Abstract
There is increasing recognition of the deleterious effects of poor nutrition on health care outcomes. Older patients appear particularly vulnerable to the effects of undernutrition. This includes both low intake as patients and chronic preadmission undernutrition. This study investigates nutrition during a critical intervening period when patients present to a hospital emergency department (ED) in the first half of the day. One third of observed patients sustained periadmission fasts in excess of 18 hours. This fasting period showed significant positive correlation to age (correlation coefficient = 0.34, P < 0.05). Analysis of the results by gender showed that men who were older than the average cohort age of 53.6 years fasted for a significantly longer period in the hospital than their younger counterparts (P < 0.02). This comparison did not reach significant levels for female patients (P > 0.05). This study raises the question as to whether food should be routinely provided in the ED unless there is reason to withhold it. Particular care should be taken to avoid unnecessary delays in offering food to older patients. There may also be a need to ensure that geriatric care indicators are considered individually for each gender.
Keywords: elderly, emergency department (ED), fasting, gender, geriatric, nutrition, starving
INTRODUCTION
The transfer from community to hospital is a stressful time due to acute physical illness, worry, and disturbance to routine. These stresses are potentially greater for the older patient, who will tend to have reduced physical reserves and may be more disoriented by the change of environment. Additional physical stress may be caused by disruption to preadmission nutrition as a result of diminished appetite and practical problems with the buying and preparing of food. Such a period of reduced nutrition may be extended by missed meals during transport to hospital and periods spent in an emergency department (ED).
Poor preadmission nutritional status has been shown to be linked to length of hospital stay, morbidity, and mortality by a number of research groups (1–3). Acute inadequate caloric intake during the first three days after admission has been shown to be associated with increased mortality in older patients (4). Our investigation considers the link period between these two situations when the patient often experiences a period of total fasting.
Short-term fasting during acute illness has been studied in the context of patients undergoing surgery (5, 6) and those in intensive care units (7). The results suggest that fasting has potentially damaging repercussions due to a reduction in insulin sensitivity leading to hyperglycemia, protein catabolism, and diminished immune defense. It is thus prudent to consider whether patients are experiencing extended periods of fasting when they present to the ED, as there will be a subset of these patients who are experiencing significant physiological stress.
The loss of insulin sensitivity has been demonstrated in healthy individuals after short-term fasting (8, 9) and also after surgery following an overnight fast (10). The authors of the first of these studies suggest that breakfast sets metabolism to the normal daytime state after the overnight fast. Insulin resistance is associated with hyperglycemia, which has a demonstrably negative effect on outcomes after surgery and in critical care (11, 12). It has been observed that it is particularly difficult to recover from an established adverse nutritional scenario during physiological stress (13), which reinforces the value of avoiding excessive periods of fasting on initial presentation to hospital.
Insulin resistance is, at least in part, related to loss of lean mass and diminished immune defense. Postsurgical infection has been demonstrated to be associated with an increased number of hyperglycemic episodes for a diabetic cohort (14). Diet has been shown to affect the septic complication rate after severe trauma (15), and overnight fasting has been demonstrated to reduce HLA-DR expression after surgery (16). Postoperative protein and muscle loss are significantly reduced by provision of carbohydrate prior to surgery (5, 17, 18).
Other research has indicated a generally reduced level of comfort in fasted patients (19) with impaired concentration and increased feelings of anxiety, tiredness, hunger, and thirst in presurgical patients who had fasted overnight. A recent study of healthy young women has shown a diminution of physical balance after a 15-hour fast (20)—a similar response in the older population could have effects on mobility and its safety.
The repercussions of a period of fasting are likely to be worse for older patients due to both their reduced physical reserve and increased difficulty in adapting to environmental change. Older subjects demonstrate a different response to periods of nutritional deprivation and have greater difficulty in regaining lost weight (21), particularly lean mass (22). Hunger levels are demonstrably lower in older subjects after an overnight fast (23) and only return some hours after a meal (24). Generally lower levels of hunger during underfeeding (25) make this group more vulnerable to a “switch” to inadequate levels of intake on admission to the hospital. Older patients show greater changes in lymphocyte populations after a 36-hour fast and persisting reductions in neutrophil migration and hydrogen peroxide production (26). They are also more susceptible to delirium, which can complicate care due to distress and reduced ability to communicate health problems to medical staff. The incidence of delirium, which can cause difficulties in both care and diagnosis, can be reduced by providing orientation support including the maintenance of regular biological patterns (27). Thus regular meals may help to combat the bright 24-hour atmosphere of an ED in this respect.
