Abstract
Background
The central third of the face is distorted by the bilateral cleft of the lip and palate and restoring the normal facial form is one of the primary goals for the reconstructive surgeons. The history of bilateral cleft lip repair has evolved from discarding the premaxilla and prolabium and approximating the lateral lip elements to a definitive lip and primary cleft nasal repair utilising the underlying musculature. The aim of this study was to review surgical outcome of bilateral cleft lip surgery (BCLS) done at the Lagos University Teaching Hospital.
Materials and Methods
A review of all cases of BCLS done between January 2007 and December 2012 at the Lagos University Teaching Hospital was done. Data analysis included age and sex of patients, type of cleft deformity and type of surgery (primary or secondary) and whether the cleft deformity was syndromic and non-syndromic. Techniques of repair, surgical outcome and complications were also recorded.
Results
A total of 39 cases of BCLS involving 21 males and 18 females were done during the period. This constituted 10% (39/390) of all cases of cleft surgery done during the period. There were 5 syndromic and 34 non-syndromic cases. Age of patients at time of surgery ranged between 3 months and 32 years. There were 24 bilateral cleft lip and palate deformities and 15 bilateral cleft lip deformities. Thirty-one of the cases were primary surgery, while 8 were secondary (revision) surgery. The most common surgical technique employed was modified Fork flap (Millard) technique, which was employed in 37 (95%) cases.
Conclusion
Bilateral cleft lip deformity is a common cleft deformity seen in clinical practice, surgical repair of which can be a challenge to an experienced surgeon. A modified Fork flap for repair of bilateral cleft lip is a reliable and versatile technique associated with excellent surgical outcome.
Keywords: Bilateral, cleft lip, outcome
INTRODUCTION
Cleft lip and palate is one of the most common occurring craniofacial developmental abnormalities.[1] The incidence of these anomalies has been reported to vary according to race, gender and cleft type. Bilateral clefts (BLC) occur in approximately 1 in 5000–6500 births based on the overall occurrence.[1,2] The presence of bilateral cleft lip and palate has the potential to significantly alter facial form and structure. This causes cosmetic, feeding, speech and dental development problems and this deformity has significant psychosocial consequences.[3,4]
The central third of the face is commonly distorted by the bilateral cleft and restoring the normal facial form is one of the primary goals for the reconstructive surgeon. Reconstructive surgery aims to restore form and function and modern techniques can leave many defects undetectable. Early lip closure in young age has been advocated to avoid unwanted anxiety and psychological impacts on child and family.[3]
The history of bilateral cleft lip repair has evolved from discarding the premaxilla and prolabium and approximating the lateral lip elements to a definitive lip and primary cleft nasal repair utilising the underlying musculature.[5] Accompanying this evolution is the increasingly important role of orthodontic support with early pre-surgical nasoalveolar molding.[6] Repositioning the maxillary and alveolar segments into a more anatomic position allows the surgeon to repair the lip and associated nasal deformity under more optimal conditions.[6]
The first reports of bilateral cleft lip repair emerged in the 14th century and were performed by the Belgian surgeon Johan Yperman.[6] Since then, several other surgical techniques have been employed for BCL repair. These includes Millard’s technique, Manchester technique and Tennisson technique.[6] The Millard’s repair involved complete elevation of the prolabium and reconstitution of the orbicularis across the premaxilla.[6–8] In addition, Millard banked lateral segments of the prolabium as “forked flaps” that were meant to add collumellar height at a later stage. This technique has more universal application and has been adjusted to give more satisfactory clinical result, the banking of the lateral component of the prolabium however give unsightly scar especially in the dark-skinned individuals, which are more prone to excessive scar formation.[9] A modification of this technique is therefore necessary to achieve a more esthetic result especially in this group of patients.
The aim of this study was to review the surgical outcome of bilateral cleft lip surgery (BCLS) done using modified fork flap technique at the Lagos University Teaching Hospital.
MATERIALS AND METHODS
A retrospective review of all cases of BCLS done between January 2007 and December 2012 at the Lagos University Teaching Hospital was done. All cases were done under general anaesthesia with orotracheal intubation. Data retrieved from the hospital record for analysis included sex of patients, month of birth; type cleft deformity, technique of repair (either lip adhesion or Modified Millar0d’s technique) and surgical outcome including complications. Modified Millard’s technique involves complete elevation of the prolabium and reconstitution of the orbicularis across the premaxilla without banking of lateral segments of the prolabium.
