Abstract
INTRODUCTION
In the majority of subchondral insufficiency fractures (SIFs) of the femoral head, T1-weighted magnetic resonance imaging shows an irregular, serpiginous, low-intensity band that is convex to the articular surface. We report a case of a cystlike formation in SIF of the femoral head in an elderly woman.
PRESENTATION OF CASE
A 71-year-old woman reported right hip pain without any history of antecedent trauma. The initial radiograph showed a slight narrowing of the joint space in the right hip. The patient was treated with conservative therapy for 2 months. Radiographs obtained 3 months after the onset of pain showed non-progressive joint-space narrowing. T1-weighted magnetic resonance images obtained 2 months after pain onset revealed a round, cystlike, low-intensity area just beneath the articular cartilage. The patient underwent total hip arthroplasty. Histopathological examination showed fracture callus and granulation tissue in the subchondral area, surrounded by vascular-rich granulation tissue and fibrous tissue, which corresponded to the round, low-intensity band observed on the T1-weighted image.
DISCUSSION
This case was a rare SIF of the femoral head which had a cystlike formation with a low signal intensity on T1-weighted images and a very high signal intensity on STIR sequences in the superolateral portion of the femoral head, surrounded by a pattern of edema in the bone marrow. To our knowledge, no similar cases were cited in the literature.
CONCLUSION
It is important for surgeons to keep in mind that sometimes SIFs of the femoral head can appear as a round cystlike formation.
Keywords: Subchondral insufficiency fracture, Femoral head, Histopathology
1. Introduction
Subchondral insufficiency fractures (SIFs) of the femoral head occur mainly in elderly women with osteoporosis.1,2 In the majority of patients, radiographs obtained at the onset of hip pain show no obvious findings, but T1-weighted magnetic resonance imaging (MRI) reveals an irregular, serpiginous, low-intensity band that is convex to the articular surface.1–4 This band histologically corresponds to a fracture line, and it is also one of the characteristic findings in SIF.5 We report herein a case of SIF in which a cystlike formation was seen on magnetic resonance images in addition to a pattern of edema in the bone marrow.
2. Presentation of case
A 71-year-old-woman presented with a 1-month history of right hip pain without any history of antecedent trauma. She had no history of corticosteroid therapy or alcoholism. Her height was 150 cm, and at a weight of 51.0 kg and a body mass index of 22.7 kg/m2, she was not overweight.6 The range of motion in her right hip was 100° in flexion, 10° in extension, 30° in abduction, 20° in adduction, 20° in external rotation, and 0° in internal rotation. Her values on laboratory tests—C-reactive protein, lipid profile, liver and renal function, alkaline phosphatase, serum calcium and phosphorus, and clotting function—were all within normal ranges. Furthermore, findings were negative for rheumatoid factor and anticyclic citrullinated peptide antibodies. Her bone mineral density, measured by dual X-ray absorptiometry, was 0.739 g/cm2 (T score, −2.5) for her lumbar spine and 0.576 g/cm2 (T score, −2.1) for her right femoral head. Initial radiographs obtained 1 month after pain onset revealed mild acetabular dysplasia [center-edge angle,7 