Abstract
Although post-mortem MRI (PMMR) was proposed as an alternative to conventional autopsy more than a decade ago, the lack of systematic validation has limited its clinical uptake. Minimally invasive autopsy (MIA) using PMMR together with ancillary investigations has now been shown to be as accurate as conventional autopsy in foetuses, newborns and infants and is particularly useful for cerebral, cardiac and genitourinary imaging. Unlike conventional autopsy, PMMR provides a permanent three-dimensional auditable record, with accurate estimation of internal organ volumes. MIA is becoming highly acceptable to parents and professionals, and there is widespread political support and public interest in its clinical implementation in the UK. In the short to medium term, it is desirable that a supraregional network of specialist centres should be established to provide this service within the current National Health Service framework.
The value of paediatric and perinatal autopsy in confirming or refuting ante-mortem diagnosis, advancing medical science and providing accurate epidemiological data about disease prevalence is undisputed. A number of studies have shown that clinically important information is obtained from autopsy in the majority of hospital deaths, and such information may have prevented death in around 10% of cases, if it had been available.1–3 However, these proportions have been largely unchanged over several decades, and there remains widespread variation in clinical practice, with judgements made regarding which cases do and do not need a full autopsy often depending on an individual pathologist's or coroner's preference.
Advances in early antenatal diagnosis and screening programmes have resulted in an increase in the number of terminations of pregnancies in the past decade, and improvements in antenatal ultrasound imaging mean that there is now complete agreement between prenatal ultrasound and autopsy findings in >80% of cases.4 However, in up to one-quarter of cases, additional information which changes the underlying diagnosis or the information given to parents during counselling may be acquired from a formal autopsy.5–9 This figure may be higher in paediatric rather than perinatal cases.1 Several studies have also shown a significant discrepancy rate between what clinicians think is the cause of death and full traditional autopsy findings,3,10 and error rates can be as high as 50% on medical certificates in stillbirths.11
The clinical information gained from performing a full post-mortem examination forms the basis of National Health Service autopsy service provision following foetal and childhood deaths in the UK, and despite its inherent limitations is the key part in developing appropriate preventative measures.12
Declining autopsy rates
Autopsy rates in the UK and across mainland Europe13 have been declining for the past decade. The UK national data show that only 44% of stillbirths, 38% of perinatal deaths and 25% of neonatal deaths result in an autopsy being performed.12 This is well below the UK Royal Colleges' recommendations of 75% and means that a large amount of information that could be used to counsel parents about future pregnancies and contribute to epidemiological studies regarding infantile deaths is currently missing. Consented (non-forensic) paediatric autopsies are virtually non-existent.14
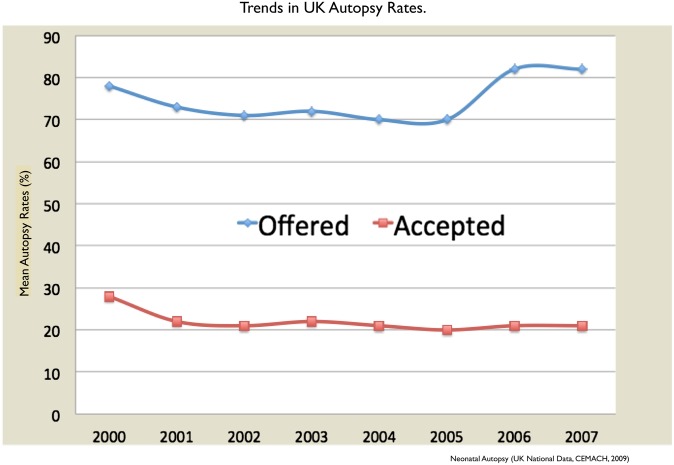
This decline cannot be attributed to clinicians failing to offer autopsies to parents, as the number of clinicians offering autopsies has increased in recent years from 89% to 97% in stillbirths and from 77% to 87% in neonatal deaths.12 Therefore, the current low autopsy rate is primarily due to parental refusal (Figure 1).
Figure 1.
Changes in the neonatal autopsy rate (line with diamonds) and proportion of cases in which autopsy was offered to parents (line with squares) between 2000 and 2007 in the UK (adapted from the CEMACH data12).
This reluctance to consent for a conventional invasive autopsy is multifactorial, including religious reasons, fear of disfigurement (especially towards opening the head), the time an autopsy takes, which may delay burial or funeral plans, and not wanting to put a baby or child through any more tests when it may not provide additional information.15
EARLY PAEDIATRIC STUDIES USING POST-MORTEM IMAGING
For almost two decades, the concept of using post-mortem MRI (PMMR) as an alternative to conventional autopsy has been under discussion. One of the earliest reports of whole-body MRI as an alternative to conventional autopsy was in 1996. This study found that, in 60% of cases, MRI had equivalent or better diagnostic sensitivity than conventional autopsy, but included only 20 patients. Since then, many other similar small-scale studies16–21 have shown the potential of PMMR, particularly for the central nervous system (CNS) (Table 1). Brain and spinal cord anomalies account for 20% of fatal congenital abnormalities in foetuses, and PMMR has a high sensitivity and specificity for detecting these abnormalities in foetuses.19,32 Several studies have also recently demonstrated that PMMR can be used to perform non-diagnostic tasks usually performed during autopsy, such as organ weight and volume estimation,28,29,33 thus suggesting that it may be a suitable alternative to autopsy in some cases. Whole-body imaging and specific imaging in other body systems have not been fully evaluated until recently.23
Table 1.
