Abstract
Very young adolescents (VYAs) between the ages of 10 and 14 represent about half of the 1.2 billion adolescents aged 10–19 in the world today. In lower- and middle-income countries, where most unwanted pregnancies, unsafe abortions, maternal deaths and sexually transmitted infections occur, investment in positive youth development to promote sexual and reproductive health (SRH) is increasing. Most interventions, though, focus on older adolescents, overlooking VYAs. Since early adolescence marks a critical transition between childhood and older adolescence and adulthood, setting the stage for future SRH and gendered attitudes and behaviours, targeted investment in VYAs is imperative to lay foundations for healthy future relationships and positive SRH. This article advocates for such investments and identifies roles that policy-makers, donors, programme designers and researchers and evaluators can play to address the disparity.
Keywords: adolescence, very young adolescents, puberty, reproductive health, gender
Introduction
There are 1.2 billion adolescents aged 10–19 in the world today and almost 90% live in lower- and middle-income countries. Half are very young adolescents (VYAs) ages 10–14 (UN Population Division, 2011). Since 1990, several global conferences have focused attention on sexual and reproductive health (SRH) issues affecting adolescents in developing countries, followed by increases in policies and programmes to improve their situation. However, most efforts are directed at older youth and focused on HIV and pregnancy prevention, while the diverse circumstances and needs of younger adolescents – most whom are dealing with emerging fertility and sexuality in the context of rapid puberty changes and not yet sexually active – have been overlooked. This article assesses VYA issues (the term younger adolescent is used interchangeably with VYA) from the ecological and life-course perspective found in the adolescent health framework (Figure 1) recently published in The Lancet (Blum, Bastos, Kabiru, & Le, 2012). The ecological framework examines the multiple effects and interrelatedness of social elements on individuals, while the life-course perspective recognises that individuals construct their own pathway through their choices and actions, tempered by the opportunities and constraints of their experiences and their historical and social circumstances (Elder & Giele, 2009).
Figure 1.
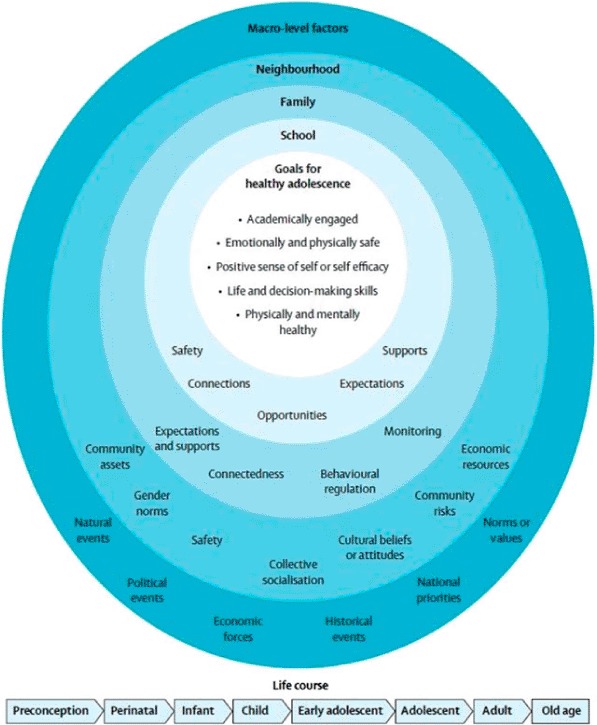
An ecological framework for adolescent health (Blum et al., 2012).
We address the sexual, reproductive and gender role development of younger adolescents during puberty and then move to a discussion of meso-level influences on boys and girls, including families, communities and institutions, such as schools and health services, as well as macro-level influences (specifically, policies). We recognise that gender norms affect all levels and drive SRH and well-being and that it is during the VYA years that gender roles are solidified. Investing in younger adolescents can produce an ‘SRH and gender' dividend by addressing root causes rather than intervening after problems develop. Implementing holistic, gendered policies and programmes that recognise and respond to the unique needs of this life-course phase represents an opportunity to facilitate healthy transitions into adulthood, including initiation of sexual and reproductive life (Blum et al., 2012, Gavin, Catalano, David-Ferdon, Gloppen, & Markham, 2010; Sawyer et al., 2012).
Younger adolescents as healthy individuals
I am not happy that my body is changing into a man's because I don't know how to behave as an older person, I still feel like a child. (VYA boy, Uganda)
I thought what was going on with my body was a curse. Because I didn't like menstruation … [it was not] normal. (VYA girl, Rwanda)
Being healthy in younger adolescence means being not only physically and mentally healthy but also emotionally and physically safe, having a positive sense of self (including emerging gender and sexual identities), decision-making and life skills and academic engagement (Blum et al., 2012). A distinguishing feature of younger adolescence is that the experience of rapid and significant changes brought about by the onset of puberty (Table 1)1 directly affects physical, mental and emotional health, sense of self and self-esteem and the ability to assess risks and consequences. VYAs gain self-awareness as they mature and begin to intensify relationships with their peers. They may feel anxiety and embarrassment over the intense bodily and emotional changes they are experiencing. At a time when sexuality and gender identities are emerging, younger adolescents may experiment with adult sexual behaviours, but because of their cognitive developmental stage, are unlikely to correctly assess risks and consequences (Dixon-Mueller, 2011; UNAIDS, 2004).
