Abstract
AIM: To investigate the expression of Cyclooxygenase-2 (COX-2), proliferating cell nuclear antigen (PCNA), Ki-67 and p53 in gastrointestinal stromal tumors (GISTs) and its relationship with histopathological parameters.
METHODS: Twenty-five GISTs were examined by light microscopy and immunohistochemistry. c-kit, CD34, SMA, S-100 protein, COX-2, PCNA, Ki-67 and p53 were detected immunohistochemically and the relationship was evaluated among histopathologic parameters such as mitotic index (MI), tumor grade, tumor size, COX-2, PCNA, Ki-67 and p53.
RESULTS: COX-2 protein expression was found in 19 of 25 (76%) of the tumors, and expression was noted in the cytoplasm of the tumor cells. p53 was significantly related to MI and tumor grade but no relationship was found between COX-2, proliferation markers and MI, tumor grade and tumor size.
CONCLUSION: COX-2 is expressed in most GISTs and it may play an important role in the proliferation and progression of these tumors or a useful marker to identify GIST. Although immunohistochemical assessment of p53 can be used for distinguishing the risk groups of GISTs, tumor size and mitotic rate should be considered at the same time.
Keywords: Gastrointestinal stromal tumor, Cyclooxygenase-2, Proliferating cell nuclear antigen, Ki-67, p53, Immunohistochemistry
INTRODUCTION
Gastrointestinal stromal tumors (GISTs) are specific mesenchymal tumors of gastrointestinal tract (GI) that may occur in the entire length of GI tract from the esophagus to the anus[1]. Its histopathological origin has recently been suggested to be the intertistial cells of Cajal (ICC)[2]. For the majority of GISTs, it may be very difficult or impossible to determine the presence of any specific line of differentiation histologically. Tumors showing partial or incomplete myogenic, neural or myenteric ganglionic features may present virtually identical features under light microscopy[3].
However, immunohistochemistry of GISTs yields a diverse and confusing array of data, the antibodies most commonly used to characterize GISTs are those direct against vimentin, desmin, muscle spesific actin (MSA), smooth muscle actin (SMA), S-100 protein, neurofilament (NF), neurone spesific enolase (NSE), PGP9.5, CD34 and CD117 (c-kit). The myogenic markers MSA and SMA are variably expressed, whereas desmin is almost never present. Furthermore, MSA and SMA are generally only focally present or completely absent, indicating that most smooth muscle differentiation is incomplete. A possible schwannian/neural differentiation (S-100 protein, PGP9.5 and NSE positivity) may be present in a proportion of SMA and MSA negative tumors, both myogenic and schwannian/neural differentiation in a small proportion of tumors, whereas a small number of GISTs were positive for vimentin only and exhibited no detectable differentiation immunohistochemically[1-4].
The results of recent molecular pathologic studies that most GISTs are immunoreactive for CD34, a hematopoietic progenitor cell antigen, and CD117, c-kit proto-oncogen protein, as well as the gain of function c-kit gene mutations cause pathologic activation of the tyrosine kinase of c-kit in GISTs, seem to support the concept of GISTs as a biologically distinct entity[5,6].
The cyclooxygenase (COX) isoenzymes, COX-1 and COX-2 catalyze in the oxidation of arachidonic acid to prostaglandins, prostacyclin and tromboxanes and are inhibited by aspirin and non-steroidal anti-inflammatory drugs (NSAIDs)[7]. COX-1 is constitutively expressed in most normal tissues; COX-2 is induced by cytokines, mitogenic agents, and growth factors, and it produces inflammation and cell growth. Up-regulation of this enzyme in vitro has several tumorigenic effects such as induction of cell cycle arrest, resistance to apoptosis, increased cell growth, and stimulation of mitogenesis[7-8]. Recent studies have shown that COX-2 expression is elevated in gastrointestinal carcinomas but little is known about COX-2 expression in GISTs[9-11].
Multiple histological parameters such as mitosis, tumor size, cellularity, necrosis and pleomorphism have been used to predict the biological behavior of GISTs with limited success[2,12]. The proliferation markers Ki-67 and PCNA and tumor suppressor gene p53 have been reported as prognostic markers in many tumors, but only a few such studies have been reported in GISTs[2].
In this study, we used CD34, SMA and S-100 for differentiation of GISTs and investigated the expression of COX-2 in an attempt to correlate histopathologic parameters such as mitotic index (MI), tumor grade and tumor size and COX-2, proliferating cell nuclear antigen (PCNA), Ki-67 and p53.
