Abstract
Purpose of review
Pneumonia is considered the leading infectious diseases cause of death and the seventh leading cause of death overall in the US. There is significant interest in understanding the relationship between community-acquired pneumonia (CAP) and mortality.
Recent findings
Most clinical studies examining patients with CAP have used an arbitrary in-hospital or 30-day mortality as a short-term mortality clinical end point. However, long-term mortality (arbitrary >3 months) factors, incidence, prediction, and implications on patient care are important issues that require further evaluation in patients with CAP. This review focuses on the most recent literature assessing the importance and the frequency of long-term associated outcomes in patients with CAP, the risk factors, and possible implications for future strategies. Multiple risk factors that include age, sex, comorbid conditions, type of pneumonia, and severity of illness are associated with higher long-term mortality. In addition, several biomarkers were demonstrated to be independently associated with long-term mortality.
Summary
Despite advances in the understanding of long-term mortality among CAP patients, there is still a high unacceptable long-term mortality. Public health programs should address this important gap, considering the high level of complexity factors in patients with CAP.
Keywords: biomarkers, community-acquired pneumonia, outcome
INTRODUCTION
Community-acquired pneumonia (CAP) is an important problem with significant morbidity, mortality, and cost. CAP accounts for 3–5 cases per 1000 person-years, particularly in the elderly with a 10-fold increased incidence rate [1–3]. In addition, the incidence of CAP has not decreased over the past few decades, despite advances in supportive care. CAP remains a frequent problem in clinical practice, particularly for those patients who require hospitalization and ICU admission [4]. Approximately 10% of the patients admitted to the hospital with a diagnosis of CAP require ICU care [5,6▪]. The mortality associated with CAP greatly depends on the clinical setting where it is treated. This mortality is only less than 3% in the outpatient setting, around 5–10% in inpatients not requiring ICU care, as high as 25% in intubated patients, and nearly 50% in ICU patients requiring vasopressors [7,8]. Therefore, the in-hospital case fatality rate for patients with severe disease remains unacceptably high.
Pneumonia is considered the seventh leading cause of death overall, and accounted for more than 59 000 deaths in the year 2008 in the USA [9]. In addition, in 2008, influenza and pneumonia together was the seventh cause of death for those aged 1–24 years and for those aged 65 years or older [9]. The total cost of pneumonia was approximately $20 billion, including $14 billion in healthcare expenditures and $6 billion in lost productivity [9]. Patients with pneumonia are also at risk for developing complications such as requiring mechanical ventilation for hypoxemic respiratory failure, need for vasopressors for hemodynamic instability, and multiorgan system failure [4]. There is significant interest in understanding the relationship between CAP and mortality. Most clinical studies examining patients with CAP have used an arbitrary in-hospital or 30-day mortality as a short-term mortality clinical end point [10–12]. The use of 30-day outcomes in clinical studies may underestimate the morbidity and mortality and may lead to inaccurate inferences [13▪]. Therefore, the understanding of long-term mortality (arbitrary >3 months) factors, incidence, prediction, and implications on patient care are important issues that require further evaluation in patients with CAP [14,15]. Multiple studies have addressed the association of pneumonia and pneumonia-related factors with long-term mortality [16–20,21▪,22,23,24▪,25,26▪,27,28,29▪–33▪,34,35,36▪–38▪,39,40▪,41–51,52▪, 53,54▪,55–70,71▪–74▪,75,76]. This review focuses on the most recent literature assessing the importance and the frequency of long-term associated outcomes in patients with CAP, the risk factors and possible implications for future strategies.
WHAT IS THE LONG-TERM MORTALITY RATE AFTER DEVELOPING COMMUNITY-ACQUIRED PNEUMONIA?
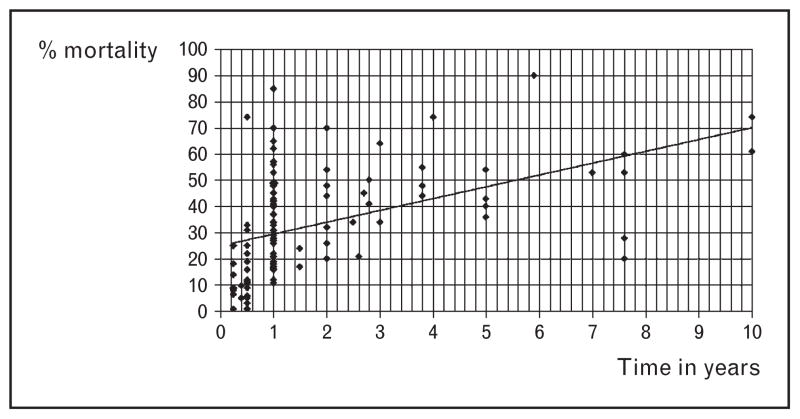
Over the past few decades multiple studies have reported variable long-term mortality rates for patients with CAP [16–20,21▪,22,23,24▪,25,26▪,27, 28,29▪–33▪,34,35,36▪–38▪,39,40▪,41–51,52▪,53,54▪, 55–70,71▪–74▪,75,76]. The variability in the reports depends on several factors that include: demographic characteristics, comorbid conditions, ambulatory vs. hospitalized patient location, severity of illness at presentation, time to follow-up, and other associated risk factors (Table 1 and Fig. 1). In general there is an incremental risk of death after surviving the pneumonia episode and the hospitalization-related event. In addition, the excess mortality observed among CAP patients who survived the initial event could be as high as 50% within 5 years after hospital discharge. Despite the higher rates of mortality observed in elderly patients, the unacceptable high long-term mortality persists after adjusting for demographic characteristics (e.g. age), comorbid conditions, and other factors [16,17,25]. Therefore, it is unclear why CAP is not considered a public health threat and major funding is not devoted to this important healthcare problem around the world. Comparing CAP with other important healthcare problems should strengthen the rationale for a call to action on this matter.