Table 1.
Developmental characteristics of early adolescence – age 10–14 years (adapted from Sawyer et al., 2012).
| Physical development | Cognitive development | Social and emotional development |
|---|---|---|
|
|
|
Gender bias, beginning in early childhood, can influence the physical health of younger adolescents; for example, poor nutrition often results in inadequate pelvic structure and anaemia among girls, increasing their likelihood of dying in childbirth (Murphy, 2003). Gender role bias also influences the social domain, the way girls and boys learn to view themselves and behave, at a time when their gender attitudes are forming (Institute for Reproductive Health [IRH], 2010). In many settings, VYA girls are socialised towards ‘helpful’ femininity, while boys are socialised towards hegemonic masculinity; girls take on more adult chores, while boys have fewer responsibilities. Boys may move more freely outside the home, giving them greater opportunities than girls to engage in leisure and income-generating activities (Mensch, Bruce, & Greene, 1998; Ricardo, Barker, Pulerwitz, & Rocha, 2006). Gender role expectations lead to behaviours that disadvantage boys as well, increasing their risk of violence, substance abuse and accidents (Barker & Mikulencak, 2000; Barker & Ricardo, 2005).
Yet information from lower-and middle-income countries on the SRH knowledge, attitudes and behaviours of younger adolescents is scant. Demographic and Health Surveys (DHS) include older adolescents and collect limited retrospective information about age of first intercourse and pregnancy during early adolescence but do not explore knowledge of their sexuality, rights or responsibilities. Surveys collecting information from adolescents, including VYAs (often collected retrospectively from older adolescents), reveal awareness of issues such as consequences of unprotected sex but a lack of accurate SRH knowledge. Misinformation abounds about fertility (first menstruation and ejaculation), sex and sexuality, and VYAs often rely on equally uninformed peers or older siblings and radio, television and other media for information (Albert, Brown, & Flannigan, 2003; Bankole, Biddlecom, Guiella, Singh, & Zulu, 2007; Dixon-Mueller et al., 2007; World Health Organization [WHO], 2010). Misinformation – for example, a belief that one cannot conceive the first time one has sex – may result in unsound sexual decisions (Boonstra, 2007). Around 11% of girls and 6% of boys age 15–19 report having sex before turning 15 (UNICEF, 2011). Extreme violence, including sexual assault and rape, affects at least one-third of all females and a high, possibly rising, proportion of girls younger than 15 years (Bruce, 2011).
Although they may not yet be sexually active, gender role expectations that older VYA boys should begin to experiment sexually to learn to become “real men” reinforce norms that view girls as sex objects. In many settings, VYA girls are expected to be passive, which may lead to situations of male sexual dominance or even coercion (Edmeades, Hayes, Hollingworth, & Warner, 2012). Even when not passive, e.g. younger girls exchanging sex for resources, girls, not their partners, are often held solely accountable for outcomes such as pregnancy or HIV infection. For both sexes, any non-heterosexual feelings or experiences are hidden.
In sum, at a time when sexual feelings and experimentation are beginning, inequitable gender norms are also consolidating, potentially leading to unhealthy behaviours and relationships that result in poor SRH later in life (Edmeades et al., 2012; Murphy, 2003).
Engaging families, schools and neighbourhoods – meso-level influences and challenges
Life for boys and girls is not equal in our community. Boys have freedom but our parents do not allow our sisters to go outside of home. Boys can play games while girls have to look after household chores. Boys should do boyish work, not girl's work. If people in our community see boys doing girlish work they will laugh at them. They are believed to be inferior. (VYA boy, Nepal)
As everywhere, younger adolescents in lower-and middle-income countries move within social systems that significantly influence their life trajectories. With the onset of puberty and fertility, families, schools and neighbourhoods respond to the rapidly changing pubescent individuals in their lives.
Younger adolescents see parents as a primary source of information and support, but most parents are ill-equipped to address issues related to puberty, SRH and gender roles, and lack communication skills attuned to the young adolescents in their lives (IRH, 2010). Parental desire to protect their children is often exercised through behavioural regulation and monitoring rather than through positive support to their growing child, and gender-related ‘rules’ and inequities intensify. Parents begin preparing their daughters for roles as future wives and mothers, while their brothers are given greater mobility and authority over their sisters and other females is expected (Greene & Levack, 2010). Parents worry that their daughters' emerging fertility and sexuality could lead to premarital pregnancy and keep their daughters close to home to ensure safety.