This investigation considers the combined period for which ED patients fast before and after their arrival. These periods are compared for cohorts of older and younger patients and a gender disparity is identified. We found that older individuals fast for significantly longer periods after arrival in the ED and this difference is particularly evident in the case of older men.
METHOD
Inclusion Criteria
Participants were admitted to the Major Treatment Area of a South London ED on four successive weekdays between 0600 and 1330 hours. This area receives all patients who are seriously ill but not in immediately life- threatening danger. All such admissions were included in the study unless they were categorized as belonging to one of the exclusion groups.
Patients were excluded for ethical reasons if they were unable to consent to participation or were aged younger than 18 years. Three further categories of patients were excluded as it was impractical for them to receive nourishment; these were those in need of immediate resuscitation, those attending due to diarrhea/vomiting, and those categorized as “nil by mouth” due to anticipated surgery. Patients in two of the ten nonresuscitation bays were also excluded as their location made it difficult to observe whether food was being provided.
All patients were asked to agree to their anonymous inclusion in a nutritional survey that would require the measurement of their arms and observation of their nutritional intake in the hospital.
No patient declined participation. No patients were lost to follow-up. The total number of participants was 38. The patients were divided into groups according to whether they were older or younger than the average cohort age of 53.6 years. The characteristics of the participants are shown in Table 1.
TABLE 1.
Ages and Middle Upper Arm Circumference (MUAC) of Participants
| Younger women, <53.6 years |
Older women, >53.6 years |
Younger men, <53.6 years |
Older men, >53.6 years |
|||||
|---|---|---|---|---|---|---|---|---|
| Age | MUAC | Age | MUAC | Age | MUAC | Age | MUAC | |
| 20 | 25.3 | 54 | 35.5 | 21 | 30.5 | 58 | 33.8 | |
| 25 | 24.6 | 67 | 22.7 | 25 | 31.3 | 65 | 31.4 | |
| 28 | 28.5 | 70 | 27.8 | 31 | 32.6 | 71 | 29.3 | |
| 28 | 27 | 78 | 29.6 | 35 | 32.4 | 79 | 25.8 | |
| 40 | 32.4 | 79 | 39.5 | 36 | 30 | 79 | 28.3 | |
| 42 | 28.6 | 80 | 26 | 37 | 30.2 | 83 | 31.2 | |
| 43 | 33.3 | 84 | 29 | 38 | 29.3 | |||
| 43 | 33.5 | 89 | 32.7 | 44 | 36.2 | |||
| 43 | 29.8 | 90 | 29.6 | 46 | 39.3 | |||
| 47 | 24.6 | 90 | 24.5 | 49 | 30.1 | |||
| 50 | 30 | 51 | 33.6 | |||||
| Average | 37.2 | 28.9 | 78.1 | 29.7 | 37.5 | 32.3 | 72.5 | 30.0 |
| Number | n = 11 | n = 10 | n = 11 | n = 6 | ||||
Data About Participants
Each participant provided retrospective information about the time when they had last eaten. These interviews all took place within one hour of admission. The date of birth, arrival time, and discharge date for each patient were obtained from hospital records.
Departmental Information
The staff in the ED were aware that patients were being interviewed for a survey about hospital nutrition and that it was not commissioned by hospital management. There are no provisions for the purchase of food within the department and thus any private sources of nutrition need to be brought in by the patient or his or her visitors. Sandwiches and hot drinks are available from ED staff.
Measurements and Observations
Nutritional status
Many of the patients were unable to stand for weighing and thus a proxy measurement was used to represent nutritional status. The British Association for Parenteral and Enteral Nutrition recommends the measurement of mid-upper arm circumference (MUAC) in these circumstances (28). Independent research is supportive of a close relationship between MUAC and body mass index (BMI) (29). The arm diameter was measured mid-way between the left acromion and the left olecranon process. A value less than 23.5 cm is indicative of a BMI less than 20kg/m2 while a value in excess of 32 cm suggests a BMI greater than 30 kg/m2.
Nutrition/discharge events
The participants were observed to establish when they were first offered food at the hospital. The discharge time was noted if this occurred first. The interval between arrival and the earlier of two events, discharge or the offer of food, was recorded as the period of in-hospital fasting.