Table 1.
Risk factors associated with long-term mortality in patients with community-acquired pneumonia
| Age (> 65 years of age) | Neurocognitive disorders |
| Male | Cardiovascular diseases |
| Black | Chronic obstructive pulmonary disease |
| Nursing home residence | Preexisting malignancy |
| High school level or less | Poor nutritional states |
| Pneumonia characteristics | Charlson comorbidity score |
| Lack of fever | Pharmacotherapies |
| Healthcare associated pneumonia | Corticosteroids |
| Pleural effusion | Immunizations |
| Gram-negative bacilli infection | Statins |
| Severity of disease at presentation | Other |
| Low albumin level | Do not resuscitate order |
| Inflammatory and cardiovascular biomarkers | Living will |
FIGURE 1.
Long-term mortality rates among patients that develop community-acquired pneumonia. The figure represents the long-term mortality rates [◆] among community-acquired pneumonia patients reported in whole cohorts and subgroup analyses by multiple studies available in the literature [16–18,20,21▪,22,23,24▪,25,26▪,27,28,30▪,31▪,33▪,34,35,42,45–47,54▪,55,57,64,65,70,72▪,73▪,77▪,79▪,82].
IS COMMUNITY-ACQUIRED PNEUMONIA PER SE A RISK FACTOR FOR LONG-TERM MORTALITY?
Community-acquired pneumonia alone, without medical complications, may also have significant unappreciated long-term outcomes secondary to effects on various organ systems, especially the cardiovascular system, by possible pathogenetic mechanisms related to causal microorganisms, the bacterial load, the host response, or a combination of these factors. Consequently, several studies have addressed the impact of CAP in comparison with other important conditions. The initial observation by Hedlund et al. [59] in 1993 suggested that CAP, particularly in elderly patients (>50 years of age), had a significant mortality during the 3 years following discharge. In addition, the mortality directly associated with CAP was higher compared to other infections. Kaplan et al. [18] evaluated 158 960 hospitalized patients with CAP and non-CAP controls. The authors found a 1-year mortality of 41% among the CAP cohort vs. 20% of hospitalized control patients (P <0.001), and among hospital survivors a 1-year mortality of 34 vs. 25% (P <0.001), respectively. The differences among groups were not explained by underlying disease. In addition, Yende et al. [20] focused on a high-functioning cohort of older hospitalized patients with CAP. The authors found that CAP was associated with greater long-term mortality (5 years) independent of prehospitalization comorbid conditions. However, CAP long-term mortality rates were similar to other hospital-related chronic diseases, such as heart failure, cerebrovascular disease, and fracture.
These data suggest that CAP carries a significant long-term mortality even when compared to chronic conditions. However, the complex interactions that occur in a patient with an acute condition like CAP, with present chronic comorbid conditions, individual characteristics, and chronic pharmacological therapies may also influence the long-term mortality rate.
WHAT RISK FACTORS ARE ASSOCIATED WITH LONG-TERM MORTALITY IN PATIENTS WITH COMMUNITY-ACQUIRED PNEUMONIA?
Multiple studies have reported a series of risk factors deserving further exploration and evaluation that have shown an association with long-term mortality (Table 1).
Age
The aging process is something really alarming in the USA and around the globe. The proportion of US elderly patients (>65 years or older) is expected to increase from 12% in the year 2000 to almost 20% in the year 2030, and will double by the year 2050 [55]. Elderly patients tend to have higher rates of chronic comorbid conditions, poor functional status and disability, and are more likely to require care at a long-term care facility. Several studies have identified that advanced age is associated with higher long-term care mortality as shown in Table 1 [16–18,22,23,24▪,25,58]. Klapdor et al. [77▪] suggested that CAP is a different entity in younger patients due to the lower 6-month mortality compared to older patients with CAP. However, the risk of aging is variable, with a starting risk as early as 50 years of age as reported by Hedlund et al. [58] and as late as above 70 years of age as described by Sligl et al. [55]. In conclusion, increased age is associated with higher risk of long term-mortality in CAP.
Sex
Several studies [17,18,22,26▪,27] identify male sex as an important risk factor associated with higher risk of long-term CAP mortality (Table 1).
Race
A study by Polsky et al. [28], in the Medicare Provider Analysis and Review File and the Veterans Administration Patient Treatment File from 1998 to 2002, retrospectively assessed racial differences in mortality at 30 days and up to 2 years following a hospital admission for the elderly (>65 years of age) with common medical conditions. The authors found that by day 90, blacks with CAP had higher mortality compared to whites. In addition, the long- term (1 and 2-year) mortality rate among blacks and whites was unacceptably high (42 and 54% for blacks vs. 40 and 51% for whites, respectively). The long-term mortality at 2 years (54%) was higher among blacks compared to whites with other common admission diagnoses such as heart failure (44%), gastrointestinal bleeding (37%), hip fracture (41%), stroke (42%), and acute myocardial infarction (40%).
Type of pneumonia
A limited number of studies have assessed the association of different types of pneumonia and long-term outcomes in patients with CAP. Cecere et al. [25] studied younger adults and patients with health-care-associated pneumonia (HCAP) in comparison with CAP patients. The authors concluded that admission to the hospital for HCAP, and to a lesser degree CAP, was associated with long-term mortality even in young patients. Similar results were reported by Hsu et al. [29▪], who showed that 1-year HCAP mortality was nearly twice that of CAP, and that HCAP was an independent predictor of 1-year mortality [odds ratio (OR) 1.99, 95% confidence interval (CI) 1.87–2.11]. In addition, HCAP patients incurred significantly higher costs during the initial hospital stay and in the following 12 months. Mortensen et al. [22] also showed that patients who required nursing home residence were more likely to have long-term mortality (hazard ratio 1.5, 95% CI 1.1–2.1). Nursing home residence is one of the most common risk factors for HCAP diagnosis [15].
