Abstract
INTRODUCTION
Thrombosis of the inferior vena cava (IVC) is governed by Virchow's triad of stasis of blood flow, endothelial damage and hypercoagulability. Causes may be secondary to malignancy, congenital anomalies or other infrequent events such as external compression. We present a case of external compression of the IVC leading to extensive thrombus burden secondary to a benign hepatic cyst.
PRESENTATION OF CASE
A 72 year old African American female presented to the emergency department with new onset shortness of breath, right lower extremity weakness and swelling. CT imaging demonstrated multiple hepatic cysts compressing the IVC, leading to extensive clot burden. Treatment with heparin drip was initiated without resolution of her symptoms. Transcatheter mechanical thrombectomy and tPA infusion was performed. After 24 h, swelling and weakness were nearly resolved. The patient was bridged to therapeutic low molecular weight heparin in preparation for surgery.
DISCUSSION
Management of IVC thrombosis has typically been with a heparin drip and transition to oral anticoagulants. Thrombolysis has been shown to promote complete clot lysis more often than compared to standard anticoagulant therapy. In addition, venous patency was better maintained.
CONCLUSION
We feel that the added benefit of short term effects of improved venous patency and long term benefits of less post thrombotic syndrome, catheter based tPA administration and mechanical thrombectomy for thrombus offers an adjuvant treatment in the setting of large clot burden refractory to standard treatment.
Introduction
Thrombosis of the inferior vena cava (IVC) is governed by Virchow's triad of stasis of blood flow, endothelial damage and hypercoagulability.1 Thrombosis is typically an extension of a deep vein thrombosis; however, there are other isolated causes of occlusion. Thrombus causing occlusion of the inferior vena cava (IVC) is a known complication of malignancy, whether due to the hypercoaguable state that malignancy produces or due to the direct extension of the tumor burden.2 Benign causes of occlusion are a rarer event. They may be due to internal occlusion, as such the case with membranous obstruction of the IVC. Occlusion may be due to congenital anomalies such as an absent hepatic segment of the IVC or double inferior vena cava with narrowing. External compression is a known, but infrequent cause of IVC occlusion leading to thrombosis. This has been documented as a result of retroperitoneal tumors, hepatic hydatid cysts, non-parasitic liver cyst, intra-cystic hemorrhage into a hepatic cyst, polycystic kidneys, hepatic trauma and ruptured abdominal aortic aneurysm.2–6
Presentation of case
A 72 year old African American female presented to her primary care physician with lower abdominal pain, constipation and anorexia: CT evaluation showed multiple hepatic cysts. She was scheduled for elective resection when she presented to the emergency department.
On presentation she complained of new onset shortness of breath, right lower extremity weakness and swelling. Repeat imaging showed interval enlargement of her hepatic cysts and compression of the IVC (Fig. 1). Lab evaluation demonstrated acute renal failure and elevated liver enzymes. Vascular duplex demonstrated a right common femoral clot from her trifurcation extending up to the midsegment of the left renal vein and severe external compression on her intrahepatic segment of the IVC. Anticoagulation was initiated with heparin drip. The patient underwent simultaneous percutaneous drainage of the hepatic cyst and suprarenal IVC filter placement by interventional radiology.
Fig. 1.