MATERIALS AND METHODS
Formalin-fixed, paraffin-embedded tissue sections from 25 primary GISTs were obtained from the files of the Faculty of Medicine, Cukurova University, and Department of Pathology, Baskent University Adana Resarch and Practice Hospital. The material consisted of 11 gastric, 11 small intestinal, and 3 large intestinal tumors. The GIST cases were re-evaluated to confirm the diagnosis, and choose appropriate blocks of paraffin-embedded tissue for immunohistochemical analysis. Clinical information, including tumor size, was obtained from the surgical and pathological records. The tumors were reclassified as very low risk, low risk, intermediate risk and high risk according to MI (mitotic figures per 50 high-power fields; HPF) and tumor size (Table 1)[13].
Table 1.
Risk categories in GISTs
| Size | Mitotic count | |
| Very low risk | < 2 cm | < 5/50 HPF |
| Low risk | 2-5 cm | < 5/50 HPF |
| Intermediate risk | < 5 cm | 6-10/50 HPF |
| 5-10 cm | < 5/50 HPF | |
| High risk | > 5 cm | > 5/50 HPF |
| > 10 cm | Any mitotic rate | |
| Any size | > 10/50 HPF |
Immunohistochemical analysis
Immunohistochemistry was performed using a strept avidin-biotin-peroxidese technique with antibodies to c-kit (CD117, monoclonal mouse antibody, Novacastra-dilution 1:30), CD34 (monoclonal mouse antibody, Dako-dilution 1:40), vimentin (monoclonal mouse antibody, Biogenex-dilution 1:100), SMA (monoclonal mouse antibody, Novacastra-dilution 1:50), S-100 protein (polyclonal rabbit antibody, Novacastra-dilution 1:200), COX-2 (polyclonal goat antibody, Santa Cruz-dilution 1:100), Ki-67 (polyclonal rabbit antibody, Dako-dilution 1:50), PCNA (monoclonal mouse antibody, Biogenex-dilution 1:25), p53 (monoclonal mouse antibody, Dako-dilution 1:60). A 5-μm thick sections of formalin-fixed, paraffin-embedded tissue samples were deparaffinized and rehydrated through a series of graded alcohols. Endogenous peroxidase activity was blocked by a 30-min incubation in 3% hydrogen peroxide-methanol solution and washed in phosphate-buffered saline (PBS). The slides were kept in citrate buffer for 5-10 min in a microwave oven, rinsed in PBS at room temperature and incubated for 20-30 min with A2 blocking serum (citrate buffer incubation was not performed for vimentin, and the sections were incubated with 0.1% trypsin for 30 min). After washing, the sections were incubated for 60-120 min with primary antibodies and incubated for 30 min with biotinylated horse anti-mouse IgG immunglobulin (Dako, K0675). The sections were incubated for 30 min with strept avidin peroxidase reagent and washed again. The immunoperoxidase was visualized with AEC (3 amino 9 ethyl carbazole), (Dako, AEC substrate K0696). The sections were counterstained with Mayer’s hematoxylin and then coverslipped.
Assessment of staining reactions
The cytoplasmic immunostaining for c-kit, vimentin, CD34, SMA, S-100 and COX-2, and nuclear staining for Ki-67, PCNA and p53 were considered as positive reaction. The following scoring system was used for Ki-67 and PCNA: score 0, not positive; score 1, positively stained nuclei in < 10% of the tumor cells; score 2, 10-50% positive; and score 3, > 50% positive. The following scoring system was used for p53 evaluation: 0, not positive; 1+, 1-25% positive; 2+, 25-50% positive; 3+, 50-75% positive and 4+, > 75% positive.
Statistical analysis
Chi-square test was used to analyse the relation between MI, tumor grade, tumor size and COX-2, Ki-67, PCNA and p53. A P value of < 0.05 was considered significant in difference. Statistical analyses were performed with SPSS version 10.0 (Chicago, USA).
