Abstract
Context
The complex anatomy and the importance of ligaments in providing stability at the upper cervical spine region (O–C1–C2) require the use of many imaging modalities to evaluate upper cervical injuries (UCI). While separate classifications have been developed for distinct injuries, a more practical treatment algorithm can be derived from the injury pattern in UCI.
Objective
To propose a practical treatment algorithm to guide treatment based on injuries characteristic of UCI.
Methods
A literature review was performed on the Pubmed database using the following keywords: (1) “occipital condyle injury”; (2) “craniocervical dislocation or atlanto-occipital dislocation or craniocervical dislocation”; (3) “atlas fractures”; and (4) “axis fractures”. Just articles containing the diagnosis, classification, and treatment of specific UCI were included. The data obtained were analyzed by the authors, dividing the UCI into two groups: Group 1 – patients with clear ligamentous injury and Group 2 – patients with fractures without ligament disruption.
Results
Injuries with ligamentous disruption, suggesting surgical treatment, include: atlanto-occipital dislocation, mid-substance transverse ligament injury, and C1–2 and C2–3 ligamentous injuries. In contrast, condyle, atlas, and axis fractures without significant displacement/misalignment can be initially treated using external orthoses. Odontoid fractures with risk factors for non-union are an exception in Group 2 once they are better treated surgically. Patients with neurological deficits may have more unstable injuries.
Conclusions
Ascertaining the status of relevant ligamentous structures, fracture patterns and alignment are important in determining surgical compared with non-surgical treatment for patients with UCI.
Keywords: Upper cervical spine, Traumatic, Injury, Management, Treatment, Classification
Introduction
Upper cervical injuries (UCI) consist of a diverse group of injuries that affect the skull base, the atlas, and the axis and are generally associated with high-energy trauma.1 This group of injuries has several unique features that distinguish it from the subaxial cervical spine: (i) a complex bony and vascular anatomy, (ii) the relationship of the atlas and axis with the cranial base, and (iii) that the intrinsic stability of this region relies heavily on ligamentous structures. Moreover, the majority of axial rotation of the cervical spine occurs at the atlantoaxial complex and may be compromised after a traumatic event resulting in spinal instability.1 In addition, even though flexion and extension are more widely distributed throughout the entire cervical spine, the occiput–C1 joint is the level with greatest range of motion in this plane also making it vulnerable to instability after a traumatic event.2
When considering the diagnostic tools in the workup of the upper cervical spine trauma, conventional X-rays may be insufficient to diagnose an injury in this region. Computed tomography (CT) with coronal and sagittal multi-planar reconstructions allows for precise measurement and quantification of the complex relationships between anatomical landmarks, thereby establishing the diagnosis of UCI.3–5 In many cases, magnetic resonance imaging (MRI) may also be necessary to evaluate spinal cord or brainstem injury as well as the integrity of the intervertebral disk, the ligamentous structures, and the facet joints.3–5 A detailed radiological description of craniocervical traumatic injuries is given elsewhere.6–8
Many separate classification schemes have been developed for each of the distinct anatomical components of the occiput–C1–C2 complex: Anderson and D'Alonzo (fractures of the odontoid process), Traynelis (atlanto-occipital dislocations (AODs)), and Effendi (fractures of the ring of the axis), among many others.9–11 There are major drawbacks in these schemes, including a high level of complexity to the schemes themselves, and no unifying theme to the varied classification. The complex upper cervical anatomy and the wide range of injury patterns have, on the other hand, created a fractionated approach to the classification of upper cervical trauma. The lack of a unifying classification system has, furthermore, prevented development of an objective approach to guide treatment decisions.12
A more objective unified approach may be possible with consideration of the unique anatomical properties of the O–C1–C2 complex. The role of the ligamentous complex to maintain stability, prevent deformity, and protect neurological function is of paramount importance. Ligamentous injury is probably the most important factor in guiding the decision for surgical treatment of UCI. In this paper, we present a literature review of the UCI, grouping the studies according to factors that can guide the treatment decisions.
Methods
We performed a literature review of the main UCI. The following injuries were included: AOD, transverse-ligament (TL) injuries, occipital condyle, atlas, and axis fractures (including odontoid, traumatic spondylolisthesis, and axis body fractures). The literature search was performed on the Pubmed database. The following keywords were used: “occipital condyle injury”; “craniocervical dislocation or AOD or craniocervical dislocation”; “atlas fractures”; and “axis fractures”. We included English language articles, published before 2012. We excluded case reports, surgical techniques, and literature reviews. We selected studies that clearly defined the diagnosis, classification, and treatment of specific UCI, according to the purpose of our review. The data obtained were then reviewed and analyzed by the authors, grouping patients with UCI in two groups, based on the importance of ligamentous complex injury to guide the decision for surgical treatment: Group 1 (patients with clear ligamentous injury, with or without fractures), and Group 2 (patients with fractures without clear ligament disruption).