Chronic comorbid conditions
The concurrence of an acute illness such as CAP in patients with chronic conditions may be associated with greater morbidity, mortality, and cost. This interaction of an acute condition with chronic comorbid conditions leads to higher healthcare utilization, particularly among elderly patients [55]. Several comorbid conditions including neurodegenerative disorders, cardiovascular diseases, chronic obstructive pulmonary disease (COPD), malignancy, HIV, and poor nutritional status are some of the most common entities linked to long-term mortality in patients with CAP (Table 1) [16–20,21▪, 22,23,24▪,25,26▪,27,28,29▪–33▪,34,35,36▪–38▪,39,40▪,41–51,52▪,53,54▪,55–70,71▪–74▪,75,76,78,79▪, 80,83▪,84]. Many studies tend to combine or include the list of associated comorbid conditions in severity of illness scores validated for pneumonia or for chronic comorbid conditions, such as the Charlson comorbidity index [85], in order to predict mortality [22,30▪,55]. Below are a few of the most relevant hot topics regarding the association of long-term mortality in patients with CAP.
Neurodegenerative disorders such as dementia, stroke, and cognitive impairment have been associated with long-term mortality [21▪,27,31▪,32▪,51, 78,79▪]. Van der Steen et al. [31▪] showed that male nursing home residents with advanced dementia and lower respiratory tract infection (e.g. CAP) had a substantial 6-month mortality (74%) despite antibiotic treatment. Sachs et al. [32▪] evaluated the association between cognitive impairment and increased long-term mortality among primary care patients aged 60 years and older. The authors found a few important notable differences in the causes of death among the groups. Influenza and pneumonia together was the seventh leading cause of death overall, but the fourth leading cause of death for those with moderate to severe cognitive impairment. Similarly, Sligl et al. [21▪] found that prehospital functional dependence was associated with increased 1-year mortality (hazard ratio 3.0, 95% CI 1.5–6.1).
Cardiovascular conditions that include acute coronary syndromes (e.g. acute myocardial infarction), heart failure, arrhythmias, and stroke are associated with higher rates of long-term mortality among CAP patients [37▪,38▪,39,40▪,41,80,83▪]. A recent European Respiratory Journal perspective article by Ewig and Torres [36▪] compared the similarities between CAP and acute coronary syndromes, and suggested the need for a more aggressive and intensified approach to diagnose, treat, and prevent CAP. Dong et al. [83▪] showed in their meta-analysis that acute respiratory infection was associated with an increased risk of acute coronary syndromes. In addition, a provocative series of articles by Corrales-Medina et al. [37▪,38▪,39,40▪,41], which builds on the experience of the association of short-term mortality and acute coronary syndromes in patients with pneumonia, suggests interesting hypotheses on the possible triggering mechanisms of infection.
Pre-existent malignancy at the time of CAP diagnosis, or a new diagnosis of malignancy after initial presentation, is also associated with a higher long-term mortality [24▪,59,84]. Bruns et al. [24▪] reported, in a prospective observational study in a Dutch population, that most CAP patients died because of malignancy (27%), respiratory diseases (27%, COPD the most common respiratory reason in 19%), and vascular diseases (16%). Hedlund et al. [59] also reported that after an episode of CAP, the most important causes of death were cardiovascular diseases and malignancies. Mortensen et al. [84] confirmed an important association between post-pneumonia pulmonary malignancy and higher short and long-term mortality, long-term survival, and length of hospital stay. Patients diagnosed with lung cancer had improved survival for the first 90 days postpneumonia hospitalization, but lower survival after 90 days and total survival of less than 2 years. The authors found that the risk factors associated with a new diagnosis of pulmonary malignancy included current tobacco use, any malignancy, metastatic solid tumor, COPD, congestive heart failure, and male sex.
Chronic obstructive pulmonary disease is another risk factor previously mentioned. Bruns et al. [24▪] showed that individuals who recovered from CAP had a four-fold increased risk of dying because of COPD as compared with the general population. This could be a result of statistical confounding, as the prevalence of COPD is higher in the CAP cohort than in population controls. However, other studies have confirmed similar poor survival associated with COPD [43,44].
The above information regarding comorbidities emphasizes the importance of optimal management of chronic conditions in CAP patients. Early recognition and appropriate management of comorbidities may play a role in favorable long-term outcomes.
Severity of illness
Most of the severity risk assessments focus on short-term mortality by measuring the variables involved in organ dysfunction in patients with CAP. Admission to the hospital or the development of moderate to severe pneumonia may influence the risk of long-term mortality [22,42]. In a study by Karhu et al. [30▪], severe CAP (ICU-admitted patients with pneumonia) compared to hospital-acquired and ventilator-associated pneumonia had the lowest 1-year mortality. However, severity of illness was measured by ICU admission and not by any of the validated pneumonia severity of illness scores. The two most widely used and validated methods include the pneumonia severity index score (PSI) and the CURB-65 [10–12]. The PSI is a 20-point score used at the time of clinical presentation that classifies patients into five risk categories. It uses three demographic parameters, five comorbid conditions, five physical examination findings, and seven laboratory/imaging findings to calculate the final score. The number of points for each variable are added and then stratified into the risk categories based on their percentage risk to predict 30-day mortality. PSI is heavily influenced by age, and the large number of variables evaluated makes it complex to use. In contrast are the CURB-65, CURB, and CRB (simpler tool that does not require blood urea nitrogen). CURB-65 is a less complex score derived from the original CURB with the addition of age as a new variable. This score is also based on the 30-day mortality risk and is composed of only five variables (accounting for one point each): confusion, urea, respiratory rate, blood pressure, and age above 65 years of age (CURB-65). Despite the simplicity, the ability of this tool to predict long-term mortality is not adopted in clinical practice. Sligl et al. [55] showed that, among several risk factors, high PSI score (modified for age) was associated with higher 1-year mortality. However, most of the studies addressing severity of illness have included inflammatory or infection parameters to assess outcomes, with certain limitations. This is why significant interest has emerged in cardiovascular biomarkers as important predictive tools.