Studies on post-mortem MRI (PMMR) in foetuses and infants
| Study | Design | MR sequence | N | Organs examined | Results |
|---|---|---|---|---|---|
| Brookes et al16 | Prospective | 1.5-T, 2D T2W, saline bags and small coils used to improve signal | 20 | Whole body | Comparable accuracy only in 12 cases, although good correlation for brain lesions. MRI missed bladder abnormality, periaqueductal bleed, pulmonary hyperplasia. Poor accuracy for cardiac lesions |
| Alderliesten et al22 | Prospective | 2D T1W in 16, 2D T2W in 10 | 26 | Whole body | 8 of 18 major malformations were missed by PMMR. Poor accuracy for cardiac lesions |
| Woodward et al21 | Prospective | 3D T2W with 3-mm slice thickness | 26 | Whole body | 37 of 47 major malformations detected by MRI. Accuracy better for CNS abnormalities and poor for cardiac lesions |
| Breeze et al23 | Prospective | 2D T2W | 30 | Whole body | High sensitivity (87%) for detection of brain lesions, but poor for heart (25%) and lungs (62%) |
| Griffiths et al19 | Prospective | 1.5-T, 2D T2W | 32 | Brain and spine | MR 100% sensitivity for detection of CNS lesions. How the gold standard was PMMR, rather than autopsy, in some of these foetuses |
| Hagmann et al24 | Unclear | 1.5-T, 2D T2W | 37 | Kidneys | PMMR detected all five cases that had a structural renal abnormality. Blinding of radiologists and pathologist unclear |
| Widjaja et al25 | Unclear | 1.5-T, 2D T2W | 41 | Spine | 10 cases with a spinal abnormality noted on prenatal USS and 31 foetuses without abnormality included. Post-mortem MR detected abnormality in all cases. Selected cases and blinding of radiologists and pathologist unclear |
| Huisman et al26 | Prospective | 1.5-T, 2D T1/T2W | 10 | Whole body | PMMR detected all abnormalities noted at autopsy. Blinding of radiologists and pathologist unclear. Small number of likely preselected cases |
| Cohen et al27 | Retrospective | 1.5-T, 2D T2W | 100 | Brain | Retrospective review with inclusion of previous cases. 60% agreement between MR and autopsy findings |
| Thayyil et al28 | Prospective | 9.4-T, 1.5-T, 3D T2W | 18 | Whole body | High-field MRI gives good tissue characterization in small foetuses less than 22 weeks old |
| Breeze et al17 | Prospective | 2D T2W | 44 | Whole body | MIA done, including MRI and percutaneous organ biopsies. MIA provided information of at least equivalent clinical significance for 72.7% of cases |
| Sebire et al20 | Prospective | 1.5-T, T1/T2W | 10 | Whole body | MIA done, including MRI and percutaneous organ biopsies. Good concordance with autopsy results |
| Cannie et al18 | Prospective | 1.5-T, 2D T1/T2W | 96 | Whole body | Virtopsy is reliable for most structures except heart and urogenitals, can be confidently used in the second half of pregnancy to determine normality or abnormality |
| Votino et al29 | Prospective | 9.4-T, 3.0-T, 1.5-T 2D and 3D T2W | 24 | Heart | High-field MRI gave good visualization of the heart irrespective of gestational age (4-T MRI could identify 7 of 8 cases of major congenital heart disease) |
| Sandaite et al30 | Retrospective | 3-T, 3D T2W | 39 | Heart | Normal cardiac structures visualized for foetuses beyond 14 weeks of gestation |
| Thayyil et al31 | Prospective | 1.5-T, T1/T2W | 400 | Whole body | 89.3% concordant with conventional autopsy. Better in foetuses and newborns and infants. Less accurate in children |
2D, two-dimensional; 3D, three-dimensional; CNS, central nervous system; MIA, minimally invasive autopsy; T1W, T1 weighted; T2W, T2 weighted; USS, ultrasounds scan.
Table adapted with permission from Elsevier.3
Paediatric PMMR clearly showed promise but needed a thorough evaluation. A systematic review in 2010 of all PMMR studies demonstrated that there was still inadequate evidence at that time to validate the use of PMMR as an alternative to conventional autopsy.34 The Chief Medical Officer, the UK government's senior advisor on health, recommended that a systematic evaluation of PMMR as an alternative to conventional autopsy in adults and children be completed for the UK.
MINIMALLY INVASIVE AUTOPSY
The conventional autopsy is considered the gold standard, and involves invasive components such as in situ, macroscopic and histological assessments of the brain and the internal organs and non-invasive ancillary assessments, including full clinical history, ante-mortem diagnostic studies, post-mortem plain-film radiography, external examination of the body, placental histopathological examination for foetuses, and laboratory tests, including genetic, metabolic and microbiological studies. The term minimally invasive autopsy (MIA) has now been developed to describe a range of less invasive ways of obtaining post-mortem information without open dissection of the body. Together with the ancillary assessments described, this may give sufficient information for a diagnosis to be made, without having to perform a full autopsy. Typically, MIA involves sampling tissues by either needle biopsy through the skin (percutaneous approach) or keyhole techniques using endoscopy,20 which may involve image guidance, to acquire adequate tissue for histology but simultaneously minimizing the disfigurement of the body, which will be discussed later in this review.
Cross-sectional imaging techniques that can help include CT, MRI and ultrasound. One term given to encompass the use of any imaging technique is the virtual autopsy or virtopsy.35 Exact descriptions of the type of procedure on offer are important to understand the full diagnostic potential of tests, and whether each technique has been validated in a particular setting.
Minimally invasive autopsy: adjunct or alternative?