Based on this information, a critical evaluation was performed and a rational approach was proposed to guide surgical treatment, with clinical examples to illustrate its use.
There was no external funding source for this study and the funding sources did not play a role in the investigation.
Results
Group 1 – Patients with clear ligamentous injury (with or without fractures)
Definitive ligamentous injury can be inferred by abnormal spinal misalignment, outside of the normative ranges of alignment involving the following articulations: occipital condyle–C1, C1–2, or subaxial vertebral facet joints, seen with distraction or rotational injuries.3,4,12 Perched or locked cervical facet joints and an increase in the atlanto-dens interval of more than 3.5 mm are examples of ligamentous instabilities that may be detected with CT imaging, MRI, or dynamic plain radiography.3,4,12 Three injuries patterns were included in this group: (1) AOD (with or without concomitant atlantoaxial instability), (2) TL injured intra-substance (with or without atlas ring fracture), and (3) C2–3 ligamentous injuries (generally in the context of fractures of the posterior elements of the axis).
Atlanto-occipital dislocation
The diagnosis of AOD can be made based on an increasing of the occipital condyle–C1 lateral masses interval, as proposed by Pang et al.,13,14 measured at CT scan reconstructions. Radiologically, AOD can have a combination of anterior, vertical, or posterior dislocation (respectively, classified as type 1, 2, and 3, according to Traynelis et al.; Table 1), although this may be of minimal significance, since the position of the dislocation can vary with changing patient positioning.10,15 AOD may be associated with occipital condyle fractures (OCFs).16 Treatment of this highly unstable injury pattern includes occipito-cervical fixation with an arthrodesis.3,4,12 Without treatment, patients are at high risk for progressive neurological worsening.12,16
Table 1 .
AOD – types of injuries according to Traynelis et al.
| Type | Description | Morphology |
|---|---|---|
| 1 | Anterior displacement of the occiput with respect to atlas |  |
| 2 | Longitudinal distraction |  |
| 3 | Posterior displacement of the occiput on the atlas |  |
As a general conclusion, all patients diagnosed with AOD should be surgically stabilized.7,10,17 Atlantoaxial dislocation can be found together with AOD or in isolation and should also be treated surgically (Fig. 1).10
Figure 1 .

This 22-year-old woman presented to the emergency department after a severe car accident. She had an atlantoaxial dislocation with bilateral condilar fractures, as seen in sagittal (A and B) and coronal (C) reconstructions. Clear ligamentous injury could be inferred based on the CT findings and an occipito-C2–3 instrumentation and fusion was performed (D, E, and F).
TL injured intra-substance
When the TL sustains an intra-substance injury, with or without a C1 ring fracture, surgical stabilization of C1–2 is recommended because of subsequent instability (see Table 2 – types of TL according to Dickman et al.18). Diagnosis of a TL injury can be based on measurement of the atlanto-dens interval (>3.5 mm), lateral displacement of the lateral mass of the atlas greater than 6.9 mm (the “rule of Spence”), or with CT and MRI imaging, probably the gold standard.18,19 This injury requires surgical stabilization of C1–2 to restore spinal stability (Fig. 2).17
Table 2 .
Transverse atlantal ligament – types of injuries according to Dickman et al.
| Type | Description | Morphology |
|---|---|---|
| 1 | Disruption of the substance of the ligament |  |
| 2 | Fractures and avulsions involving the tubercle insertion of the TL on the C1 lateral mass | 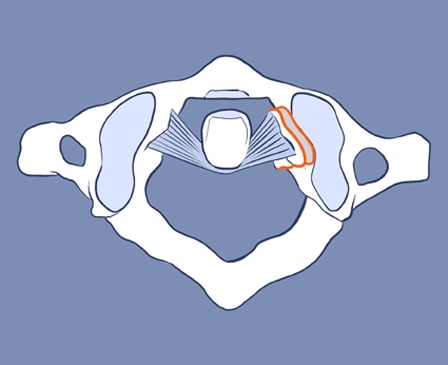 |
Figure 2 .

This patient is a 50-year-old man who presented to the emergency department after a car accident with severe neck pain and no bone fractures. Cervical lateral radiograph in flexion showed a 5 mm atlanto-dens interval distance (A) with total reduction in extension (B). A diagnosis of TL injury in its substance was established, since there is no fracture in its points of insertion at C1, as shown in this axial CT scan of the atlas (C). Based on our algorithm, ligament injury in the craniocervical spine leads to surgical intervention. A C1–2 fusion (D) was performed as shown in this cervical lateral radiograph and the patient was doing well.
