Abstract
Context
Chelation therapy with disodium ethylene diamine tetraacetic acid (EDTA) has been used for over 50 years to treat atherosclerosis without proof of efficacy.
Objective
To determine if an EDTA-based chelation regimen reduces cardiovascular events.
Design and Setting
Double-blind placebo-controlled 2×2 factorial multicenter randomized trial. NIH Funding was approved in August 2002. The first patient was enrolled in September 2003, and the last follow-up took place in October 2011. Median follow-up was 55 months. Participants were recruited from 134 US and Canadian clinical sites.
Participants
1708 patients, age 50 or older and at least 6 weeks post myocardial infarction, with a serum creatinine <2.0 mg/dL. 289 patients (17% of total; 115 in the EDTA group and 174 in the placebo group) withdrew consent for continued follow-up over the course of the trial.
Interventions
Patients were randomized to receive 40 infusions of a 500 mL chelation solution (containing 3 grams of disodium EDTA, 7 grams of ascorbate, B-vitamins, electrolytes, procaine, and heparin) versus placebo, and to an oral vitamin and mineral regimen or an oral placebo. Infusions were administered weekly for 30 weeks, followed by 10 infusions 2 to 8 weeks apart. Patients received 55,222 infusions. 15% discontinued infusions for adverse events.
Main outcome measure
The pre-specified primary endpoint was a composite of total mortality, recurrent myocardial infarction, stroke, coronary revascularization, or hospitalization for angina. Followup for clinical events began upon randomization. This report describes the intent-to-treat comparison of EDTA chelation versus placebo. To account for multiple interim analyses, the significance threshold required at the final analysis was p=0.036.
Results
The qualifying myocardial infarction occurred a median of 4.6 years before enrollment. Median age was 65 years, 18% were female, 9% were nonwhite, 31% were diabetic. 83% had prior coronary revascularization, and 73% were on statins. The primary endpoint occurred in 222 (26%) of the chelation group and 261 (30%) of the placebo group (hazard ratio 0.82, 95% confidence interval 0.69–0.99, p=0.035). There was no effect on total mortality (chelation: 87 deaths (10%) placebo 93 (11%): hazard ratio (HR) 0.93, 95% confidence interval 0.70–1.25, p=0.64), but the study was not powered for this comparison. The effect of EDTA chelation on the components of the primary endpoint other than death was of similar magnitude as its overall effect (myocardial infarction HR 0.77 95% confidence interval (0.54,1.11); stroke HR 0.77 95% confidence interval (0.34, 1.76); coronary revascularization HR 0.81 95% confidence interval (0.64, 1.02); hospitalization for angina HR 0.72 95% confidence interval (0.35, 1.47). Extensive sensitivity analyses examining the effect of patient drop out and varying treatment compliance did not alter the study’s conclusions.
Conclusions and Relevance
In stable patients with a history of MI, the use of an intravenous chelation regimen with disodium EDTA, compared with placebo, modestly reduced the risk of a composite of adverse cardiovascular outcomes, many of which were revascularization procedures. These results provide evidence to guide further research but are not, by themselves, sufficient to support the routine use of chelation therapy for treatment of post-MI patients.
Keywords: chelation, EDTA, vitamin C, myocardial infarction, diabetes, alternative medicine
INTRODUCTION
The treatment of lead toxicity with chelation was first reported with ethylenediamine tetra acetic acid (EDTA) in the early 1950s1. Apparent success in reducing metastatic calcium deposits2 led Clarke3, in 1956, to treat angina patients with EDTA, and others to use chelation for various forms of atherosclerotic disease4,5,6. Chelation therapy evolved to constitute infusions of vitamins and disodium EDTA, a drug that binds divalent and some trivalent cations, including calcium, magnesium, lead, cadmium, zinc, iron, aluminum, and copper, facilitating their urinary excretion 7,8. Over the next decades, based on favorable anecdotal and case report experience, chelation practitioners increased their use of EDTA for coronary and peripheral artery disease. The 2007 National Health Statistics Report compared chelation use since 2002 and noted an increase of 68%, from 66,000 to 111,000 adults using chelation therapy9, although the indications for therapy were not clearly defined.
Three small clinical trials have assessed the effects of chelation on surrogate outcomes, such as walking distance in patients with claudication (2 trials, 185 patients total) and time to exercise-induced ischemia in patients with coronary disease (1 trial, 84 patients). These studies did not find any evidence of treatment efficacy but were underpowered for evaluation of clinical events 10,11,12. As a consequence, mainstream medical organizations consider the therapeutic value of chelation for atherosclerotic vascular disease unproven13 and the use of this therapy potentially dangerous. Disodium EDTA, particularly when infused too rapidly, may cause hypocalcemia and death 14. The Trial to Assess Chelation Therapy (TACT, clinical trials.gov identifier NCT00044213) was conducted to respond to the public health problem posed by EDTA chelation therapy: large numbers of patients being exposed to undefined risks for unproven benefits.