Another area that may require clarification is whether a procedure is being offered as an alternative, or adjunct, to conventional autopsy. To be a useful adjunct, imaging should be able to detect abnormalities that are difficult to identify or might be missed during a conventional autopsy. For example, post-mortem brain MRI as a routine adjunct to perinatal autopsy may provide important information, especially when the foetal brain is autolysed. Imaging techniques are already being used clinically as part of a full post-mortem in many hospitals, but validating MRI as an alternative to conventional autopsy has only recently been investigated.31
The MRI autopsy study
The MRI Autopsy Study (MaRIAS) was the first large prospective study to evaluate the clinical usefulness of PMMR as an alternative to full conventional autopsy in foetuses and children. A total of 400 unselected cases were analysed, which included 277 (69%) foetuses and 123 (31%) children younger than 16 years.36 All cases had a post-mortem whole body 1.5-T MRI completed before full conventional autopsy. MRI findings alone, and MRI findings in conjunction with ancillary assessments (termed MIA), were compared with conventional autopsy findings, the diagnostic gold standard, for accuracy of detecting cause of death or major pathological abnormalities. For the purposes of this study, MIA is defined as post-mortem investigations with no incisions or dissections but with post-mortem blood sampling via needle puncture and other non-invasive ancillary investigations as described in detail above. This definition of MIA was chosen because the parental objections may be related to the invasive components of autopsy, i.e. open dissection and internal examination of visceral organs. Although a number of parents may also refuse percutaneous or endoscopic tissue sampling, parents are less likely to object to external examinations, blood tests and placental assessment.
The MaRIAS had three major conclusions for paediatric post-mortem (PM) imaging. First, that MIA (MRI + ancillary tests) had a high concordance for identifying the same cause of death and/or major pathological lesion as full invasive autopsy (357/400; 89.3%) across the paediatric group. This was highest in foetal cases (n = 263/277; 94.9%) but concordance reduced with increasing age. Concordance between MIA and autopsy was better for younger children aged less than 1 month (34/42; 81%) and 1–12 months (45/53; 84.9%) than for those aged over 1 year (15/28; 53.6%).31 This gave an overall concordance rate in children of 76.4% (94/123), mainly as a result of undetected myocarditis or pneumonia, or systemic sepsis.
Second, could an autopsy have been replaced by MIA in any of the cases studied? The combination of an experienced pathologist and radiologist who reviewed MIA findings blinded to the autopsy findings, using a pre-defined flow chart, suggested that, in 41% (165/400) of all cases, the cause of death or major pathological lesion was accurately identified without the need for full autopsy. Within this subgroup concordance with full autopsy was 99.4%, with one apparent false-positive brain lesion being the only discordance. This suggests that in almost half (41%) of the cases referred for conventional autopsy, MIA could be performed instead of a full autopsy without missing significant lesions that contribute to the cause of death.
Third, was PMMR alone sufficient to give a cause of death or diagnosis in most cases, i.e. replace autopsy in its entirety? In this study, the accuracy of MRI alone, without ancillary post-mortem investigations, was average at 55.5% (222/400) concordance. This lower concordance with conventional autopsy was mainly because of undetected abnormalities in the placenta for foetuses and poor accuracy in detecting infection, most commonly lung infection, in children. We conclude that PMMR in isolation is not yet able to provide a reliable alternative to autopsy, and more work needs to be done if this is to be proposed as a working model in the future.31
The data from the MaRIAS emphasized that PMMR was most accurate in detecting cerebral (Figure 2), cardiac and renal abnormalities. When MRI was used as part of an MIA, in 65% (258/400) of cases opening the head for formal brain autopsy was unnecessary. The formal neuropathological examination provided clinically important new information for only 2 (0.7%) of these cases when MRI was normal. On the other hand, in 30% (13/43) of cases (small foetuses) in which neuropathology was inconclusive as a result of autolysis, MRI was able to detect clinically important lesions. This suggests not only that PMMR of brain and spinal cord should be routinely performed in all foetuses for obtaining optimal post-mortem information31 but also that opening the skull when PMMR was normal did not yield significant additional pathological information contributing to the cause of death
Figure 2.
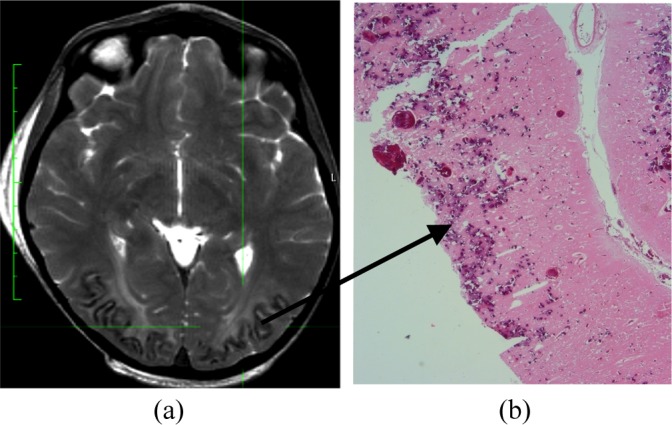
Post-mortem MRI (axial T2 weighted sequence) of a four-year-old child with leukoencephalopathy, showing capillary haemangioma in the occipital region (arrow) with underlying white matter disease (a). Histology (haematoxylin and eosin stain) showing the capillary haemangioma (b).
POST-MORTEM MRI SEQUENCES AND ARTEFACTS
Most studies to date have used standard clinical MR sequences for PM imaging. T1 weighted images have poor contrast, and high-resolution T2 weighted sequences offer much better contrast for PMMR. A multitude of factors, including post-mortem interval, maceration (increase in T1 and T2) and lower body temperature (reduction in T1 and T2) may affect the T1 and T2 values, and hence the image contrast.37,38 Thus, sequences specifically optimized for PMMR and body temperature may offer better image contrast.