Analysis of Results
The covariance and standard deviations of the data were used to analyze correlations between age and fasting periods, both before and after arrival at the hospital. Similarly, correlations between age, MUAC, and period of hospital stay were examined. All correlations were tested for significance using Student's t test.
The relationship between age and in-hospital fasting was further analyzed by gender using correlation analysis, a t-test, and the Mann-Whitney U test. Here the participants were divided into two age groups; those below the average age for the cohort and those who were older. The 95% confidence intervals for these gender-age groups were plotted.
The in-hospital fasting period was also correlated to age for the subset of patients who were provided with food in hospital.
RESULTS
The average prehospital fast was 9.0 hours; the average in-hospital fast was 4.2 hours. One third of patients experienced a total fast in excess of 18 hours; 13% fasted for more than 22 hours (Table 2).
TABLE 2.
Fasting Periods
| Total period of fast |
Prehospital |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Average fast (hrs) |
> 18 hrs |
> 22 hrs |
40 hrs |
≥ 12 hrs |
|||||||
| Participants | Prehosp | In-hosp | Total period | n | % | n | % | n | % | n | % |
| Age < 53.6 yrs | 10.5 | 3.7 | 14.1 | 8 | 36 | 3 | 14 | 2 | 9 | 15 | 41 |
| Age > 53.6 yrs | 6.9 | 4.8 | 11.9 | 5 | 31 | 2 | 13 | 0 | 0 | 9 | 38 |
| All participants | 9.0 | 4.2 | 13.2 | 13 | 34 | 5 | 13 | 2 | 5 | 6 | 39 |
Note. Prehosp = before Emergency Department arrival; In-hosp = after arrival; hrs = hours; yrs = years; n = number.
There were significant positive correlations between age and both duration of hospital stay and the in-hospital fasting period (Age/hospital stay = 0.52 P ≤ 0.001; age/in-hospital fasting = 0.34 P ≤ 0.05) (Table 3).
TABLE 3.
Correlations With Age
| Prehospital fasting period |
In-hospital fasting period |
Total fasting period |
Hospital stay |
|||||
|---|---|---|---|---|---|---|---|---|
| Participants | Correlate | Probability | Correlate | Probability | Correlate | Probability | Correlate | Probability |
| All | −0.21 | NS | 0.34 | <0.05 | −0.12 | NS | 0.52 | <0.001 |
| Women | −0.27 | NS | 0.20 | NS | −0.20 | NS | 0.50 | <0.05 |
| Men | −0.11 | NS | 0.66 | <0.005 | 0.03 | NS | 0.60 | <0.05 |
Gender analysis of the correlation between age and the in-hospital fasting period indicated that there was a significant correlation for men (male age/in-hospital fasting = 0.66 P ≤ 0.005) but not for women (female age/in-hospital fasting = 0.20 P > 0.05) (Table 3). Average in-hospital fasting periods for each group are shown in Figure 1. The Mann-Whitney U test describes the relationship on a more stringent basis by considering the participants in two age-defined groups (under and over the cohort average of 53.6 years). This shows a significant result for the in-hospital fasting of older men relative to younger men (U = 7, n1 = 11, n2 = 6, P < 0.02) while the comparison for the whole group does not reach a 5% level of significance (U = 114, n1 = 22, n2 = 16, P ≤ 0.1) (Table 4).
FIGURE 1.
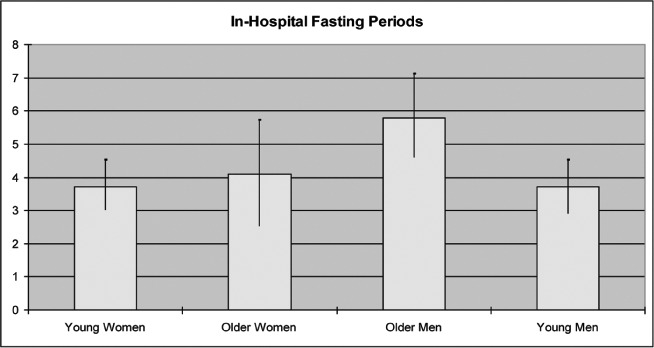
Average hours of in-hospital fasting with 95% confidence intervals. Young women 3.73 ± 0.74 (n = 11), older women 4.10 ± 1.63 (n = 10), young men 3.73 ±0.80 (n = 11), older men 5.83 ±1.23 (n = 6). There is a significant difference between the values for older and younger men (P < 0.05). (Color figure available online.)