BIOMARKERS
Multiple biomarkers have been studied alone or in combination with severity of illness scores attempting to predict short and long-term outcomes [33▪,34,35,46,48,49,54▪,72▪,73▪,82]. Several bio-markers were demonstrated in univariate and multivariate analyses to be independently associated with long-term mortality [33▪,34,35,46,54▪,72▪,73▪,82]. However, routine use of these biomarkers is not widely accepted or utilized and may take some time to become the standard of care. Procalcitonin is a biomarker that has shown benefit in the diagnosis and guidance on discontinuation of antibiotic in patients with CAP [81]. Bello et al. [33▪] performed a prospective study in immunocompetent CAP patients and found that pro-adrenomedullin (proADM) had a high predictive power for short and long-term mortality. Similar results were observed by Kruger et al. [34], who showed that midregional-proADM, midregional-pro-antinatriuretic peptide (MR-pro-ANP), copeptin, proendothelin 1 (CT-ET-1), and CRB-65 are good predictors for 3-month mortality. Moreover, MR-pro-ADM is a better predictor for 3-month mortality than MR-pro-ANP, copeptin, CT-ET-1, procalcitonin, C-reactive protein, and white blood cell count. These data suggest that the complexity associated with death includes cardiovascular, inflammatory, and infectious processes, better measured by a biomarker.
CONCLUSION
Community-acquired pneumonia is an important problem with significant morbidity, mortality, and cost. There is significant interest in understanding the relationship between CAP and mortality for patients who survive the initial acute event. A better understanding of long-term mortality (arbitrary >3 months) factors, incidence, prediction, and implications on patient care are important issues that require further evaluation in patients with CAP. This review focused on the most recent literature assessing the importance and the frequency of long-term associated outcomes in patients with CAP, the risk factors, and possible implications for future strategies.
KEY POINTS.
Community-acquired pneumonia is associated with significantly high long-term mortality (>3 months).
Multiple risk factors that include demographic characteristics, comorbid conditions, location of hospitalization, severity of illness at presentation, and time to follow-up are associated with poor long-term survival among patients with community-acquired pneumonia.
Several biomarkers have been demonstrated to predict long-term mortality in patients with community acquired pneumonia.
Acknowledgments
The author is grateful to Dr Stephanie M. Levine for her editorial support.
Footnotes
Conflicts of interest
Dr Marcos I. Restrepo participated as a consultant in the data safety monitoring board for clinical trials run by Theravance and Trius.
Financial Support: Dr Restrepo time is partially protected by Award Number K23HL096054 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, And Blood Institute or the National Institutes of Health. The funding agencies had no role in the preparation, review, or approval of the manuscript. The views expressed in this article are those of the author and do not necessarily represent the views of the Department of Veterans Affairs.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (pp. 205–206).
- 1.Almillar J, Bolivar I, Vidal J, et al. Epidemiology of community-acquired pneumonia in adults: a population-based study. Eur Respir J. 2000;15:757–763. doi: 10.1034/j.1399-3003.2000.15d21.x. [DOI] [PubMed] [Google Scholar]
- 2.Ewig S, Birkner N, Strauss R, et al. New perspectives on community-acquired pneumonia in 388 406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax. 2009;64:1062–1069. doi: 10.1136/thx.2008.109785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martson BJ, Plouffe JF, File TM, Jr, et al. Incidence of community-acquired pneumonia requiring hospitalization. Results of a population-based active surveillance Study in Ohio. The Community-Based Pneumonia Incidence Study Group. Arch Intern Med. 1997;157:1709–1718. [PubMed] [Google Scholar]
- 4.Restrepo MI, Anzueto A. Severe community-acquired pneumonia. Infect Dis Clin North Am. 2009;23:503–520. doi: 10.1016/j.idc.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Renaud B, Santin A, Coma E, et al. Association between timing of intensive care unit admission and outcomes for emergency department patients with community-acquired pneumonia. Crit Care Med. 2009;37:2867–2874. doi: 10.1097/CCM.0b013e3181b02dbb. [DOI] [PubMed] [Google Scholar]
- 6▪.Ewig S, Woodhead M, Torres A. Towards a sensible comprehension of severe community-acquired pneumonia. Intensive Care Med. 2011;37:214–223. doi: 10.1007/s00134-010-2077-0. Application of the whole spectrum of severity criteria may have more sensitivity than individual severe pneumonia predictive scores. [DOI] [PubMed] [Google Scholar]
- 7.Angus DC, Marrie TJ, Obrosky DS, et al. Severe community-acquired pneumonia: use of intensive care services and evaluation of American and British Thoracic Society diagnostic criteria. Am J Respir Crit Care Med. 2002;166:717–723. doi: 10.1164/rccm.2102084. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez A, Mendia A, Sirvent JM, et al. Combination antibiotic therapy improves survival in patients with community-acquired pneumonia and shock. Crit Care Med. 2007;35:1493–1498. doi: 10.1097/01.CCM.0000266755.75844.05. [DOI] [PubMed] [Google Scholar]