Systematic studies exploring various PMMR artefacts38 in foetuses and children are lacking. Intracardiac gas is a common finding in foetuses terminated by foeticide using intracardiac injection. There are limited reports of more widespread intravascular gas occurring in children, and may occur following trauma or resuscitation,39 although the true significance of post-mortem gas remains unknown. In our experience, widespread PM gas is rarely seen in foetuses and children, in the absence of resuscitation and when imaged prior to significant body decomposition.
TISSUE SAMPLING TECHNIQUES
It is clear that, even in the best hands, imaging will still require histological assessment of tissue to confirm or refute proposed diagnoses. This is particularly evident in infants and children, and less so in foetuses. The MaRIAS data showed that, in infants and children, pneumonias and myocarditis were missed using PMMR alone. To perpetuate the ideal minimally invasive PM approach, needle or endoscopic tissue sampling approaches also need to be assessed in this paediatric context.
PM needle biopsies have been used since the 1950s as a less invasive alternative. There have been two good quality prospective studies performed on foetuses and infants in the past 5 years. The first study was of 30 neonatal cases that found adequate biopsy tissue was collected in 86% of lung and 76% of liver biopsies but in under 50% for other organs.40 However, none of the histological abnormalities found during conventional autopsy were identified in the needle biopsy samples, i.e. the samples appeared to be adequate by volume but were non-diagnostic.40 The second included 25 newborn infants and reported adequate tissue volumes collected for liver, lungs and brain biopsy in 92%, 84% and 68% of cases, respectively, but only 56%, 24% and 20% for right kidney, left kidney and spleen.41 Final diagnosis could be made from the needle biopsy samples in 68% of cases with 56% full concordance with conventional autopsy.41 Needle biopsy appears to be more accurate in neonates than foetuses, but complications such as the small size of foetuses, neonates and infants and the added complication of maceration in foetuses makes accurate blinded needle biopsy sampling difficult and not suited for post-mortem investigations in this population.
Image guidance could improve these sampling detection rates, and ultrasound image guidance has been used in older children and adults, with “adequate biopsy” sample rates approaching 100% for liver, spleen, lungs and brain, and high concordance (83%) with conventional autopsy findings.42 CT- and MRI-guided biopsies could also be used to increase the accuracy of biopsy samples but need very specialized training and equipment. As yet, paediatric PM image-guided needle biopsy adequacy remains to be established.
Alternatively, endoscopic sampling may offer the solution to obtaining reliable tissue samples without the need for large incisions. Studies in adults have shown that endoscopic diagnosis was 94.4% accurate when compared with conventional autopsy findings.43 Initial studies in foetuses and neonates have found that this technique provides good visualization of most internal anatomy and adequate tissue for histological examination even in small foetuses. In one study, clinically significant information was gained by endoscopy examination and histological examination in 70% of cases, compared with PMMR alone.20 The other advantages of endoscopy are improved visualization owing to illumination and magnification, a visual record of the procedure and, most importantly, no large incisions. The combination of image-guided needle sampling and endoscopic evaluation, where appropriate, is likely to provide the best autopsy combination of accurate tissue diagnosis with maximal parental acceptance.
VISCERAL ORGAN VOLUME ESTIMATION AND RAPID PROTOTYPING
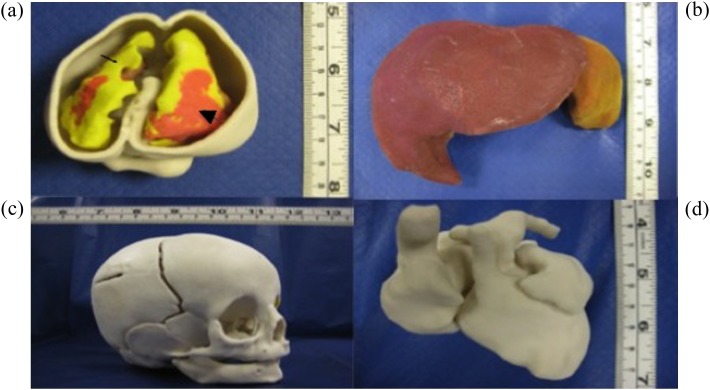
Estimation of internal organ volumes is an integral part of autopsy, and it is important to show that equivalent data can be provided by non-invasive imaging methods (Figure 3). Several studies have demonstrated that PMMR can be used to perform non-diagnostic tasks usually performed during autopsy, such as organ weight and volume estimation.28,29,33 However, several of the techniques involved used manual segmentations and semi-automated technique,29 which can be time consuming and requires specialist image analysis expertise. Automated segmentation systems may improve the speed and generalizability of these techniques in future. Rapid prototyping of the visceral organs may be useful in understanding complex pathologies and explaining these to parents and to the jury in forensic cases (Figure 3).
Figure 3.
Rapid prototyping of foetal and neonatal organs from post-mortem MRI data. (a) Foetal brain inside the skull. Cerebrospinal fluid is shown in white with black arrow and intraventricular bleed in grey with black arrowhead. (b) Liver of a newborn. (c) Parietal skull fracture in an infant. (d) Foetal heart.