RESULTS
Sixteen (64%) of 25 GIST cases were male and 9 (36%) were female. Their ages ranged from 38 to 81 with a mean age of 62.30 ± 11.18 years (male: 62.86 ± 10.97, female: 61.44 ± 12.12). Eleven (44%) of the tumors originated from stomach, 11 (44%) from small intestine and 3 (12%) from large intestine. The mean size of the tumor was 7.70 ± 3.62 cm, 10.0 ± 4.43 cm and 5.0 ± 1.73 cm and the mean mitotic index of the tumor was 5.60 ± 5.10, 11.0 ± 10.76 and 16.0 ± 7.21 in stomach, small intestine and large intestine, respectively. The tumors were classified as low risk (n = 3), intermediate risk (n = 6) and high risk (n = 16). Two of the low risk tumors were gastric and one was small intestinal. Four of the intermediate risk tumors were gastric and two were small intestinal tumors. Five of the high risk tumors were gastric, eight were small intestinal and three were large intestinal tumors. The clinicopathological data of the 25 patients with GIST are summarized in Table 2. The immunostaining results are listed in Table 3.
Table 2.
Clinicopathological features of 25 patients with GISTs
| Variables | Cases n (%) |
| Sex | |
| Male | 16 (64) |
| Female | 9 (36) |
| Site | |
| Stomach | 11 (44) |
| Small intestine | 11 (44) |
| Large intestine | 3 (12) |
| Tumor size (cm) | |
| < 2 cm | 0 (0) |
| 2-5 cm | 4 (16) |
| 5-10 cm | 16 (64) |
| > 10 cm | 5 (20) |
| Mitosis | |
| < 5 | 11 (44) |
| ≥ 5 | 14 (56) |
| Diagnosis | |
| Very low risk | 0 (0) |
| Low risk | 3 (12) |
| Intermediate risk | 6 (24) |
| High risk | 16 (64) |
Table 3.
Immunostaining results of 25 cases of GISTs
| Site of origin | c-kit | COX-2 | CD34 | SMA + | SMA + | SMA - | SMA - |
| + | + | + | S-100 + | S-100 - | S-100 + | S-100 - | |
| Stomach (n = 11) | |||||||
| Low risk | 2 | 1 | 2 | - | - | 1 | 1 |
| Intermediate risk | 4 | 4 | 3 | - | - | 2 | 2 |
| High risk | 5 | 3 | 4 | 2 | - | 1 | 2 |
| Small intestine | |||||||
| (n = 11) | |||||||
| Low risk | 1 | 1 | 1 | - | 1 | - | - |
| Intermediate risk | 2 | 1 | 2 | 1 | - | 1 | - |
| High risk | 7 | 6 | 6 | 2 | 2 | 4 | - |
| Large intestine | |||||||
| (n = 3) | |||||||
| High risk | 2 | 3 | 3 | 2 | - | - | 1 |
| Total n (%) | 23 (92) | 19 (76) | 21 (84) | 7 (28) | 3 (12) | 9 (36) | 6 (24) |
All 25 cases of GIST were positive for vimentin. Twenty-three (92%) tumors were positive for c-kit. Only one small intestinal and one large intestinal tumors were negative for c-kit but these tumors showed positive reactivity with CD34. There was diffuse cytoplasmic staining for both c-kit and CD34. CD34 reactivity was found in 21(84%) tumors. Two gastric and two small intestinal tumors were negative for CD34. Ten (40%) tumors were positive for SMA. There was focal cytoplasmic staining for SMA. The frequency of SMA reactivity was higher in the nonstomach tumors (6 in small intestine and 2 in large intestine). S-100 reactivity was found in 16 tumors (6 in stomach, 8 in small intestine and 2 in large intestine). There was focal staining for S-100. Both SMA and S-100 reactivity were found in 5 intestinal tumors while they were found only in 2 gastric tumors. In contrast, 5 gastric tumors were negative for SMA and S-100 while only one intestinal tumor was negative.
COX-2 immunostaining was found in 19 of 25 (76%) of the tumors (Figure 1). Three gastric and three small intestinal tumors were negative for COX-2. In the stomach, two high risk and only one low risk tumor were negative. In the small intestine, two high risk and one intermediate risk tumors showed negative staining with COX-2 (Table 3).
Figure 1.
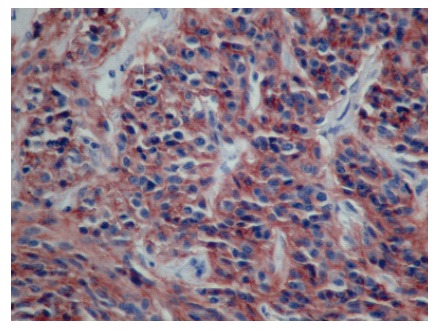
Diffuse cytoplasmic staining of COX-2 in the tumor cells of GIST.