Finally, in many contexts, parents view early marriage (under the age of 18) as protective, despite laws against it (UN Committee on the Rights of the Child, 2003). An estimated, one in nine girls (12%) is married before her fifteenth birthday (Hervish & Feldman-Jacobs, 2011). Concentrated in West Africa and South Asia, early marriage exposes girls to domestic violence, and places them at five times greater risk of death from maternal causes than women aged 20–24 due to under-developed pelvic structures and poor access to maternal health services (Le Fevre, Quiroga, & Murphy, 2004; Mathur, Greene, & Malhotra, 2003; Population Council, 2012; Smith, Ashford, Gribble, & Clifton, 2009).
Educational institutions play prominent roles in younger adolescents' lives. Primary school attendance itself protects against early marriage and its accompanying health risks and allows passage to secondary school and its inherent individual and social benefits (Murphy & Carr, 2007). Schools that exist within cultures that condone physical discipline and violence, however, can also be places where children experience violence, ranging from teasing (e.g. about menstruation and developmental differences) and bullying to sexual harassment or physical and sexual violence (UN Girls' Education Initiative, 2012). If the school system discriminates against girls, or the school environment or travel to school are unsafe, young girls may be withdrawn, increasing their risk of premarital sex or early marriage (Mensch, Clark, Lloyd, & Erulkar, 2001).
Thus, parental and community norms serve to reinforce individuals' behaviours and relationships that lead to poor adult SRH (Murphy, 2003). Community institutions such as schools, which should play a protective role, often have structural issues influenced by gender and cultural norms that diminish protection, particularly for girls in puberty. Of note, VYA-focused health programmes are essentially non-existent.
Challenges of reaching VYAs through organised programmes and platforms
As stated earlier, despite years of ASRH programmes implemented through various platforms – including family life education, youth centres, youth-friendly health services, peer education – programmes for younger adolescents are grossly lacking. VYAs, including those married or otherwise living apart from their families and other vulnerable, hard-to-reach young people, have been excluded. A recent review of (only) 18 evaluated ASRH programmes serving younger adolescents in Africa, South Asia, Latin America and the Caribbean found a predominance of narrowly focused pregnancy- and HIV-prevention interventions, with minimal tailoring for VYAs. Identified programme gaps include overemphasis on facts, inadequate attention to gender norms and protective mesofactors (i.e. involving parents, teachers and neighbourhoods, ensuring safe spaces within community institutions) and failure to build skills for safe transitions into later adolescence and adulthood (IRH, 2009, 2010). Another recent review from sub-Saharan Africa found that most youth-serving organisations reach older youth, often in their early 20s, and more males than females (Bruce & Chong, 2006).
VYA health care needs are neither well-defined nor well-served; most prevention programmes are geared to reducing mortality rates, and younger adolescents are not a high-risk group. Consequently, data on health service utilisation by VYAs is sparse. Too old to be captured by child health services and generally too young to be experiencing pregnancy-related services, there is little demand for or attention to SRH-related services for this age group.
Policy-making and VYAs – influences and challenges of macro-level factors
While a range of macro-environmental factors affects the lives of younger adolescents, including poverty and conflict situations, the macro-level focus in this article is on global and national policies, which set institutional norms and guide programme development, resource allocation and implementation.
International conventions
The Convention of the Rights of the Child (CRC), established in 1989, defines as children all persons up to age 18 unless married or economically emancipated and grants them special protections and entitlements, including the right to safe environments, information, skills and various services, and rights to have their voices heard and to be free of certain adult responsibilities. General comment 4: Adolescent health and development in the context of the CRC, was written in 2003 to support countries in their regular review at the Committee of CRC. In the 1973 Minimum Age Convention, the ILO declares child labour prohibited at age 14 years or younger, except for light work, domestic labour and work in a family enterprise (Dixon-Mueller, 2011; International Planned Parenthood Federation [IPPF], 2006). The Convention on the Elimination of all Forms of Discrimination against Women (CEDAW), adopted in 1979, provides guidance on marriage including consent and a minimum marriage age of 18 years. Registration of all marriages is called for in the 2003 Maputo Protocol. Other world conferences, over the last decade, affirm the rights of youth to high-quality SRH information, education and services.2 Moreover, these conventions promote mutually respectful gender relations, protection from sexual abuse and violence, quality of care and non-discrimination. CRC-ratifying countries have committed to take measures to secure these rights, investigate violations and provide services to victims (Temin & Levine, 2009).
Challenges of enacting protective policies for VYAs
All interested parties want to avoid unwanted pregnancy and STIs among adolescents, yet getting agreement on the correct course of action leads to numerous policy challenges. The rights of VYAs often fall through the cracks, as younger adolescents are not a specific focus of protection or empowerment initiatives, nor are younger adolescents included in policies that deal with child health or SRH, including STIs.