PAEDIATRIC AND PERINATAL POST-MORTEM CT
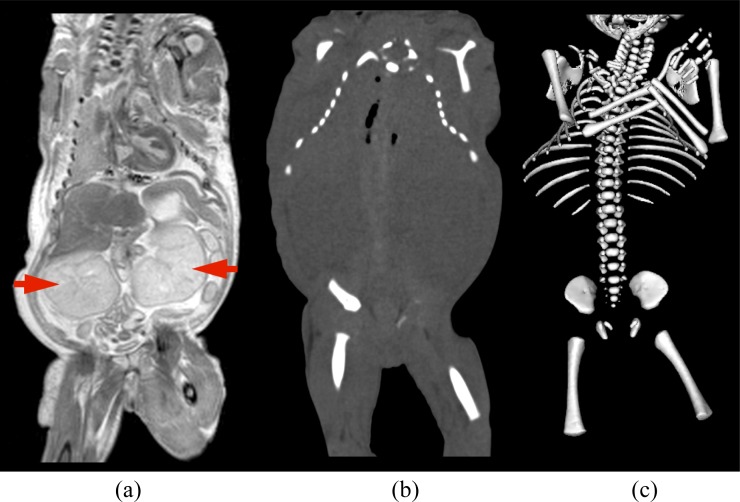
The main advantage of post-mortem CT (PMCT) scanning is that it is considerably cheaper and faster than MRI. However, the soft-tissue contrast of CT is considerably inferior to MRI in foetuses and children (Figure 4), and there is little evidence to use CT as an alternative for autopsy in foetuses and children. This may be because of the reduced perivisceral fat in foetuses and newborns, when compared with older children and adults. Several studies in adults show that CT has better diagnostic performance than MRI in providing an overall cause of death,44 and CT angiography is rapidly becoming the PM imaging technique of choice in adults.45 This is largely because the common causes of adult death, such as ischaemic heart disease and vascular insults, account for its significant proportion, and it is particularly useful to demonstrate the bone and soft-tissue effects of high-impact trauma or gunshot wounds. In children, PMCT is gaining acceptability in forensic imaging, where detailed imaging of suspicious bone injuries is required, typically in cases of suspected non-accidental or inflicted injury, but non-contrast-enhanced CT in children is known to be of limited diagnostic value for both CNS and other body pathology. Non-contrast CT in foetuses is likely to be of limited value, except in certain specific diagnostic cases, such as in rare skeletal dysplasias, as has been suggested from a recent small study of 14 foetuses.46 Nevertheless, CT may be useful in demonstrating skeletal injuries and abnormalities, particularly in forensic cases.
Figure 4.
Comparison of post-mortem MRI (a) and post-mortem CT (b) of a 27-week-old foetus with renal dysplasia (arrows). Visceral organs are not clearly seen on post-mortem CT, whilst the bony skeleton is clearly displayed on reconstruction of the CT image (c).
PROFESSIONAL AND PARENTAL ATTITUDE CHANGES TOWARDS MINIMALLY INVASIVE AUTOPSY
An important factor to consider when discussing the effectiveness of PMMR as a clinical tool is the attitude of those most closely involved. Healthcare professionals have to carefully explain these procedures to gain informed consent from bereaved parents, which is no easy task. Their attitude towards autopsy will influence if and how they approach and inform parents about autopsy and are therefore extremely important. A recent study examined the acceptability of minimally invasive perinatal/paediatric autopsy to healthcare professionals.47 This study found that, regardless of ethnicity or religion, there was a general agreement across all professionals involved that autopsy was important in providing additional information for future pregnancies and medical research, with MIA being significantly more acceptable across a range of ethnic and religious groups than traditional autopsy.47 Professionals also strongly agreed that having the option of MIA would make discussing autopsy options easier with parents and that it would be useful for parents to be able to meet with a doctor or pathologist to discuss the post-mortem procedure.47 One of the major issues with the post-mortem consent process highlighted by this research is that a very low number of professionals had formal training in autopsy consent. Many agreed that having additional educational material or even witnessing an autopsy themselves would be beneficial.47
However, parental attitude towards autopsy is the most important factor in determining whether a post-mortem examination will take place. A recent study involving almost 100 parents investigated parental attitudes to less invasive autopsy involving PM imaging only. PM imaging was considered acceptable by 99% of the parents involved, including the 33% of parents who did not consent to conventional autopsy, and religious groups for whom conventional autopsy was not acceptable.18
We examined parental attitudes towards MIA in a qualitative study funded by the Lullaby Trust, London, UK. Most parents reported that the fact that the head would not be cut open was an important factor in choosing MIA over conventional autopsy or no autopsy. All parents stated that they had a clear understanding of the general procedure of MIA when explained to them at the time of consent, but there was a lack of detailed information provided. Some parents felt that staff did not know much about the procedure and most felt that the final results were explained inadequately. Many parents still were not clear about the outcomes of the MIA and the tests exactly done, and some parents felt they did not get the chance to discuss the outcomes and whether the reason for the death had been explained or confirmed by the MIA. The length of time between death and the results of the MIA, when parents received little or no support, also caused unnecessary distress. However, even with these initial issues, the participants interviewed were still comfortable with their decision to choose MIA over full autopsy or no autopsy.
A systematic approach will be required to make sure that adequate training and information on MIA techniques is available for professionals and the full process is fully understood by all parties involved in the post-mortem process.
IMPLEMENTATION
The ability to accurately interpret paediatric and perinatal PM imaging is highly specialized and requires a specific skill set that needs to be acquired by most future practitioners. An in-depth knowledge of anatomy, foetal and childhood syndromes and pathology, imaging physics training and an awareness of normal PM imaging findings and specific knowledge of perinatal tissue sampling and autopsy techniques will all be required to maximize the yield from each post-mortem case. As these skills currently lie in the domains of paediatricians, pathologists, radiologists and foetal medicine specialists, it is likely that close collaboration between these specializations will be required to manage the cases effectively, with a pathologist in a central co-ordinating role. The importance of acquiring appropriate imaging and obtaining expert radiological opinion is already a part of the UK perinatal pathology training curriculum, but a separate unique training programme for pathologists and paediatric radiologists may be required in the future, together with funded programmes to validate training and develop the appropriate clinical standards.