C2–3 ligamentous injuries
For traumatic spondylolisthesis of the axis (also known as Hangman's fracture or fractures of the par interarticularis), a number of classification systems have been reported in the literature including those of Pepin and Hawkins, Francis, Effendi, and Levine Edwards.11,20,21 These classifications are based on the involvement of the body, degree of angulation/displacement, and the mechanism of injury. Table 3 illustrated the classification proposed by Levine and Edwards.21 The literature suggests that most patients with these injuries can be successfully treated with external immobilization.12 Recommendations for surgery are typically reserved for fractures with disruption of the C2–3 disk space (Effendi Type III) and locked facets (with unilateral or bilateral locked facets, as in the Effendi type 3 and Levine Edwards's type 3 fractures). The recommendation for surgery (C2–3 stabilization) in such cases are consequent to disruption of the disk or ligamentous structures between C2 and C3 that cannot heal with immobilization alone.11,21
Table 3 .
Fracture of the posterior elements of the axis according to Levine and Edwards
| Type | Description | Morphology |
|---|---|---|
| I | Bilateral pedicle fractures, non-displaced (less than 3 mm of anterior axis body displacement), and with no angulation |  |
| II | Severe angulation and displacement (>3 mm of horizontal displacement) with a vertical fracture line |  |
| IIA | No horizontal displacement but significant angulation and a horizontal fracture line | 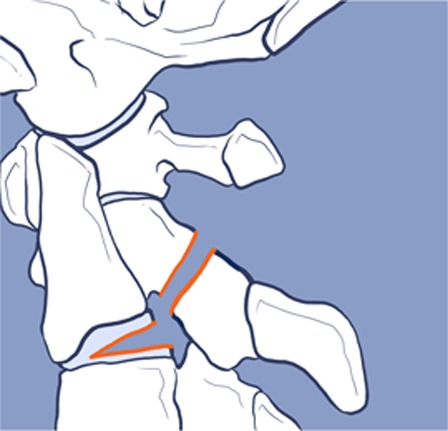 |
| III | Severe displacement and angulation associated with uni- or bilateral C2–3 facet dislocation | 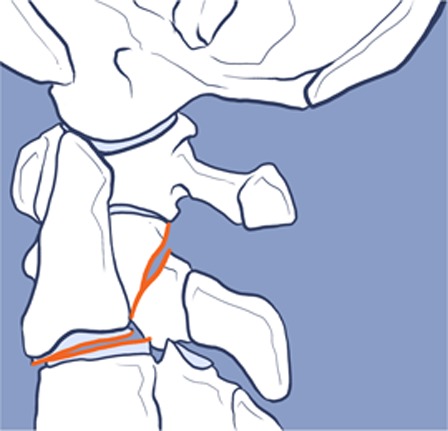 |
Group 2 – Patients with fractures without clear ligament disruption
All of the patients with fractures without dislocations, abnormal subluxations, or perched facet joints, without instability detected on dynamic radiological evaluation (not usually obtained in the immediate post-injury setting) are included in this group. Patients with subtle MRI abnormalities without clear CT scan abnormalities may be included as well.
Occipital condyle fractures
Nearly all OCFs, without associated ligamentous injury, may be managed without surgical treatment.22–24 This is probably due to the combination of good cancellous fracture surfaces that promote healing with stability provided by the ligaments of the occipito-cervical junction.14,25,26 Even in the presence of cranial nerve deficits, external immobilization can be used satisfactorily regarding the condyle fracture subtypes without ligament injury (type 1, 2, and 3).25 These fractures, when not associated with other injuries, or obvious instability due to fracture displacement or ligament disruption/incompetence can be treated with external immobilization.12,22,23,25
Atlas (C1) fractures
Isolated fractures of the atlas without TL injury can typically be treated with cervical immobilization alone.12 These injuries include isolated anterior or posterior arch, lateral mass, or combined anterior/posterior arch fractures.12 When associated with other cervical injuries, treatment is guided based on the concomitant injury.12,25
Axis (C2) fractures
Axis fractures can be defined by the anatomical location: odontoid, vertebral body, and/or posterior element fractures. Normal motion of C1 on C2 is restricted by the TL, securing the odontoid process to the anterior arch of the ring of C1. Subsequently, odontoid fractures share similar biomechanical properties of TL injuries which may, therefore, require stabilization or fracture healing.9 Table 4 illustrated the classification proposed by Anderson and D'Alonzo for odontoid fractures. The literature suggests that risk factors associated with a high degree of non-surgical failure include: age greater than 50 years old,27 dens displacement greater than 5 mm, comminution on the base of the odontoid process (traditional type IIA fractures), or inability to achieve or maintain acceptable fracture alignment with external immobilization.12,28 In the presence of one or more of these risk factors for non-union, early surgery is a reasonable option (Fig. 3). Odontoid fracture constitutes an exception of UCI, whose stability is based on bone anatomy rather than ligamentous restraint. Surgery may also be recommended for those patients with severe fracture displacement or delayed union after treatment with external immobilization.11,12,29,30
Table 4 .