- 9.National Heart, Lung, and Blood Institute. Morbidity and mortality: 2012 chart book on cardiovascular, lung, and blood diseases. Bethesda, Maryland: US Department of Health and Human Services. Public Health Service. National Institutes of Health; Feb, 2012. [Accessed September 9, 2012]. www.nhlbi.nih.gov/resources/docs/2012_ChartBook.pdf. [Google Scholar]
- 10.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 11.Lim WS, Lewis S, Macfarlane JT. Severity prediction rules in community acquired pneumonia: a validation study. Thorax. 2000;55:219–223. doi: 10.1136/thorax.55.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13▪.Chalmers JD, Mandal P, Singanayagam A, et al. Severity assessment tools to guide ICU admission in community-acquired pneumonia: systematic review and meta-analysis. Intensive Care Med. 2011;37:1409–1420. doi: 10.1007/s00134-011-2261-x. Severity scores designed to predict 30-day mortality perform less well to predict ICU admission. [DOI] [PubMed] [Google Scholar]
- 14.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44:S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Thoracic Society/Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator associated and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 16.Bordon J, Wiemken T, Peyrani P, et al. CAPO Study Group. Decrease in long-term survival for hospitalized patients with community-acquired pneumonia. Chest. 2010;138:279–283. doi: 10.1378/chest.09-2702. [DOI] [PubMed] [Google Scholar]
- 17.Johnstone J, Eurich DT, Majumdar SR, et al. Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine (Baltimore) 2008;87:329–334. doi: 10.1097/MD.0b013e318190f444. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan V, Clermont G, Griffin MF, et al. Pneumonia: still the old man’s friend? Arch Intern Med. 2003;163:317–323. doi: 10.1001/archinte.163.3.317. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan V, Angus DC, Griffin MF, et al. Hospitalized community-acquired pneumonia in the elderly: age- and sex-related patterns of care and outcome in the United States. Am J Respir Crit Care Med. 2002;165:766–772. doi: 10.1164/ajrccm.165.6.2103038. [DOI] [PubMed] [Google Scholar]
- 20.Yende S, Angus DC, Ali IS, et al. Influence of comorbid conditions on long-term mortality after pneumonia in older people. J Am Geriatr Soc. 2007;55:518–525. doi: 10.1111/j.1532-5415.2007.01100.x. [DOI] [PubMed] [Google Scholar]
- 21▪.Sligl WI, Eurich DT, Marrie TJ, Majumdar SR. Only severely limited, premorbid functional status is associated with short- and long-term mortality in patients with pneumonia who are critically ill: a prospective observational study. Chest. 2011;139:88–94. doi: 10.1378/chest.10-1054. This article addresses the importance of premorbid functional status in critically ill patients with pneumonia. [DOI] [PubMed] [Google Scholar]
- 22.Mortensen EM, Kapoor WN, Chang CC, Fine MJ. Assessment of mortality after long term follow-up of patients with community-acquired pneumonia. Clin Infect Dis. 2003;37:1617–1624. doi: 10.1086/379712. [DOI] [PubMed] [Google Scholar]
- 23.Myles PR, Hubbard RB, Gibson JE, et al. Pneumonia mortality in a UK general practice population cohort. Eur J Public Health. 2009;19:521–526. doi: 10.1093/eurpub/ckp081. [DOI] [PubMed] [Google Scholar]
- 24▪.Bruns AH, Oosterheert JJ, Cucciolillo MC, et al. Cause-specific long-term mortality rates in patients recovered from community-acquired pneumonia compared with the general Dutch population. Clin Microbiol Infect. 2011;17:763–768. doi: 10.1111/j.1469-0691.2010.03296.x. This study shows that causes of death in the years following an episode of CAP are mostly comorbidity-related, and not attributable to recurrent pneumonia. [DOI] [PubMed] [Google Scholar]
- 25.Cecere LM, Rubenfeld GD, Park DR, et al. Long-term survival after hospitalization for community-acquired and healthcare-associated pneumonia. Respiration. 2010;79:128–136. doi: 10.1159/000255764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26▪.Guertler C, Wirz B, Christ-Crain M, et al. Inflammatory responses predict long term mortality risk in community-acquired pneumonia. Eur Respir J. 2011;37:1439–1446. doi: 10.1183/09031936.00121510. Pronounced clinical and laboratory signs of systemic inflammatory host response upon initial hospital stay were associated with favorable long-term prognosis. [DOI] [PubMed] [Google Scholar]
- 27.Koivula I, Sten M, Makela PH. Prognosis after community-acquired pneumonia in the elderly: a population-based 12-year follow-up study. Arch Intern Med. 1999;159:1550–1555. doi: 10.1001/archinte.159.14.1550. [DOI] [PubMed] [Google Scholar]
- 28.Polsky D, Jha AK, Lave J, et al. Short- and long-term mortality after an acute illness for elderly whites and blacks. Health Serv Res. 2008;43:1388–1402. doi: 10.1111/j.1475-6773.2008.00837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29▪.Hsu JL, Siroka AM, Smith MW, et al. One-year outcomes of community acquired and healthcare-associated pneumonia in the Veterans Affairs Healthcare System. Int J Infect Dis. 2011;15:e382–e387. doi: 10.1016/j.ijid.2011.02.002. This study assessed the impact on mortality and comorbidities, pneumonia severity and risk factors for multidrug-resistant infection in patients with HCAP compared to CAP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪.Karhu J, Ala-Kokko TI, Ylipalosaari P, et al. Hospital and long-term outcomes of & ICU-treated severe community- and hospital-acquired, and ventilator-associated pneumonia patients. Acta Anaesthesiol Scand. 2011;55:1254–1260. doi: 10.1111/j.1399-6576.2011.02535.x. This study suggests that nosocomial pneumonia may have a higher long-term mortality compared to community-acquired pneumonia. [DOI] [PubMed] [Google Scholar]