Implementation challenges are numerous. Adolescent sexuality is often a sensitive and controversial topic for parents, communities and governments, and many believe it is too early to talk to younger adolescents about SRH-related issues (ASRH programmes typically focus on family planning and sexual rights). Further, parental rights and protection responsibilities can be at odds with individual VYA rights.
Narrow health promotion approaches, often driven by donors' HIV/AIDS or child-survival priorities, create obstacles to holistic approaches that strengthen protective factors and self-advocacy skills. Even within narrowly defined policies, younger adolescents are squeezed out, falling between child survival initiatives (targeted at children under 5 years) and SRH programmes that serve adolescents 15 years and older.
For those older VYAs who become sexually active, access to contraceptives and safe abortion remains largely unavailable due to regulations requiring parental approval or informal health care policies (WHO, 2011). In many settings, policies discouraging early marriage are undermined by loopholes and inconsistencies in minimum age requirements (in some countries, such as India, girls are permitted to marry earlier than boys) and civil registration systems. Such policies and practices, combined with lack of political will and resources, represent an ongoing challenge in addressing this unique group of adolescents.
Looking forward: building evidence and promising programmes for healthy VYAs
Widespread, effective programmes addressing SRH challenges faced by younger adolescents are possible, but not yet the reality. Evaluated VYA programmes are too few to generate clear programme guidance. The dearth of such programmes is related to the lack of explicit VYA language and content in policy documents, since policies are preconditions for budgeted programmes.
While ASRH programmes have for decades reached a diverse population through multiple channels – school- and community-based services, combined vocational and SRH training, hotlines, community mobilisation and specifically targeted programmes (i.e. married adolescents, boys and parents; Bruce & Chong, 2006; Temin & Levine, 2009) – work is needed to tailor such approaches to younger adolescents.
While there is much to explore before drawing firm conclusions about lessons learned, VYA-specific programming that aims to improve SRH knowledge and behaviours, shapes equitable gender attitudes, strengthens protective factors and mitigates threats can contribute to the VYA SRH and gender dividend and should be a priority. Holistic programmes that (1) provide a space to learn about puberty, fertility and sexuality; (2) allow exploration of attitudes; (3) address gender inequity; and (4) link adolescents to caring parents and other adults, schools, health services and supportive neighbourhoods are key to improving and sustaining VYA well-being. Recommendations from the review of VYA programmes are found in the programme section of Table 2 (IRH, 2010), and several are highlighted below. As these recommendations are put into practice, they will be most effective if they address the specific needs of diverse VYA subgroups, differentiated by age, gender, marital status, school attendance, social status and other relevant factors.
Table 2.
A call to action: Specific recommendations for programmers, researchers and policy-makers.
For programme designers and implementers
For researchers and evaluators
For policy-makers
|
Sources: For programme designers and implementers: Bruce & Chong (2006), ICRW (2010), IRH (2010), Temine and Levine (2009), Palmer (2010).
For researchers and evaluators: Brady (2011), Chong et al. (2006), Dixon-Mueller (2011), IRH (2010), UNAIDS (2004), WHO (2010).
For policy-makers: Bruce and Chong (2006), Dixon-Mueller (2011) and Pathfinder international (2010).
Programmes to reach younger adolescents at large scale
The absolute number of VYAs, and the reality that many ASRH programmes do not operate at scale, means it is important to focus on programmes with potential to reach large numbers of younger adolescents. Given rapidly expanding access in lower-and middle-income countries to Internet and social media, there is potential to achieve significant coverage with media programmes that reinforce positive and gender-transformative messages. Some have demonstrated impact on adolescent knowledge and attitudes and, in rare cases, behaviour (Temin & Levine, 2009). According to a study of adolescents and the media, younger adolescents are aware of social messages communicated through mass media but criticise them as vague and irrelevant to their concerns (UNAIDS, 2004).
Another recommendation identifies the potential of well-designed curriculum-based approaches (e.g. simple, participatory, using social and behaviour change communication concepts) that can be implemented with consistency due to their standardised nature to reach in- and out-of-school VYAs at scale. To encourage and facilitate standardised implementation of school or institution-based sex education worldwide, UNESCO has reviewed curricula from 12 countries and developed a gendered sexual education guidance document – that includes specific guidance for VYAs – for use by education, health and other relevant authorities and organisations (United Nations Educational, Scientific and Cultural Organization [UNESCO], 2009).
Gender-transformative programmes for boys and girls
Early adolescence, when social norms and gender roles are in flux, is an optimal time to encourage gender-transformative programmes (Barker, Ricardo, & Nascimento, 2007; Bruce & Chong, 2006). Gender-transformative programmes – those that promote equal value of females and males and challenge prevailing gender-inequitable norms, rules and roles for girls and boys – can become a gateway for improving a broad range of outcomes, including SRH, mutual respect and non-violence. For sustainable outcomes, adolescent (VYA) programmes should include these objectives and involve parents, teachers, religious leaders and other mentors and ‘gatekeepers’ (Edmeades et al., 2012).