Odontoid fractures – types of injuries according to Anderson and D'Alonzo
| Type | Description | Morphology |
|---|---|---|
| 1 | Avulsion fracture through the upper part of the odontoid process |  |
| 2 | Fracture occurring at the base of the odontoid |  |
| 3 | Fracture line extends through the body of the atlas and can involve the superior articular facet |  |
Figure 3 .

This 77-year-old woman fell from the stairs with a cervical spine fracture on the base of the odontoid with moderate posterior dens displacement (A – sagittal CT scan reconstruction). She had an important risk factor for non-union (age > 50 years old), she underwent a C1 lateral mass with C2 pars screws instrumentation. Post-operative CT scan showed good dens alignment (B) and left side C1–2 instrumentation (C). (D) One year after surgery, bone healing in the dens base was demonstrated.
Fractures of the body of the axis can be treated with external immobilization. The large cancellous surface of fractures of the C2 body typically provides stability as well as fracture healing.3,4,12,29
For traumatic spondylolisthesis of the axis without disruption of ligamentous injury exposed above (C2–3 disk space disruption of locked facet joints), most authors suggest that patients can be successfully treated with external immobilization and radiological follow-up (Figs. 4 and 5).11,20,21
Figure 4 .
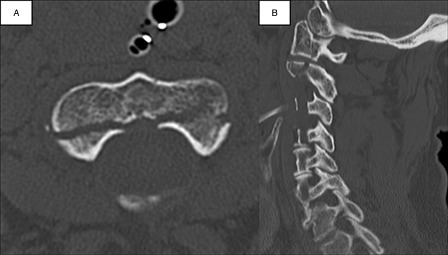
This patient is a 30-year-old man who presented with a C2 fracture after a motorcycle accident. No ligament injury was diagnosed. (A) shows an axial CT scan of the axis, with a posterior elements fracture without significant displacement. In the cervical lateral radiography (B), there was no spinal deformity or bone misalignment. This patient was successfully treated with a cervical collar.
Figure 5 .

This 19-year-old boy presented with serious neck pain after a car accident. In (A) and (B), a sagittal CT scan reconstruction showed a fracture in the body and in the posterior elements of the axis. (C) A coronal reconstruction showed a linear fracture in the body of the axis. Once there was no evident ligamentous injury or risk factors for non-union and misalignment, this patient was treated conservatively for 12 weeks, with a cervical collar. A CT scan was then performed, with good evidence of bone healing (D and E). The maintenance of the cervical alignment was demonstrated in the lateral plain cervical X-ray (F).
Discussion
Clinical instability is defined as a loss in the ability of the spine under physiological loads to maintain relationships between vertebrae in such a way that there is neither damage nor subsequent irritation to the spinal cord or nerve roots.31 In addition, clinical instability may be associated with incapacitating deformity or pain due to structural changes.31 Any injury pattern that can lead toward further neurological deficits, pain, or deformity should be addressed as an unstable injury, although not all unstable injuries require surgical treatment. Consequently, surgical treatment of spinal injuries should have three main goals: (i) prevent further neurological injury, (ii) reduce and stabilize the injured segment, and (iii) provide long-term stability and/or prevent deformity.19
A vast number of classification systems for upper cervical spine injuries have been published.9,11,18,21,32 That this large body of literature and wide array of classification systems exists is an attestation to the variation and the controversies surrounding their evaluation. The need for an objective and universal system to help guide medical decision-making in the setting of the UCI is presented, much like that developed for the subaxial cervical spine (SLIC) and the thoracolumbar spine (TLICS).33,34
After evaluation of the classical surgical indications for UCI based on the traditional classification systems described, we noted that the main factors that appeared to guide the treatment were based upon a compromised ligamentous complex in the occipito-cervical junction, in the atlantoaxial complex, and in the C2–3 complex as well as specific fracture patterns (occipital condyle, atlas, and axis). This observation has also been described by Jackson et al.19, suggesting that ligamentous injuries should be better managed surgically.