15°; inclination angle of the weight-bearing portion of the acetabulum,8 13°] and joint-space narrowing in the weight-bearing area (Fig. 1). There was no history of any corticosteroid intake. Also, No evidence of malignancy, infection or inflammatory diseases was noted. The patient was treated with an intra-articular injection (1.65 mg of dexamethasone sodium phosphate and 3 ml of 0.5% lidocaine) and instructed to take an anti-inflammatory drug (loxoprofen, 60 mg, three times daily). However those treatments only relieved her temporarily. At 2 months after the onset of hip pain, radiographs showed no significant changes since the initial radiographs (Fig. 2A). Computed tomography (CT) showed a cystlike formation in the superolateral portion of the femoral head, facing the acetabular rim (Fig. 2B). MRI showed a low signal intensity on T1-weight images and a very high signal intensity on the short τ inversion recovery (STIR) sequence of the superolateral portion of the femoral head, which was surrounded by a pattern of edema in the bone marrow. The edema pattern was found not only in the femoral head but also in the acetabulum facing the cystic lesion on the femoral head (Fig. 2C, D). Interestingly, although radiographs obtained just before surgery showed no remarkable changes (Fig. 3A), MRI performed at the same time showed that the edema pattern had been slightly alleviated compared with 1 month earlier (Fig. 3B, C). Three months after the onset of hip pain, we performed a total hip arthroplasty for the patient because of her persistent pain (Fig. 4). During surgery, we found an inverted labrum (Fig. 5A) with degenerative changes in the acetabular cartilage just beneath it (Fig. 5B). Similarly, there were degenerative changes of the femoral head cartilage on the superolateral portion, which corresponded to the area of the inverted labrum (Fig. 5C). A midcoronal cross-section showed a round, whitish gray mass of tissue under the cartilage (Fig. 6A). There was no well-demarcated, wedge-shaped, opaque yellow necrotic region, such as is seen in osteonecrosis.9 Microscopically, the whitish gray region consisted of fracture callus and granulation tissue (Fig. 6B), which corresponded to the round, low-intensity area on T1-weighted magnetic resonance images. Both edematous changes and vascular-rich granulation tissue were seen around this fractured lesion. There was no evidence of osteonecrosis characterized by zone formation (into separate areas of necrotic, reparative, and viable tissue) in any part of the femoral head. Also, detritic synovitis, as is found in rapidly destructive arthrosis (RDA) of the hip joint, was not seen. These histopathological findings confirmed the diagnosis of SIF. Surprisingly, subchondral bone just beneath the articular cartilage was intact despite the breakage of slightly distal trabeculae (Fig. 6B). Although the articular cartilage on the broken trabeculae had mild degenerative changes, it maintained continuity. Therefore, we found no articular cartilage fragments in the area surrounded by the round, low-intensity band that appeared on T1-weighted magnetic resonance images.
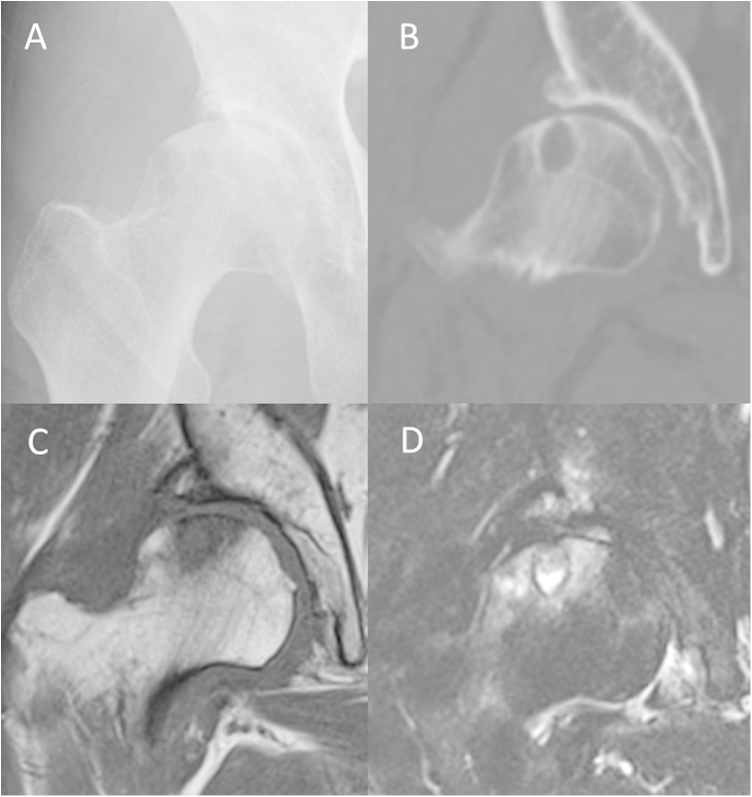
Fig. 1.

A supine anteroposterior radiograph obtained 1 month after the onset of pain in the right hip shows acetabular dysplasia, the lytic area in the superolateral portion of the femoral head and slight joint-space narrowing.
Fig. 2.