Programmes with focus on families, schools and neighbourhoods
Holistic programmes, that promote healthy adolescence, must reach not only younger adolescents but should also involve parents, teachers, religious leaders and other community members to create a safe, supportive environment for boys and girls at home, in school and elsewhere.
Promoting parenting skills for healthy parent-VYA relationships is particularly critical (WHO, 2007). Adolescents who perceive that they are loved and accepted by their parents or caregivers are less likely to engage in risky behaviours. Evidence reviewed by WHO in over 50 countries found that protective factors such as supportive families, schools and communities and spiritual and ethical beliefs help delay sexual initiation and reduce substance abuse and depression, while family conflict, negative role models and neglectful or disrespectful parenting place VYAs at higher risk (WHO, 2002).
A 2011 study by International Center for Research on Women (ICRW) identified approximately 150 initiatives to prevent child marriage that provide skills and education to girls and also encourage families and communities to change gender norms that perpetuate early marriage. Programmes working directly to empower girls were more effective than efforts to change laws or policies (Malhotra, Warner, McGonagle, & Lee-Rife, 2011). Explicit or not, successful programmes not only built agency and decision-making skills but also increased parental and community connectedness for VYA support.
Programmes for most-vulnerable VYAs
Among the population of 10 – 14-year-olds living in diverse conditions, some VYAs are at greater risk than others and particularly vulnerable to pregnancy, HIV and violence. These include not only married 10 – 14-year-olds but also orphans, refugees, street children, domestic workers and younger adolescents with disabilities; those abused during childhood and gay, lesbian, bisexual, transgendered and questioning youth (Pinheiro, 2006). Although not a focus of this article, these adolescents not only have common needs but also unique concerns; holistic, gendered programme approaches must be tailored to each vulnerable population's context.
Preventive health programmes and services
Preventive health services designed to suit VYA health needs are virtually non-existent in lower-and middle-income countries. Reaching VYA girls and boys for preventive health services would allow for systematic health checks and establish health-seeking behaviours. Services could include nutrition monitoring, mental health checks, HPV vaccinations and sexual/fertility health checks (Temin & Levine, 2009). The concept of youth camps, mobile health services operating at community level to reach VYA girls, boys and their parents has been successfully tested in Uganda (Abeja-Apunyo, 2011).
Looking forward: policy revision and implementation
Encouragingly, international human rights laws are beginning to be applied to VYAs. As documentation of holistic programmes increases and as they become better linked to ongoing ASRH and child health policy dialogues, bottom-up advocacy could begin to influence this critical macro-level barrier to VYA programmes and contribute to the VYA dividend. At the same time, global advocacy to define VYA-specific policy targets could have a top-down effect. See policy recommendations in Table 2.
Looking forward: better policies and programmes through research and evaluation
To design effective VYA programme interventions better evidence is needed about programmes that work. Research and evaluation and better programme monitoring can help identify gaps, create awareness and build consensus among policy-makers that focusing on younger adolescents is a relevant, actionable policy investment.
Research is needed to elucidate the developmental trajectories of VYAs in various settings worldwide, especially where more vulnerable children are located. Identifying the social determinants and developmental assets (Scales & Leffert, 2004) that predispose VYAs to risky behaviour is also a priority. Additional research recommendations appear in Table 2.
A participatory research approach is needed, one that engages younger adolescent boys and girls as competent, reliable informants with their own perspectives to share. Interdisciplinary teams – not only ASRH specialists – could bring perspectives and tools to better capture the wider context of the lives of younger adolescents (WHO, 2011).
Qualitative research and evaluation methods are particularly suited to capturing VYAs' opinions, emotions, values, expectations and hopes. Current research is focused on capturing knowledge and not on the context for sexuality related decision-making (Chong, Hallman, & Brady, 2006; WHO, 2011). Most research methodologies advantage adults in terms of social and communication skills or knowledge (Clark, 2011). Alternative approaches are needed that create trust and rapport between researchers and younger adolescents and that are cognitively appropriate for this age group. Participatory, visually oriented methodologies facilitate rich discussion, especially among younger adolescents, who tend to respond better to non-formal research methods (Clark, 2011; Lundgren, Beckman, Chaurasiya, Subhedi, & Kerner, 2012). Successfully used methodologies and techniques include diary-keeping, game-based methodologies, visual techniques such as photography, drawing or collage, PEER and Think Aloud ACASI.3 (Chong et al., 2006; IRH, 2010; Lundgren et al., 2012; WHO, 2011).