Based on these, we have to answer a critical question to propose a rational approach to upper cervical trauma: what is the status of the ligamentous complex in the occipito-cervical junction, in the atlantoaxial complex, and in the C2–3 complex compromised?
Ligamentous status of the craniocervical junction
The ligamentous status of the craniocervical junction is the most important factor in deciding between surgical and non-surgical treatment after a UCI is diagnosed. The important ligaments of this region supply stability to the occiput and C1 as well as between C1–2–3. The special arrangements of the occipito-atlantoaxial ligaments allow a wide range of motion with concomitant stability.1 Traumatic ligamentous injuries have a poor prognosis for healing and patients often respond best to surgical stabilization in order to avoid late deformity and neurological deficits.35
There are three important ligament groups in this region: (i) ligaments attaching the occiput to the body and dens of C2 (tectorial membrane, paired alar ligaments, apical ligament, and the ligament nuchae); (ii) ligaments attaching the occiput to the atlas (articular capsules of the atlanto-occipital joints and anterior and posterior atlanto-occipital membranes); and (iii) ligaments supporting the atlas to the axis (cruciate ligament, anterior and posterior longitudinal ligaments, the TL, and the articular capsules surrounding the opposing articular facets).24 Direct ligamentous injury can lead to instability and surgical treatment is indicated due to the lack of stability and small potential for structural ligamentous healing with non-surgical treatment.19
MRI and the evaluation of ligamentous injuries
Interpretation of the MRI findings in craniocervical trauma should be used together with clinical and CT scan findings. Of note, the MRI should be obtained in the first 48 hours after traumatic injuries. Horn et al.36 retrospectively evaluated radiological findings of 33 patients with AOD. The measurement of the axial-basion dens interval on CT scan was the most sensitive method used for diagnosis. They concluded that abnormal findings on the MRI associated with no or questionable abnormalities on CT scan provide a rationale for non-operative management. Radcliff et al. evaluated 18 patients with acute traumatic occipito-cervical injuries of which 17 had MRI imaging. Thirteen patients had bony displacement outside the normal range. Six had occipitoatlantal and atlantoaxial joints displacement, five had only atlantoaxial displacement, and two had an abnormal basion-dental interval. All five patients with occipitoatlantal displacement had injury in the occipitoatlantal capsule illustrated with MRI. Patients without occipitoatlantal displacement did not have occipitoatlantal capsular injury on MRI.37 Also, the patients without displacement or ligamentous injury on MRI were neurologically intact. In conclusion, although the MRI findings may suggest ligamentous injury, surgery often should not be based solely on isolated MRI findings, similar to injuries involving the subaxial and thoracolumbar spine.
Specific fracture patterns
If ligamentous injury is excluded, the second point to consider is the fracture location. As a general rule, non-displaced and well-aligned fractures often heal well. Surgery should be reserved for patients with the inability to achieve or maintain acceptable fracture alignment with external immobilization. Surgical treatment is therefore indicated most commonly in the elderly patient with an odontoid fracture known to be at high risk for non-union, C1 ring fracture with severe lateral mass displacement with resultant occipital, C1 or C2 subluxation, or pathological subluxations or dislocations (Fig. 6). Inadequate treatment of these injuries can lead to fracture displacement, dislocation, and subsequent neural impingement with late neurological deterioration, deformity, and refractory pain.11,12,18,30,38
Figure 6 .

This 21-year-old man presented with a C1 left lateral mass fracture and severe neck pain, as shown in the axial CT scan of the axis (A) and in the sagittal reconstruction (B). The TL was probably incompetent due to the fracture of this insertion region with the floating left lateral mass. When good spinal alignment could not be re-established, an occipital C2–3 fusion was performed, as shown in the sagittal (C) and coronal CT scan reconstructions.
This rational approach to craniocervical traumatic injuries is summarized in the flow chart (Fig. 7, Tables 5 and 6).
Figure 7 .

Proposed treatment algorithm to help in the decision-making process – operative versus non-operative treatment. OCD, occipito-cervical dislocation; AA, atlantoaxial instability; LT, ligament transverse.
Table 5 .
Suggested treatment for ligamentous injuries in the upper cervical spine
| Injuries | Treatment |
|---|---|
| AOD | Occipito-cervical stabilization |
| Atlantoaxial dislocation | Atlantoaxial stabilization |
| Ligament transverse injury at its substance | |
| C2–3 disk disruption or locked facet joints | C2–3 stabilization |
Table 6 .
