Abstract
Context/objective
Examine the relationship of post-traumatic psychological growth (PTG), depression, and personal and injury characteristics in persons with spinal cord injury (SCI).
Design
Cross-sectional survey.
Setting
Community.
Participants
Eight hundred and twenty-four adults with SCI.
Interventions
None.
Outcome measures
Five items from the Post-traumatic Growth Inventory, reflecting positive change after injury in life priorities, closeness to others, new opportunities being available, stronger faith, and personal strength.
Results
Initial structural equation model testing of a conceptual model of personal and injury characteristics, violent etiology, depression, and PTG resulted in a poor fit. Model modifications resulted in an improved fit, but explained only 5% of the variance in PTG. Being female, younger, having less formal education, and less time since injury had significant relationships with PTG, whereas depression, violent etiology, and injury level/severity did not. In each PTG domain, between 54 and 79% of the sample reported at least some positive change after injury.
Conclusions
The results of this study, while promising, explained only a small portion of the variance in PTG. A majority of the sample experienced some positive change after injury, with the greatest change in discovering that they were stronger than they thought they were. Comparing means previously reported in a non-SCI sample of those who experienced trauma, positive change after injury was comparable for each PTG item except for new opportunities being available, which was significantly lower for those with SCI. Future directions of research include the development of theoretical models of PTG after SCI.
Keywords: Spinal cord injuries, Depression, Trauma
Introduction
Post-traumatic psychological growth (PTG), also referred to as stress-related growth, adversarial growth, or benefit finding,1 is characterized as a positive change that occurs as a result of a highly challenging life crisis, such as trauma.2 Although the potentially transformative power of suffering is not a new concept, academic interest in PTG did not emerge until the 1980s and the use of the term “post-traumatic growth” did not appear until 1996.2 The burgeoning interest in PTG and the development of conceptual models diverge from an exclusive focus on negative emotions, allowing that psychological growth and adjustment are equally important outcomes of traumatic events. In fact, some researchers argue that growth rather than pathology, is a normal outcome of traumatic stress.3 Tedeschi and Calhoun's conceptualization of PTG is one of the most widely cited. In their model, growth does not occur as a direct result of trauma but from the struggle with a new reality as its aftermath. This struggle is critical to whether or not and the extent to which PTG occurs. This struggle ultimately leads to growth and wisdom, even in the face of enduring distress; this process is also influenced by personal qualities, cognitive processing, and the individual's social system.2
Several recent systematic reviews of PTG among persons with serious medical conditions,1 and in relation to psychological and physical health,4 provide support for the influence of disease-related and personal characteristics, coping styles, spirituality, and outlook on the degree to which PTG occurs after trauma. According to these reviews, female sex, White race, being married, younger age, having greater emotional support, and positive health behaviors are associated with higher PTG. Such characteristics as optimism, religiosity, self-efficacy, and self-esteem also have been closely linked to PTG in these reviews. High levels of PTG are related to lower depression and emotional distress, and lower PTG is associated with higher post-traumatic stress disorder (PTSD) symptoms.
Despite considerable interest in PTG and its relevance to the adjustment process after traumatic injury, there are few coherent theoretical models of PTG as they apply to disability.5 Most individuals with acquired spinal cord injury (SCI) have experienced significant trauma. Negative psychological consequences, such as PTSD, depression, and anxiety, have all been well studied. Over 25% of individuals with SCI have clinically significant anxiety or depression, compared with 12-month prevalence estimates in the general population (e.g. 18% for anxiety disorders and 9% for depressive disorders.6–8) The suicide rate in persons with SCI is two to six times greater compared with the non-SCI population, with the highest rates occurring during the first 5 years post-injury.9,10 PTSD disorder ranges from 10 to 40% in the SCI population, compared with a 12-month prevalence of less than 4% in the general population.8,11 Despite these negative outcomes, many individuals with SCI report a positive quality of life,12 cope well with their injury,13 make an effective psychological adjustment,14 and experience positive life changes.15 Consequently, clinicians and researchers have become interested in positive psychological responses to SCI, such as PTG. Tedeschi and Calhoun2 speculate that greater PTG might arise from traumatic experiences that are more “shattering” of a person's life and beliefs. Spinal cord injury is often described as among the most catastrophic injury people can sustain and, thus, potentially an opportunity for PTG.