PCNA index was high in most cases; score 3 was found in 18 (72%) tumors; and score 2 in 5 (20%) (Figure 2). Only one case was negative for PCNA. Based on Ki-67 index, score 0 was assigned to 9 (36%) tumors; score 1, to 10 (40%); score 2, to 5 (20%); and score 3, to only one (4%) (Figure 3).
Figure 2.
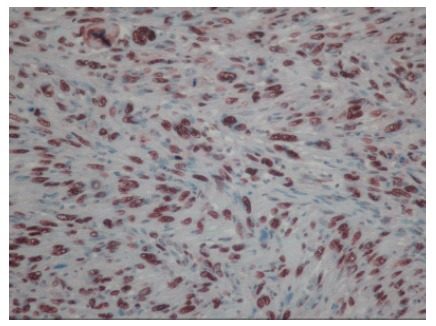
High PCNA immunoreactivity in GIST with more than 50% of nuclear positivity.
Figure 3.
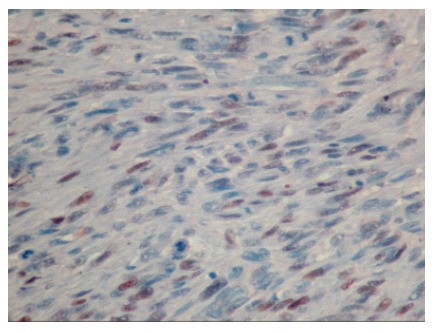
Low Ki-67 immunoreactivity in GIST with less than 50% of nuclear positivity.
p53 was positive in 18 (72%) tumors whereas it was negative in 7 (28%) (Figure 4). Immunostaining results for p53 are shown in Table 4.
Figure 4.
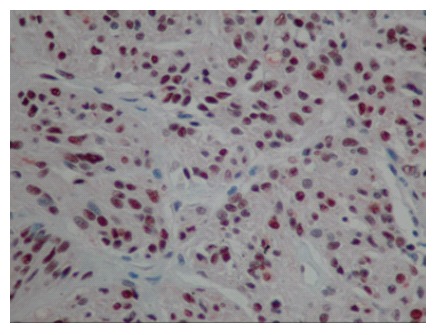
High p53 immunoreactivity in GIST with more than 75% of nuclear positivity.
Table 4.
The results of immunohistochemical staining for p53
| p53 index | 0 | 1 | 2 | 3 | 4 |
| Low risk | 1 | 1 | 1 | 0 | 0 |
| Intermediate risk | 0 | 2 | 1 | 1 | 2 |
| High risk | 6 | 6 | 2 | 2 | 0 |
| Total | 7 | 9 | 4 | 3 | 2 |
Follow-up information was available in 13 cases. Four patients died in early postoperative period (4-21 d). Two patients died 18-24 mo after diagnosis. Seven patients are alive 36-12 mo after diagnosis.
Statistically, p53 was related to MI and tumor risk groups (P < 0.05). Although p53 score was markedly high in cases with tumor size > 5 cm in diameter, it was statistically insignificant (P = 0.05). There was no relationship between COX-2, proliferation markers (PCNA, Ki-67) and MI, tumor risk groups and tumor size (P > 0.05).
DISCUSSION
GISTs differ from true leiomyomas, leiomyosarcomas and schwannomas, and their histological origin has recently been suggested to be the ICC. These cells are located between the muscular layers of gastric and intestinal wall associated with the myenteric plexus which are thought to play a role incoordinating intestinal motility. Ultrastructurally, they show both incomplete myogenic and neural differentiation and characterized by dual immunopositivity for CD34 and CD117[4,13]. It is also accepted that the term ‘‘GIST’’ should apply only to neoplasms expressing CD117 with only very rare exceptions. The majority of studies have demonstrated that immunoreactivity for CD34 is seen in 60%-80% of cases[6,13,14].
Beside consistent positivity for CD117 and CD34, 30%-40% of GISTs show immunopositivity for SMA and usually 5%-10% and rarely up to 40% show immunopositivity for S-100 protein[3,13,15].
In our study, SMA positivity was seen most often in bowel tumors with a ratio of 40%. Some studies have showed a reciprocal relationship with CD34 expression and SMA positivity. Similarly, SMA negative tumors were often CD34 positive in our cases. Additionally, the percentage of S-100 protein reactivity was higher than most of the previous studies. Beside conflicting results in the literature this finding may represent autonomic nerve-like differentiation in a proportion of GISTs so that the relationship between GAN and GISTs can not be ignored. Also, a significant number of gastric tumors were negative for SMA and S-100 protein while most of bowel tumors had showed S-100 protein and/or SMA positivity.