TABLE 4.
Fasting Periods (Hours) Compared for Younger and Older Patients
| 95% Confidence intervals for fasting periods |
Mann whitney U values |
||||||
|---|---|---|---|---|---|---|---|
| Participants | Prehospital | In-hospital | Total | U | n1 | n2 | Significance |
| Young women | 3.8–19.8 | 3.0–4.5 | 7.4–23.3 | 51 | 11 | 10 | NS |
| Older women | 1.4–10.6 | 2.5–5.7 | 4.8–16.0 | ||||
| Young men | 2.2–16.2 | 2.9–4.5 | 5.8–19.8 | 7 | 11 | 6 | P < 0.02 |
| Older men | 2.8–13.9 | 4.6–7.1 | 9.0–19.7 | ||||
| All young | 6.2–14.8 | 3.2–4.7 | 8.3–17.2 | 114 | 22 | 16 | P < 0.1 |
| All older | 4.5–14.0 | 3.7–5.3 | 9.0–18.5 | ||||
The in-hospital fasting period was examined further by excluding all participants who left the hospital before they had received food. This led to an increased correlation between male age and the in-hospital fasting period of 0.79 (P ≤ 0.02) while the relationship remained nonsignificant for female patients (—0.04, P > 0.05) (Table 5).
TABLE 5.
Patients Who Received Food in Hospital—Correlation Between Age and In-hospital Fasting Period
| Age: In-hospital fasting period |
||
|---|---|---|
| Participants | Correlate | Probability value |
| All | 0.34 | insignificant |
| Women | −0.04 | insignificant |
| Men | 0.79 | P < 0.02 |
There was a nonsignificant negative relationship between age and the prehospital fasting period (Table 3).
Only one patient had a MUAC measurement suggestive of underweight status (MUAC < 23.5 cm). A total of 32% of participants had MUAC measurements in excess of 32 cm, thus indicating a likelihood of obesity (Table 1). This factor did not show a significant relationship to length of hospital stay or fasting periods, which is unsurprising in view of the absence of a malnourished cohort.
DISCUSSION
The consideration of prehospital fasting in conjunction with the unfed period in the ED leads to the recognition that patients are often without food for many hours. Glycogenolysis shows a straight-line fall for the first 22 hours of fasting (30) while gluconeogenesis increases and becomes critical after 18–24 hours (31, 32). This suggests that adverse metabolic shifts may be minimized by aiming to hold total fasting periods fewer than 18 hours for ED patients. A total of 34% of participants in this study fasted for longer than 18 hours. Had food been provided within an hour of registration, this number would have been reduced to 10.5%.
In-hospital fasting is shorter than prehospital fasting but is more easily addressed by such interventions. The period has probably reduced in recent years due to shorter stays in the ED as observations during this study indicated that food was generally offered when patients were transferred to a ward. These patients were not in need of emergency resuscitation or deemed “nil by mouth,” and many of them could have received food on arrival at the hospital if this were the default position in recognition of the fact that patients often arrive after an extended period of fasting. An alternative, more limited, solution would be the placement of food vending facilities within the ED.
The delay in receiving food, once in the hospital, was significantly greater for the older cohort in this study despite the fact that they are a more vulnerable group. The issue became even more significant when the provision of food to older men was compared to that provided to younger men. The reasons for these variations are unclear although a number of possible causes can be excluded:
The data were examined to establish whether this was due to accompanying family members feeding younger patients, but this only occurred on two occasions and both of the recipients were female.
Another possibility was that the older patients were less likely to be discharged quickly, without food, and thus register a shorter in-hospital fasting period. However the correlation of the in-hospital fast with age increased when considering only male patients who received food in the hospital.
Refusal of food did not explain the results since being offered food was counted as discharging the fast. There was, in fact, one such refusal in each of the four gender-age groups.
Requests for food did not appear to be more numerous in the younger or female cohorts. Only one patient, an older man, was observed to request food and this effect therefore reduced the observed discrepancies.
It is possible that younger patients are generally dealt with in a more timely fashion because they are perceived to be “busy people” who do not have unlimited spare time and this could extend to offering them refreshments more quickly. There is research that supports a low regard for elderly nutritional need by hospital staff, which is based on a questionnaire completed by nurses in geriatric units. One might expect particularly high standards in such a unit, but only 53% of participants were described as having a positive attitude to factors of importance for nutritional nursing care (33).