Prediction of PTG might aid in helping individuals to experience more positive changes after a trauma. Several factors have been identified that potentially mediate or predict PTG. For example, PTG has been closely aligned with resilience. Resilience after trauma is characterized by a stable trajectory of healthy psychological and physical functioning.16,17 In persons with SCI, resilience has been linked to accepting challenges and the use of active coping,13 and it also acts as a buffer against the impact of stress on depression.18 In the few investigations of PTG in SCI to date, family relationships and engagement in and appreciation of life appear to be salient predictors of PTG.15,19 The conceptual framework of Tedeschi and Calhoun and research on the correlates of PTG in various populations lay the groundwork to pursue fundamental questions that remain about the prevalence and correlates of PTG after SCI. Determining whether or not PTG is related to demographic and clinical characteristics will set the stage for more theory-driven research and the development of therapeutic interventions to improve growth after SCI.
For the current analysis, we wanted to examine the degree of PTG and the factors associated with it in a large, heterogeneous sample of persons with SCI. Based on data available for our sample and previous SCI research,15,20 we constructed a conceptual model to examine the association of personal and injury-related factors and depression with PTG (Fig. 1). Based on the “shattering” notion,2 we expected that certain factors (i.e. younger age, violent etiology, and more severe injury) would be significantly associated with PTG. We also examined the association of depression and PTG, based on Tedeschi and Calhoun's2 model that PTG and emotional distress can co-exist.
Figure 1 .
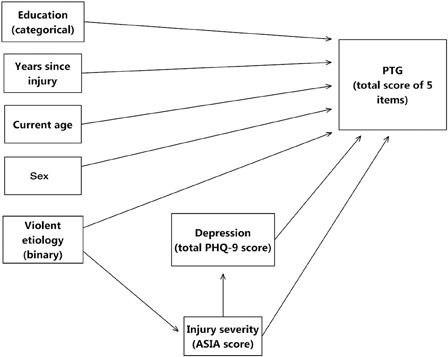
Conceptual model
Methods
Sample description
The sample for the current analysis (N = 824) was drawn from the screening phase of a larger study examining the efficacy of the antidepressant venlafaxine XR for treating major depression disorder (MDD) in adults with SCI. The Project to Improve Symptoms and Mood after SCI (PRISMS) is a multicenter study at five sites across the US: BLINDED (University of Washington (Seattle, WA), Rehabilitation Institute of Chicago (Chicago, IL), University of Alabama at Birmingham (Birmingham, AL), University of Michigan (Ann Arbor, MI), and Baylor Institute for Rehabilitation (Houston, TX)). Screening phase inclusion criteria were being at least 18 years old and having a history of traumatic SCI, at any level and/or severity. Study exclusion criteria were: (i) being non-English speaking; (ii) too cognitively impaired to comprehend study materials; and/or (iii) referral to the study from a clinician, based on the belief that the person was indeed depressed. Institutional Review Boards at each site approved this research project and each participant provided informed consent.
Data collection and measures
The survey was conducted in person or by telephone by trained research staff. Structured interviews lasted 15–20 minutes. For the current analysis, the following measures were used.
The Post-traumatic Growth Inventory (PTGI)21 was developed in 1996 to measure PTG in people who had experienced a traumatic event; it is one of the most commonly used PTG scales. A confirmatory factor analysis by Taku et al.22 supported a five-factor structure of: (1) relating to others; (2) new opportunities being available; (3) personal strength; (4) spiritual change; and (5) appreciation for life. The sample for that confirmatory factor analysis (N = 926) consisted of adults from 14 other PTG studies and who had experienced a traumatic event at some point in their lives. For this current analysis, we selected a single item from each of the five factors with high factor loadings, and that also represented the dimension of PTG most relevant to SCI. To reduce respondent burden, five items were selected in favor of the entire scale, given the overall length of the screening interview. The instructions to respondents were slightly modified, with the injury as the reference point for positive change. Each item was rated on 6-point Likert scales, ranging from 0 (no change) to 5 (very great change). Internal consistency (Cronbach's alpha) of the five items was 0.758, which is in the acceptable range.
