed] [Google Scholar]
- 49.Andrade RJ, Lucena MI, Fernández MC, González M. Fatal hepatitis associated with nimesulide. J Hepatol. 2000;32:174. doi: 10.1016/s0168-8278(00)80208-1. [DOI] [PubMed] [Google Scholar]
- 50.Lucena MI, Andrade RJ, Gomez-Outes A, Rubio M, Cabello MR. Acute liver failure after treatment with nefazodone. Dig Dis Sci. 1999;44:2577–2579. doi: 10.1023/a:1026620029470. [DOI] [PubMed] [Google Scholar]
- 51.Bianchi L. Liver biopsy in elevated liver functions tests? An old question revisited. J Hepatol. 2001;35:290–294. doi: 10.1016/s0168-8278(01)00155-6. [DOI] [PubMed] [Google Scholar]
- 52.Degott C, Feldmann G, Larrey D, Durand-Schneider AM, Grange D, Machayekhi JP, Moreau A, Potet F, Benhamou JP. Drug-induced prolonged cholestasis in adults: a histological semiquantitative study demonstrating progressive ductopenia. Hepatology. 1992;15:244–251. doi: 10.1002/hep.1840150212. [DOI] [PubMed] [Google Scholar]
- 53.Aithal PG, Day CP. The natural history of histologically proved drug induced liver disease. Gut. 1999;44:731–735. doi: 10.1136/gut.44.5.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown SJ, Desmond PV. Hepatotoxicity of antimicrobial agents. Semin Liver Dis. 2002;22:157–167. doi: 10.1055/s-2002-30103. [DOI] [PubMed] [Google Scholar]
- 55.Van Steenbergen W, Peeters P, De Bondt J, Staessen D, Büscher H, Laporta T, Roskams T, Desmet V. Nimesulide-induced acute hepatitis: evidence from six cases. J Hepatol. 1998;29:135–141. doi: 10.1016/s0168-8278(98)80188-8. [DOI] [PubMed] [Google Scholar]
- 56.Herrine SK, Choudhary C. Severe hepatotoxicity associated with troglitazone. Ann Intern Med. 1999;130:163–164. doi: 10.7326/0003-4819-130-2-199901190-00021. [DOI] [PubMed] [Google Scholar]
- 57.Bonkovsky HL, Azar R, Bird S, Szabo G, Banner B. Severe cholestatic hepatitis caused by thiazolidinediones: risks associated with substituting rosiglitazone for troglitazone. Dig Dis Sci. 2002;47:1632–1637. doi: 10.1023/a:1015895925374. [DOI] [PubMed] [Google Scholar]
- 58.Andrade RJ, Lucena MI. Drug-induced hepatotoxicity. N Engl J Med. 2003;349:1974–1976; author reply 1974-1976. [PubMed] [Google Scholar]
- 59.Aithal GP, Rawlins MD, Day CP. Accuracy of hepatic adverse drug reaction reporting in one English health region. BMJ. 1999;319:1541. doi: 10.1136/bmj.319.7224.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hutchinson TA, Lane DA. Assessing methods for causality assessment of suspected adverse drug reactions. J Clin Epidemiol. 1989;42:5–16. doi: 10.1016/0895-4356(89)90020-6. [DOI] [PubMed] [Google Scholar]
- 61.Bate A, Lindquist M, Edwards IR, Olsson S, Orre R, Lansner A, De Freitas RM. A Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol. 1998;54:315–321. doi: 10.1007/s002280050466. [DOI] [PubMed] [Google Scholar]
- 62.Pere JC, Begaud B, Haramburu F, Albin H. Computerized comparison of six adverse drug reaction assessment procedures. Clin Pharmacol Ther. 1986;40:451–461. doi: 10.1038/clpt.1986.206. [DOI] [PubMed] [Google Scholar]
- 63.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, Janecek E, Domecq C, Greenblatt DJ. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–245. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 64.García-Cortés M, Lucena MI, Andrade RJ, Camargo R, Alcántara R. Is the Naranjo probability scale accurate enough to ascertain causality in drug-induced hepatotoxicity? Ann Pharmacother. 2004;38:1540–1541. doi: 10.1345/aph.1E007. [DOI] [PubMed] [Google Scholar]
- 65.Danan G, Benichou C. Causality assessment of adverse reactions to drugs--I. A novel method based on the conclusions of international consensus meetings: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–1330. doi: 10.1016/0895-4356(93)90101-6. [DOI] [PubMed] [Google Scholar]
- 66.Benichou C, Danan G, Flahault A. Causality assessment of adverse reactions to drugs--II. An original model for validation of drug causality assessment methods: case reports with positive rechallenge. J Clin Epidemiol. 1993;46:1331–1336. doi: 10.1016/0895-4356(93)90102-7. [DOI] [PubMed] [Google Scholar]
- 67.Maria VA, Victorino RM. Development and validation of a clinical scale for the diagnosis of drug-induced hepatitis. Hepatology. 1997;26:664–669. doi: 10.1002/hep.510260319. [DOI] [PubMed] [Google Scholar]
- 68.Lucena MI, Camargo R, Andrade RJ, Perez-Sanchez CJ, Sanchez De La Cuesta F. Comparison of two clinical scales for causality assessment in hepatotoxicity. Hepatology. 2001;33:123–130. doi: 10.1053/jhep.2001.20645. [DOI] [PubMed] [Google Scholar]
- 69.Aithal GP, Rawlins MD, Day CP. Clinical diagnostic scale: a useful tool in the evaluation of suspected hepatotoxic adverse drug reactions. J Hepatol. 2000;33:949–952. doi: 10.1016/s0168-8278(00)80127-0. [DOI] [PubMed] [Google Scholar]
- 70.Lee WM. Assessing causality in drug-induced liver injury. J Hepatol. 2000;33:1003–1005. doi: 10.1016/s0168-8278(00)80136-1. [DOI] [PubMed] [Google Scholar]
- 71.Andrade RJ, Lucena MI. Acute fulminant hepatitis after treatment with rabeprazole and terbinafine: is rabeprazole the culprit? Arch Intern Med. 2002;162:360–361. doi: 10.1001/archinte.162.3.360. [DOI] [PubMed] [Google Scholar]
- 72.Watkins PB, Seeff LB. Drug-induced liver injury: summary of a single topic clinical research conference. Hepatology. 2006;43:618–631. doi: 10.1002/hep.21095. [DOI] [PubMed] [Google Scholar]
- 73.Takamori Y, Takikawa H, Kumagi T, Oriyi M, Watanaba M, Shibuya A, Hisamochi A, Kumashiro R, Ito T, Mitsumoto Y, et al. Assessment of the diagnostic scale for drug-induced liver injury by the international consensus meeting and a proposal of its modifications. Hepatology. 2003;38 Suppl 1:703A. doi: 10.1016/s1386-6346(03)00232-8. [DOI] [PubMed] [Google Scholar]