- 31▪.van der Steen JT, Lane P, Kowall NW, et al. Antibiotics and mortality in patients with lower respiratory infection and advanced dementia. J Am Med Dir Assoc. 2012;13:156–161. doi: 10.1016/j.jamda.2010.07.001. In nursing home residents with advanced dementia and lower respiratory tract infections, antibiotics prolonged life but in many cases only for a few days. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32▪.Sachs GA, Carter R, Holtz LR, et al. Cognitive impairment: an independent predictor of excess mortality: a cohort study. Ann Intern Med. 2011;155:300–308. doi: 10.7326/0003-4819-155-5-201109060-00007. This study suggests that any grade (from mild to severe) of cognitive impairment is independently associated with an increased risk of mortality in primary care patients aged 60 years or older. [DOI] [PubMed] [Google Scholar]
- 33▪.Bello S, Lasierra AB, Mincholé E, et al. Prognostic power of proadrenomedullin in community-acquired pneumonia is independent of aetiology. Eur Respir J. 2012;39:1144–1155. doi: 10.1183/09031936.00080411. Midregional-proADM showed predictive power for complications and short- and long-term mortality (1 year) and improved accuracy of clinical predictive scores in patients with CAP. [DOI] [PubMed] [Google Scholar]
- 34.Kruger S, Ewig S, Giersdorf S, et al. Cardiovascular and inflammatory biomarkers to predict short- and long-term survival in community-acquired pneumonia: results from the German Competence Network, CAPNETZ. Am J Respir Crit Care Med. 2010;182:1426–1434. doi: 10.1164/rccm.201003-0415OC. [DOI] [PubMed] [Google Scholar]
- 35.Kruger S, Ewig S, Kunde J, et al. Pro-atrial natriuretic peptide and pro-vasopressin for predicting short-term and long-term survival in community-acquired pneumonia: results from the German Competence Network CAPNETZ. Thorax. 2010;65:208–214. doi: 10.1136/thx.2009.121178. [DOI] [PubMed] [Google Scholar]
- 36▪.Ewig S, Torres A. Community-acquired pneumonia as an emergency: time for an aggressive intervention to lower mortality. Eur Respir J. 2011;38:253–260. doi: 10.1183/09031936.00199810. This editorial emphasized the importance of considering community-acquired pneumonia as an emergency. Patients with increased risk of death using clinical prediction tools should receive an aggressive approach. [DOI] [PubMed] [Google Scholar]
- 37▪.Corrales-Medina VF, Suh KN, Rose G, et al. Cardiac complications in patients with community-acquired pneumonia: a systematic review and meta-analysis of observational studies. PLoS Med. 2011;8:e1001048. doi: 10.1371/journal.pmed.1001048. Patients with CAP have a high risk of cardiac complications. This study suggests that strategies for preventing pneumonia in populations at high risk need to be optimized. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪.Corrales-Medina VF, Musher DM, Wells GA, et al. Cardiac complications in patients with community-acquired pneumonia: incidence, timing, risk factors, and association with short-term mortality. Circulation. 2012;125:773–781. doi: 10.1161/CIRCULATIONAHA.111.040766. Incident cardiac complications are common in patients with CAP and are associated with increased short-term mortality. According to this study, risk factors are older age, nursing home residence, pre-existing cardiovascular disease and pneumonia severity. [DOI] [PubMed] [Google Scholar]
- 39.Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10:83–92. doi: 10.1016/S1473-3099(09)70331-7. [DOI] [PubMed] [Google Scholar]
- 40▪.Corrales-Medina VF, Musher DM. Immunomodulatory agents in the treatment of community-acquired pneumonia: a systematic review. J Infect. 2011;63:187–199. doi: 10.1016/j.jinf.2011.06.009. This study showed that immunomodulatory agents (e.g. macrolides, aspirin, and statins) could be beneficial in patients with CAP to reduce excessive inflammatory response and “cytokine storm’. [DOI] [PubMed] [Google Scholar]
- 41.Corrales-Medina VF, Serpa J, Rueda AM, et al. Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine (Baltimore) 2009;88:154–159. doi: 10.1097/MD.0b013e3181a692f0. [DOI] [PubMed] [Google Scholar]
- 42.Mortensen EM, Coley CM, Singer DE, et al. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 2002;162:1059–1064. doi: 10.1001/archinte.162.9.1059. [DOI] [PubMed] [Google Scholar]
- 43.Restrepo MI, Mortensen EM, Pugh JA, Anzueto A. COPD is associated with increased mortality in patients with community-acquired pneumonia. Eur Respir J. 2006;28:346–351. doi: 10.1183/09031936.06.00131905. [DOI] [PubMed] [Google Scholar]
- 44.Molinos L, Clemente MG, Miranda B, et al. Community-acquired pneumonia in patients with and without chronic obstructive pulmonary disease. J Infect. 2009;58:417–424. doi: 10.1016/j.jinf.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 45.Johnstone J, Eurich DT, Minhas JK, et al. Impact of the pneumococcal vaccine on long-term morbidity and mortality of adults at high risk for pneumonia. Clin Infect Dis. 2010;51:15–22. doi: 10.1086/653114. [DOI] [PubMed] [Google Scholar]
- 46.Yende S, D’Angelo G, Kellum JA, et al. Inflammatory markers at hospital discharge predict subsequent mortality after pneumonia and sepsis. Am J Respir Crit Care Med. 2008;177:1242–1247. doi: 10.1164/rccm.200712-1777OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brancati FL, Chow JW, Wagener MM, et al. Is pneumonia really the old man’s friend? Two-year prognosis after community-acquired pneumonia. Lancet. 1993;342:30–33. doi: 10.1016/0140-6736(93)91887-r. [DOI] [PubMed] [Google Scholar]