The Patient Health Questionnaire (PHQ-9)23 was developed as a screening measure for major depression,24 and has been validated against Diagnostic and Statistical Manual of Mental Disorders, version IV (DSM-IV) criteria for a major depression in people with SCI.25 Nine items parallel the DSM-IV criteria for MDD. Items are self-rated according to how often the person has been bothered by the symptoms over the preceding 2 weeks, ranging from 0 (not at all) to 3 (nearly every day). There are two scoring methods for the PHQ-9, both of which were used in this study. The first uses the same symptom criteria as the DSM-IV, with a classification of “probable MDD”. This approach has demonstrated good sensitivity (88%) and specificity (88%), in both primary care and obstetrics-gynecology samples.24,26 The other scoring method is the sum of all nine items (ranging from 0 to 27) as a measure of overall depressive symptom severity.
Demographic and injury characteristics collected from participants were current age, sex, racial/ethnic background, marital status, level of education achieved, current employment status, violent etiology of injury, level of injury, and severity of injury using the American Spinal Injury Association injury scale (AIS).27 The use of psychiatric services in the past 3 months was also collected using the Cornell services index.28 Services include clinical case management, medication management, psychotherapy (individual and group), diagnostic intake, alcohol/drug visit, and self-help groups.
Statistical analysis
Basic descriptive statistics (means and frequencies) were used to describe scores on study variables. We tested whether there were significant differences in the five PTG item means between this sample and the confirmatory factor analysis sample of the PTGI by Taku et al.22 (referred hereafter as the mixed, non-SCI sample), using an independent samples t-test. A structural equation model (SEM) was used to examine the relationship between PTG items (summary score) and demographics, injury characteristics, and depression (predictors). To determine how well the theoretical model represented the observed data, the chi-square statistic was generated and a number of fit indices were examined.
Based on suggestions for “favorable” model fit provided by Kline,29 the following criteria were used to assess the fit of the theoretical model shown in Fig. 1: (i) a non-significant goodness-of-fit chi-square statistic (P > 0.05); (ii) a chi-square to degrees of freedom ratio of ≤3; and (iii) a comparative fit index (CFI) of ≥0.95. The CFI ranges from 0 to 1, where 0 reflects no fit and 1 indicates that the theoretical model perfectly fits the observed data.29 The root-mean-square error of approximation (RMSEA) was also examined as another criterion; Hu and Bentler30 have suggested that RMSEA ≤ 0.06 indicates a good model fit. Finally, the model was estimated using the maximum-likelihood method.
The values used to label single-headed arrows (Fig. 2) are standardized direct-effect coefficients. They indicate the strength of a direct relationship between two variables, much like standardized regression coefficients. Because these values are standardized, they typically range from 0 to 1, with higher values indicating a stronger relationship between variables. Each indirect-effect coefficient represents the effect of a predictor variable through one or more mediators to the outcome variable. The coefficient can be calculated by taking the product of the standardized direct-effect coefficient between the predictor and the mediator and the standardized direct-effect coefficient between the mediator and the outcome. Again, higher values indicate a stronger indirect effect. A bootstrap method was used to obtain significance levels of indirect effects. Total effects are the sum of direct and indirect effects. The use of direct and indirect effect terminology is not meant to imply causation, but is used as a matter of convention for interpreting SEM results.
Figure 2 .
PTG item response distributions
Mplus 6.1 (Muthén & Muthén, Los Angeles, CA, USA) and SPSS® 20 (IBM SPSS Statistics for Windows, Version 20.0. IBM Corp., Armonk, NY, USA) were used to analyze the data. Mplus was selected for analysis, because it is able to handle categorical- and binary-dependent variables for SEM analysis. Power was estimated based on parameters and degrees of freedom in the final model. To estimate the minimum sample size needed to obtain a close fit of the model at 80% power, we employed Kim's31 method using RMSEA to compute the non-centrality parameter. With seven degrees of freedom and α = 0.05, the minimum sample size needed to achieve 80% power was 821.