Images obtained 2 months after the onset of hip pain: (A) radiograph showing no remarkable changes in the joint space. (B) Computed tomography multiplanar reconstruction showing a lytic lesion with a well-defined sclerotic margin in the superolateral portion of the femoral head. (C) Coronal T1-weighted magnetic resonance image showing diffuse low signal intensity in the superolateral portion of the femoral head and acetabular rim. (D) Corresponding area of high signal intensity on the short τ inversion recovery (STIR) sequence. On the femoral side, there is a very high signal intensity area on the STIR sequence as well. A well-delineated round, low-intensity band is also visible on the T1-weighted image and the STIR sequence.
Fig. 3.
Images obtained 3 months after the onset of hip pain. (A) Radiograph showing that the joint space had been maintained. Magnetic resonance images (B, T1-weighted; C, short τ inversion recovery sequence) showing that the marrow edema pattern in the bone marrow had slightly lessened.
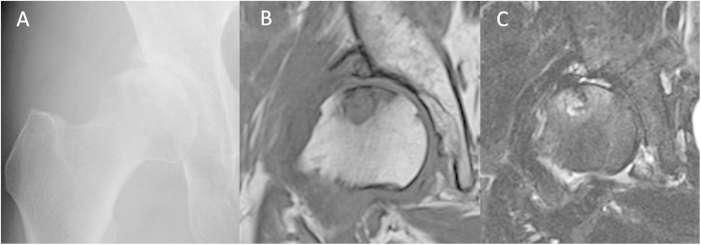
Fig. 4.

A supine anteroposterior radiograph obtained immediately after total hip arthroplasty.
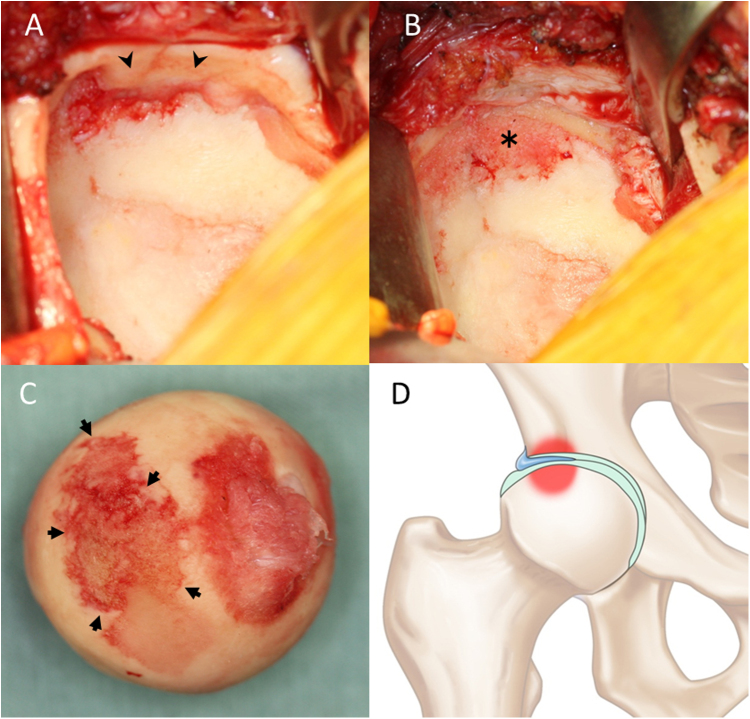
Fig. 5.
(A) During surgery, the anterosuperior labrum was found to be inverted into the articular space (arrowheads). (B) After resection of the inverted labrum (asterisk) and (C) resection of the femoral head, it was apparent that only the area of the articular cartilage in contact with the inverted labrum was damaged (arrows). (D) Illustration indicating how the inverted labrum affect articular cartilage and subchondral bone.