The gender discrepancy reflected by the greater delay in feeding older men is even more difficult to explain. It raises the possibility that this population may be vulnerable to poorer care levels generally and that these may be masked by failure to examine such issues on a gender basis. A similar “masking” of poorer care to a specific group is described in research where consideration of geriatric care indicators shows that general indicators can miss weaknesses for a more vulnerable subgroup (34). It may be that older men have a less demanding appearance—they are said to “suffer more quietly” by one researcher (35)—or they may arouse fewer nurturing emotions in their carers. The importance of this effect may be magnified by the fact that older men are the group who are most vulnerable to sarcopenia as a result of hospital weight loss because weight replacement afterwards fails to replenish the lean tissue that has been lost (22).
This is a small study with a number of limitations. The observations could be atypical as they are restricted to a single hospital ED. The lack of an undernourished cohort and the exclusion of patients who could not give consent mean that two particularly vulnerable groups were not included in the study. There is potential recall bias about prehospital fasting, as that information could not be confirmed objectively. However, this was minimized by ensuring that interviews were completed within an hour of admission. The need to gain consent from participants meant that both they, and the ED staff, were aware that a nutritional study was in progress, which may have caused them to modify their behavior. This may mean, for example, that patients were offered food more regularly, although it is less likely that any such changes would have varied by age or gender.
TAKE AWAY POINTS
We studied pre- and postadmission fasting in patients admitted to a London Emergency Department and examined potential age and gender differences in the duration.
Acute inadequate caloric intake around the time of hospital admission has been linked with poor outcomes, especially in older patients.
Of the participants in this investigation, 34% fasted for an excess of 18 hours. This value would have been reduced to 10.5% by providing food within one hour of arrival in the Emergency Department.
Compared to younger patients, older patients waited for a significantly longer period (average of 4.8 hours) before they were served food within the hospital (correlation with age: 0.34, P < 0.05). Particular effort needs to be made to avoid an extended delay in this more vulnerable patient group.
The observed age-related delay in receiving food exceeded 95% significance in the male cohort but not the female cohort (correlation with age: male 0.66 P < 0.005, female 0.20 P > 0.05). This raises the question as to whether geriatric care indicators may mask similarly reduced levels of care when they are not considered on a gender-specific basis.
Our findings support a default recommendation of providing food within one hour for Emergency Department patients for whom there is no clinical reason for starvation.
REFERENCES
- 1.Feldblum I, German L, Bilenko N, Shahar A, Enten R, Greenberg D, et al. Nutritional risk and heath care use before and after an acute hospitalisation among the elderly. Nutrition. 2009;25:415–20. doi: 10.1016/j.nut.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Lumbers M, Driver LT, Howland RJ, Older MWJ, William CM. Nutritional status and clinical outcome in elderly female surgical orthopaedic patients. Clin Nutr. 1996;15:101–7. doi: 10.1016/s0261-5614(96)80033-1. [DOI] [PubMed] [Google Scholar]
- 3.Stratton RJ, King CL, Stroud MA, Jackson AA, Elia M. “Malnutrition Universal Screening Tool” predicts mortality and length of hospital stay in acutely ill elderly. Br J Nutr. 2006;95:325–30. doi: 10.1079/bjn20051622. [DOI] [PubMed] [Google Scholar]