Suggested treatment for fractures without clear ligamentous injury in the upper cervical spine
| Injuries | Treatment |
|---|---|
| Condyle fractures | Non-surgical treatment |
| Atlas fractures | |
| Axis fractures* |
*Exceptions: fractures at the base of the dens in patients with risk factors for non-union (>50 years old, severe displacement between bone fractures and comminution).
Craniocervical injuries: relationship between neurological deficit and stability
Neurological injury is one of the most influential predictors of treatment after subaxial cervical and thoracolumbar spinal trauma.33,34,39 Neurological status is used in the two recently proposed scoring systems for cervical and thoracolumbar spine trauma, the SLICS (Subaxial Injury Classification system), and the TLICS (Thoracolumbar Injury Classification System).33,34 However, as presented above, surgical indications available in the literature for upper cervical traumatic injuries have been dictated by ligamentous injuries or fracture patterns. These indications have not typically been linked to the presence of neurological deficits, even though the presence of a neurological injury may be consistent with a more highly unstable injury pattern.
Cranial nerves injuries in the setting of UCI are not a clear indication for surgical management. Condyle fractures, for example, can present with hypoglossal, glossopharyngeal, or vagal nerve injuries. Multiple authors report neurological improvement with external immobilization, generally not requiring surgery.12,40
Isolated atlas fractures generally are stable and are not associated with neurological injuries. Given that most C1 ring fractures result in disruption and expansion of the ring, post-traumatic cord compression is rare. In addition, the space available for the cord, at baseline, is greater at the C1–2 area than the subaxial spine. Therefore, minor fracture encroachment into the canal typically does not result in spinal cord compression. Among a series of 57 patients, Hadley et al.,41 reported 32 patients with isolated atlas fractures, none with a neurological injury. Fowler et al.42 also reported their series of 48 patients with atlas fractures that no patients with an isolated atlas fracture presented with a neurological deficit.
Fractures of the posterior elements of the axis (Hangman's fractures) are not commonly reported with neurological injury. As with C1 ring fractures, canal expansion is typically found with C2 posterior element fractures with the exceptions being those with significant translation or fracture encroachment into the spinal canal. Francis et al.32 reported a series of 123 patients, 8 (6%) sustained neurological injury. Tan's retrospective series of 33 patients included 19 (57%) patients with neurological deficits ranging from quadriparesis to urinary retention.43 Seven (26%) of the 27 patients in the Mirvis series also had neurological findings.44 Starr and Eismont45 reported a variant C2 fracture called atypical Hangman's fracture, occurring through the posterior aspect of the vertebral body with unilateral or bilateral continuity of the posterior cortex or pedicle, narrowing the spinal canal, with a paralysis incidence of 33%.
Similarly, in odontoid fractures, the relatively larger canal of the upper cervical spine may reduce the likelihood of neurological injury.45 Thus, odontoid fractures are an infrequent cause of neurological injury, with an incidence ranging from 0 to 27%; generally caused by motor vehicle accidents and are associated with a high mortality rate.30,31,41,46–48
In clearly unstable lesions with ligamentous disruption, a high incidence of neurological damage is reported. AOD is associated with neurological injury in 20% of patients, among those that survived the initial traumatic event.12 In the largest report of 39 cases, Dickman et al.18 found just 2 cases (about 5%) of neurological injury. Among five patients with C2–3 translational injuries (unilateral or bilateral facet dislocation), Levine et al. reported three of them (60%) with neurological injury related to the spinal fracture, while Effendi reported two of nine patients (22.2%) with neurological deficits.11,21
In summary, the literature demonstrates that a neurological deficit associated with an upper cervical spine injury typically suggests an unstable injury pattern. The instability and the presence of a neurological injury can guide surgical treatment, which often involves early stabilization and rehabilitation. The literature is replete with case examples of unstable injuries in association with a neurological deficit managed successfully non-operatively. This is often in the context of prolonged immobilization and bed rest, which is associated with the side effects of such management. In some of these cases occult instability is noted with delayed dynamic imaging requiring late surgical intervention.
Conclusion
Ascertaining the status of relevant ligamentous structures, the fracture alignment/stability and the presence of neurological deficit may be important in determining surgical versus non-surgical treatment for patients with injuries to the craniocervical region.
The proposed recommendations for treatment of UCI are options based on our literature review. While the proposed approach is based on the best available evidence, our theory should be validated in the clinical setting. Ongoing studies are necessary to establish the safety, reliability, and clinical validity of our proposed scheme for evaluation and treatment of UCI.