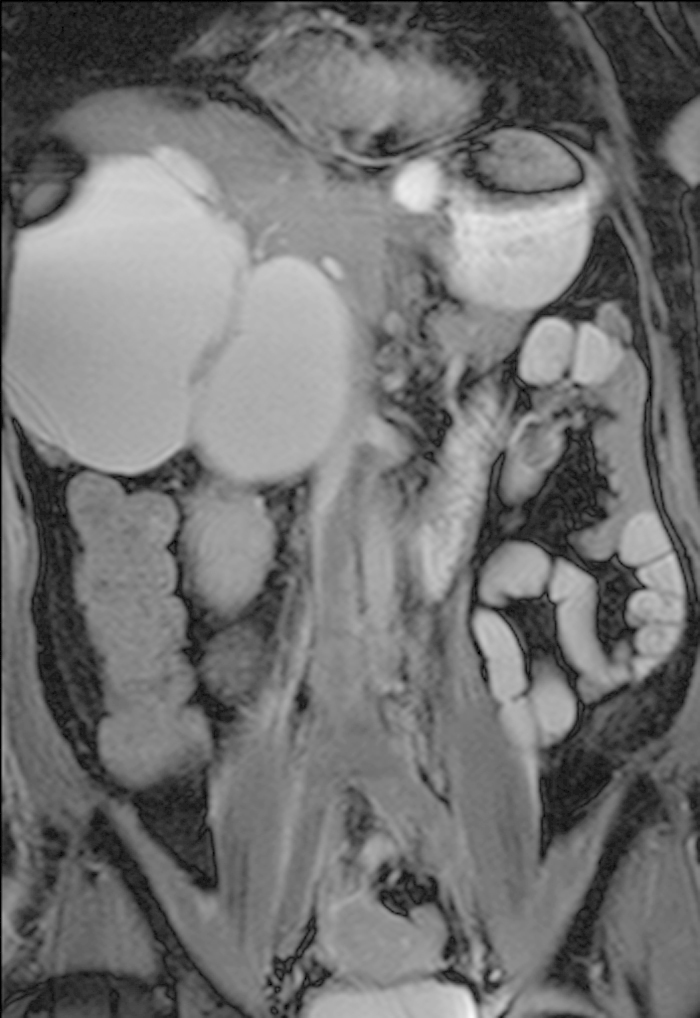
Simple hepatic cysts causing IVC compression and extensive thrombus burden.
Symptoms of renal failure, extremity swelling and weakness persisted 48 h while on heparin drip. Therefore, transcatheter mechanical thrombectomy of the inferior vena cava and right lower extremity with tissue plasminogen activator (tPA) infusion was performed. Post procedure venogram demonstrated near resolution of the clot burden. She was recovered in ICU with a continuous tPA infusion via popliteal sheath. Infusion was continued for 24 h with monitoring of fibrinogen levels.
Overnight the patients’ lower extremity swelling and weakness nearly resolved. In addition renal function trended back to baseline. She was discharged on therapeutic low molecular weight heparin in preparation for surgery. Subsequent imaging two weeks post discharge demonstrated continued resolution of the IVC thrombus (Fig. 2). Of note, one of the hepatic cysts had enlarged after the percutaneous drains had been removed prior to the patients discharge. She subsequently underwent laparoscopic wide cyst fenestration of segments 2, 4 and 8. Post intervention she was begun on low molecular weight heparin with bridging to warfarin.
Fig. 2.

Patent IVC post thrombectomy and tPA infusion.
Discussion
Management of IVC thrombus has typically been with a heparin drip and transition to oral anticoagulants. Iguchi et al. demonstrated a similar presentation of compression leading to obstruction from a hepatic cyst with intra-cystic hemorrhage that was managed with a heparin drip and bridging to warfarin.6 England et al., demonstrated the extremes of treatment for this condition, from oral anticoagulation alone to open operative removal of clot burden.2 We present the first case of management of IVC thrombus secondary to external compression by a simple hepatic cyst by means of tPA infusion and mechanical thrombectomy. After 24 h of therapy the patients’ renal function improved and her lower extremity edema and weakness started to resolve. Although a plausible treatment, this technique is not without complication. Bleeding complications have been greater in those treated with thrombolysis therapy. With stricter exclusion criteria as well as catheter directed systems as opposed to systemic treatment, the risk has decreased. With catheter directed tPA this allows for swifter resolution of clot burden.7 Subsequent definitive cyst treatment therefore can occur at an earlier time, an important point as these cysts have a high recurrence rate with just drainage alone. Of note if percutaneous drainage prior to definitive surgical treatment is required to relieve compressive symptoms, it is important to place the IVC filter first. This to prevent emboli once the compression on the IVC is relieved. With the advent and improvement in laparoscopy, laparoscopic surgical treatment is now a viable option for cyst treatment. As described by Kashiwagi et al., single site procedures may also be a feasible treatment option.8 Care must be taken, however, if laparoscopy is chosen. In the setting of IVC thrombus, insufflation in itself can propagate clot formation. Therefore completion angiography prior to tPA catheter removal and surgical planning should be performed to show clot resolution.