- 4.Incalzi RA, Capparella O, Gemma A, Landi F, Pagano F, Cipriani L, Carbonin P. Inadequate caloric intake: a risk factor for mortality of geriatric patients in the acute-care hospital. Age Ageing. 1998;27:303–10. [Google Scholar]
- 5.Svanfeldt M, Thorell A, Hausel J, Soop M, Rooyackers O, Nygren J, Ljungqvist O. Randomized clinical trial of the effect of preoperative oral carbohydrate treatment on postoperative whole-body protein and glucose kinetics. Br J Surg. 2007;94(11):1342–50. doi: 10.1002/bjs.5919. [DOI] [PubMed] [Google Scholar]
- 6.Diks J, van Hoorn DEC, Nijveldt RJ, Boelens PG, Hofman Z, Bouritius H, et al. Preoperative fasting: an outdated concept? J Parenter Enteral Nutr. 2005;29(4):298–304. doi: 10.1177/0148607105029004298. [DOI] [PubMed] [Google Scholar]
- 7.Doig GS, Heighes PT, Simpson F, Sweetman EA, Davies AR. Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials. Intensive Care Med. 2009;35:2018–27. doi: 10.1007/s00134-009-1664-4. [DOI] [PubMed] [Google Scholar]
- 8.Nygren J, Thorell A, Brismar K, Karpe F, Ljungqvist O. Short-term hypocaloric nutrition but not bed rest decrease insulin sensitivity and IGF-1 bioavailability in healthy subjects: the importance of glucagon. Nutrition. 1997;13(11–12):945–51. doi: 10.1016/s0899-9007(97)00335-3. [DOI] [PubMed] [Google Scholar]
- 9.Svanfeldt M, Thorell A, Hausel J, Soop M, Nygren J, Ljungqvist O. Effect of “pre- operative” oral carbohydrate treatment on insulin action—a randomised cross-over unblended study in healthy subjects. Clin Nutr. 2005;24:815–21. doi: 10.1016/j.clnu.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Soop M, Nygren J, Myrenfors P, Thorell A, Ljungqvist O. Preoperative oral carbohydrate treatment attenuates immediate postoperative insulin resistance. Am J Physiol Endocrinol Metab. 2001;280:E576–E583. doi: 10.1152/ajpendo.2001.280.4.E576. [DOI] [PubMed] [Google Scholar]
- 11.Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. NEJM. 2001;345(19):1359–67. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 12.Soop M, Nygren J, Thorell A, Ljungqvist O. Stress-induced insulin resistance: recent developments. Curr Opin Clin Nutr Metab Care. 2007;10(2):181–6. doi: 10.1097/MCO.0b013e32801481df. [DOI] [PubMed] [Google Scholar]
- 13.Tappy L, Berger HM, Chiolero RL. Nutrition and stress. Annales de Medecine Interne. 2000;151(7):584–93. [PubMed] [Google Scholar]
- 14.Pomposelli JJ, Baxter JK, Babineau TJ, Pomfret EA, Driscoll DF, Forse RA, Bistrian BR. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr. 1998;22(2):77–81. doi: 10.1177/014860719802200277. [DOI] [PubMed] [Google Scholar]
- 15.Kudsk KA, Minard G, Croce MA, Brown RO, Lowrey TS, Pritchard FE, et al. A randomized trial of isonitrogenous enteral diets after severe trauma—an immune-enhancing diet reduces septic complications. Ann Surg. 1996;224(4):531–40. doi: 10.1097/00000658-199610000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melis GC, van Leewen PAM, von Blomberg-van der Flier BME, Goedhart-Hiddinga AC, Uitdehaag BMJ, et al. A carbohydrate-rich beverage prior to surgery prevents surgery-induced immunodepression: a randomized, controlled, clinical trial. J Parenter Enteral Nutr. 2006;30(1):21–6. doi: 10.1177/014860710603000121. [DOI] [PubMed] [Google Scholar]
- 17.Crowe PJ, Dennison A, Royle GT. The effect of pre-operative glucose loading on postoperative nitrogen metabolism. Br J Surg. 1984;71:636–7. doi: 10.1002/bjs.1800710828. [DOI] [PubMed] [Google Scholar]
- 18.Yuill KA, Richardson RA, Davidson HIM. Garden OJ, Parks RW. The administration of an oral carbohydrate-containing fluid prior to major elective upper- gastrointestinal surgery preserves skeletal muscle mass postoperatively—a randomised trial. Clin Nutr. 2005;24(1):32–7. doi: 10.1016/j.clnu.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Hausel J, Nygren J, Lagerkranser M, Hellstrom PM, Hammarqvist F, Almstrom C, et al. A carbohydrate-rich drink reduces preoperative discomfort in elective surgery patients. Anesth Analges. 2001;93(5):1344–50. doi: 10.1097/00000539-200111000-00063. [DOI] [PubMed] [Google Scholar]