Data collected was subjected to simple statistical analysis using the Statistical Package for Social Sciences (SPSS), SPSS® for Windows, version 16.0 (SPSS Inc., Chicago, IL) statistical software package. Frequencies and means of the variables were estimated. Some pre-operative, intra operative and post-operative clinical photographs were also retrieved and are presented.
RESULT
A total of 390 patients were managed for cleft lip and palate deformity during the period. Thirty-nine (10%) of these were BCLS out of which 5 were syndromic and 34 non-syndromic cases. There were 18 females and 21 males. Age of patients at time of surgery ranged between 3 and 384 months with the mean age of 52 ± 104.34 months. There were 24 bilateral cleft lip and palate deformities and 15 bilateral cleft lip deformities. Majority of the subjects (89.7%) had complete cleft lip deformity.
The most common surgical technique employed was Modified Millard’s technique, which was employed in 37 (95%) cases. Lip adhesion was the technique of choice in 2 (5%) cases. Thirty-one (79.5%) of the cases were primary surgery while 8 (20.5%) were secondary (revision) surgery. All patients were admitted for a period of 7 days.
Surgical outcome was considered satisfactory if there were: Adequate length of the upper lip, symmetrical nostrils, reconstituted philtrum and adequate columella length. Surgical outcome was considered satisfactory in 37 (95%) of the 39 cases while four cases need further surgical revision. The four cases were: All the 2 cases repaired with lip adhesion technique and 2 of 37 cases repaired with Modified Millard’s technique. Columella shortening was a major drawback in Modified Millard technique and obvious in all cases immediate post-operation. However, improvement was noticed over time. Figures 1–5 show the pre-operative and post-operative photographs of patients with BCL repair using Modified Millard’s Technique.
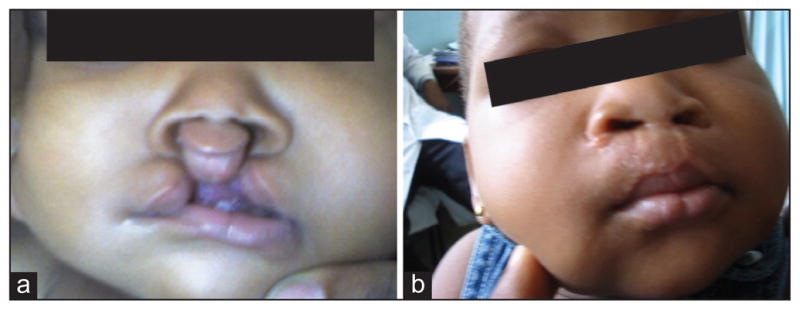
Figure 1.

(a) A 3-month old girl with a complete bilateral cleft lip deformity. (b) The same patient 6 months after repair
Figure 5.

(a) A 27-year old female requiring secondary repair of a previously repaired bilateral cleft lip deformity. (b) The same patient 2 weeks after repair
DISCUSSION
Bilateral cleft lip deformity is a common cleft deformity seen in clinical practice, surgical repair of which can be a challenge to an experienced surgeon. The most striking feature of BCL is the premaxilla, which for centuries has been assailed as the principal obstacle to closure; the excision was therefore advised and practiced for many years.[8] The surgical repair of bilateral cleft lip repair has however evolved from discarding the premaxilla and prolabium and approximating the lateral lip elements to a definitive lip and primary cleft nasal repair utilising the underlying musculature.[7–9]
Mulliken 1985 described the basic principles for BLC repair, which are maintaining nasolabial symmetry, securing orbicularis oris continuity to construct the muscular ring and minimise philtral distortion, designing proper philtral size/shape, construct the median tubercle using the lateral labial elements, position and secure the displaced lower lateral cartilages to establish normal nasal projection and columellar length.[10,11]
The surgical repair of BCL is complex and still controversial, though various techniques have been reported and described in detail.[11] The results of primary repair of bilateral cleft lip traditionally have been less satisfactory than those of unilateral cleft lip. The typical labial stigmata are a broad, bowed and undimpled philtrum, lateral muscular bulges and a thin median tubercle, accentuated by hanging lateral labial elements.[12] Established and well-described surgical procedures though with many variations for the repair of bilateral cleft lip include the repairs of Veau, Tennison, Manchester and Millard.[6,7]
Millard’s repair involved complete elevation of the prolabium and reconstitution of the orbicularis across the premaxilla.[6] In addition, Millard banked lateral segments of the prolabium as “forked flaps” that were meant to add columellar height at a later stage.[6] The prolabium is an important component in BCL repair, Millard has earlier stressed that in BLC of the lip, the prolabium regardless of its size should always be positioned to the vermilion boarder. While Millard’s technique advocated the complete elevation of the prolabium and reconstitution of the orbicularis across the premaxilla with banking of lateral segments of the prolabium; however, the Modified Millard’s Technique complete the repair without banking of lateral segments of the prolabium.