Results
Demographic and injury characteristics
Demographic and injury characteristics for the sample are given Table 1.
Table 1 .
Demographic and injury characteristics of sample (N = 824)
| Characteristics | Time in years (SD), range in years |
|---|---|
| Current age | 43.67 (13.7), 18–83 |
| Years post-injury | 10.75 (9.4), 1–60 |
| Characteristics | No. (%) |
| Male sex | 632 (76.7) |
| Race | |
| Caucasian | 551 (68.3) |
| African American | 192 (23.8) |
| Native American | 6 (0.7) |
| Asian | 10 (1.2) |
| Other | 48 (5.8) |
| Marital status | |
| Single | 387 (47.0) |
| Married | 269 (32.7) |
| Divorced | 135 (16.4) |
| Separated | 13 (1.6) |
| Widowed | 15 (1.8) |
| Other | 5 (0.5) |
| Education, N | |
| < High school | 90 (10.9) |
| High school/GED | 446 (54.1) |
| College (associate or bachelor) | 247 (27.6) |
| Graduate degree | 56 (6.8) |
| Other/unknown | 5 (0.6) |
| Current occupational status | |
| Working | 192 (23.3) |
| Retired | 100 (12.2) |
| Unemployed | 313 (38.2) |
| Student, other, unknown | 219 (26.6) |
| Level of injury | |
| Paraplegia | 381 (46.2) |
| Tetraplegia | 415 (50.4) |
| Missing/unknown | 28 (3.4) |
| Completeness of injury | |
| AIS A | 366 (50.1) |
| AIS B | 111 (15.2) |
| AIS C | 113 (15.5) |
| AIS D | 141 (19.3) |
| Missing/unknown | 93 (11.3) |
| Violence as cause of injury | 128 (15.5) |
| Psychiatric services received in last 3 months* | |
| Clinical case management | 21 (2.5) |
| Medication visit | 38 (4.6) |
| Combined med and psychotherapy | 6 (0.7) |
| Psychotherapy, individual | 44 (5.3) |
| Psychotherapy, group | 10 (1.2) |
| Psychotherapy, couple | 8 (1.0) |
| Diagnostic intake | 13 (1.6) |
| Alcohol/drug visit | 1 (0.1) |
| Self-help group | 14 (1.7) |
| Other psychiatric service | 8 (1.0) |
*Individuals were able to select more than one service.
Descriptive statistics
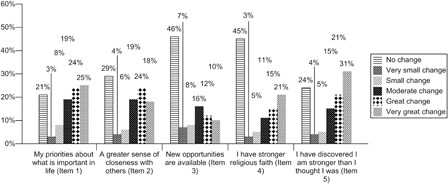
The overall mean of the five PTG items was 12.40 (SD 6.8), with a range of 0–25. Between 21 and 46% of the sample reported no positive change after injury for any of the five items. When change did occur, the degree of change varied depending on the PTG domain (see Fig. 2). The prevalence of probable MDD was 11.2% (N = 92), using the PHQ-9 scoring algorithm. The overall mean depressive symptom severity was 6.0 (SD 5.5; range 0–27), which is in the mild range.24
The SCI sample and the mixed, non-SCI sample varied on certain demographic characteristics. The SCI sample was significantly older (43.7 vs. 30.7 years, respectively, P < 0.001), with a greater proportion of males (76.7 vs. 26.1%, respectively, P ≤ 0.001) and a smaller proportion of married persons (47.0 vs. 59.5%, respectively, P ≤ 0.001). Each sample had a comparable majority of White participants (68.3 vs. 69.2%, respectively). In the mixed, non-SCI sample, close to half (48.2%) had experienced a traumatic event in the 12 months prior to assessment of PTG. For the SCI sample, significantly fewer (19%, P ≤ 0.001) had sustained their injury in the previous 12 months. Comparison of mean scores of each of the five PTG items between samples suggested that only the item of “new opportunities were available” was significantly lower in the SCI group (Table 2).
