Abstract
INTRODUCTION
Gastric polyps are usually found incidentally during upper gastrointestinal endoscopic examinations. These polyps are generally benign, with hyperplasia being the most common. While gastric polyps are often asymptomatic, they can cause gastric outlet obstruction.
PRESENTATION OF CASE
A 64 years-old female patient presented to our polyclinic with a history of approximately 2 months of weakness, occasional early nausea, vomiting after meals and epigastric pain. A polypoid lesion of approximately 25 mm in diameter was detected in the antral area of the stomach, which prolapsed through the pylorus into the duodenal bulbus, and subsequently caused gastric outlet obstruction, as revealed by upper gastrointestinal endoscopy of the patient. The polyp was retrieved from the pyloric canal into the stomach with the aid of a tripod, and snare polypectomy was performed.
DISCUSSION
Currently, widespread use of endoscopy has led to an increase in the frequency of detecting hyperplastic polyps. While most gastric polyps are asymptomatic, they can cause iron deficiency anemia, acute pancreatitis and more commonly, gastric outlet obstruction because of their antral location. Although there are no precise principles in the treatment of asymptomatic polyps, polyps >5 mm should be removed due to the possibility of malignant transformation.
CONCLUSION
According to the medical evidence, polypectomy is required for gastric hyperplastic polyps because of the risks of complication and malignancy. These cases can be successfully treated endoscopically.
Keywords: Hyperplastic polyp, Gastric outlet obstruction, Endoscopic polypectomy
1. Introduction
Gastric polyps are detected incidentally at a rate of 2–3% during upper gastrointestinal (GI) endoscopic examination.1 These polyps are mostly benign and of inflammatory, regenerative or hyperplastic types.2,3 The most common type of gastric polyp is hyperplastic, which accounts for 85–90% of all cases.1,4 Adenomas account for only 5–10% of gastric polyps, and less than 1% of these lesions are reported to have malignant changes.5 These polyps can be pedunculated or sessile and are generally less than 20 mm in diameter.4 While gastric polyps are commonly asymptomatic, they can cause dyspepsia, epigastric pain, bleeding due to ulceration, anemia and gastric outlet obstruction.6
We present a patient with complaints of epigastric pain, nausea and vomiting after meals, who developed intermittent gastric outlet obstruction by an antral gastric polyp as revealed by endoscopy.
2. Presentation of case
A 64 year-old female patient presented to our polyclinic with a history of approximately 2 months of weakness, occasional early nausea, vomiting after meals and epigastric pain. Physical examination revealed no pathological findings other than mild epigastric tenderness in the upper abdomen. Laboratory examinations of the patient showed the blood values to be normal, with the exception of a hemoglobin level of 10.9 mg/dL and a haematocrit of 35.6%. The fecal occult blood test was negative, and colonoscopy of this patient was normal.
On upper gastrointestinal endoscopy, a polypoid lesion of approximately 25 mm in diameter was detected in the antrum of the stomach, which prolapsed through the pylorus into the duodenal bulbus to form gastric outlet obstruction (Fig. 1). The polyp was retrieved from the pyloric canal into the stomach with the aid of a tripod, and snare polypectomy was performed (Fig. 2). Histopathological examination of the polyp revealed cystic, dilated glandular structures, edema and mild inflammation (Fig. 3). No findings suggesting intestinal metaplasia, dysplasia or malignancy were detected. The patient was tested positive for Helicobacter pylori which was treated. This case was diagnosed as a hyperplastic polyp, and no pathology was found in the follow-up endoscopy performed 2 months later.
Fig. 1.
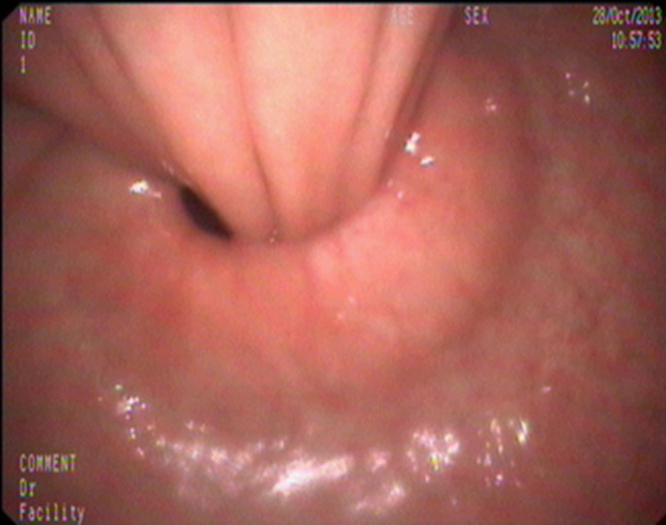
Endoscopic image of the polyp, which prolapsed through the pylorus into the duodenal bulbus and, subsequently, created gastric outlet obstruction.