The surgical outcome was assessed as achieving adequate length of the upper lip, symmetrical nostrils, reconstructed nasal floor without excessive scar tissue, reconstituted philtrum and philtral ridges.
In our surgical plan, after raising a forked flap (two lateral elements and one central element), the lateral element of the prolabium is discarded; the median element is used to reconstruct the philtrum and the philtral ridges. A careful muscle dissection and more anatomical repair gave us good shape of the bilateral lip repair. The obvious drawback of this technique is the loss of lateral element, which could be used for the lengthening of the columella. However, a secondary rhinoplasty can be done later in life if the need arises.
CONCLUSION
A Modified Millard’s Technique (without banking of lateral elements) for bilateral cleft lip cheilorrhaphy is a reliable and versatile technique associated with excellent surgical outcome. The clinical results showed less scar formation, adequate length of the upper lip and reconstituted symmetrical nostrils.
Figure 2.
(a) A 3-month old boy with an incomplete bilateral cleft lip deformity. (b) The same patient at the age of 11 months
Figure 3.
(a) A 3-month old girl with a complete bilateral cleft lip deformity. (b) The same patient 6 months after repair
Figure 4.
(a) A 3-month old boy with a complete bilateral cleft lip deformity. (b) The same patient 5 months after repair
References
- 1.Turner SR, Rumsey N, Sandy JR. Psychological aspects of cleft lip and palate. Eur J Orthod. 1998;20:407–15. doi: 10.1093/ejo/20.4.407. [DOI] [PubMed] [Google Scholar]
- 2.Bartzela TN, Carels CE, Bronkhorst EM, Rønning E, Rizell S, Kuijpers-Jagtman AM. Tooth agenesis patterns in bilateral cleft lip and palate. Eur J Oral Sci. 2010;118:47–52. doi: 10.1111/j.1600-0722.2009.00698.x. [DOI] [PubMed] [Google Scholar]
- 3.Bitter K. Repair of bilateral clefts of lip, alveolus and palate. Part 2: Concomitant lip closure and columella lengthening after lip adhesion. J Craniomaxillofac Surg. 2001;29:44–8. doi: 10.1054/jcms.2000.0186. [DOI] [PubMed] [Google Scholar]
- 4.Bitter K. Repair of bilateral cleft lip, alveolus and palate. Part 3: Follow-up criteria and late results. J Craniomaxillofac Surg. 2001;29:49–55. doi: 10.1054/jcms.2000.0185. [DOI] [PubMed] [Google Scholar]
- 5.Precious DS, Goodday RH, Morrison AD, Davis BR. Cleft lip and palate: A review for dentists. J Can Dent Assoc. 2001;67:668–73. [PubMed] [Google Scholar]
- 6.Millard DR., Jr Closure of bilateral cleft lip and elongation of columella by two operations in infancy. Plast Reconstr Surg. 1971;47:324–31. doi: 10.1097/00006534-197104000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Elhadidy AM, Eldeen AM, Elbassiouny L. An improved technique for repair of bilateral cleft lip deformities through extensive muscle dissection in one stage surgery Egypt. J Plast Reconstr Surg. 2006;30:131–7. [Google Scholar]
- 8.Holdsworth WG. Cleft Lip and Palate. 4. London: Heinemann (Medical Books) Ltd; 1973. pp. 81–94. [Google Scholar]
- 9.Chike-Obi CJ, Cole PD, Brissett AE. Keloids: Pathogenesis, clinical features, and management. Semin Plast Surg. 2009;23:178–84. doi: 10.1055/s-0029-1224797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mulliken JB. Repair of bilateral cleft lip and its variants. Indian J Plast Surg. 2009;42 (Suppl):S79–90. doi: 10.4103/0970-0358.57194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aziz SR, Rhee ST, Redai I. Cleft surgery in rural Bangladesh: Reflections and experiences. J Oral Maxillofac Surg. 2009;67:1581–8. doi: 10.1016/j.joms.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 12.Padwa BL, Mulliken JB. Complications associated with cleft lip and palate repair. Oral Maxillofac Surg Clin North Am. 2003;15:285–96. doi: 10.1016/S1042-3699(02)00103-6. [DOI] [PubMed] [Google Scholar]