Table 2 .
Mean item score comparisons with mixed, non-SCI sample16
| Item (range 0–5) | SCI mean (SD) | Mixed, non-SCI mean (SD) | t, P value |
|---|---|---|---|
| My priorities about what is important in life | 2.99 (1.83) | 3.01 (1.69) | 0.238, 0.812 |
| A greater sense of closeness with others | 2.59 (1.90) | 2.52 (1.72) | 0.808, 0.419 |
| New opportunities are available | 1.72 (1.85) | 2.01 (1.93) | 3.20, 0.001 |
| I have stronger religious faith | 2.11 (2.10) | 2.12 (1.92) | 0.10, 0.92 |
| I discovered I am stronger than I thought I was | 3.00 (1.96) | 2.91 (1.78) | 1.00, 0.31 |
SEM (conceptual model testing)
Testing our conceptual model (Fig. 1), using the AIS score and a continuous PHQ-9 score, all fit indices were outside the desirable range. A significant chi-square value (χ2 = 61.33, df = 8, P ≤ 0.001) suggested a discrepancy between the theoretical model and the observed data, with chi square to degrees of freedom ratio of 7.66. The CFI = 0.51 and RMSEA = 0.091 (90% confidence interval (CI): 0.070–0.112) also were outside of acceptable limits.
Final model
Given the poor fit of the conceptual model, we revised the model to include a relationship between sex and depression (modification 1), replaced the AIS score with an injury level of tetraplegia vs. paraplegia (modification 2), and replaced the continuous PHQ-9 score with a binary score (yes/no) of probable MDD (modification 3). The final model testing resulted in improved, although still not entirely consistent, fit statistics. While a significant chi-square value, again, indicated a significant discrepancy between the theoretical model and the observed data (χ2 = 17.531, df = 7, P = 0.014), the CFI = 0.845 approached the ≥0.95 threshold. RMSEA = 0.043 (90% CI: 0.018–0.069) was also within acceptable limits. The R2 of PTG in the final model was 0.056, indicating that it accounted for only 5% of the variance in PTG for this sample.
In this current analysis, we were most interested in the association of injury and depression with PTG, while accounting for personal characteristics, such as education and age. The results of the model testing indicated that personal characteristics of lower education, younger age, being female, and less time since the injury had statistically significant and positive associations with PTG (Fig. 3). Depression, level of injury, and violent etiology had non-significant relationships with PTG. The indirect-effect coefficients (Table 3) were all non-significant, indicating that significant and non-significant associations with PTG were not mediated by other variables.
Figure 3 .
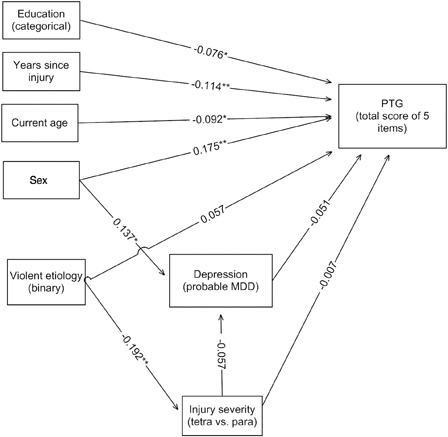
Final model
Table 3 .
Direct, indirect, and total effects1 of SEM model
| Model variables | Direct effects | Indirect effects | Total effects |
|---|---|---|---|
| Education on PTGI | −0.076* | – | −0.076* |
| Years since injury on PTGI | −0.144* | – | −0.144* |
| Current age on PTGI | −0.091* | – | −0.092* |
| Depression on PTGI | −0.051 | – | −0.051 |
| Level of injury on depression | −0.057 | – | −0.057 |
| Sex on PTGI (via depression) | 0.175** | −0.007 | 0.168** |
| Level of injury on PTGI (via depression) | −0.007 | 0.003 | −0.004 |
| Violent etiology on depression (via level of injury) | 0.011 | 0.093 | 0.104 |
| Violent etiology on PTGI (via level of injury and via depression, respectively) | 0.057 | 0.001 and −0.005 | 0.053 |
1All effects are standardized.* P ≤ 0.05.