Fig. 2.

Endoscopic image shows the polyp retracted into the stomach from the pyloric canal.
Fig. 3.
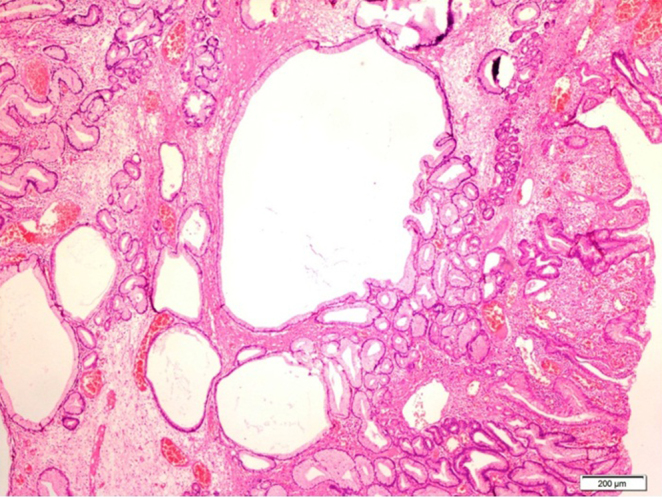
Light microscopic image shows cystic dilated glandular structures, inflammation and edema in the stroma (H&E, 40×).
3. Discussion
Currently, widespread use of endoscopy has led to an increase in the detection of hyperplastic polyps, which account for approximately of 85–90% of all gastric polyps. They are generally seen in adults >60 years old.1,4 Polyps are lesions that are sessile or pedunculated, solitary and pinkish in color. While most gastric polyps are asymptomatic, they can cause iron deficiency anemia, acute pancreatitis due to compression of ampulla of Vater following prolapse into the duodenum, and more commonly, gastric outlet obstruction because of their antral location.7,8
Most gastric hyperplastic polyps are <20 mm, and the risks of complications such as obstruction and bleeding increase with increased polyp diameter.9 In this case, the polyp diameter was 25 mm, which caused both gastric outlet obstruction and anemia. Although in the medical literature there are reports of iron deficiency anemia due to bleeding,7 in this case, the iron and iron-binding values were within normal ranges. At the time of the gastric outlet obstruction, there were no clinical findings in the patient other than epigastric pain and occasional vomiting. However, there were periods when no symptoms were experienced. Although we believed that the anemia developed due to the polyp, in order to exclude colonic pathologies, the patient also received colonoscopy to rule out any colorectal pathologies.
There are still no generally accepted principles in the treatment of asymptomatic polyps, polyps >5 mm should be removed due to the possibility of malignant transformation. Some authors recommend endoscopic follow-ups in patients with small hyperplastic polyps to avoid polypectomy complications,10 while some other authors stated that biopsy samples obtained with forceps are misleading with respect to the polyp diameter and histopathology.11 In this case, polypectomy was performed.
The treatment of gastric polyps is excision, either endoscopically or surgically. Currently, endoscopic polypectomy is the recommended treatment.11,12 In endoscopic excision, the procedure becomes difficult with increase in polyp diameter, and complications such as bleeding and perforation may occur.13 There may also be some difficulties in retrieving the polyps that have prolapsed into the duodenum. In this case, we encountered a problem while retrieving the polyp into stomach, which was then solved with the aid of a tripod. Polypectomy was completed without any complications with a snare
In some studies, there have been reports of co-existing of H. pylori and hyperplastic polyps. It has been reported that eradication of H. pylori resulted in regression of the existing polyps, and prevented new polyp to develop.14,15 Since this case was positive for H. pylori, medical treatment for eradication and monitoring were initiated.
4. Conclusion
According to the medical evidence, polypectomy is required for a gastric hyperplastic polyp because of the risks of complication and malignancy, and these cases can be successfully treated endoscopically. Endoscopic polypectomy allows for histopathological diagnosis of the polyp and relief of the patient's symptoms. This also prevents any possible polyp-related complications. These patients should be monitored for pathologies that may have been overlooked or may develop in the future.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest
The authors declare that there is no conflict of interest in under-taking this study.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Ibrahim Aydin and Ender Ozer: surgery, writing; Halil Rakici: medical and endoscopical management; Ibrahim Sehitoglu: histopathological evaluation; Ahmet Fikret Yucel, Ahmet Pergel and Dursun Ali Sahin: writing and revision.