METHODS
Overview
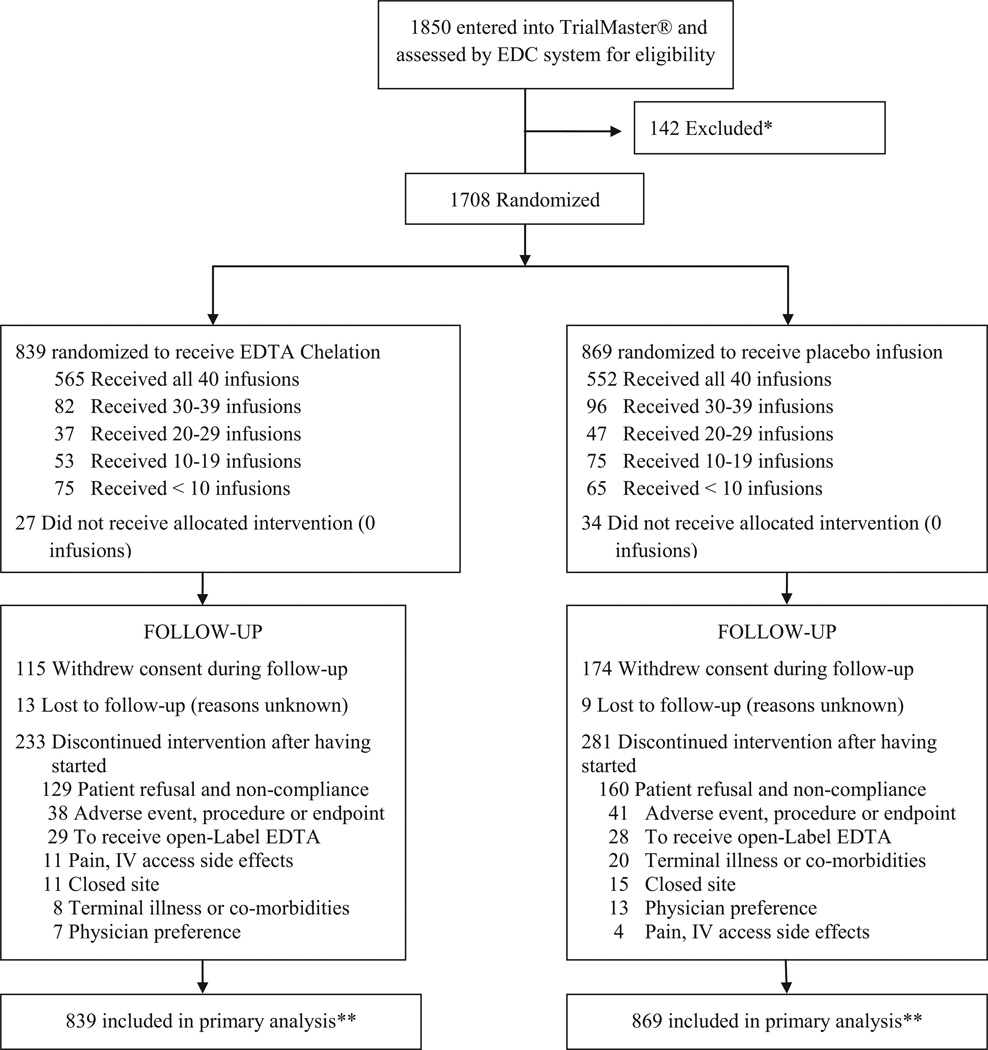
TACT was a double-blind 2×2 factorial trial: patients were randomized to receive 40 infusions of disodium EDTA chelation or placebo, and additionally to an oral high-dose vitamin and mineral regimen or placebo. Details of the study protocol have been published.15 This report describes the results of the EDTA chelation versus placebo comparison (Figure 1).
Figure 1.
TACT Consort Diagram
* Screened patients not randomized due to inclusion/exclusion criteria, unwillingness to participate, or other reasons.
** All patients were included in the primary “time to event” analysis for the duration of their follow-up, including the patients who withdrew consent or were lost to follow-up.
The National Heart, Lung, and Blood Institute (NHLBI) and the National Center for Complementary and Alternative Medicine (NCCAM) provided sponsorship (RFA-AT-010004) and oversight. The US Food and Drug Administration approved an Investigational New Drug application for disodium EDTA for coronary artery disease. A data and safety monitoring board (DSMB), appointed by NCCAM (the primary institute at the time) and approved by Directors of both sponsoring institutes, monitored patient safety, treatment effects, and the conduct of the trial. Institutional Review Boards approved the final protocol and provided ongoing oversight. All patients provided written informed consent. The Duke Clinical Research Institute (DCRI) performed data management and statistical analyses. The authors had full access to all the data, performed all the analyses and are responsible for the final contents and conclusions. No companies or commercial entities provided funding or had any role in the execution, interpretation or submission for publication of this work.
Study population
Eligible patients were at least 50 years of age and had sustained a myocardial infarction 6 weeks or more prior to enrollment. Patients were ineligible if they were women of childbearing potential, had a serum creatinine >2.0 mg/dL, platelet count <100,000/mm3, abnormal liver function studies, blood pressure >160/100 mmHg, past intolerance to the chelation or vitamin components, chelation therapy within 5 years, coronary or carotid revascularization planned or having taken place within 6 months, cigarette smoking within 3 months, active heart failure or heart failure hospitalization within 6 months, or inability to tolerate 500cc infusions weekly15. Patients were enrolled at 134 sites, of which 81 (60%) were sites in which chelation therapy was already practiced. Race and ethnicity were self-reported and collected as required in federally-funded trials.
Treatment
The refrigerated blinded active chelation solution was prepared by a central pharmacy with the ascorbate and EDTA in two separate syringes and shipped to arrive at the sites within 24 hours of preparation. Placebo infusions were shipped with identical packaging and two separate placebo syringes. Following mixing, the sites were instructed to infuse within 24 hours. The active, 10-component, chelation solution was selected to most closely match the standard solution used by chelation practitioners16, and consisted of up to 3 grams disodium EDTA, adjusted downward based on estimated glomerular filtration rate, 7 grams of ascorbic acid, 2 grams of magnesium chloride, 100 mg of procaine HCl, 2500 U of unfractionated heparin, 2 mEq potassium chloride, 840 mg sodium bicarbonate, 250 mg pantothenic acid, 100 mg thiamine, 100 mg pyridoxine, and sterile water to make up 500 mL of solution. The identical-appearing placebo solution consisted of 500 mL of normal saline and 1.2% dextrose (2.5 grams total). The chelation or placebo infusions were administered through a peripheral intravenous line – weekly for the first 30 infusions, followed by an additional 10 infusions 2 to 8 weeks apart. Infusions were administered over at least 3 hours unless the serum calcium corrected for albumin concentration was between 8.0 and 8.5 mg/dL, or the patient was unable to tolerate the 3-hour infusion due to heart failure. In those cases the infusions were administered more slowly. During the infusion phase of the trial, all study patients, including those randomized to placebo infusions, received a daily low-dose vitamin regimen consisting of vitamin B6 25 mg, zinc 25 mg, copper 2 mg, manganese 15 mg, and chromium 50 mcg, to prevent potential depletion by the chelation regimen. Investigators were trained in and monitored for the use of evidence-based post-MI therapy.
Follow-up
Study follow-up for clinical events began upon randomization. Patients were seen at baseline, and at each of the 40 infusion visits. Following the infusion phase, patients were called quarterly; attended annual clinic visits; and were seen at the end of the trial or at the 5 year follow-up, whichever was first. Patient follow-up continued without censoring if a non-mortal endpoint occurred.
Safety
Safety monitoring included periodic physical examinations and laboratory assessments. These included glucose, calcium, renal function, hepatic function, and hematologic parameters. Patients had body weight assessed prior to infusions, to determine whether there was fluid retention. Infusions were delayed until specific abnormal physical or laboratory findings resolved. Rapid infusions were reported electronically to the coordinating centers. A medical monitor at DCRI masked to patient treatment assignment reviewed deaths and unexpected serious adverse events.
Endpoints
The primary endpoint was a composite of death from any cause, reinfarction, stroke, coronary revascularization, or hospitalization for angina. The composite of cardiovascular death, reinfarction, or stroke was a prespecified secondary endpoint. A blinded independent clinical events committee at Brigham and Women’s Hospital adjudicated all non-procedural components of the primary end-point. The occurrence of coronary revascularizations was verified from the source medical record by DCRI.
