Abstract
Isolated pancreatic tuberculosis is an extremely rare condition, more so in an immunocompetent individual. Its presentation as pancreatic abscesses with colonic perforation has not been reported so far. This condition poses difficulties in clinical diagnoses. Herein we report a case who was operated in another hospital for pancreatic abscesses, and referred to our institution later when he developed fecal peritonitis due to colonic perforation. Re-laparotomy, resection and exteriorisation of the colon were done. Acid fast bacilli was seen in the histopathological examination of the resected colon. The patient responded remarkably to anti-tuberculous therapy and two sittings of debridement. Post procedure the patient developed pancreatic fistula, which was managed successfully with stenting. Pancreatic tuberculosis should be considered as a differential diagnosis when pancreatitis is atypical.
Keywords: Pancreas, Tuberculosis, Acute pancreatitis, Pancreatic abscess, Colonic perforation
INTRODUCTION
Tuberculosis (TB) of the abdomen is seen in 12% of patients with miliary TB[1]. Isolated involvement of the pancreas without military TB or immunocompromised status is extremely rare. In view of the non-specific clinical presentation, the disease can elude a diagnosis, but once diagnosed it responds favourably to anti-tuberculous therapies (ATT).
CASE REPORT
A 28-year-old male patient was admitted to the casualty department with suspected fecal peritonitis 10 d after having undergone a laparotomy and drainage for pancreatic abscesses at another hospital. He was put on continuous peritoneal lavage. The patient had a history of vague back pain for the past 6 mo. The diagnosis was based on a CT scan as he presented with an unexplained and non-responding fever. CT showed multiple hypodense well defined lesions behind the pancreas (Figure 1).
Figure 1.
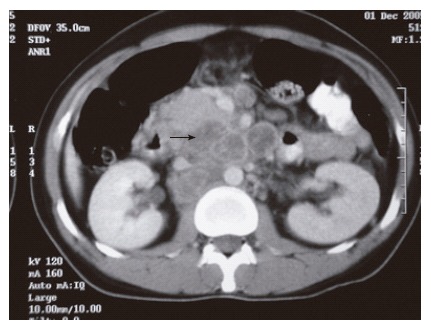
Low density area within lymph node.
On admission to our institution, the patient was in a state of severe sepsis with ventilator and hemodynamic support. His abdomen was distended and there was feculent discharge from the main wound and drain. The patient underwent an exploratory laparotomy, which revealed 1 L of purulent fluid and two perforations in the transverse colon. The pancreas appeared edematous and collections of pus were found behind the head of the pancreas. Limited segmental excision of the colon, peritoneal lavage, proximal colostomy and end mucous fistula were done. The patient was managed in the intensive care unit (ICU) in the post-operative period. The patient continued to be in sepsis and was performed a re-exploration, lavage, and laparotomy.
Histopathological examinations (HPE) revealed acid fast bacilli (AFB) (Figure 2) in the specimen of the serosal side of the colon and hence the patient was started on streptomycin/izoniazid/rifampicin/ethambutol. The patient recovered well in the post operative period except for increased pancreatic fluid in the drain tube (71 318 IU/L). The ERCP showed pancreatic ductal disruption and a normal biliary tree. Pancreatic stenting was done. Two days later he was operated for the wound closure. The patient improved with ATT/antibiotics/octreotide/ionotropes and nutritional support and was discharged after two weeks. He has improved and gained weight on follow up. A colostomy closure is planned as he has recovered completely.
Figure 2.
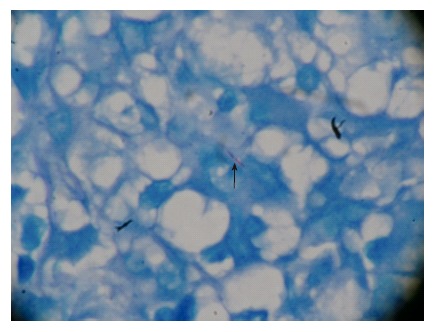
Acid fast bacilli.