Overexpression of COX-2 has been reported in various types of gastrointestinal carcinomas[9-11]. COX-2 is located in tumor-derived epithelial cells of colonic adenocarcinomas, whereas it is found in stroma cells in tissues of colonic adenoma and colorectal carcinoma[9,16]. In addition, COX-2 is also located in interstitial cells of colonic adenomatous polyps[17-19]. These discrepant findings should be sorted out to determine the role of COX-2 in not only carcinogenesis but also tumor growth and progression of human carcinomas in terms of epithelial-stromal interactions[8]. Asano et al[8] showed that the expression of COX-2 in gallbladder carcinoma was increased in parallel to the depth of invasion. Sheehan et al[7] described for the first time the expression of COX-2 in GISTs, and demonstrated COX-2 protein expression in 12 of 15 (80%) of the tumors. Stewart et al[20] showed COX-2 protein expression in 35 of 38 (92%) GISTs and indicated that COX-2 may be useful as an additional molecular marker to aid in the identification of GIST, particularly in those cases with epithelioid histology or where KIT is only weakly or focally positive. Epidemiologic data suggest that the treatment with aspirin and NSAIDs prevents colorectal cancer and reduces the size and number of corectal polyps[21,22]. There is no evidence of inhibitory effect of aspirin or NSAIDs in GISTs but treatment with COX inhibitors as adjuvant therapy may be beneficial.
There are many parameters for distinguishing benign from malignant GISTs such as MI, tumor size, cellularity, necrosis, mucosal invasion. MI and tumor size are the most reasonable and replicable parameters[13,23]. Other parameters have been studied to evaluate GISTs behaviors, including immunohistochemical markers of cell proliferation (e.g., Ki-67, MIB-1, PCNA), flow cytometry, image analysis, telomerase activity and assessment of nucleolar organizer regions[13,24].
There are controversies about prognostic impact of PCNA[25-28]. Ray and et al[25] demonstrated that PCNA index was correlated with necrosis, high grade atypia, cellularity and mitotic rate. In contrast, Sbasching et al[27] did not find a correlation of PCNA expression with survival in GIST. More recently, Ki-67 analogues have replaced PCNA because PCNA index is instable due to variations in antigen preservation and recovery[29]. Seidal et al[30] studied 31 cases of GIST and found a correlation with Ki-67 and outcome of patients. Wang et al[2] showed that expression of Ki-67 was more frequently seen in malignant GISTs than in benign GISTs. Regarding p53 expression in GIST, only a few studies have been carried out, with conflicting results. Al-Bozom[23] evaluated p53 expression in 15 cases and concluded that p53 is usefull in distinguishing between benign and malignant GIST. In contrast, Lopes et al[31] studied 33 cases and did not find any correlation between p53 and behavior.
In our study, p53 was found to be related to MI and tumor grade (P < 0.05). Although p53 score was markedly high in the cases with tumor size > 5 cm in diameter, it was statistically insignificant (P = 0.05). We could not find any significant relationshiop between proliferation markers (PCNA, Ki-67), MI, tumor grade and tumor size (P > 0.05).
In conclusion, COX-2 is expressed in most GISTs and may play an important role in the proliferation and progression of these tumors or a useful marker to help identify GIST. Immunohistochemical assessment of p53 can be used for distinguishing the risk groups of GISTs but the best way to distinguish the risk groups of these tumors is thought to be the tumor size and mitotic rate. We found out that PCNA and Ki-67 are independent factors from MI, tumor grade and tumor size. Further studies to find additional prognostic parameters will provide valuable insights into the behavior of GISTs.