Pre-Specified Subgroups
TACT pre-specified several subgroups for analyses based on assessing under-represented populations (women and minorities), the elderly (age >70 years), high risk patients (MI location, diabetes and metabolic syndrome); and other subgroups of interest (time from index MI to trial enrollment, patients in whom statin therapy was not being used). We also assessed any interaction of the infusion therapy with the oral high-dose vitamin and mineral component of the factorial trial, and with the type of enrolling site (chelation practice versus not a chelation practice).
Statistical analysis
TACT originally planned to enroll 2372 patients over 3 years with a minimum follow-up of 1 year. This number provided 85% power for detecting a 25% relative reduction in the primary endpoint, assuming a 2.5-year event rate in the placebo arm of 20% and a level of significance of 0.05. In July 2009, continued difficulties in recruitment of patients led the blinded investigators to request approval from the DSMB for a reduction of total enrollment to 1700, with a compensatory extension in the length of follow-up to maintain the same level of unconditional statistical power as described above for the original sample of 2372 patients. The DSMB approved the request, and 1708 patients were randomized. The follow-up period for the trial closed October 31, 2011, approximately 1 year after the last patient was enrolled. (see Supplementary Appendix for additional details)
Secure web-based randomization was performed using permuted blocks stratified by clinical site. Time 0 was defined as the time of randomization. Treatment comparisons were performed according to the intention-to-treat principle and included all patients in the arm to which they were randomized and all follow-up information that was available on each patient. Patients who withdrew consent or were lost to follow-up were included in the analysis with as much follow-up (person-time) as was available until they withdrew or were lost, including any events that occurred prior to their becoming lost or withdrawing from the study. The log-rank test17 was used for the statistical comparison of treatment. Although patients could experience more than one component of the primary and secondary endpoint, each patient was counted only once in the analysis using the time until the occurrence of their first event. All treatment comparisons were performed using two-sided significance tests. Cumulative event rates were calculated according to the Kaplan-Meier method18. Relative risks were expressed as hazard ratios (HR) with associated confidence intervals (CI), and were calculated using the Cox proportional hazards model19. The Cox model was also used to assess the consistency of treatment effects by testing for interactions between treatment and the baseline characteristics pre-specified for subgroup analyses as detailed in the previous section. Continuous variables are expressed as medians and interquartile ranges (IQR) unless otherwise specified. Final statistical analyses were performed using SAS software, versions 8.2 and 9.2 (SAS Institute, Cary NC).
Over the prolonged duration of the trial, the DSMB requested 11 interim analyses of the data. Interim treatment comparisons for the primary endpoint were monitored with the use of two-sided symmetric O’Brien-Fleming-like boundaries generated with the Lan-DeMets alpha spending function approach to group-sequential testing20,21. The monitoring boundaries were based on an overall alpha level of 0.05. Because of the sequential monitoring, the level of significance required for the primary two-sided analysis at the completion of the study was 0.036 (see Supplementary Appendix).
Post hoc sensitivity analyses
The primary treatment comparisons were performed without any imputation of outcomes in the patients for whom we did not have complete follow-up due to consent withdrawal or loss to follow-up. However, to assess the robustness of study findings, sensitivity analyses were performed with imputation of missing outcome data. These analyses incorporated event rate assumptions for withdrawn or lost patients in the placebo group that ranged from 10% to 30%. The differential event rate among withdrawn or lost patients in the chelation group was varied from 10% lower, or slightly favorable to chelation, to 25% higher, or moderately unfavorable to chelation. Using imputed event data among the withdrawn/lost patients combined with the actual follow-up data for all other patients, the treatments were then compared with respect to the primary endpoint. For each different event-rate scenario, multiple replications (500) were performed and the results averaged to obtain the hazard ratio and confidence interval (Supplementary Appendix).
RESULTS
Between September 10, 2003 and October 4, 2010, 1708 patients were randomized, 839 patients to chelation, and 869 patients to placebo. The last infusion was administered September 3, 2011, and the last follow-up visit completed October 31, 2011. The median duration of follow-up was 55 months (IQR 26,60) overall. Active treatment patients were followed 56 (28, 60) months, and placebo patients were followed 53 (24, 60) months. The median time (IQR) from randomization to first infusion was 8 days (6, 12) overall [8 (6, 12) in the chelation group, and 7 (6, 12) in the placebo group].
Baseline characteristics
Baseline characteristics were similar between treatment groups (Table 1). The median (IQR) age was 65 (59,72) years, 18% were female, 9% minority, and the median BMI was 30 kg/m2. The qualifying myocardial infarction had occurred 4.6 (1.6, 9.2) years prior to enrollment. The study population had a high prevalence of diabetes (31%), of prior coronary revascularizations (83%), and guideline recommended medication use of aspirin (84%), beta-blocker (72%), and statin (73%). Patients had a fasting glucose of 102 mg/dL (92,121), and low-density lipoprotein level of 89 mg/dL (67,115).
Table 1.
Baseline Characteristics Infusion Arms.
| Clinical Characteristics- No. (%) | EDTA Chelation (N= 839) |
Placebo (N= 869) |
|---|---|---|
| Age-years | 65 (59, 72) | 66 (59, 72) |
| Female | 152 (18) | 147 (17) |
| Caucasian | 790 (94) | 815 (94) |
| Hispanic | 22 (3) | 29 (3) |
| Black or African American | 29 (3) | 31 (4) |
| Asian | 10 (1) | 18 (2) |
| American Indian/ Alaska Native | 11 (1) | 6 (1) |
| Native Hawaiian or Other Pacific Islander | 3 (0.4) | 3 (0.3) |
| BMI (kg/m2) | 30 (27, 34) | 30 (27, 34) |
| Blood Pressure (mmHg) | ||
| Systolic | 130 (120, 140) | 130 (120, 140) |
| Diastolic | 76 (70, 80) | 76 (70, 80) |
| History- No. (%) | ||
| Hypercholesterolemia | 676 (82) | 694 (81) |
| Hypertension | 568 (68) | 601 (69) |
| Former cigarette smoker | 467 (56) | 488 (56) |
| Angina pectoris | 461 (55) | 465 (54) |
| Anterior MI | 337 (40) | 337 (39) |
| Diabetes | 265 (32) | 273 (31) |
| Congestive heart failure | 154 (18) | 153 (18) |
| Peripheral vascular disease | 126 (15) | 142 (16) |
| Valvular heart disease | 92 (11) | 83 (10) |
| Atrial fibrillation | 85 (10) | 110 (13) |
| Stroke | 57 (7) | 54 (6) |
| Time from qualifying MI to randomization-years | 4.3 (1.8, 9.1) | 4.8 (1.5, 9.5) |
| Current NYHA heart failure class- No. (%) | ||
| No heart failure or Class I | 764 (91) | 795 (91) |
| Class II | 63 (8) | 59 (7) |
| Class III | 12 (1) | 15 (2) |
| Class IV | 0 | 0 |
| Coronary revascularizations- No. (%) | ||
| Either CABG or PCI | 694 (83) | 720 (83) |
| PCI | 491 (59) | 516 (59) |
| CABG | 384 (46) | 390 (45) |
| Concomitant Medications- No. (%) | ||
| Aspirin, warfarin or clopidogrel | 768 (92) | 784 (90) |
| Aspirin* | 717 (85) | 710 (82) |
| Beta-blocker | 611 (73) | 615 (71) |
| Statin | 615 (73) | 633 (73) |
| ACEI or ARB | 525 (63) | 559 (64) |
| Clopidogrel | 212 (26) | 213 (25) |
| Warfarin | 73 (9) | 75 (9) |
| Diabetes medication | ||
| Oral hypoglycemic | 191 (24) | 189 (23) |
| Insulin | 73 (9) | 87 (10) |
| Multivitamin | 356 (44) | 359 (43) |
| Other vitamins/minerals | 428 (52) | 424 (50) |
| Herbal products | 281 (34) | 279 (34) |
| Laboratory Examinations (mg/dL) | ||
| Total cholesterol | 164 (139, 192) | 166 (143, 198) |
| Triglycerides | 135 (94, 199) | 147 (99, 208) |
| Glucose | 103 (92, 121) | 102 (92, 121) |
| LDL | 87 (66, 112) | 90 (68, 117) |
| HDL | 43 (36, 52) | 43 (36, 50) |
| Creatinine* | 1.1 (0.9, 1.2) | 1.1 (0.9, 1.2) |
P<0.05.