- 20.Johnson S, Leck K. The effects of dietary fasting on physical balance among healthy young women. Nutr J. 2010;9:18. doi: 10.1186/1475-2891-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts SB, Fuss P, Heyman MB, Evans WJ, Tsay R, Rasmussen H, et al. Control of food intake in older men. JAMA. 1994;20:1601–6. doi: 10.1001/jama.1994.03520200057036. [DOI] [PubMed] [Google Scholar]
- 22.Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, et al. Weight change and the conservation of lean mass in old age: the health, aging and body composition study. Am J Clin Nutr. 2005;82:872–8. doi: 10.1093/ajcn/82.4.872. [DOI] [PubMed] [Google Scholar]
- 23.Serra-Prat M, Palomera E, Clave P, Puig-Domingo M. Effect of age and frailty on ghrelin and cholecystokinin responses to a meal test. Am J Clin Nutr. 2009;89:1410–7. doi: 10.3945/ajcn.2008.27076. [DOI] [PubMed] [Google Scholar]
- 24.Di Francesco V, Zamboni M, Dioli A, Zoico E, Mazzali G, Omizzolo F, et al. Delayed postprandial gastric emptying and impaired gallbladder contraction together with elevated cholecystokinin and peptide YY serum levels sustain satiety and inhibit hunger in healthy elderly persons. J Gerontol. 2005;60A(12):1581–5. doi: 10.1093/gerona/60.12.1581. [DOI] [PubMed] [Google Scholar]
- 25.Moriguti JC, Das SK, Saltzman E, Corrales A, McCrory MA, Greenberg AS, Roberts SB. Effects of a 6-week hypocaloric diet on changes in body composition, hunger and subsequent weight regain in healthy young and older adults. J Gerontol. 2000;12:B580–B587. doi: 10.1093/gerona/55.12.b580. [DOI] [PubMed] [Google Scholar]
- 26.Walrand S, Moreau K, Caldefie F, Tridon A, Chassagne J, Portefaix G, et al. Specific and non-specific immune responses to fasting and refeeding in healthy young adult and elderly persons. Am J Clin Nutr. 2001;74:670–8. doi: 10.1093/ajcn/74.5.670. [DOI] [PubMed] [Google Scholar]
- 27.Vidan MT, Sanchez E, Alonso M, Montero B, Ortiz J, Serra JA. An intervention integrated into daily clinical practice reduces the incidence of delirium during hospitalisation in elderly patients. JAGS. 2009;S7:2029–36. doi: 10.1111/j.1532-5415.2009.02485.x. [DOI] [PubMed] [Google Scholar]
- 28.British Association for Parenteral and Enteral Nutrition. Malnutrition Universal Screening Tool. Accessed at http://www.bapen.org.uk/pdfs/must/must_full.pdf on 23 February 2010.
- 29.Powell-Tuck J, Hennessy EM. A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin Nutr. 2003;22(3):307–12. doi: 10.1016/s0261-5614(03)00009-8. [DOI] [PubMed] [Google Scholar]
- 30.Rothman DL, Magnusson I, Katz LD, Shulman RG, Shulman GI. Quantitation of hepatic glycogenolysis and gluconeogenesis in fasting humans with 13C NMR. Science. 1991;254(5031):573–6. doi: 10.1126/science.1948033. [DOI] [PubMed] [Google Scholar]
- 31.Klover PJ, Mooney RA. Hepatocytes: critical for glucose homeostasis. Int J Biochem Cell Biol. 2004;36:753–8. doi: 10.1016/j.biocel.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Sprangers F, Thien HV, Ackermans MT, Endert E, Sauerwein HP. Glycogenolysis during short-term fasting in malaria and healthy subjects—the potential regulatory role of glycogen content on glycogen breakdown: a hypothesis. Clin Nutr. 2004;23:1051–9. doi: 10.1016/j.clnu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Bachrach-Lindstrom M, Jensen S, Lundin R, Christensson L. Attitudes of nursing staff working with older people towards nutritional nursing care. J Clin Nurs. 2007;16:2007–14. doi: 10.1111/j.1365-2702.2006.01868.x. [DOI] [PubMed] [Google Scholar]
- 34.Arora VM, Johnson M, Olson J, Podrazik PM, Levine S, DuBeau CE, et al. Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders. JAGS. 2007;55:1705–11. doi: 10.1111/j.1532-5415.2007.01444.x. [DOI] [PubMed] [Google Scholar]
- 35.Brantervik AM, Jacobbson IE, Grimby A, Wallen TCE, Bosaeus IG. Older hospitalised patients at risk of malnutrition: correlation with quality of life, aid from the social welfare system and length of stay? Age Ageing. 2005;34:444–9. doi: 10.1093/ageing/afi125. [DOI] [PubMed] [Google Scholar]