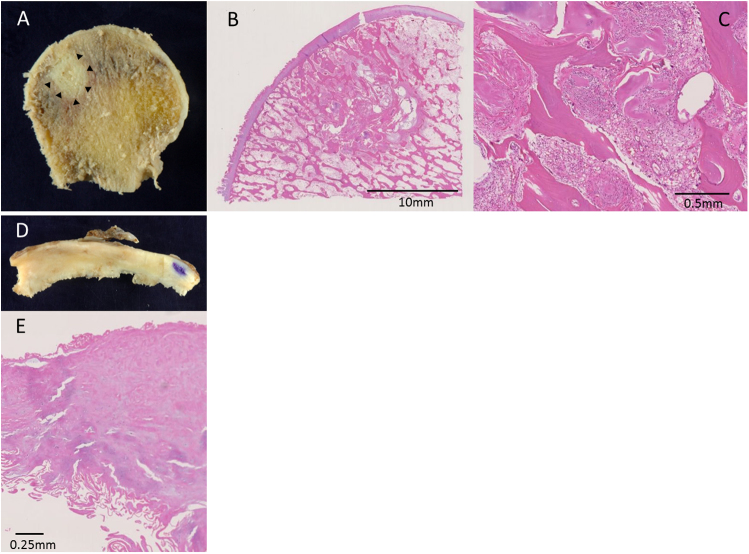
Fig. 6.
(A) A midcoronal cross-section of the resected femoral head shows a whitish round area (arrowheads) beneath the articular cartilage. (B, C) Photomicrographs obtained from the subchondral area shown in Fig. A outlined by black arrowheads demonstrates a fracture callus and granulation tissue (hematoxylin and eosin staining). (D) A photograph of the resected inverted labrum and (E) its photomicrograph show that the free end of the inverted labrum is severely fibrillated because of abrasion, but detritic changes are not remarkable.
3. Discussion
The concept of SIF, first described in 1996,10 involves bone fragility usually secondary to osteoporosis or osteopenia leading to subchondral fractures in the femoral head without of any evidence of osteonecrosis. Although bone fragility due to osteoporosis is considered the most important cause of SIF the reason why bone fractures occur in the subchondral area is unknown. SIF is generally seen in elderly women with osteoporosis, who are occasionally obese. Bilateral involvement is rare.1,5,10 Histopathological criteria for the diagnosis of SIF have been established.1,5 On gross examination, a linear, narrow, irregular whitish gray zone in the bone marrow space parallel to the subchondral bone endplate is generally seen. Microscopically, this area consists of irregularly arranged fracture callus, reactive cartilage, and granulation tissue. It should be noted that since all fractures lead to some bone and bone marrow necrosis on either side of the fracture line, small segments of necrotic bone trabeculae may be observed. However, such necrotic regions should not be diagnosed as primary osteonecrosis. The initial radiographic appearance of SIF is often unremarkable. In the advanced stage, crescent sign is commonly seen in SIF, as is the case with osteonecrosis. Previous reports have suggested that MR images are useful for the diagnosis of subchondral insufficiency fracture. Especially the shape of the low-intensity band on T1-weighted images may be useful for the diagnosis of SIF.1–4,10,11 In SIF of the femoral head, the low-intensity band has been reported to have an irregular serpentine shape and to be convex to the articular surface, because the band corresponds to the fracture line.1–4,10,11 However, our patient had a cystlike formation with a low-signal intensity on T1-weighted images and a very high signal intensity on STIR sequences in the superolateral portion of the femoral head, surrounded by a pattern of edema in the bone marrow. Histopathologically, this patient's low-intensity band corresponded to the edema and vascular-rich granulation that formed around the fractured area. These findings suggest that both edematous changes and granulation tissue around the fractured area may present as a round, low-intensity band on T1-weighted images in SIF. Zhao et al. reported a similar phenomenon in SIF.12 The shape of the low-intensity band on T1-weighted images could be helpful for differentiating SIF from osteonecrosis.1–3,9,10,13,14 In SIF, the low-intensity band corresponds to a subchondral fracture. Therefore, it is often irregular, serpentine, and parallel to the articular surface. In osteonecrosis, the low-intensity band represents a reactive interface between live and necrotic bone, which is well circumscribed, concave, and a mirror image of the articular surface. In osteoarthritic bone cysts, there is a well-defined, round, homogeneous area with low signal intensity on T1-weighted images and with pronounced hyperintensity on T2 fat-suppressed images.15,16 In our patient, it was difficult to differentiate between those conditions. Osteoarthritis which is the primary differential diagnosis of this case may coexist or contribute to the etiology of SIF. We may need to keep in mind that occasionally subchondral insufficiency fractures can appear as a round cystlike