There were no other statistically significant differences between groups. Continuous data are reported as median (IQR).
Abbreviations used: ACEI= angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker; HDL = high-density lipoprotein; LDL = low-density lipoprotein.
Treatment compliance
Patients received a total of 55,222 infusions. The median number of infusions received was 40 (30,40); 76% of patients completed at least 30 infusions, and 65% completed all 40 infusions; 30% discontinued study infusions; 5% died or had the study end before infusions could be completed. The most common reason for discontinuation was patient refusal to continue treatment. There were a total of 289 patients (17% of total; 115 in the EDTA group and 174 in the placebo group) who, during the course of the trial, withdrew consent for continued follow-up in the study. A plot of Kaplan-Meier curves depicting the pattern of consent withdrawals in the two randomized arms is presented in Figure A-1 (Appendix). There were an additional 22 patients who were lost to follow-up (13 in the chelation group and 9 in the placebo group). With an average of approximately 3 years of follow-up in these patients, the loss of information was less than the loss among patients who withdrew consent (See online Appendix for additional details and analyses).
Outcome events
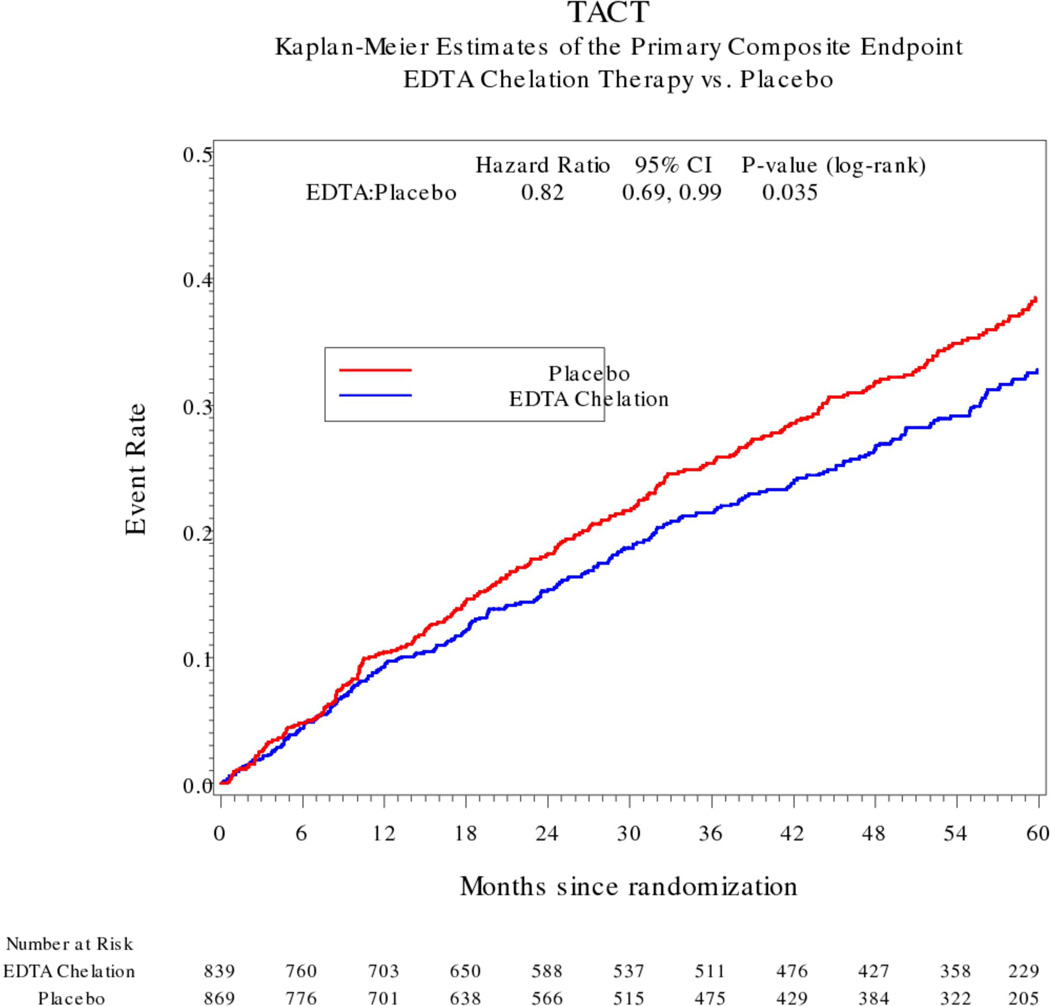
The Kaplan-Meier 5-year estimates for the primary event were 32.8% (95% CI 29.1, 36.5) in the chelation group and 38.5% (95% CI 34.6, 42.3) in the placebo group, (HR 0.82, 95% CI 0.69–0.99, p=0.035, Figure 2). Although treatment comparisons of the components of the primary endpoint were not individually significant, point estimates for the relative treatment effects (HRs 0.72 to 0.81) were larger than that for the primary endpoint for all components except death (HR 0.93) (Table 2). Revascularizations accounted for 45% of primary endpoint events; non-revascularization events accounted for the other 55%. The composite of cardiovascular death, non-fatal MI, or non-fatal stroke occurred in 96 (11%) chelation patients and 113 (13%) placebo patients (HR 0.84, 95% CI 0.64, 1.11, p=0.22).