Building evidence for VYA programme best practices has been hindered by lack of documentation and standardised programme indicators. Health information systems do not systematically collect disaggregated data on this age group. Donor programmes supporting global health agendas such as HIV infection and maternal mortality are not collecting information on adolescents (Patton et al., 2012). Government and donor ASRH programmes should prioritise collection of age and sex-disaggregated monitoring data to build evidence on VYA participation. Monitoring and evaluation should be an integral part of VYA programming to identify effective approaches and determine those components critical to success. Organisations should post programme evaluation reports on their websites to help others learn from their experiences (IRH, 2010). Outcome indicators beyond knowledge are imperative, even though it is difficult to operationalise concepts such as gender attitudes and norms, and even more challenging to ascertain whether programmes have effected change. Scales do exist that might be adapted for use with younger adolescents, but there are cognitive development challenges requiring further exploration (IRH, 2010; Lundgren et al., 2012).
Formative, operations and evaluation research (and programmes) with 10- to 14-year-olds require high ethical standards and special protection against exploitation, abuse and other harmful outcomes. Consent and assent, respectively, are required from parents or other legal guardians and from VYAs to ensure they are not complying just to please adults. But contextual challenges remain, and additional guidance needs to be developed. For example, when reaching married, younger adolescent girls, how does one determine whether their (older) husbands are appropriate ‘legal guardians’ to provide support or ethical oversight?
Conclusion and moving forward
[We need] a paradigm shift away from simply thinking about how best to deliver information and services to adolescents who want and need them, towards a more global view of prevention and harm reduction that begins at the societal level and filters down through multiple institutional layers to the individual. (WHO technical consultation, Geneva 2010)
[We need] a portfolio of research on the very young adolescent age group, with the goal of helping researchers and programmers ‘do the research that will lead to guidelines, to policy, and to actions.’ (Dr. Marlene Temmerman of WHO – Inter-Agency Youth Working Group and IRH technical consultation, Washington, DC 2013)
As the VYA population burgeons worldwide, advocates must strive to put this critical group on the global health and development map, moving them from a position of vulnerability to one of empowerment. To achieve scale, concerted efforts are needed to achieve this shift worldwide. As younger adolescents experience rapid transitions to unfamiliar experiences and face life-changing situations such as leaving school, having sex, becoming parents or acquiring HIV, parents, teachers and concerned others have a narrow window of opportunity to facilitate their healthy transition into later adolescence and adulthood. If programmes, based on the healthy adolescent framework, rooted in human rights and gender equity, are implemented at a time when adolescents are still malleable and relatively free of SRH problems and gender role bias, VYAs can be guided safely through this life stage, supported by their parents, families and communities. Investments in emerging SRH and gender role formation among VYAs – working at root level – will yield important dividends, and consequently, fewer investments will be needed later in adolescence and adulthood. The field is nascent; relatively little VYA-specific programming and research has been conducted and disseminated. As more experiences occur and are documented, moving from grey to published literature, the complex theoretical and practical issues and tensions surrounding SRH-related programmes, policies and research for and about younger adolescents will allow practical refinement in all domains. This review of VYA challenges and opportunities represents a call to action for policy-makers, donors, programme designers and researchers/evaluators to broaden their vision for younger adolescents to holistic goals and shift their focus from short- to long-term, sustainable programming. Finally, it will be critical to encourage dialogue with younger adolescents, the significant adults in their lives and local communities and to document and disseminate VYA research and programmatic lessons in order to influence positive investments on behalf of this future generation.
Acknowledgements
The authors would like to thank Jane Ferguson of WHO for her review and pertinent comments of an earlier version of this article and those who provided blind reviews, which informed later improvements in this article. The contents of this document do not necessarily reflect the views or policies of USAID or Georgetown University.
Notes
The timing and pace of these transformations vary widely across individuals and between boys and girls.
The International Conference on Population and Development in 1994, the Fourth World Conference on Women in 1995, the UN Special Session on AIDS in 2001 and the World Summit on Children in 2002.
Participatory Ethnographic Evaluation and Research (PEER) and Audio Computer-Assisted Self-Interviewing (ACASI).
A scheduled health check-up as promoted by Judith Bruce and the Population Council, already a practice in some public health programmes in the USA.
Funding
This publication was made possible through support provided by the US Agency for International Development (USAID) under the terms of the Cooperative Agreement [No. GPO-A-00-07-00003-00].
References
- Abeja-Apunyo C. Final evaluation of the DSW young adolescent pilot program. 2011. (Unpublished).