** P ≤ 0.001.
Discussion
The results of this study provided preliminary support for our conceptual model; however, the final model explained only a small proportion of the variance associated with PTG. In this sample, greater PTG was associated with being female and younger; in fact, of all the variables in the model, sex was the variable most strongly related to PTG. Greater PTG among women has also been found in other research,1 and it may be related to how women process and consider different dimensions of PTG. The inverse and significant relationship between age and PTG, found in this study, is consistent with the notion that SCI earlier in life may be more likely to dramatically alter personal schemas and require substantial re-evaluation, ultimately leading to greater PTG.32 Alternatively, being younger may reflect greater openness to change,1 with older individuals relying on an established style of coping with traumatic events. The years since injury had the second strongest direct relationship with PTG. Unexpectedly, lower levels of PTG were associated with a longer time since injury, in contrast to findings in other disability samples.5 Other research has suggested that PTG accrues over time as the adjustment process unfolds, but the time course of this evolutionary process remains to be fully understood.1
The fact that violent etiology and injury severity were unrelated to PTG casts doubt on the applicability of the “shattering hypothesis”2 in the current analysis; this finding may be explained, in part, by differences in sample composition of this study as compared with the extant literature. Studies examining PTG and violence typically include individuals who all have experienced violence; for example, a positive association of violence and PTG has been found in women survivors of domestic violence.33 In contrast, our study had only a small proportion of individuals with violent injury etiology. With regard to injury severity, we tested both the level of injury and the AIS score, but neither had a significant association with PTG. Severity of disease in such conditions as HIV/AIDS or heart attacks also has generally not been predictive of greater PTG.1 There is, however, some evidence that a curvilinear relationship exists between disease severity and PTG in persons with various cancers.34,35
The lack of association between depression and PTG in this analysis is in contrast with a longitudinal study of persons with SCI;20 also, an inverse relationship between depression and PTG has been found in about half the studies on this topic.1 However, our finding is consistent with Tedeschi and Calhoun's2 notion that PTG and emotional distress can indeed co-exist. Research on depression and PTG has typically used samples with higher rates of MDD, and our discrepant findings may be partially explained by low rates of probable MDD in this sample. A curvilinear relationship of depression and PTG found in assault survivors suggests that moderate levels of PTG may be associated with higher depressive symptoms, while very low or very high PTG levels may not.36 While PTG can be accompanied by lower emotional distress in some people, our results suggest that this relationship is likely to be more complex in the context of SCI and thus worthy of further investigation.
The distribution of responses for each PTG item in this sample suggested that growth does not occur equally in all domains. For example, a majority of individuals in our analysis indicated some degree of change in priorities in their lives, a greater sense of closeness to others, and the discovery that they were stronger than they thought they were. Nearly half of the sample reported they did not have a stronger religious faith or that new opportunities were available to them after injury. The body of literature on PTG suggests that while many people across populations will experience some growth after trauma and adversity, this experience is not universal.1 In our analysis, comparisons with the mixed, non-SCI sample suggested that growth after SCI may be similar to growth that occurs in the aftermath of other traumatic events,5 despite the demographic differences between the samples. Moreover, people with SCI in this analysis reported less growth in the realm of having new opportunities, which may be directly related to physical and functional limitations imposed by their injury. Greater insight into processes of growth, both unique to SCI as well as reflecting a common experience among those who have experienced traumatic, is a compelling line for further inquiry.
Limitations and future directions
Our final model explained only a small amount of the variance in PTG, suggesting that there are other factors not accounted for which may contribute to PTG in SCI. Moreover, because our analysis drew from a larger set of data, we did not measure other salient psychological factors related to PTG, such as injury attributions, coping style, personality traits, spirituality, or social support. In addition, the small number of individuals in the sample recently receiving psychotherapy limited our ability to include this factor as a variable in the model. Also, we were not able to account for the mental health treatment received soon after injury, which could change the trajectory of PTG in some individuals. Including a broader range of psychological factors and mental health treatment in future studies will provide a deeper understanding of PTG in this population. We also were not able to examine the change in PTG over time because our data were cross-sectional.