Figure 2.
TACT Kaplan-Meier Estimates of the Primary Composite Endpoint EDTA Chelation Therapy vs. Placebo
Table 2.
Clinical End Points Infusion Arms.
| EDTA Chelation (N= 839) |
Placebo (N= 869) |
Hazard Ratio (95% CI) |
P Value | |
|---|---|---|---|---|
| Primary Endpoint No. (%) | 222 (26) | 261 (30) | 0.82 (0.69,0.99) | 0.035 |
| Death | 87 (10) | 93 (11) | 0.93 (0.70, 1.25) | 0.642 |
| Myocardial Infarction | 52 (6) | 67 (8) | 0.77 (0.54, 1.11) | 0.168 |
| Stroke | 10 (1) | 13 (1) | 0.77 (0.34, 1.76) | 0.531 |
| Coronary revascularization | 130 (15) | 157 (18) | 0.81 (0.64, 1.02) | 0.076 |
| Hospitalization for angina | 13 (2) | 18 (2) | 0.72 (0.35, 1.47) | 0.359 |
| Secondary Endpoint No. (%) | 96 (11) | 113 (13) | 0.84 (0.64, 1.11) | 0.221 |
| Cardiovascular Death | 50 (6) | 51 (6) | 0.98 (0.67, 1.45) | 0.936 |
The percentages in each case are based on the number of patients experiencing the event at any time during follow-up (not first events) divided by the number of patients randomized.
Primary endpoint = first occurrence of death from any cause, myocardial infarction, stroke, or hospitalization for unstable angina.
Secondary endpoint = first occurrence of death from a cardiovascular cause, myocardial infarction, or stroke.
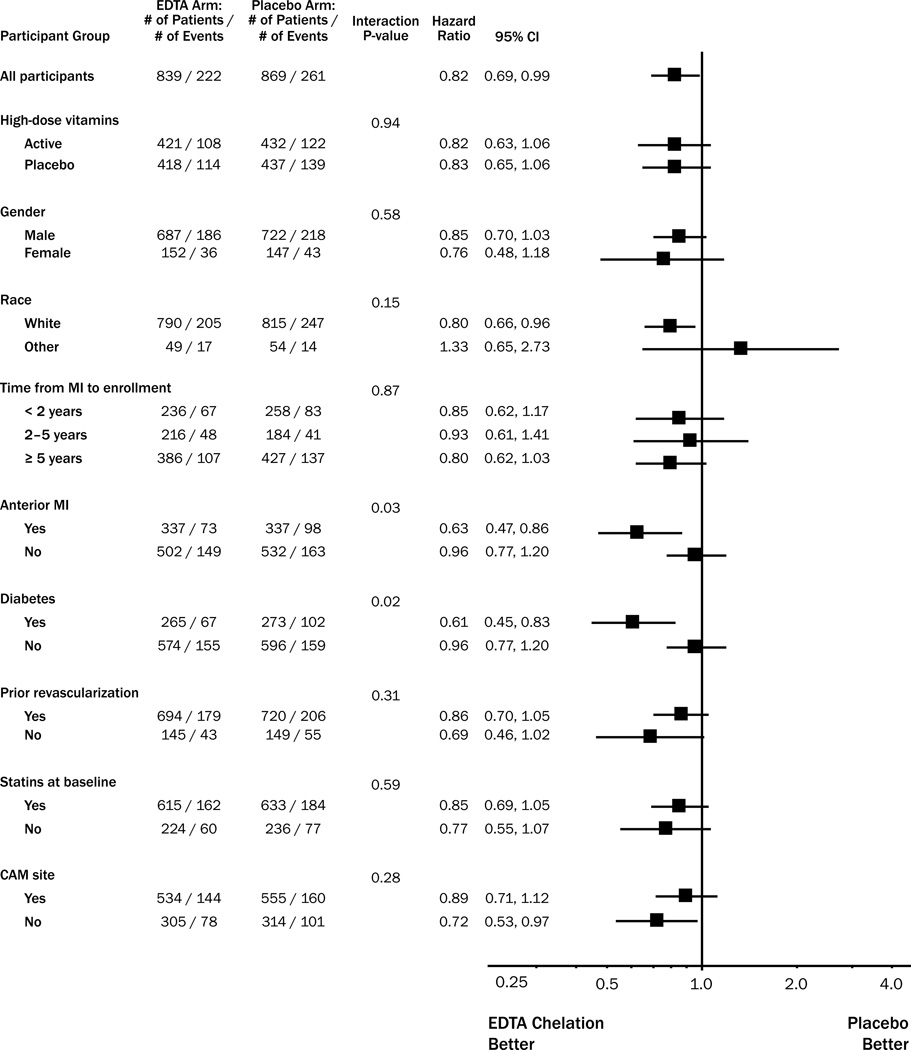
Subgroup analyses
Prespecified tests for treatment by covariate interactions (Figure 3) indicated statistically greater benefit in 2 subgroups: patients with prior anterior MI, and diabetes (Figure 4). There was no significant interaction between treatment and type of enrolling practice (chelation site versus non-chelation, p for interaction 0.28), nor between the high-dose oral vitamins and chelation therapy in the factorial design (p for interaction 0.94).
Figure 3.
Subgroup Analyses Comparing EDTA Chelation to Placebo
Figure 4.