- Albert B., Brown S., Flanigan C. M. 14 and younger: The sexual behavior of young adolescents. Summary. Washington, DC: National Campaign to Prevent Teen Pregnancy; 2003. [Google Scholar]
- Bankole A., Biddlecom A., Guiella G., Singh S., Zulu E. Sexual behavior, knowledge and information sources of very young adolescents in four sub-Saharan African countries. African Journal of Reproductive Health. 2007;11(3):28. doi: 10.2307/25549730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker G. T., Mikulencak M. What about boys? A literature review on the health and development of adolescent boys. Geneva: Department of Child and Adolescent Health Development, World Health Organization; 2000. [Google Scholar]
- Barker G., Ricardo C. Young men and the construction of masculinity in sub-Saharan Africa: Implications for HIV/AIDS, conflict, and violence. Washington, DC: World Bank; 2005. [Google Scholar]
- Barker G., Ricardo C., Nascimento M. Engaging men and boys in changing gender-based inequity in health: Evidence from programme interventions. Geneva: World Health Organization; 2007. [Google Scholar]
- Blum R. W., Bastos F. I., Kabiru C. W., Le L. C. Adolescent health in the 21st century. The Lancet. 2012;379:1567–1568. doi: 10.1016/S0140-6736(12)60407-3. [DOI] [PubMed] [Google Scholar]
- Boonstra H. Young people need help in preventing pregnancy and HIV; How will the world respond. Guttmacher Policy Review. 2007;10(3):2–8. [Google Scholar]
- Brady M. Calling attention to very young adolescents: Building the evidence base to inform policies and programs. New York, NY: The Population Council; 2011. [Google Scholar]
- Bruce J. Violence against adolescent girls: A fundamental challenge to meaningful equality. Washington, DC: Population Council and UN Adolescent Girls Task Force; 2011. [Google Scholar]
- Bruce J., Chong E. Background paper to Public Choices, Private Decisions: Sexual and Reproductive Health and the Millennium Development Goals. New York, NY: UN Millennium Project; 2006. The diverse universe of adolescents, and the girls and boys left behind: A note on research, program and policy priorities. [Google Scholar]
- Chong E., Hallman K., Brady M. Investing when it counts: Generating the evidence base for policies and programmes for very young adolescents: Guide and tool kit. New York, NY: UNFPA; 2006. [Google Scholar]
- Clark C. D. In a younger voice: Doing child-centered qualitative research. New York, Oxford: Oxford University Press; 2011. [Google Scholar]
- Dixon-Mueller R. The sexual and reproductive health of younger adolescents: Research issues in developing countries. Geneva: World Health Organisation; 2011. Retrieved from http://whqlibdoc.who.int/hq/2011/WHO_RHR_11.11_eng.pdf. [Google Scholar]
- Dixon-Mueller R., Germain A., Fredrick B., Bourne K., Kidwell J., Hilsendager C. Overlooked and uninformed: Young adolescents’ sexual and reproductive health and rights. New York, NY: International Women's Health Coalition; 2007. [Google Scholar]
- Edmeades J., Hayes R., Hollingworth G., Warner A. The girl effect: What do boys have to do with it? Meeting report. Washington, DC: International Center for Research on Women; 2012. [Google Scholar]
- Elder G., Giele J. The craft of life course research. New York, NY: The Guildford Press; 2009. [Google Scholar]
- Gavin L. E., Catalano R. F., David-Ferdon C., Gloppen K. M., Markham C. M. A review of positive youth development programs that promote adolescent sexual and reproductive health. Journal of Adolescent Health. 2010;46(3):S75–S91. doi: 10.1016/j.jadohealth.2009.11.215. [DOI] [PubMed] [Google Scholar]
- Greene M. E., Levack A. Synchronizing gender strategies: A cooperative model for improving reproductive health and transforming gender relations. Washington, DC: USAID Interagency Gender Working Group; 2010. [Google Scholar]
- Hervish A., Feldman-Jacobs C. Who speaks for me: Ending child marriage. Washington, DC: Population Reference Bureau; 2011. [Google Scholar]
- Institute for Reproductive Health. Adolescent and youth sexual and reproductive health program strategy 2009–2012. [Working Paper] Washington, DC: Institute for Reproductive Health, Georgetown University; 2009. [Google Scholar]
- Institute for Reproductive Health. Reaching very young adolescents (VYAs): Advancing program, research and evaluation practices. Washington, DC: Institute for Reproductive Health, Georgetown University; 2010. [Google Scholar]
- International Planned Parenthood Federation. Ending child marriage: A guide for global policy action. London: International Planned Parenthood Federation; 2006. [Google Scholar]
- International Center for Research on Women (ICRW) A briefing note for an expert meeting and workshop. Washington, DC: International Center for Research on Women; 2010 October 5–6. The girl effect: What do boys have to do with it? [Google Scholar]
- Le Fevre J., Quiroga R., Murphy E. Drawn in part from UNICEF report, Early Marriage, Child Spouses (UNICEF 2001) Florence: UNICEF IRC (Innocenti Research Center); 2004. Future options foreclosed: Girls who marry early. [Google Scholar]