Footnotes
S- Editor Liu Y L- Editor Ma JY E- Editor Lu W
References
- 1.Miettinen M, Lasota J. Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001;438:1–12. doi: 10.1007/s004280000338. [DOI] [PubMed] [Google Scholar]
- 2.Wang X, Mori I, Tang W, Utsunomiya H, Nakamura M, Nakamura Y, Zhou G, Kakudo K. Gastrointestinal stromal tumors: clinicopathological study of Chinese cases. Pathol Int. 2001;51:701–706. doi: 10.1046/j.1440-1827.2001.01260.x. [DOI] [PubMed] [Google Scholar]
- 3.Suster S. Gastrointestinal stromal tumors. Semin Diagn Pathol. 1996;13:297–313. [PubMed] [Google Scholar]
- 4.Graadt van Roggen JF, van Velthuysen ML, Hogendoorn PC. The histopathological differential diagnosis of gastrointestinal stromal tumours. J Clin Pathol. 2001;54:96–102. doi: 10.1136/jcp.54.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hasegawa T, Matsuno Y, Shimoda T, Hirohashi S. Gastrointestinal stromal tumor: consistent CD117 immunostaining for diagnosis, and prognostic classification based on tumor size and MIB-1 grade. Hum Pathol. 2002;33:669–676. doi: 10.1053/hupa.2002.124116. [DOI] [PubMed] [Google Scholar]
- 6.Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumors: recent advances in understanding of their biology. Hum Pathol. 1999;30:1213–1220. doi: 10.1016/s0046-8177(99)90040-0. [DOI] [PubMed] [Google Scholar]
- 7.Sheehan KM, Sabah M, Cummins RJ, O'Grady A, Murray FE, Leader MB, Kay EW. Cyclooxygenase-2 expression in stromal tumors of the gastrointestinal tract. Hum Pathol. 2003;34:1242–1246. doi: 10.1016/j.humpath.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Asano T, Shoda J, Ueda T, Kawamoto T, Todoroki T, Shimonishi M, Tanabe T, Sugimoto Y, Ichikawa A, Mutoh M, et al. Expressions of cyclooxygenase-2 and prostaglandin E-receptors in carcinoma of the gallbladder: crucial role of arachidonate metabolism in tumor growth and progression. Clin Cancer Res. 2002;8:1157–1167. [PubMed] [Google Scholar]
- 9.Sano H, Kawahito Y, Wilder RL, Hashiramoto A, Mukai S, Asai K, Kimura S, Kato H, Kondo M, Hla T. Expression of cyclooxygenase-1 and -2 in human colorectal cancer. Cancer Res. 1995;55:3785–3789. [PubMed] [Google Scholar]
- 10.Tsujii M, Kawano S, DuBois RN. Cyclooxygenase-2 expression in human colon cancer cells increases metastatic potential. Proc Natl Acad Sci USA. 1997;94:3336–3340. doi: 10.1073/pnas.94.7.3336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fujita T, Matsui M, Takaku K, Uetake H, Ichikawa W, Taketo MM, Sugihara K. Size- and invasion-dependent increase in cyclooxygenase 2 levels in human colorectal carcinomas. Cancer Res. 1998;58:4823–4826. [PubMed] [Google Scholar]
- 12.Basson MD, Modlin IM, Flynn SD. Current clinical and pathologic perspectives on gastric stromal tumors. Surg Gynecol Obstet. 1992;175:477–489. [PubMed] [Google Scholar]
- 13.Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti H, Rubin BP, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459–465. doi: 10.1053/hupa.2002.123545. [DOI] [PubMed] [Google Scholar]
- 14.Berman J, O'Leary TJ. Gastrointestinal stromal tumor workshop. Hum Pathol. 2001;32:578–582. doi: 10.1053/hupa.2001.25484. [DOI] [PubMed] [Google Scholar]
- 15.Miettinen M. Gastrointestinal stromal tumors. An immunohistochemical study of cellular differentiation. Am J Clin Pathol. 1988;89:601–610. doi: 10.1093/ajcp/89.5.601. [DOI] [PubMed] [Google Scholar]
- 16.Bamba H, Ota S, Kato A, Adachi A, Itoyama S, Matsuzaki F. High expression of cyclooxygenase-2 in macrophages of human colonic adenoma. Int J Cancer. 1999;83:470–475. doi: 10.1002/(sici)1097-0215(19991112)83:4<470::aid-ijc6>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 17.Oshima M, Dinchuk JE, Kargman SL, Oshima H, Hancock B, Kwong E, Trzaskos JM, Evans JF, Taketo MM. Suppression of intestinal polyposis in Apc delta716 knockout mice by inhibition of cyclooxygenase 2 (COX-2) Cell. 1996;87:803–809. doi: 10.1016/s0092-8674(00)81988-1. [DOI] [PubMed] [Google Scholar]