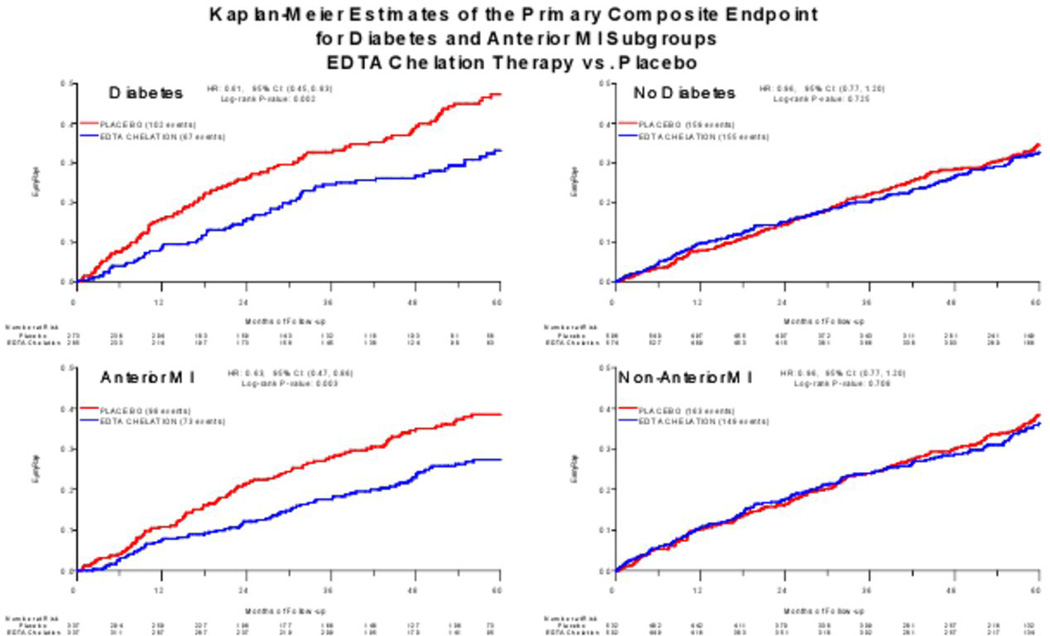
Kaplan-Meier Estimates of the Primary Composite Endpoint for Diabetes and Anterior MI Subgroups EDTA Chelation Therapy vs. Placebo
Adverse effects and safety
Four unexpected severe adverse events occurred that were possibly or definitely attributed to study therapy – 2 in the chelation group (1 death), and 2 in placebo (1 death). Heart failure was reported in 57 (7%) chelation patients, and 71 (8%) placebo patients (p=0.28). There were 330 of 55,222 (0.60%) infusions administered at least 30 minutes too rapidly. Hypocalcemia, defined as calcium < 8.5 mg/dL prior to an infusion, was reported in 52 (6.2%) chelation patients and 30 (3.5%) placebo patients (p=0.008). One patient had hypocalcemia associated with muscle cramping that led to an emergency department visit. (See the online Appendix for a complete listing of adverse events.)
Sensitivity analyses
As a sensitivity analysis, we assessed how the primary treatment comparison would be affected under a variety of assumptions regarding the occurrence of primary endpoint events among the patients who withdrew consent or were lost to follow-up. The comparison of the two groups remained significant at the 0.036 level if the relative increase of events among the withdrawn/lost patients in the active group was as much as 20% higher than in the placebo group, and even generally if the percentage of events among withdrawn/lost patients in the active arm was 25% higher than in the placebo group. The hazard ratio for all of these scenarios remained in the range of 0.80 to 0.84, and the significance of the treatment effect was maintained, not only for the scenarios for the withdrawn or lost patients that would be considered most plausible, but also for scenarios that were unfavorable to EDTA chelation (detailed analyses are in the Supplementary Appendix).
COMMENT
TACT is the first randomized trial, to our knowledge, designed and powered to evaluate the effects of an EDTA-based chelation regimen on clinical outcomes in patients with coronary disease. The trial randomized 1708 patients, administered over 55,000 double-blinded infusions, and accrued over 6200 patient-years of follow-up experience. These data showed that among patients with a prior myocardial infarction, a chelation regimen of 40 infusions of disodium EDTA, ascorbate, B-vitamins, and other components resulted in a modest reduction in a composite outcome of cardiovascular events. The treatment effect persisted over the 5-year follow-up period without evident attenuation. There was no interaction of infusion therapy with the treatment assignment for the oral vitamin regimen. The study was not designed to ascertain mechanism of action nor to identify which of the components of the infusions were responsible for the treatment effect observed.
The effect of EDTA chelation on the non-fatal components of the primary endpoint was quantitatively consistent with its overall effect. The most frequently occurring component was coronary revascularization. We saw no statistically significant treatment effect on all-cause mortality, but the trial had low statistical power for this evaluation. Likewise, the study was underpowered to detect a difference between groups for the secondary endpoint of cardiovascular death, myocardial infarction, or stroke (p=0.22). These results were observed against the background of modern evidence-based post-MI therapy given to the study patients: 83% revascularized with either coronary bypass or percutaneous intervention, 84% on aspirin, 26% on clopidogrel, 72% on beta adrenergic blockers, and 73% on statins, with a median LDL of 89 mg/dL (67,115).
While the relative reduction in cardiovascular events (18%) was smaller than the effect hypothesized in the study design (25%), no prior effectiveness data were available with which to estimate the effect size. A 25% relative reduction in the event rate is included in the 95% CI around the measured treatment effect (HR 0.69 to 0.99). Furthermore, an 18% relative treatment effect is within the range of effects that have been considered clinically important in prior trials, such as the use of clopidogrel for patients with acute coronary syndromes 22.
Two pre-specified subgroups appeared to receive particular benefit of therapy. Patients with diabetes had a reduction in risk (HR 0.61, 95% CI 0.45–0.83), and patients with anterior myocardial infarction, as localized by site investigators, also had a reduction in risk of cardiovascular events (HR 0.63, 95% CI 0.47–0.86). Both of these subgroups were prespecified based on their representing important high-risk subsets of patients but not because there was any specific biologic reason for suspecting that chelation would be uniquely beneficial for these patients. Whether the partitioning of treatment benefit evident in these subgroups will be replicable should be the subject of future investigation. Thus, at present our understanding of the significance of these subgroup findings is incomplete.
TACT is unique from a historical perspective. Chelation therapy with disodium EDTA has been in use to treat atherosclerotic disease for over 50 years 23,24,25,26. By 2007, its use had expanded in the United States to 111,000 adults, exposing this large group of patients to uncertain risks for unproven benefits. The Centers for Disease Control and Prevention have reported deaths from misuse of EDTA chelation. In a June 2008 Federal Register notice, FDA informed the public that edetate disodium was being withdrawn from the market27 Mainstream medical practitioners in general have been highly skeptical that chelation therapy provides any clinical benefit. The most recent ACP/AHA/ACC Guideline for the management of stable ischemic heart disease gives chelation therapy a Class III recommendation (not useful/effective and may be harmful)28. Disodium EDTA remains available through compounding pharmacies. Patients continue seeking out and receiving EDTA chelation therapy, and chelation practitioners continue to recommend it. It is in the context of this half-century controversy that we carried out and now report TACT.
The interpretation of TACT is made more difficult by the absence of supporting research identifying the most plausible mechanism(s) of action. Although TACT was not a mechanistic study, the data obtained do allow some cautious conjectures regarding potential mechanisms meriting future investigation. Two, in particular, can be mentioned. Heavy metal exposure, particularly to lead, has been recognized as a risk for myocardial infarction and stroke29,30. The association of heavy metal pollutants with cardiovascular events extends to antimony, cadmium, cobalt, and tungsten31. The continued separation of the Kaplan-Meier curves for chelation and placebo, long after the infusions stop in year 2, might lend support to a hypothesis that removal of heavy metals has benefit beyond the active infusion phase.