- Lundgren R., Beckman M., Chaurasiya S., Subhedi B., Kerner B. Whose turn to do the dishes? Transforming gender attitudes and behaviours among very young adolescents in Nepal. Gender & Development. 2012;12(1):127–145. [Google Scholar]
- Malhotra A., Warner A., McGonagle A., Lee-Rife S. Solutions to end child marriage: What evidence shows. Washington, DC: International Center for Research on Women; 2011. [Google Scholar]
- Mathur S., Greene M., Malhotra A. Too young to wed. The lives, rights, and health of young married girls. Washington, DC: International Center for Research on Women; 2003. [Google Scholar]
- Mensch B., Bruce J., Greene M. The uncharted passage: Girls’ adolescence in the developing world. New York, NY: The Population Council; 1998. [Google Scholar]
- Mensch B. S., Clark W. H., Lloyd C. B., Erulkar A. S. Premarital sex, schoolgirl pregnancy, and school quality in rural Kenya. Studies in Family Planning. 2001;32:285–301. doi: 10.1111/j.1728-4465.2001.00285.x. [DOI] [PubMed] [Google Scholar]
- Murphy E. M. Being born female is dangerous to your health. American Psychologist. 2003;58:205–210. doi: 10.1037/0003-066X.58.3.205. [DOI] [PubMed] [Google Scholar]
- Murphy E., Carr D. Powerful partners. Adolescent girls, education and delayed child bearing. Washington, DC: Population Reference Bureau; 2007. [Google Scholar]
- Palmer L. Advancing promising program and research/evaluation practices for evidence-based programs reaching very young adolescents: A review of the literature. Washington, DC: Institute for Reproductive Health, Georgetown University; 2010. [Google Scholar]
- Pathfinder International. Advancing adolescent and youth sexual and reproductive health in developing countries: Advocacy findings and recommendations. Watertown, MA: Author; 2010. [Google Scholar]
- Patton G. C., Coffey C., Cappa C., Currie D., Riley L., Gore F., Ferguson J. Health of the world's adolescents: A synthesis of internationally comparable data. The Lancet. 2012;379:1665–1675. doi: 10.1016/S0140-6736(12)60203-7. [DOI] [PubMed] [Google Scholar]
- Pinheiro P. Report of the independent expert for the United Nations study on violence against children. New York, NY: United Nations General Assembly Secretary; 2006. [Google Scholar]
- Population Council. Early marriage. 2012. Retrieved from http://www.popcouncil.org/topics/youth_childmarriage.asp.
- Ricardo C., Barker G., Pulerwitz J., Rocha V. Gender, sexual behaviour and vulnerability among young people. In: Ingham R., Aggleton P., editors. Promoting young people's sexual health. London: Routledge; 2006. pp. 61–78. [Google Scholar]
- Sawyer S. M., Afifi R. A., Bearinger L. H., Blakemore S. J., Dick B., Ezeh A. C., Patton G. C. Adolescence: A foundation for future health. The Lancet. 2012;379:1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- Scales P. C., Leffert N. Developmental assets: A synthesis of the scientific research on adolescent development search institute press. 2nd ed. Minneapolis, MN: Search Institute; 2004. [Google Scholar]
- Smith R., Ashford L., Gribble J., Clifton D. Family planning saves lives. 4th ed. Washington, DC: Population Reference Bureau; 2009. [Google Scholar]
- Temine M., Levine R. Start with a girl: A new agenda for global health. Washington, DC: Center for Global Development; 2009. [Google Scholar]
- UNAIDS. Seen but not heard … Very young adolescents aged 10-14 years. Geneva: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2004. [Google Scholar]
- UN Committee on the Rights of the Child. Convention on the rights of the child, general comment 4: Adolescent health and development in the convention on the rights of the child. New York, NY: Author; 2003. [Google Scholar]
- UN Girls’ Education Initiative. Engendering education: Empowerment and equality: A companion volume to the E4 Conferences. New York, NY: Author; 2012. [Google Scholar]
- UNICEF. Adolescence: An age of opportunity—the state of the world's children 2011. New York, NY: Author; 2011. [Google Scholar]
- United Nations Educational, Scientific and Cultural Organization. International technical guidance on sexuality education: An evidence-informed approach for schools, teachers and health educators. Paris: Author; 2009. [Google Scholar]
- UN Population Division. World population in 2010 by region, country and age. New York, NY: Author; 2011. [Google Scholar]
- World Health Organization. Broadening the horizon: Balancing protection and risks for adolescents. Geneva: Author; 2002. [Google Scholar]
- World Health Organization. Helping parents in developing countries improve adolescents health. Geneva: Author; 2007. [Google Scholar]
- World Health Organization. The sexual and reproductive health of young adolescents in developing countries: Reviewing the evidence, identifying research gaps, and moving the agenda. Geneva: Author; 2010. Report of a WHO Technical Consultation, Geneva, November 4–5, 2010. [Google Scholar]
- World Health Organization. Preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries: What the evidence says. 2011. Retrieved from http://whqlibdoc.who.int/hq/2012/WHO_FWC_MCA_12_02.pdf. [PubMed]