- 48.Ortqvist A, Hedlund J, Wretlind B, et al. Diagnostic and prognostic value of interleukin-6 and C-reactive protein in community-acquired pneumonia. Scand J Infect Dis. 1995;27:457–462. doi: 10.3109/00365549509047046. [DOI] [PubMed] [Google Scholar]
- 49.Glynn P, Coakley R, Kilgallen I, et al. Circulating interleukin 6 and interleukin 10 in community acquired pneumonia. Thorax. 1999;54:51–55. doi: 10.1136/thx.54.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bauer TT, Montón C, Torres A, et al. Comparison of systemic cytokine levels in patients with acute respiratory distress syndrome, severe pneumonia, and controls. Thorax. 2000;55:46–52. doi: 10.1136/thorax.55.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Waterer GW, Kessler LA, Wunderink RG. Medium-term survival after hospitalization with community-acquired pneumonia. Am J Respir Crit Care Med. 2004;169:910–914. doi: 10.1164/rccm.200310-1448OC. [DOI] [PubMed] [Google Scholar]
- 52▪.Mortensen EM. Potential causes of increased long-term mortality after pneumonia. Eur Respir J. 2011;37:1306–1307. doi: 10.1183/09031936.00194110. The author underlines how pneumonia impacts on patient’s morbidity and mortality for several years after the acute episode. [DOI] [PubMed] [Google Scholar]
- 53.Smeeth L, Cook C, Thomas S, et al. Risk of deep vein thrombosis and pulmonary embolism after acute infection in a community setting. Lancet. 2006;367:1075–1079. doi: 10.1016/S0140-6736(06)68474-2. [DOI] [PubMed] [Google Scholar]
- 54▪.Yende S, D’Angelo G, Mayr F, et al. Elevated hemostasis markers after pneumonia increases one-year risk of all-cause and cardiovascular deaths. PLoS One. 2011;6:e22847. doi: 10.1371/journal.pone.0022847. This study shows that elevations of thrombin–antithrombin complexes and D-dimer levels at hospital discharge in patients with pneumonia are associated with higher risk of death, in particular due to cardiovascular disease. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sligl WI, Eurich DT, Marrie TJ, Majumdar SR. Age still matters: prognosticating short- and long-term mortality for critically ill patients with pneumonia. Crit Care Med. 2010;38:2126–2132. doi: 10.1097/CCM.0b013e3181eedaeb. [DOI] [PubMed] [Google Scholar]
- 56.Napolitano LM, Brunsvold ME, Reddy RC, Hyzy RC. Community-acquired methicillin-resistant Staphylococcus aureus pneumonia and ARDS: 1-year follow-up. Chest. 2009;136:1407–1412. doi: 10.1378/chest.07-1511. [DOI] [PubMed] [Google Scholar]
- 57.Hedlund JU, Ortqvist AB, Kalin M, et al. Risk of pneumonia in patients previously treated in hospital for pneumonia. Lancet. 1992;340:396–397. doi: 10.1016/0140-6736(92)91473-l. [DOI] [PubMed] [Google Scholar]
- 58.Hedlund J, Hansson LO, Ortqvist A. Short- and long-term prognosis for middle-aged and elderly patients hospitalized with community-acquired pneumonia: impact of nutritional and inflammatory factors. Scand J Infect Dis. 1995;27:32–37. doi: 10.3109/00365549509018970. [DOI] [PubMed] [Google Scholar]
- 59.Hedlund JU, Ortqvist AB, Kalin ME, Granath F. Factors of importance for the long term prognosis after hospital treated pneumonia. Thorax. 1993;48:785–789. doi: 10.1136/thx.48.8.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ueda K, Hasuo Y, Ohmura T, et al. Causes of death in the elderly and their changing pattern in Hisayama, a Japanese community. Results from a long-term and autopsy-based study. J Am Geriatr Soc. 1990;38:1332–1338. doi: 10.1111/j.1532-5415.1990.tb03457.x. [DOI] [PubMed] [Google Scholar]
- 61.Ortqvist A. Prognosis in community-acquired pneumonia requiring treatment in hospital. Importance of predisposing and complicating factors, and of diagnostic procedures. Scand J Infect Dis Suppl. 1990;65:1–62. [PubMed] [Google Scholar]
- 62.Boyd DH. Failure of resolution in pneumonia. Br J Dis Chest. 1975;69:259–266. doi: 10.1016/0007-0971(75)90094-7. [DOI] [PubMed] [Google Scholar]
- 63.Myles PR, Hubbard RB, Gibson JE, et al. The impact of statins, ACE inhibitors and gastric acid suppressants on pneumonia mortality in a UK general practice population cohort. Pharmacoepidemiol Drug Saf. 2009;18:697–703. doi: 10.1002/pds.1769. [DOI] [PubMed] [Google Scholar]
- 64.Pilotto A, Addante F, Ferrucci L, et al. The multidimensional prognostic index predicts short- and long-term mortality in hospitalized geriatric patients with pneumonia. J Gerontol A Biol Sci Med Sci. 2009;64:880–887. doi: 10.1093/gerona/glp031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Reade MC, Yende S, D’Angelo G, et al. Differences in immune response may explain lower survival among older men with pneumonia. Crit Care Med. 2009;37:1655–1662. doi: 10.1097/CCM.0b013e31819da853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Venditti M, Falcone M, Corrao S, et al. Outcomes of patients hospitalized with community-acquired, healthcare-associated, and hospital-acquired pneumonia. Ann Intern Med. 2009;150:19–26. doi: 10.7326/0003-4819-150-1-200901060-00005. [DOI] [PubMed] [Google Scholar]
- 67.Chong CP, Street PR. Pneumonia in the elderly: a review of severity assessment, prognosis, mortality, prevention, and treatment. South Med J. 2008;101:1134–1140. doi: 10.1097/SMJ.0b013e31818247f1. [DOI] [PubMed] [Google Scholar]