Endothelial dysfunction is generally accepted as a common pathogenic abnormality in patients with atherosclerotic vascular disease. Improvement in endothelial function is a frequent finding with efficacious cardiovascular therapies. Disodium EDTA does not apparently show this effect32. The chelation infusions, however, also contained 7 grams of ascorbate, a vitamin that improves endothelium-dependent vasodilation33,34. Yet clinical trials of oral antioxidant vitamins have been negative35,36. Our use of repetitive intravenous infusions would have led to higher ascorbate blood levels than that of any oral regimen previously studied in cardiovascular clinical trials37. Thus, it is possible that improved endothelial function might account for some of the benefit observed. Oxidative LDL modification facilitated by transition metals is an interesting potential mechanism for the association of atherosclerosis with heavy metals. Transition metals are thought to promote LDL oxidation, while anti-oxidants are thought to retard it38. Thus, a combination of EDTA and ascorbate might lead to a beneficial effect on oxidized LDL.
Study limitations
The necessity of using a composite endpoint as the primary outcome event in a clinical trial creates some unavoidable uncertainties about the actual treatment benefit, since study power is insufficient to show an effect on any individual endpoint and the components are not considered all of equal clinical importance. In TACT, coronary revascularizations were the most frequently observed endpoint events. Revascularization events are considered “softer” due to the necessary element of physician decision-making involved in the event but such events are, nonetheless, commonly used in composite endpoints in cardiovascular trials. In TACT, the revascularization events were verified by staff masked to patient treatment assignment. The consistency of relative treatment effect on all the individual non-fatal components of the primary endpoint provides some reassurance that the observed chelation benefits were not seen only because of some extra-therapeutic effect on revascularization decisions.
There were an unusually high number of patients that withdrew consent, leading to some lost data. On the other hand, all patients had, with appropriate IRB approval to do so, their national death index checked at the end of the study, and some patients withdrew after having sustained a primary endpoint. Post hoc sensitivity analyses with imputations for missing data, included in the Supplementary Appendix, are consistent with our pre-specified analyses. Unblinding is a possible explanation for the observation that placebo patients were more likely to discontinue therapy, withdraw consent or become lost to follow-up than chelation patients. Widespread unblinding of study patients is unlikely, however. There is no evidence from an analysis of side effects that patients perceived a difference between a saline infusion and a chelation infusion. Blinding of coordinators was maintained by the techniques developed to reproduce the viscosity and mask the color of the vitamin C syringes. Finally, there was no heterogeneity in the effect of chelation therapy based on whether a patient was enrolled and followed at a chelation site or a conventional cardiology site. The imputations performed (Supplementary Appendix) support a modest benefit of chelation therapy.
The study was initiated without a well established hypothesis for the mechanism(s) of benefit, and this limits our ability to understand and use the results.
The 40-infusion chelation regimen tested in TACT is not easy for patients to receive (each infusion taking about 3 hours and the first 30 infusions being administered at weekly intervals). Finally, one trial no matter how large or well conducted cannot answer all the questions needed to transform a novel hypothesis into a clinical treatment worthy of guideline endorsement. Moreover, as the first trial of a chelation regimen in this patient population, the possibility that the results represent chance findings must be considered, especially in light of the narrow difference between the significance level calculated and that pre-specified for the analysis. Accordingly, the results of this study should be viewed as an important but single step on the long path towards better understanding the pathophysiologic and therapeutic implications of chelation therapy, but do not provide evidence to support its routine use in clinical practice.
Conclusions
In stable patients with a history of MI, the use of an intravenous chelation regimen with disodium EDTA, compared with placebo, modestly reduced the risk of a composite of adverse cardiovascular outcomes, many of which were revascularization procedures. These results provide evidence to guide further research but are not, by themselves, sufficient to support the routine use of chelation therapy for treatment of post-MI patients.
Supplementary Material
Acknowledgements
The authors gratefully acknowledge the scientific contributions and support of Yves Rosenberg MD, and Mario Stylianou PhD, both of NHLBI; the organizational skills of Ana Mon MPH Project Leader at the CCC, Alyssa Cotler at NCCAM, Susan Dambrauskas (formerly at NHLBI), and Vivian Thompson at the DCRI for their competent professional assistance, and the Florida Heart Research Institute for supporting the pilot study. The above mentioned contributors received no compensation for their work other than their usual salary. Gervasio A. Lamas MD had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The National Center for Complementary and Alternative Medicine (U01AT001156) and the National Heart, Lung and Blood Institute (U01HL092607) provided sole support for this study. Robin Boineau MD (NHLBI), Richard Nahin PhD (NCCAM), Mario Stylianou PhD (NHLBI), and Yves Rosenberg MD (NHLBI), respectively, were involved, as part of the NIH Cooperative Agreement process, in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. All statistical analyses were performed by Kerry Lee PhD, and Lauren Lindblad MS. Gervasio Lamas MD reports that from 2000 to 2003 he served as a consultant to OmniComm, the electronic data capture company used in the trial. No funds were received, and all ties were severed as of 09/10/2003.
Footnotes
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of NHLBI, NCCAM or the National Institutes of Health.