formation. If we had taken it into consideration, we could have tried another treatment options such as a non-weight bearing or a percutaneous cementoplasty but not a THA. RDA is a relatively uncommon form of arthritis that is usually seen in elderly women17–19 and is characterized by rapid joint destruction within 6–12 months after onset. The typical initial finding on radiographs is disappearance of the joint space, followed by the rapid disappearance of the femoral head.17–19 SIF is known to cause rapid destruction of the hip joint similar to that seen in RDA.20 Sugano et al. demonstrated that the diffuse abnormal pattern of low intensity on T1-weighted images and high intensity on T2-weighted images induced by a subchondral small lesion might be an early sign of RDA when joint-space narrowing is observed radiologically.21 We speculated that our patient's hip might be in the initial stage of RDA or collapse of the osteoarthritic bone cyst, even though we did not observe rapid progression of joint-space narrowing. However, histopathological findings indicated that there were no obvious rapidly destructive changes, and the area surrounded by the round, low-intensity band on T1-weighted images was SIF rather than an osteoarthritic bone cyst. Our findings indicate the possibility that SIF of the femoral head in elderly women does not always lead to RDA and that the mechanism of RDA is multifactorial. Our patient had insufficient acetabular coverage due to the mild acetabular dysplasia, which evoked high pressure on the top of the femoral head and the lateral portion of the acetabulum. Also, we found an inverted labrum between the lateral portion of the femoral head and the acetabulum. We speculate that the combination of those conditions could cause bone marrow edema in relation to SIF (Fig. 5D) and the inversion of the labrum may imply an important role for the mechanism of SIF in the femoral head and acetabulum.
4. Conclusion
It is important for surgeons to keep in mind that sometimes SIFs of the femoral head can appear as a round cystlike formation. Osteoarthritis of the hip joint may coexist or contribute to the etiology of SIF of the femoral head.
Conflict of interest statement
None.
Funding
None.
Ethical approval
“Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request”.
Author contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version for publication. Dr. Fukui had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Fukui.
Acquisition of data. Fukui, Fukushima.
Analysis and interpretation of data. Fukui, Kaneuji, Matsumoto.
Acknowledgments
Medical editor Katharine O’Moore-Klopf, ELS (East Setauket, NY, USA) provided professional English-language editing of this article.
Footnotes
Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article. Each author certifies that his institution approved the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Yamamoto T., Bullough P.G. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum. 1999;42:2719–2723. doi: 10.1002/1529-0131(199912)42:12<2719::AID-ANR31>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 2.Rafii M., Mitnick H., Klug J., Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol. 1997;168:159–163. doi: 10.2214/ajr.168.1.8976940. [DOI] [PubMed] [Google Scholar]
- 3.Ikemura S., Yamamoto T., Nakashima Y., Shuto T., Jingushi S., Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum. 2005;52:1293–1296. doi: 10.1002/art.20994. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto T., Schneider R., Iwamoto Y., Bullough P.G. Subchondral insufficiency fracture of the femoral head in a patient with systemic lupus erythematosus. Ann Rheum Dis. 2006;65:837–838. doi: 10.1136/ard.2005.041095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamamoto T., Iwamoto Y., Schneider R., Bullough P.G. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis. 2008;67:150–153. doi: 10.1136/ard.2006.066878. [DOI] [PubMed] [Google Scholar]