One of the most important limitations of this study concerns the selection of only 5 items from the 21-item PTGI scale. While we reduced the respondent burden, this approach constrains the variability in scores and relationships within the model given the small number of items, although internal consistency was acceptable. Furthermore, there is some evidence that certain PTG items may not be as robustly associated with demographic factors, such as sex and age,1 which were the dominant predictive factors in this study. Had we selected different items, our results may well have been different. There also has been some recent criticism of how the construct of PTG is measured,37 which may also limit our ability to draw valid conclusions.
Finally, there is a lack of a theoretically driven conceptualization of PTG within the context of disability and SCI specifically.5 Our conceptual model was principally guided by the variables that were available for analysis, rather than a coherent theoretical underpinning. Because PTG is a complex phenomenon, expected relationships can be elusive and unexpected relationships illuminating. Such complexity requires the development of theoretical models, based on existing models, to more fully explain PTG after the onset of SCI. The development and/or modification of measurement tools to capture these constructs are key directions for future work.
Conclusions
Our final model suggested that, in our sample, certain personal and injury characteristics are related to PTG; however, the model explained only a small proportion of the variance in PTG. In order to more fully predict growth after SCI, a broader set of variables should be studied. Our item-level analysis also suggested that persons with SCI do experience growth after injury, similar to other trauma populations. These findings, in combination with the PTG literature in SCI and other disability populations, can help guide the development of more comprehensive, theoretical models for understanding and predicting PTG after injury.
Acknowledgements
The contents of this paper were developed under a grant from the US Department of Education, NIDRR grant number H133A060107. However, the contents do not necessarily represent the policy of the Department of Education, and you should not assume endorsement by the Federal Government. The authors thank Jason Barber, MS, for his work on this project.
References
- 1.Barskova T, Oesterreich R. Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil Rehabil 2009;31(21):1709–33 [DOI] [PubMed] [Google Scholar]
- 2.Tedeschi RG, Calhoun LG. Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 2004;15(1):1–18 [Google Scholar]
- 3.Christopher M A broader view of trauma: a biopsychosocial-evolutionary view of the role of the traumatic stress response in the emergence of pathology and/or growth. Clin Psychol Rev 2004;24(1):75–98 [DOI] [PubMed] [Google Scholar]
- 4.Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol 2006;74(5):797–816 [DOI] [PubMed] [Google Scholar]
- 5.Stoelb BL, Ehde DM. A systematic review of posttraumatic growth and benefit-finding in rehabilitation populations. Rehabil Psychol (in press) [Google Scholar]
- 6.North NT The psychological effects of spinal cord injury: a review. Spinal Cord 1999;37(10):671–9 [DOI] [PubMed] [Google Scholar]
- 7.Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009;47(2):108–14 [DOI] [PubMed] [Google Scholar]
- 8.Kessler R, Chiu W, Demler O, Walters E. Prevalence, severity, and comorbidity of 12-Month DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry 2005;62(6):617–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beedie A, Kennedy P. Quality of social support predicts hopelessness and depression post spinal cord injury. J Clin Psychol Med Settings 2002;9(3):227–34 [Google Scholar]
- 10.Charlifue S, Gerhart K. Behavioral and demographic predictors of suicide after traumatic spinal cord injury. Arch Phys Med Rehabil 1991;72:488–92 [PubMed] [Google Scholar]
- 11.Kennedy P, Evans M. Evaluation of post traumatic stress in the first 6 months following SCI. Spinal Cord 2001;39:381–6 [DOI] [PubMed] [Google Scholar]
- 12.Post MWM, van Leeuwen CMC. Psychosocial issues in spinal cord injury: a review. Spinal Cord 2012;50(5):382–9 [DOI] [PubMed] [Google Scholar]