References
- 1.Bessman SP, Ried H, Rubin M. Treatment of lead encephalopathy with calcium disodium versenate. Med Ann DC. 1952;31:312–314. [PubMed] [Google Scholar]
- 2.Clarke NE, Clarke CN, Mosher RE. The in vivo dissolution of metastatic calcium; an approach to atherosclerosis. Am J Med Sci. 1955;229(2):142–149. doi: 10.1097/00000441-195502000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Clarke NE, Clarke CN, Mosher RE. Treatment of angina pectoris with disodium ethylene diamine tetraacetic acid. Am J Med Sci. 1956;232(6):654–666. doi: 10.1097/00000441-195612000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Casdorph HR. EDTA chelation therapy - efficacy in arteriosclerotic heart disease. J Holistic Med. 1981;3:53. [Google Scholar]
- 5.Grier MT, Meyers DG. So much writing, so little science: A review of 37 years of literature on Edetate Sodium chelation therapy. Ann Pharmacother. 1993;27:1504–1509. doi: 10.1177/106002809302701217. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph CJ, McDonagh EW, Barber RK. A non-surgical approach to obstructive carotid stenosis using EDTA chelation. J Adv Med. 1991;4:157–166. [Google Scholar]
- 7.Cranton EM, editor. A textbook on EDTA chelation therapy. Hampton Roads Publishing. 2001;2:503–539. [Google Scholar]
- 8.Rudolph CJ, McDonagh EW, Barber RK. Effect of EDTA chelation on serum iron. J Adv Med. 1991;4:39–45. [Google Scholar]
- 9.Barnes PM, Bloom B, Nahin RL. Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007. Natl Health Stat Report. 2010;(12):1–24. [PubMed] [Google Scholar]
- 10.Guldager B, Jelnes R, Jorgensen SJ, et al. EDTA treatment of intermittent claudication-a double-blind, placebo-controlled study. J Intern Med. 1992;231(3):261–267. doi: 10.1111/j.1365-2796.1992.tb00533.x. [DOI] [PubMed] [Google Scholar]
- 11.van Rij AM, Solomon C, Packer SG, Hopkins WG. Chelation therapy for intermittent claudication. A double-blind, randomized, controlled trial. Circulation. 1994;90(3):1194–1199. doi: 10.1161/01.cir.90.3.1194. [DOI] [PubMed] [Google Scholar]
- 12.Knudtson ML, Wyse DG, Galbraith PD, et al. Chelation therapy for ischemic heart disease: a randomized controlled trial. J Am Med Assoc. 2002;287(4):481–486. doi: 10.1001/jama.287.4.481. [DOI] [PubMed] [Google Scholar]
- 13.American Heart Association. Questions and answers about chelation therapy. Dallas, TX: AHA; 2000. [Google Scholar]
- 14.U.S. Centers for Disease Control. Morbidity and Mortality Weekly Report (MMWR) [cited 2010 Nov 16];Deaths Associated with Hypocalcemia from Chelation Therapy --- Texas, Pennsylvania, and Oregon, 2003—2005. 2006 55(08):204–207. Updated:3/2/2006; Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5508a3.htm51138.htm. [PubMed] [Google Scholar]
- 15.Lamas GA, Goertz C, Boineau R, et al. Design of the trial to assess chelation therapy (TACT) Am Heart J. 2012;163(1):7–12. doi: 10.1016/j.ahj.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rozema TC. Special issue: protocols for chelation therapy. J Adv Med. 1997;10:5–100. [Google Scholar]
- 17.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. Second Edition. New York: John Wiley & Sons, Inc; 2002. [Google Scholar]
- 18.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Statist Assn. 1958;53:457–481. [Google Scholar]
- 19.Cox DR. Regression models and life-tables (with discussion) J Royal Statist Soc B. 1972;34:187–220. [Google Scholar]
- 20.O'Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549–556. [PubMed] [Google Scholar]
- 21.Lan KKG, DeMets DL. Discrete sequential boundaries for clinical trials. Biometrika. 1983;70:659–663. [Google Scholar]
- 22.Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without STsegment elevation. N Engl J Med. 2001;345(7):494–502. doi: 10.1056/NEJMoa010746. [DOI] [PubMed] [Google Scholar]
- 23.Kitchell JR, Palmon F, Aytan N, Meltzer LE. The treatment of coronary artery disease with disodium EDTA. A reappraisal. Am J Cardiol. 1963;11:501–506. doi: 10.1016/0002-9149(63)90011-0. [DOI] [PubMed] [Google Scholar]
- 24.Lamar CP. Chelation endarterectomy for occlusive atherosclerosis. J Am Geriatr Soc. 1966;14(3):272–294. doi: 10.1111/j.1532-5415.1966.tb05318.x. [DOI] [PubMed] [Google Scholar]
- 25.Casdorph HR, Farr CH. EDTA chelation therapy III: treatment of peripheral arterial occlusion, an alternative to amputation. J Holistic Med. 1983;5:3. [Google Scholar]
- 26.Olszewer E, Carter JP. EDTA chelation therapy in chronic degenerative disease. Med Hypotheses. 1988;27(1):41–49. doi: 10.1016/0306-9877(88)90082-5. [DOI] [PubMed] [Google Scholar]
- 27.Public Health Advisory: edetate disodium (Marketed as endrate and generic products) Available from http://www.fda.gov/OHRMS/DOCKETS/98fr/E8-13273.htm.
- 28.Qaseen A, Fihn SD, Dallas P, et al. Management of patients with stable ischemic heart disease: Executive summary of a clinical practice guideline from the American College of Physicians, American College of Cardiology Foundation/American Heart Association/American Association for Thoracic Surgery/Preventive Cardiovascular Nurses Association/Society of Thoracic Surgeons. Ann Intern Med. 2012 doi: 10.7326/0003-4819-157-10-201211200-00011. available at: http://annals.org. [DOI] [PubMed] [Google Scholar]
- 29.Menke A, Muntner P, Batuman VV, Silbergeld EK, Guallar E. Blood lead below 0.48 micromol/L (10 microg/dL) and mortality among US adults. Circulation. 2006;114(13):1388–1394. doi: 10.1161/CIRCULATIONAHA.106.628321. [DOI] [PubMed] [Google Scholar]
- 30.Weisskopf MG, Jain N, Nie H, et al. A prospective study of bone lead concentration and death from all causes, cardiovascular diseases, and cancer in the department of veterans affairs normative aging study. Circulation. 2009;120(12):1056–1064. doi: 10.1161/CIRCULATIONAHA.108.827121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agarwal S, Zaman T, Tuzcu EM, Kapadia SR. Heavy metals and cardiovascular disease: Results from the national health and nutrition examination survey (NHANES) 1999–2006. Angiology. 2011;62(5):422–429. doi: 10.1177/0003319710395562. [DOI] [PubMed] [Google Scholar]
- 32.Anderson TJ, Hubacek J, Wyse DG, Knudtson ML. Effect of chelation therapy on endothelial function in patients with coronary artery disease: PATCH substudy. J Am Coll Cardiol. 2003;41(3):420–425. doi: 10.1016/s0735-1097(02)02770-5. [DOI] [PubMed] [Google Scholar]
- 33.Plantinga Y, Ghiadoni L, Magagna A, et al. Supplementation with vitamins C and E improves arterial stiffness and endothelial function in essential hypertensive patients. American journal of hypertension. 2007;20(4):392–397. doi: 10.1016/j.amjhyper.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 34.Levine GN, Frei B, Koulouris SN, Gerhard MD, Keaney JF, Jr, Vita JA. Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996 Mar 15;93(6):1107–1113. doi: 10.1161/01.cir.93.6.1107. [DOI] [PubMed] [Google Scholar]
- 35.Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: Systematic review and meta-analysis. J Am Med Assoc. 2007;297(8):842–857. doi: 10.1001/jama.297.8.842. [DOI] [PubMed] [Google Scholar]
- 36.Sesso HD, Christen WG, Bubes V, et al. Multivitamins in the prevention of cardiovascular disease in men: the Physicians' Health Study II randomized controlled trial. JAMA. 2012 Nov 7;308(17):1751–1760. doi: 10.1001/jama.2012.14805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Padayatty SJ, Sun H, Wang Y, et al. Vitamin C pharmacokinetics: Implications for oral and intravenous use. Ann Intern Med. 2004;140(7):533–537. doi: 10.7326/0003-4819-140-7-200404060-00010. [DOI] [PubMed] [Google Scholar]
- 38.Yoshida H, Kisugi R. Mechanisms of LDL oxidation. Clinica Chimica Acta. 411(2010):1875–1882. doi: 10.1016/j.cca.2010.08.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.