Conclusion
We feel that the added short term benefit of improved venous patency and long term benefits of fewer post thrombotic syndrome, catheter based tPA administration and mechanical thrombectomy for thrombus offers an adjuvant treatment in the setting of large clot burden refractory to standard treatment.
Conflict of interest
There are no financial or personal relationships with any organization that any of the authors have to declare.
Funding
None
Consent
Written informed consent was obtained from the patient for publication of this case report and case series and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Matthew Musielak–Study concept, data analysis, writing paper
Ranjodh Singh – Study concept, data analysis, writing paper
Elizabeth Hartman – Data collection
Joseph Bernstein – Study concept, data analysis
Key learning points
- tPA and mechanical thrombectomy offer adjuvant treatment in refractory thrombus, - IVC filter deployment should precede cyst aspiration, - Laparoscopy cyst fenestration is a viable option
References
- 1.Brunicardi F.C., Seymour I.S. McGraw-Hill; Health Pub. Division, New York: 2005. Venous and lymphatics disease. Schwartz's principles of surgery, Chap. 24; pp. 777–801. [Google Scholar]
- 2.England R.A., Wells I.P., Gutteridge C.M. Benign external compression of the inferior vena cava associated with thrombus formation. Brit J Radiol. 2005;78:553–557. doi: 10.1259/bjr/21010811. [DOI] [PubMed] [Google Scholar]
- 3.Okuda K. Membranous obstruction of the inferior vena cava. J Gastroenterol Hepatol. 2001;16(11):1179–1183. doi: 10.1046/j.1440-1746.2001.02577.x. [DOI] [PubMed] [Google Scholar]
- 4.Skandalakis J., Colborn G., Weidman T., Skandalakis L., Skandalakis P., Smith R., III . Chapter 12. Great vessels in the abdomen. In: Skandalakis J.E., Colburn G.L., Weidman T.A., Foster R.S. Jr., Kingsworth A.N., Skandalakis L.J., Skandalakis P.N., Mirilas P.S., editors. Skandalakis’ surgical anatomy. McGraw-Hill; New York: 2004. [Google Scholar]
- 5.Chee Y., Culligan D., Watson H. Inferior vena cava malformation as a risk factor for deep venous thrombosis in the young. Brit J Haematol. 2001;114(4):878–880. doi: 10.1046/j.1365-2141.2001.03025.x. [DOI] [PubMed] [Google Scholar]
- 6.Iguchi S., Kasai A., Kishimoto H., Suzuki K., Ito S., Ogawa Y., Nishi S., Gejyo F., Ohno Y. Thrombosis in inferior vena cava (IVC) due to intra-cystic hemorrhage into a hepatic local cyst with autosomal dominant polycystic kidney disease (ADPKD) Intern Med. 2004;43(3):209-212. doi: 10.2169/internalmedicine.43.209. [DOI] [PubMed] [Google Scholar]
- 7.Watson L., Broderick C., Armon M.P. Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst Rev. 2014;1:1–74. doi: 10.1002/14651858.CD002783.pub3. [DOI] [PubMed] [Google Scholar]
- 8.Kashiwagi H., Kumagai K., Nozue M. Single incision laparoscopic surgery for a life-threatening, cyst of liver. Tokai J Exp Clin Med. 2011 Apr 20;36(1):13–16. [PubMed] [Google Scholar]