- 13.Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P, Elfstrom ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol 2012;57(3):236–47 [DOI] [PubMed] [Google Scholar]
- 14.Kennedy P, Evans M, Sandhu N. Psychological adjustment to spinal cord injury: the contribution of coping, hope and cognitive appraisals. Psychol Health Med 2009;14(1):17–33 [DOI] [PubMed] [Google Scholar]
- 15.Chun S, Lee Y. The experience of posttraumatic growth for people with spinal cord injury. Qual Health Res 2008;18(7):877–90 [DOI] [PubMed] [Google Scholar]
- 16.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol 2011;7:511–35 [DOI] [PubMed] [Google Scholar]
- 17.Bonanno GA Uses and abuses of the resilience construct: loss, trauma, and health-related adversities. Soc Sci Med 2012;74(5):753–6 [DOI] [PubMed] [Google Scholar]
- 18.Catalano D, Chan F, Wilson L, Chiu CY, Muller VR. The buffering effect of resilience on depression among individuals with spinal cord injury: a structural equation model. Rehabil Psychol 2011;56(3):200–11 [DOI] [PubMed] [Google Scholar]
- 19.McMillen JC, Cook CL. The positive by-products of spinal cord injury and their correlates. Rehabil Psychol 2003;48(2):77–85 [Google Scholar]
- 20.Pollard C, Kennedy P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol 2007;12(Pt 3):347–62 [DOI] [PubMed] [Google Scholar]
- 21.Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9(3):455–71 [DOI] [PubMed] [Google Scholar]
- 22.Taku K, Cann A, Calhoun LG, Tedeschi RG. The factor structure of the posttraumatic growth inventory: a comparison of five models using confirmatory factor analysis. J Trauma Stress 2008;21(2):158–64 [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999;282(18):1737–44 [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR. Validity of the Patient Health Questionnaire-9 in assessing major depressive disorder during inpatient spinal cord Injury rehabilitation. Arch Phys Med Rehabil 2012;93(10):1838–45 [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD Patient Health Questionnaire in assessment of 3000 obstetric-gynecologic patients: The PRIME-MD Patient Health Questionnaire Obstetrics Gynecology Study. Am J Obstet Gynecol 2000;183(3):759–69 [DOI] [PubMed] [Google Scholar]
- 27.American Spinal Injury Association. Reference manual for the international standards for neurological classification of spinal cord injury. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 28.Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ, et al. The Cornell service index as a measure of health service use. Psychiatr Serv 2005;56(12):1564–9 [DOI] [PubMed] [Google Scholar]
- 29.Kline R.Principles and practice of structural equation modeling. 2nd ed New York, NY: Guilford; 2005 [Google Scholar]
- 30.Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 1999;6:1–55 [Google Scholar]
- 31.Kim KH The relation among fit indexes, power, and sample size in structural equation modeling. Struct Equ Model 2005;12(3):368–9 [Google Scholar]
- 32.Bombardier CH, Ehde DM, Stoelb B, Molton IR. The relationship of age-related factors to psychological functioning among people with disabilities. Phys Med Rehabil Clin N Am 2010;21(2):281–97 [DOI] [PubMed] [Google Scholar]
- 33.Cobb AR, Tedeschi RG, Calhoun LG, Cann A. Correlates of posttraumatic growth in survivors of intimate partner violence. J Trauma Stress 2006;19(6):895–903 [DOI] [PubMed] [Google Scholar]
- 34.Lechner SC, Zakowski SG, Antoni MH, Greenhawt M, Block K, Block P. Do sociodemographic and disease-related variables influence benefit-finding in cancer patients? Psychooncology 2003;12(5):491–9 [DOI] [PubMed] [Google Scholar]
- 35.Linley PA, Joseph S. Positive change following trauma and adversity: a review. J Trauma Stress 2004;17(1):11–21 [DOI] [PubMed] [Google Scholar]
- 36.Kleim B, Ehlers A. Evidence for a curvilinear relationship between posttraumatic growth and posttrauma depression and PTSD in assault survivors. J Trauma Stress 2009;22(1):45–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tennen H, Affleck G. Assessing positive life change: in search of meticulous methods. In: Park C, Lechner S, Antoni M, Stanton A (eds.) Medical illness and positive life change: can crisis lead to personal transformation? Washington, DC: American Psychological Association; 2009. p. 31–49 [Google Scholar]