In terms of service delivery, it is likely that PMMR will be performed within already established centres of specialist perinatal pathology, by those with dedicated specialist imaging skills.43 Establishing a paediatric PM service will require an ethically sensitive and medicolegally robust framework, which may vary with different institutions and countries.
One inherent limitation of the MaRIAS was that it was performed in a specialist environment, in ideal scanning and image interpretation conditions, with skilled perinatal pathologists and highly experienced specialist paediatric radiologists. Whilst this may not be reproducible in other centres without specialist expertise, it may not be necessary to try to do so. Centralized reporting of locally acquired images is one solution to this, but centralizing the whole service is more likely to be cost-effective.
However, the overall cost of PM imaging is a more difficult question to address, as offering the service is likely to yield a large increase in uptake of overall post-mortem examinations. This would initially increase the workload for both radiology and pathology departments, but should allow a more cost-effective overall PM service to develop. Several issues, including cost of imaging, geographical location, staff availability and ultimately large-scale parental demand, will need to be addressed in a formal cost-effectiveness evaluation prior to service implementation.
CONCLUSION
After almost two decades, PMMR, when used as part of an MIA, has been validated as an alternative to conventional autopsy for foetuses and infants. In foetuses, PMMR, non-invasive ancillary tests and blood tests would be sufficient in most cases. In infants and children, this approach would also be acceptable except in cases where pneumonia and myocarditis are present, for which tissue sampling may be needed for accurate diagnosis. Successful implementation of MIA into routine clinical practice still has a long way to go with many issues to consider to ensure that the best possible service is provided. However, validation of MIA has provided a more acceptable option for foetal and neonatal post-mortem examination and will hopefully lead to an increase in post-mortem consent and to better understanding of disease in this population.
REFERENCES
- 1.Stambouly JJ, Kahn E, Boxer RA. Correlation between clinical diagnoses and autopsy findings in critically ill children. Pediatrics 1993; 92: 248–51. [PubMed] [Google Scholar]
- 2.Cardoso MP, Bourguignon DC, Gomes MM, Saldiva PH, Pereira CR, Troster EJ. Comparison between clinical diagnoses and autopsy findings in a pediatric intensive care unit in Sao Paulo, Brazil. Pediatr Crit Care Med 2006; 7: 423–7. doi: 10.1097/01.PCC.0000235257.86519.16 [DOI] [PubMed] [Google Scholar]
- 3.Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 2003; 289: 2849–56. doi: 10.1001/jama.289.21.2849 [DOI] [PubMed] [Google Scholar]
- 4.Vogt C, Blaas HG, Salvesen KA, Eik-Nes SH. Comparison between prenatal ultrasound and postmortem findings in fetuses and infants with developmental anomalies. Ultrasound Obstet Gynecol 2012; 39: 666–72. doi: 10.1002/uog.10106 [DOI] [PubMed] [Google Scholar]
- 5.Akgun H, Basbug M, Ozgun MT, Canoz O, Tokat F, Murat N, et al. Correlation between prenatal ultrasound and fetal autopsy findings in fetal anomalies terminated in the second trimester. Prenat Diagn 2007; 27: 457–62. [DOI] [PubMed] [Google Scholar]
- 6.Amini H, Antonsson PE, Papadogiannakis N, Ericson K, Pilo C, Eriksson L, et al. Comparison of ultrasound and autopsy findings in pregnancies terminated due to fetal anomalies. Acta Obstet Gynecol Scand 2006; 85: 1208–16. doi: 10.1080/00016340600880886 [DOI] [PubMed] [Google Scholar]
- 7.Gordijn SJ, Erwich JJ, Khong TY. Value of the perinatal autopsy: critique. Pediatr Dev Pathol 2002; 5: 480–8. doi: 10.1007/s10024-002-0008-y [DOI] [PubMed] [Google Scholar]
- 8.Gordijn SJ, Erwich JJ, Khong TY. The perinatal autopsy: pertinent issues in multicultural Western Europe. Eur J Obstet Gynecol Reprod Biol 2007; 132: 3–7. doi: 10.1016/j.ejogrb.2006.10.031 [DOI] [PubMed] [Google Scholar]
- 9.Sankar VH, Phadke SR. Clinical utility of fetal autopsy and comparison with prenatal ultrasound findings. J Perinatol 2006; 26: 224–9. doi: 10.1038/sj.jp.7211482 [DOI] [PubMed] [Google Scholar]
- 10.Wittschieber D, Klauschen F, Kimmritz AC, von Winterfeld M, Kamphues C, Scholman HJ, et al. Who is at risk for diagnostic discrepancies? Comparison of pre- and post-mortal diagnoses in 1800 patients of 3 medical decades in East and West Berlin. PLoS One 2012; 7: 22. doi: 10.1371/journal.pone.0037460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cockerill R, Whitworth MK, Heazell AE. Do medical certificates of stillbirth provide accurate and useful information regarding the cause of death? Paediatr Perinat Epidemiol 2012; 26: 117–23. doi: 10.1111/j.1365-3016.2011.01247.x [DOI] [PubMed] [Google Scholar]