DISCUSSION
TB of the pancreas is a rare disease and the incidence has been reported to be around 0%-4.7%[2,3]. So far 38 cases of TB of the pancreas were reviewed in a report published in 2000[4] and many more case reports have been published. Various modes of presentation have been reported including pancreatic abscesses[5], acute or chronic pancreatitis, gastrointestinal (GI) bleeding, obstructive jaundice, portal vein obstruction and pancreatic mass mimicking malignancy. Our case is an extremely rare presentation with pancreatic abscesses and colonic perforation. The patient did not have a personal or family history of TB and was immunocompetent with no evidence of any other foci of TB.
Infection is said to involve the pancreas by direct extension, lymphohematogenous dissemination or following reactivation of previous abdominal TB[5,6]. Contrast enhanced CT (CECT) scans may demonstrate a focal hypodense mass, diffuse enlargement of the pancreas, but none of the signs are pathognomonic. Ring enhancement or low-density areas within enlarged lymph nodes should make one suspect tuberculous lymph nodes[7].
In the case we have reported the diagnosis of TB was a surprise and was revealed on HPE of the biopsy specimen obtained at a laparotomy[5], the demonstration of AFB is even more rare as most of the abdominal tuberculosis are paucibacillary. Percutaneous image guided fine needle aspiration of suspicious lesions might suggest the diagnosis of tuberculosis, thereby obviating the need for a diagnostic laparotomy[5].
The presence of caseating granulomatous inflammation is the commonest finding on HPE. In almost half of the patients with extra pulmonary TB, Ziehl Neelson staining for AFB and prolonged culture for mycobacterium tuberculosis has been found negative[8]. Very few are diagnosed by FNA/BIOPSY[5-10]. Once the diagnosis has been established, the majority of patients with tuberculosis respond favourably to ATT[5].
In view of the nonspecific clinical presentation and absence of pathognomonic features on imaging studies, the physician should be alert and have a high index of suspicion, particularly when dealing with young patients, coming from endemic areas with a short duration of symptoms of common pancreatic diseases.
Footnotes
S- Editor Wang GP L- Editor Zhu LH E- Editor Bi L
References
- 1.Haddad FS, Ghossain A, Sawaya E, Nelson AR. Abdominal tuberculosis. Dis Colon Rectum. 1987;30:724–735. doi: 10.1007/BF02561699. [DOI] [PubMed] [Google Scholar]
- 2.Bhansali SK. Abdominal tuberculosis. Experiences with 300 cases. Am J Gastroenterol. 1977;67:324–337. [PubMed] [Google Scholar]
- 3.Auerbach O. Acute Generalized Miliary Tuberculosis. Am J Pathol. 1944;20:121–136. [PMC free article] [PubMed] [Google Scholar]
- 4.Evans JD, Hamanaka Y, Olliff SP, Neoptolemos JP. Tuberculosis of the pancreas presenting as metastatic pancreatic carcinoma. A case report and review of the literature. Dig Surg. 2000;17:183–187. doi: 10.1159/000018828. [DOI] [PubMed] [Google Scholar]
- 5.Stambler JB, Klibaner MI, Bliss CM, LaMont JT. Tuberculous abscess of the pancreas. Gastroenterology. 1982;83:922–925. [PubMed] [Google Scholar]
- 6.Stock KP, Riemann JF, Stadler W, Rösch W. Tuberculosis of the pancreas. Endoscopy. 1981;13:178–180. doi: 10.1055/s-2007-1021678. [DOI] [PubMed] [Google Scholar]
- 7.Hulnick DH, Megibow AJ, Naidich DP, Hilton S, Cho KC, Balthazar EJ. Abdominal tuberculosis: CT evaluation. Radiology. 1985;157:199–204. doi: 10.1148/radiology.157.1.4034967. [DOI] [PubMed] [Google Scholar]
- 8.Farer LS, Lowell AM, Meador MP. Extrapulmonary tuberculosis in the United States. Am J Epidemiol. 1979;109:205–217. doi: 10.1093/oxfordjournals.aje.a112675. [DOI] [PubMed] [Google Scholar]
- 9.Addison NV. Abdominal tuberculosis--a disease revived. Ann R Coll Surg Engl. 1983;65:105–111. [PMC free article] [PubMed] [Google Scholar]
- 10.Khoury GA, Payne CR, Harvey DR. Tuberculosis of the peritoneal cavity. Br J Surg. 1978;65:808–811. doi: 10.1002/bjs.1800651113. [DOI] [PubMed] [Google Scholar]