- 6.Yoshiike N., Matsumura Y., Zaman M.M., Yamaguchi M. Descriptive epidemiology of body mass index in Japanese adults in a representative sample from the National Nutrition Survey 1990–1994. Int J Obes Relat Metab Disord. 1998;22:684–687. doi: 10.1038/sj.ijo.0800651. [DOI] [PubMed] [Google Scholar]
- 7.Wiberg G. Studies on dysplastic acetabulum and congenital subluxation of the hip joint with special reference to the complications of osteoarthritis. Acta Chir Scand. 1939;83:29–38. [Google Scholar]
- 8.Massie W.K., Howorth M.B. Congenital dislocation of the hip. Part I. Method of grading results. J Bone Joint Surg Am. 1950;32:519–531. [PubMed] [Google Scholar]
- 9.Yamamoto T., DiCarlo E.F., Bullough P.G. The prevalence and clinicopathological appearance of extension of osteonecrosis in the femoral head. J Bone Joint Surg Br. 1999;81:328–332. [PubMed] [Google Scholar]
- 10.Bangil M., Soubrier M., Dubost J.J., Rami S., Carcanagues Y., Ristori J.M. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed. 1996;63:859–861. [PubMed] [Google Scholar]
- 11.Vande Berg B.C., Malghem J., Goffin E.J., Duprez T.P., Maldague B.E. Transient epiphyseal lesions in renal transplant recipients: presumed insufficiency stress fractures. Radiology. 1994;191:403–407. doi: 10.1148/radiology.191.2.8153313. [DOI] [PubMed] [Google Scholar]
- 12.Zhao G., Yamamoto T., Ikemura S., Nakashima Y., Mawatari T., Motomura G. A histopathological evaluation of a concave-shaped low-intensity band on T1-weighted MR images in a subchondral insufficiency fracture of the femoral head. Skeletal Radiol. 2010;39:185–188. doi: 10.1007/s00256-009-0750-6. [DOI] [PubMed] [Google Scholar]
- 13.Kubo T., Yamazoe Y., Sugano N., Fujioka M., Naruse S., Yoshimura N. Initial MRI findings of non-traumatic osteonecrosis of the femoral head in renal transplant recipients. Magn Reson Imaging. 1997;15:1017–1023. doi: 10.1016/s0730-725x(97)00159-8. [DOI] [PubMed] [Google Scholar]
- 14.Mankin H.J. Nontraumatic necrosis of bone (osteonecrosis) N Engl J Med. 1992;326:1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 15.Leydet-Quilici H., Le Corroller T., Bouvier C., Giorgi R., Argenson J.N., Champsaur P. Advanced hip osteoarthritis: magnetic resonance imaging aspects and histopathology correlations. Osteoarthritis Cartilage. 2010;18:1429–1435. doi: 10.1016/j.joca.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Zubler V., Mengiardi B., Pfirrmann C.W.A., Duc S.R., Schmid M.R., Hodler J. Bone marrow changes on STIR MR images of asymptomatic feet and ankles. Eur Radiol. 2007;17:3066–3072. doi: 10.1007/s00330-007-0691-1. [DOI] [PubMed] [Google Scholar]
- 17.Postel M., Kerboull M. Total prosthetic replacement in rapidly destructive arthrosis of the hip joint. Clin Orthop Relat Res. 1970;72:138–144. [PubMed] [Google Scholar]
- 18.Rosenberg Z.S., Shankman S., Steiner G.C., Kastenbaum D.K., Norman A., Lazansky M.G. Rapid destructive osteoarthritis: clinical, radiographic, and pathologic features. Radiology. 1992;182:213–216. doi: 10.1148/radiology.182.1.1727284. [DOI] [PubMed] [Google Scholar]
- 19.Motomura G., Yamamoto T., Nakashima Y., Shuto T., Jingushi S., Iwamoto Y. Outcome of the contralateral hip in rapidly destructive arthrosis after total hip arthroplasty: a preliminary report. J Arthroplasty. 2006;21:1026–1031. doi: 10.1016/j.arth.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Yamamoto T., Bullough P.G. The role of subchondral insufficiency fracture in rapid destruction of the hip joint: a preliminary report. Arthritis Rheum. 2000;43:2423–2427. doi: 10.1002/1529-0131(200011)43:11<2423::AID-ANR8>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 21.Sugano N., Ohzono K., Nishii T., Sakai T., Haraguchi K., Yoshikawa H. Early MRI findings of rapidly destructive coxopathy. Magn Reson Imaging. 2001;19:47–50. doi: 10.1016/s0730-725x(01)00221-1. [DOI] [PubMed] [Google Scholar]