- 12.Confidential Enquiry into Maternal and Child Health (CEMACH). Perinatal mortality 2007: United Kingdom. London, UK: CEMACH; 2009. [Google Scholar]
- 13.Sieswerda-Hoogendoorn T, van Rijn RR. Current techniques in postmortem imaging with specific attention to paediatric applications. Pediatr Radiol 2010; 40: 141–52. doi: 10.1007/s00247-009-1486-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shojania KG, Burton EC. The vanishing nonforensic autopsy. N Engl J Med 2008; 358: 873–5. doi: 10.1056/NEJMp0707996 [DOI] [PubMed] [Google Scholar]
- 15.McHaffie HE, Fowlie PW, Hume R, Laing IA, Lloyd DJ, Lyon AJ. Consent to autopsy for neonates. Arch Dis Child Fetal Neonatal Ed 2001; 85: F4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brookes JA, Hall-Craggs MA, Sams VR, Lees WR. Non-invasive perinatal necropsy by magnetic resonance imaging. Lancet 1996; 348: 1139–41. doi: 10.1016/S0140-6736(96)02287-8 [DOI] [PubMed] [Google Scholar]
- 17.Breeze AC, Jessop FA, Set PA, Whitehead AL, Cross JJ, Lomas DJ, et al. Minimally-invasive fetal autopsy using magnetic resonance imaging and percutaneous organ biopsies: clinical value and comparison to conventional autopsy. Ultrasound Obstet Gynecol 2011; 37: 317–23. [DOI] [PubMed] [Google Scholar]
- 18.Cannie M, Votino C, Moerman P, Vanheste R, Segers V, Van Berkel K, et al. Acceptance, reliability and confidence of diagnosis of fetal and neonatal virtuopsy compared with conventional autopsy: a prospective study. Ultrasound Obstet Gynecol 2012; 39: 659–65. doi: 10.1002/uog.10079 [DOI] [PubMed] [Google Scholar]
- 19.Griffiths PD, Paley MN, Whitby EH. Post-mortem MRI as an adjunct to fetal or neonatal autopsy. Lancet 2005; 365: 1271–3. doi: 10.1016/S0140-6736(05)74816-9 [DOI] [PubMed] [Google Scholar]
- 20.Sebire NJ, Weber MA, Thayyil S, Mushtaq I, Taylor A, Chitty LS. Minimally invasive perinatal autopsies using magnetic resonance imaging and endoscopic postmortem examination (“keyhole autopsy”): feasibility and initial experience. J Matern Fetal Neonatal Med 2012; 25: 513–18. [DOI] [PubMed] [Google Scholar]
- 21.Woodward PJ, Sohaey R, Harris DP, Jackson GM, Klatt EC, Alexander AL, et al. Postmortem fetal MR imaging: comparison with findings at autopsy. AJR Am J Roentgenol 1997; 168: 41–6. doi: 10.2214/ajr.168.1.8976917 [DOI] [PubMed] [Google Scholar]
- 22.Alderliesten M, Peringa J, van der Hulst V, Blaauwgeers H, van Lith J. Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG 2003; 110: 378–82. [PubMed] [Google Scholar]
- 23.Breeze AC, Cross JJ, Hackett GA, Jessop FA, Joubert I, Lomas DJ, et al. Use of a confidence scale in reporting postmortem fetal magnetic resonance imaging. Ultrasound Obstet Gynecol 2006; 28: 918–24. doi: 10.1002/uog.3886 [DOI] [PubMed] [Google Scholar]
- 24.Hagmann C, Robertson N, Sams V, Brookes J. Postmortem magnetic resonance imaging as an adjunct to perinatal autopsy for renal-tract abnormalities. Arch Dis Child Fetal Neonatal Ed 2007; 92: F215–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Widjaja E, Whitby E, Cohen M, Paley M, Griffiths P. Post-mortem MRI of the foetal spine and spinal cord. Clin Radiol 2006; 61: 679–85. [DOI] [PubMed] [Google Scholar]
- 26.Huisman T, Wisser J, Stallmach T, Krestin G, Huch R, Kubik-Huch R. MR autopsy in fetuses. Fetal Diagn Ther 2002; 17: 58–64. [DOI] [PubMed] [Google Scholar]
- 27.Cohen M, Paley M, Griffiths P, Whitby E. Less invasive autopsy: benefits and limitations of the use of magnetic resonance imaging in the perinatal postmortem. Pediatr Dev Pathol 2008; 11: 1–9. [DOI] [PubMed] [Google Scholar]
- 28.Thayyil S, Schievano S, Robertson NJ, Jones R, Chitty LS, Sebire NJ, et al. A semi-automated method for non-invasive internal organ weight estimation by post-mortem magnetic resonance imaging in fetuses, newborns and children. Eur J Radiol 2009; 72: 321–6. doi: 10.1016/j.ejrad.2008.07.013 [DOI] [PubMed] [Google Scholar]
- 29.Votino C, Verhoye M, Segers V, Cannie M, Bessieres B, Cos T, et al. Fetal organ weight estimation by postmortem high-field magnetic resonance imaging before 20 weeks' gestation. Ultrasound Obstet Gynecol 2012; 39: 673–8. doi: 10.1002/uog.11151 [DOI] [PubMed] [Google Scholar]
- 30.Sandaite I, De Catte L, Moerman P, Gewillig M, Fedele L, Deprest J, et al. A morphometric study of the human fetal heart on post-mortem 3-tesla magnetic resonance imaging. Prenat Diagn 2013; 33: 318–27. [DOI] [PubMed] [Google Scholar]
- 31.Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong W, Olsen O, et al. Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 2013; 382: 223–33. doi: 10.1016/S0140-6736(13)60134-8 [DOI] [PubMed] [Google Scholar]