References
- 1.Menezes AH, Traynelis VC. Anatomy and biomechanics of normal craniovertebral junction (a) and biomechanics of stabilization (b). Childs Nerv Syst 2008;24(10):1091–100 [DOI] [PubMed] [Google Scholar]
- 2.Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 1998;88(6):962–8 [DOI] [PubMed] [Google Scholar]
- 3.Joaquim AF, Patel AP. Occipito cervical trauma: evaluation, classification and treatment. Contemp Spine Surg 2010;11(4):1–5 [Google Scholar]
- 4.Joaquim AF, Patel AP. C1 and C2 spine trauma: evaluation, classification and treatment. Contemp Spine Surg 2010;11(3):1–7 [Google Scholar]
- 5.Wadhwam R, Shamieh S, Haydel J, Caldito G, Williams M, Nanda A. The role of flexion and extension computed tomography with reconstruction in clearing the cervical spine in trauma patients: a pilot study. J Neurosurg 2011;14(3):341–7 [DOI] [PubMed] [Google Scholar]
- 6.Gonzalez LF, Fiorella D, Crawford NR, Wallace RC, Feiz-Erfan I, Drumm D, et al. Vertical atlantoaxial distraction injuries: radiological criteria and clinical implications. J Neurosurg Spine 2004;1(3):273–80 [DOI] [PubMed] [Google Scholar]
- 7.Chang W, Alexander MT, Mirvis SE. Diagnostic determinants of craniocervical distraction injury in adults. AJR Am J Roentgenol 2009;192(1):52–8 [DOI] [PubMed] [Google Scholar]
- 8.Monu J, Bohrer SP, Howard G. Some upper cervical spine norms. Spine 1987;12(6):515–9 [DOI] [PubMed] [Google Scholar]
- 9.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am 1974;56(8):1663–74 [PubMed] [Google Scholar]
- 10.Traynelis VC, Marano GD, Dunker RO, Kaufman HH. Traumatic atlanto-occipital dislocations: case report. J Neurosurg 1986;65(6):863–70 [DOI] [PubMed] [Google Scholar]
- 11.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br 1981;63(3):319–27 [DOI] [PubMed] [Google Scholar]
- 12.Hadley MN, Walters BC, Grabb PA, Oyesiku NM, Przybylski GJ, Resnick DK, et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin Neurosurg 2002;49:407–98 [PubMed] [Google Scholar]
- 13.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation: part 1 – normal occipital condyle-C1 interval in 89 children. Neurosurgery 2007;61(3):514–21 [DOI] [PubMed] [Google Scholar]
- 14.Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation – part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery 2007;61(5):995–1015 [DOI] [PubMed] [Google Scholar]
- 15.Harris JH Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol 1994;162(4):881–6 [DOI] [PubMed] [Google Scholar]
- 16.Bellabarba C, Mirza SK, West GA, Mann FA, Dailey AT, Newell DW, et al. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine 2006;4(6):429. [DOI] [PubMed] [Google Scholar]
- 17.DiBenedetto T, Lee CK. Traumatic atlanto-occipital instability. A case report with follow-up and a new diagnostic technique. Spine 1990;15(6):595–7 [DOI] [PubMed] [Google Scholar]
- 18.Dickman CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery 1996;38(1):44–50 [DOI] [PubMed] [Google Scholar]
- 19.Jackson RS, Banit DM, Rhyne AL, Darden BV. Upper cervical spine injuries. J Am Acad Orthop Surg 2002;10(4):271–80 [DOI] [PubMed] [Google Scholar]
- 20.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop Relat Res 1985;193(3):178–83 [PubMed] [Google Scholar]
- 21.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985;67(2):217–26 [PubMed] [Google Scholar]
- 22.Capuano C, Costagliola C, Shamsaldin M, Maleci A, Di Lorenzo N. Occipital condyle fractures: a hidden nosologic entity. An experience with 10 cases . Acta Neurochir (Wien) 2004;46(8):779–84 [DOI] [PubMed] [Google Scholar]
- 23.Caroli E, Rocchi G, Orlando ER, Delfini R. Occipital condyle fractures: report of five cases and literature review. Eur Spine J 2005;14(5):487–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malham GM, Ackland HM, Jones R, Williamson OD, Varma DK. Occipital condyle fractures: incidence and clinical follow-up at a level 1 trauma centre. Emerg Radiol 2009;16(4):291–7 [DOI] [PubMed] [Google Scholar]