- 18.Hull MA, Booth JK, Tisbury A, Scott N, Bonifer C, Markham AF, Coletta PL. Cyclooxygenase 2 is up-regulated and localized to macrophages in the intestine of Min mice. Br J Cancer. 1999;79:1399–1405. doi: 10.1038/sj.bjc.6690224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shattuck-Brandt RL, Varilek GW, Radhika A, Yang F, Washington MK, DuBois RN. Cyclooxygenase 2 expression is increased in the stroma of colon carcinomas from IL-10(-/-) mice. Gastroenterology. 2000;118:337–345. doi: 10.1016/s0016-5085(00)70216-2. [DOI] [PubMed] [Google Scholar]
- 20.Stewart AE, Heslin MH, Arch J, Jhala N, Ragland B, Gomez F, Bland KI, Arnoletti JP. Cyclooxygenase-2 expression and clinical outcome in gastrointestinal stromal tumors. J Gastrointest Surg. 2006;10:315–319. doi: 10.1016/j.gassur.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Thun MJ, Namboodiri MM, Calle EE, Flanders WD, Heath CW. Aspirin use and risk of fatal cancer. Cancer Res. 1993;53:1322–1327. [PubMed] [Google Scholar]
- 22.Steinbach G, Lynch PM, Phillips RK, Wallace MH, Hawk E, Gordon GB, Wakabayashi N, Saunders B, Shen Y, Fujimura T, et al. The effect of celecoxib, a cyclooxygenase-2 inhibitor, in familial adenomatous polyposis. N Engl J Med. 2000;342:1946–1952. doi: 10.1056/NEJM200006293422603. [DOI] [PubMed] [Google Scholar]
- 23.Al-Bozom IA. p53 expression in gastrointestinal stromal tumors. Pathol Int. 2001;51:519–523. doi: 10.1046/j.1440-1827.2001.01233.x. [DOI] [PubMed] [Google Scholar]
- 24.Sakurai S, Fukayama M, Kaizaki Y, Saito K, Kanazawa K, Kitamura M, Iwasaki Y, Hishima T, Hayashi Y, Koike M. Telomerase activity in gastrointestinal stromal tumors. Cancer. 1998;83:2060–2066. doi: 10.1002/(sici)1097-0142(19981115)83:10<2060::aid-cncr3>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 25.Ray R, Tahan SR, Andrews C, Goldman H. Stromal tumors of the stomach: prognostic value of the PCNA index. Mod Pathol. 1994;7:26–30. [PubMed] [Google Scholar]
- 26.Amin MB, Ma CK, Linden MD, Kubus JJ, Zarbo RJ. Prognostic value of proliferating cell nuclear antigen index in gastric stromal tumors. Correlation with mitotic count and clinical outcome. Am J Clin Pathol. 1993;100:428–432. doi: 10.1093/ajcp/100.4.428. [DOI] [PubMed] [Google Scholar]
- 27.Sbaschnig RJ, Cunningham RE, Sobin LH, O'Leary TJ. Proliferating-cell nuclear antigen immunocytochemistry in the evaluation of gastrointestinal smooth-muscle tumors. Mod Pathol. 1994;7:780–783. [PubMed] [Google Scholar]
- 28.Shirai H, Takeuchi T, Naka T, Minaghi S, Kimura A, Hamazaki S, Ito H. Gastrointestinal stromal tumor of the stomach: report of a case. Surg Today. 2001;31:346–349. doi: 10.1007/s005950170158. [DOI] [PubMed] [Google Scholar]
- 29.Carrillo R, Candia A, Rodriguez-Peralto JL, Caz V. Prognostic significance of DNA ploidy and proliferative index (MIB-1 index) in gastrointestinal stromal tumors. Hum Pathol. 1997;28:160–165. doi: 10.1016/s0046-8177(97)90100-3. [DOI] [PubMed] [Google Scholar]
- 30.Seidal T, Edvardsson H. Expression of c-kit (CD117) and Ki67 provides information about the possible cell of origin and clinical course of gastrointestinal stromal tumours. Histopathology. 1999;34:416–424. doi: 10.1046/j.1365-2559.1999.00643.x. [DOI] [PubMed] [Google Scholar]
- 31.Lopes JM, Silva P, Seixas M, Cirnes L, Seruca R. Microsatellite instability is not associated with degree of malignancy and p53 expression of gastrointestinal stromal tumours. Histopathology. 1998;33:579–581. doi: 10.1046/j.1365-2559.1998.0525d.x. [DOI] [PubMed] [Google Scholar]