- 32.Whitby EH, Paley MN, Cohen M, Griffiths PD. Post-mortem fetal MRI: what do we learn from it? Eur J Radiol 2006; 57: 250–5. doi: 10.1016/j.ejrad.2005.11.024 [DOI] [PubMed] [Google Scholar]
- 33.Prodhomme O, Seguret F, Martrille L, Pidoux O, Cambonie G, Couture A, et al. Organ volume measurements: comparison between MRI and autopsy findings in infants following sudden unexpected death. Arch Dis Child Fetal Neonatal Ed 2012; 97: F434–8. [DOI] [PubMed] [Google Scholar]
- 34.Thayyil S, Chandrasekaran M, Chitty LS, Wade A, Skordis-Worrall J, Bennett-Britton I, et al. Diagnostic accuracy of post-mortem magnetic resonance imaging in fetuses, children and adults: a systematic review. Eur J Radiol 2010; 75: e142–8. doi: 10.1016/j.ejrad.2009.10.007 [DOI] [PubMed] [Google Scholar]
- 35.Thali MJ, Yen K, Schweitzer W, Vock P, Boesch C, Ozdoba C, et al. Virtopsy, a new imaging horizon in forensic pathology: virtual autopsy by postmortem multislice computed tomography (MSCT) and magnetic resonance imaging (MRI)–a feasibility study. J Forensic Sci 2003; 48: 386–403. [PubMed] [Google Scholar]
- 36.Thayyil S, Sebire NJ, Chitty LS, Wade A, Olsen O, Gunny RS, et al. Post mortem magnetic resonance imaging in the fetus, infant and child: a comparative study with conventional autopsy (MaRIAS protocol). BMC Pediatr 2011; 11: 120. doi: 10.1186/1471-2431-11-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tofts PS, Jackson JS, Tozer DJ, Cercignani M, Keir G, MacManus DG, et al. Imaging cadavers: cold FLAIR and noninvasive brain thermometry using CSF diffusion. Magn Reson Med 2008; 59: 190–5. doi: 10.1002/mrm.21456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thayyil S, De Vita E, Sebire NJ, Bainbridge A, Thomas D, Gunny R, et al. Post-mortem cerebral magnetic resonance imaging T1 and T2 in fetuses, newborns and infants. Eur J Radiol 2012; 81: 232–8. doi: 10.1016/j.ejrad.2011.01.105 [DOI] [PubMed] [Google Scholar]
- 39.Hillewig E, Aghayev E, Jackowski C, Christe A, Plattner T, Thali MJ. Gas embolism following intraosseous medication application proven by post-mortem multislice computed tomography and autopsy. Resuscitation 2007; 72: 149–53. [DOI] [PubMed] [Google Scholar]
- 40.Breeze AC, Jessop FA, Whitehead AL, Set PA, Berman L, Hackett GA, et al. Feasibility of percutaneous organ biopsy as part of a minimally invasive perinatal autopsy. Virchows Arch 2008; 452: 201–7. doi: 10.1007/s00428-007-0548-7 [DOI] [PubMed] [Google Scholar]
- 41.Garg S, Punia RP, Basu S, Mohan H, Bal A. Comparison of needle autopsy with conventional autopsy in neonates. Fetal Pediatr Pathol 2009; 28: 139–50. doi: 10.1080/15513810902772482 [DOI] [PubMed] [Google Scholar]
- 42.Fariña J, Millana C, Fdez-Aceñero MJ, Furió V, Aragoncillo P, Martín VG, et al. Ultrasonographic autopsy (echopsy): a new autopsy technique. Virchows Arch 2002; 440: 635–9. doi: 10.1007/s00428-002-0607-z [DOI] [PubMed] [Google Scholar]
- 43.Fan JK, Tong DK, Poon JT, Lo OS, Beh PS, Patil NG, et al. Multimodality minimally invasive autopsy—a feasible and accurate approach to post-mortem examination. Forensic Sci Int 2010; 195: 93–8. doi: 10.1016/j.forsciint.2009.11.019 [DOI] [PubMed] [Google Scholar]
- 44.Roberts ISD, Benamore RE, Benbow EW, Lee SH, Harris JN, Jackson A, et al. Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 2012; 379: 136–42. doi: 10.1016/S0140-6736(11)61483-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ruder TD, Hatch GM, Ebert LC, Flach PM, Ross S, Ampanozi G, et al. Whole body postmortem magnetic resonance angiography. J Forensic Sci 2012; 57: 778–82. doi: 10.1111/j.1556-4029.2011.02037.x [DOI] [PubMed] [Google Scholar]
- 46.O'Donoghue K, O'Regan KN, Sheridan CP, O'Connor OJ, Benson J, McWilliams S, et al. Investigation of the role of computed tomography as an adjunct to autopsy in the evaluation of stillbirth. Eur J Radiol 2012; 81: 1667–75. doi: 10.1016/j.ejrad.2011.03.093 [DOI] [PubMed] [Google Scholar]
- 47.Ben-Sasi K, Chitty LS, Franck LS, Thayyil S, Judge-Kronis L, Taylor AM, et al. Acceptability of a minimally invasive perinatal/paediatric autopsy: healthcare professionals' views and implications for practice. Prenat Diagn 2013; 33: 307–12. [DOI] [PubMed] [Google Scholar]
- 48.NHS Implementation Subgroup of the Department of Health Post Mortem Fosensic and Disaster Imaging Group. Can cross-sectional imaging as an adjunct and/or alternative to the invasive autopsy be implemented within the NHS? Report from the NHS Implementation Sub-group of the Department of Health Post Mortem Forensic and Disaster Imaging Group. 2012. Available from: www.dh.gov.uk/health/2012/10/less-invasive-autopsy/ [Google Scholar]