- 25.Anderson PS, Montesano XP. Morphology and treatment of occipital condyle fractures. Spine 1988;13(7):731–836 [DOI] [PubMed] [Google Scholar]
- 26.Maserati MB, Stephens B, Zohny Z, Lee JY, Kanter AS, Spiro RM, et al. Occipital condyle fractures: clinical decision rule and surgical management. J Neurosurg Spine 2009;11(4):388–95 [DOI] [PubMed] [Google Scholar]
- 27.Lennarson PJ, Mostafavi H, Traynelis VC, Walter BCl. Management of type II dens fractures: a case-control study. Spine (Phila Pa 1976) 2000;25(10):1234–7 [DOI] [PubMed] [Google Scholar]
- 28.Hadley MN, Browner CM, Liu SS, Sonntag VK. New subtype of acute odontoid fractures (type IIA). Neurosurgery 1988;22(1):67–71 [DOI] [PubMed] [Google Scholar]
- 29.Mestdagh H, Letendart J, Sensey JJ, Duqquennoy A. Treatment of fractures of the posterior axial arch. Results of 41 cases. Rev Chir Orthop Reparatrice Appar Mot 1984;70(1):21–8 [PubMed] [Google Scholar]
- 30.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22(16):1843–52 [DOI] [PubMed] [Google Scholar]
- 31.Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg 1993;78(1):32–5 [DOI] [PubMed] [Google Scholar]
- 32.Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br 1981;63(3):313–8 [DOI] [PubMed] [Google Scholar]
- 33.Vaccaro AR, Hulbert RJ, Patel AA, Fisher C, Dvorak M, Lehman RA Jr, et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine (Phila Pa 1976) 2007;32(21):2365–74 [DOI] [PubMed] [Google Scholar]
- 34.Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 2005;30(20):2325–33 [DOI] [PubMed] [Google Scholar]
- 35.White AA, Panjabi MM. Clinical biomechanics of the spine. Philadelphia: Lippincott; 1978 [Google Scholar]
- 36.Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine 2007;6(2):113–20 [DOI] [PubMed] [Google Scholar]
- 37.Radcliff K, Kepler C, Reitman C, Harrop J, Vaccaro A. CT and MRI-based diagnosis of craniocervical dislocations: the role of the occipitoatlantal ligament. Clin Orthop Relat Res 2012;470(6):1602–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fairholm D, Lee ST, Lui TN. Fractured odontoid: the management of delayed neurological symptoms. Neurosurgery 1996;38(1):38–43 [DOI] [PubMed] [Google Scholar]
- 39.Patel AA, Dailey A, Brodke DS, Daubs M, Anderson PA, Hurlbert RJ, et al. Subaxial cervical spine trauma classification: the Subaxial Injury Classification System and case examples. Neurosurg Focus 2008;25(5):E8. [DOI] [PubMed] [Google Scholar]
- 40.Legros B, Fournier P, Chiaroni P, Ritz O, Fusciardi J. Basal fracture of the skull and lower (IX, X, XI, XII) cranial nerves palsy: four case reports including two fractures of the occipital condyle– a literature review. J Trauma Inj Infect Crit Care 2000;48(2):342–48 [DOI] [PubMed] [Google Scholar]
- 41.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: a review of 229 cases. J Neurosurg 1989;71(5):642–7 [DOI] [PubMed] [Google Scholar]
- 42.Fowler JL, Sandhu A, Fraser RD. A review of fractures of the atlas vertebra. J Spinal Disord 1990;3(1):19–24 [PubMed] [Google Scholar]
- 43.Tan ES, Balachandran N. Hangman's fracture in Singapore (1975–1988). Paraplegia 1992;30(3):160–4 [DOI] [PubMed] [Google Scholar]
- 44.Mirvis SE, Young JW, Lim C, Greenberg J. Hangman's fracture: radiologic assessment in 27 cases. Radiology 1987;163(3):713–7 [DOI] [PubMed] [Google Scholar]
- 45.Starr JK, Eismont FJ. Atypical Hangman's fractures. Spine (Phila Pa 1976) 1993;18(14):1954–7 [DOI] [PubMed] [Google Scholar]
- 46.Harrop JS, Sharan AD, Przybylski GJ. Epidemiology of spinal cord injury after acute odontoid fractures. Neurosurg Focus 2000;15;8(6):E4. [PubMed] [Google Scholar]
- 47.Ekong CE, Schwartz ML, Tator CH, Rowed DW, Edmonds VE. Odontoid fracture: management with early mobilization using the halo device. Neurosurgery 1981;9(6):631–7 [DOI] [PubMed] [Google Scholar]
- 48.Apuzzo MLJ, Heiden JS, Weiss MH, Ackerson TT, Harvey JP, Kurze T. Acute fractures of the odontoid process. An analysis of 45 cases. J Neurosurg 1978;48(1):85–91 [DOI] [PubMed] [Google Scholar]