- 68.Frostad A, Soyseth V, Haldorsen T, et al. Respiratory symptoms and 30 year mortality from obstructive lung disease and pneumonia. Thorax. 2006;61:951–956. doi: 10.1136/thx.2006.059436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hamel MB, Phillips RS, Davis RB, et al. Outcomes and cost-effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med. 2000;109:614–620. doi: 10.1016/s0002-9343(00)00591-x. [DOI] [PubMed] [Google Scholar]
- 70.Carriere KC, Jin Y, Marrie TJ, et al. Outcomes and costs among seniors requiring hospitalization for community-acquired pneumonia in Alberta. J Am Geriatr Soc. 2004;52:31–38. doi: 10.1111/j.1532-5415.2004.52007.x. [DOI] [PubMed] [Google Scholar]
- 71▪.Ewig S, Klapdor B, Pletz MW, et al. Nursing-home-acquired pneumonia in & Germany: an 8-year prospective multicentre study. Thorax. 2012;67:132–138. doi: 10.1136/thoraxjnl-2011-200630. This study underlines that nursing-home acquired pneumonia is frequently considered and managed as a terminal event. Excess mortality in these patients results from increased comorbidities. [DOI] [PubMed] [Google Scholar]
- 72▪.Vazquez M, Jockers K, Christ-Crain M, et al. MR-pro-atrial natriuretic peptide (MR-proANP) predicts short- and long-term outcomes in respiratory tract infections: a prospective validation study. Int J Cardiol. 2012;156:16–23. doi: 10.1016/j.ijcard.2010.10.037. This study confirms the high prognostic performance of MR-proANP for short- and long-term mortality, particularly its high negative predictive value. [DOI] [PubMed] [Google Scholar]
- 73▪.Nowak A, Breidthardt T, Christ-Crain M, et al. Direct comparison of three natriuretic peptides for prediction of short- and long-term mortality in patients with community-acquired pneumonia. Chest. 2012;141:974–982. doi: 10.1378/chest.11-0824. NT-proBNP, MR-proANP, and BNP are all simple and powerful predictors of short and long-term mortality for CAP patients. [DOI] [PubMed] [Google Scholar]
- 74▪.Douglas I, Evans S, Smeeth L. Effect of statin treatment on short term mortality after pneumonia episode: cohort study. Br Med J. 2011;342:d1642. doi: 10.1136/bmj.d1642. Patients on long term statin treatment had a lower risk of dying in the six months after pneumonia. The authors highlight the need of further studies to prove this protective effect in patients that start statins when they first develop pneumonia. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.El Moussaoui R, Opmeer BC, de Borgie CA, et al. Long-term symptom recovery and health-related quality of life in patients with mild-to-moderate-severe community-acquired pneumonia. Chest. 2006;130:1165–1172. doi: 10.1378/chest.130.4.1165. [DOI] [PubMed] [Google Scholar]
- 76.Vila-Corcoles A, Ochoa-Gondar O, Rodriguez-Blanco T, et al. Epidemiology of community-acquired pneumonia in older adults: a population-based study. Respir Med. 2009;103:309–316. doi: 10.1016/j.rmed.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 77▪.Klapdor B, Ewig S, Pletz MW, et al. Community-acquired pneumonia in younger patients is an entity on its own. Eur Respir J. 2012;39:1156–1161. doi: 10.1183/09031936.00110911. This article suggests that CAP in young patients is a different entity from CAP in the elderly. This is mainly due to far less comorbidity, more classical clinical presentation and less severe symptoms in younger patients. [DOI] [PubMed] [Google Scholar]
- 78.Torres OH, Muñoz J, Ruiz D, et al. Outcome predictors of pneumonia in elderly patients: importance of functional assessment. J Am Geriatr Soc. 2004;52:1603–1609. doi: 10.1111/j.1532-5415.2004.52492.x. [DOI] [PubMed] [Google Scholar]
- 79▪.Pratt N, Roughead EE, Ramsay E, et al. Risk of hospitalization for hip fracture and pneumonia associated with antipsychotic prescribing in the elderly: a self-controlled case-series analysis in an Australian healthcare claims database. Drug Saf. 2011;34:567–575. doi: 10.2165/11588470-000000000-00000. This study shows that antipsychotic use in the elderly is associated with increased risk of hospitalization due to hip fracture and pneumonia. It suggests that practitioners should consider these risks when prescribing antipsychotics to elderly patients with dementia. [DOI] [PubMed] [Google Scholar]
- 80.Emsley HC, Hopkins SJ. Acute ischaemic stroke and infection: recent and emerging concepts. Lancet Neurol. 2008;7:341–353. doi: 10.1016/S1474-4422(08)70061-9. [DOI] [PubMed] [Google Scholar]
- 81.Schuetz P, Christ-Crain M, Thomann R, et al. ProHOSP Study Group. Effect of procalcitonin-based guidelines vs. standard guidelines on antibiotic use in lower respiratory tract infections: the ProHOSP randomized controlled trial. J Am Med Assoc. 2009;302:1059–1066. doi: 10.1001/jama.2009.1297. [DOI] [PubMed] [Google Scholar]
- 82.Kellum JA, Kong L, Fink MP, et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167:1655–1663. doi: 10.1001/archinte.167.15.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83▪.Dong M, Liu T, Li G. Association between acute infections and risk of acute coronary syndrome: A meta-analysis. Int J Cardiol. 2011;147:479–482. doi: 10.1016/j.ijcard.2011.01.035. This meta-analysis suggests that there is a causal association between acute respiratory tract infection and acute coronary syndrome. [DOI] [PubMed] [Google Scholar]
- 84.Mortensen EM, Copeland LA, Pugh MJ, et al. Diagnosis of pulmonary malignancy after hospitalization for pneumonia. Am J Med. 2010;123:66–71. doi: 10.1016/j.amjmed.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Charlson ME, Pompei P, Ales KL, MackKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]