References
- 1.Silverstein F.E., Tytgat G.N.J. Stomach II: tumors and polyps. In: Silverstein F.E., Tytgat G.N.J., editors. Gastrointestinal endoscopy. Mosby; London: 1997. pp. 147–180. [Google Scholar]
- 2.Tomasulo J. Gastric polyps: histological types and their relationship to gastric carcinoma. Cancer. 1971;27:1346–1355. doi: 10.1002/1097-0142(197106)27:6<1346::aid-cncr2820270612>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 3.Zea-Iriarte W., Sekine I., Itsuno M., Makiyama K., Naito S., Nakayama T. Carcinoma in gastric hyperplastic polyps. A phenotypic study. Dig Dis Sci. 1996;41:377–386. doi: 10.1007/BF02093832. [DOI] [PubMed] [Google Scholar]
- 4.Owen D.A. The stomach. In: Sternberg S.S., editor. Diagnostic surgical pathology. Lippincott Williams & Wilkins; Philadelphia: 1999. pp. 1311–1347. [Google Scholar]
- 5.Kamiya T., Morishita T., Asakura H., Miura S., Munakata Y., Tsuchiya M. Long-term follow-up study on gastric adenoma and its relation to gastric protruded carcinoma. Cancer. 1982;50:2496–2503. doi: 10.1002/1097-0142(19821201)50:11<2496::aid-cncr2820501140>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Sun C.-K., Yang K.-C., Liao C.-S. Endoscopic management of gastric polyp with outlet obstruction without polypectomy. Case Rep Gastroenterol. 2011;5:267–271. doi: 10.1159/000328443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de la Cruz R.A., Albillos J.C., Oliver J.M., Dhimes P., Hernandez T., Trapero M.A. Prolapsed hyperplastic gastric polyp causing pancreatitis: case report. Abdom Imaging. 2001;26:584–586. doi: 10.1007/s00261-001-0014-y. [DOI] [PubMed] [Google Scholar]
- 8.Alper M., Akcan Y., Belenli O. Large pedunculated antral hyperplastic gastric polyp traversed the bulbus causing outlet obstruction and iron deficiency anemia: endoscopic removal. World J Gastroenterol. 2003;9:633–634. doi: 10.3748/wjg.v9.i3.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parikh M., Kelley B., Rendon G., Abraham B. Intermittant gastric outlet obstruction caused by a prolapsing antral gastric polyp. World J Gastrointest Oncol. 2010;2:242–246. doi: 10.4251/wjgo.v2.i5.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muchldorfer S.M., Stolte M., Martus P., Hahn E.G., Ell C. Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut. 2002;50:465–470. doi: 10.1136/gut.50.4.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szaloki T., Toth V., Nemeth I., Tiszlavicz L., Lonovics J., Czako L. Endoscopic mucozal resection: not only therapoutic, but a diagnostic procedure for sessile gastric polyps. J Gastroenterol Hepatol. 2008;23:551–555. doi: 10.1111/j.1440-1746.2007.05247.x. [DOI] [PubMed] [Google Scholar]
- 12.Dang S., McElreath D.P., Kumar S. “Giant gastric hyperplastic polyp: not always a benign lesion. J Ark Med Soc. 2010;107(5):89–92. [PubMed] [Google Scholar]
- 13.Katsinelos P., Beltsis A., Paroutoglou G., Galanis I., Tsolkas P., Mimidis K. Endoclipping for gastric perforation after endoscopic polypectomy: an alternative treatment to avoid surgery. Surg Laparosc Endosc Percutan Tech. 2004;14:279–281. doi: 10.1097/00129689-200410000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Gencosmanoglu R., Sen-Oran E., Kurtkaya-Yapicier O., Tozun N. Antral hyperplastic polyp causing intermittent gastric outlet obstruction: case report. BMC Gastroenterol. 2003;3:16. doi: 10.1186/1471-230X-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ljubicic N., Banic M., Kujundzic M., Antic Z., Vrkljan M., Kovacevic I. The effect of eradicating Helicobacter pylori infection on the course of adenomatous and hyperplastic gastric polyps. Eur J Gastroenterol Hepatol. 1999;11:727–730. doi: 10.1097/00042737-199907000-00008. [DOI] [PubMed] [Google Scholar]


