Abstract
Virtual anthropology is made possible by modern cross-sectional imaging. Multislice CT (MSCT) can be used for comparative bone and dental identification, reconstructive identification and lesion identification. Comparative identification, the comparison of ante- and post-mortem imaging data, can be performed on both teeth and bones. Reconstructive identification, a considerable challenge for the radiologist, identifies the deceased by determining sex, geographical origin, stature and age at death. Lesion identification combines virtual autopsy and virtual anthropology. MSCT can be useful in palaeopathology, seeking arthropathy, infection, oral pathology, trauma, tumours, haematological disorders, stress indicators or occupational stress in bones and teeth. We examine some of the possibilities offered by this new radiological subspeciality that adds a new dimension to the work of the forensic radiologist. A multidisciplinary approach is crucial and involves communication and data exchange between radiologists, forensic pathologists, anthropologists and radiographers.
Virtual autopsies are currently becoming increasingly common worldwide in forensic medicine.1 Use of multislice CT (MSCT) or multidetector CT (MDCT) before classic medicolegal autopsy gives the forensic pathologist considerable information on injuries and cause of death.2 A recent advance in forensic imaging is post-mortem CT angiography, which yields further information on soft tissues and visceral and vascular injuries.3
Modern cross-sectional imaging can be used in virtual anthropological studies as well as in virtual autopsy.4
In biological anthropology, it can be applied to compare bone or dental criteria between species. An important application is forensic anthropology, to obtain positive identification of an unknown decedent. The introduction of imaging in anthropology is of course not new, and many radiographic applications have been already described and published.
In virtual anthropology, teeth and bones can be studied by MRI or by MSCT. MRI has numerous applications,5,6 and it will certainly become an important tool in forensic study of the living, particularly for age assessment. This technique presents many advantages compared with MSCT, and, like ultrasound, it is X-ray free. However, access to MRI in thanatology is currently difficult, mainly because of limited time availability of the machine.
The wide range of possibilities offered by MSCT may seem bewildering to a non-radiologist! If an MSCT examination is to give optimal results, many technical conditions must be adhered to in terms of image quality, spatial resolution and contrast. If not, the final images may even be unusable, in particular, for analysis of fine trabecular bone lesions (Figure 1). The initial CT must be performed with appropriate voltage, amperage, field of view and slice thickness. After acquisition, reconstruction time is critical. Choice of thickness and interval and choice of filters influence voxel size and the possibility of radiological interpretation. Post-processing requires powerful computers. Choice of reconstruction technique must be appropriate for the initial objectives: two-dimensional (2D) reconstructions [multiplanar reconstructions (MPRs): sagittal, coronal and oblique] or three-dimensional (3D) reconstructions [maximum intensity projection (MIP), surface-shaded display or volume rendering technique (VRT)].
Figure 1.
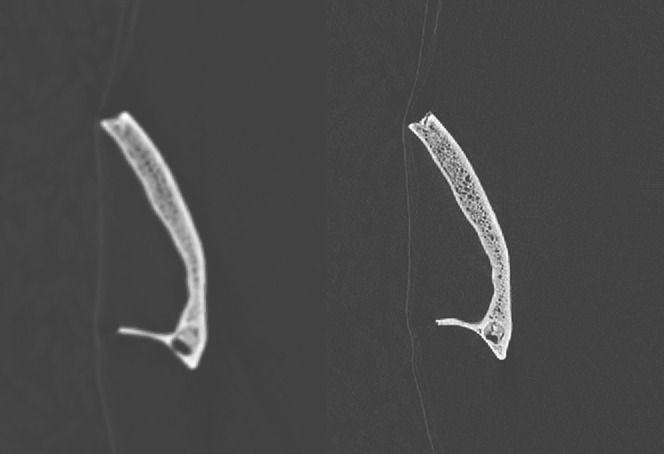
Sagittal multiplanar reconstructions of a fragmentary frontal bone. (Left image) Soft-tissue filter (B30). (Right image) Bone filter (H70). The trabecular bone of the diploe and the frontal sinus, filled with sediment, can only be examined with the dedicated bone filter.
The material studied may range from one single bone or part of a bone to partial skeletal remains, or less often complete skeletal remains. The state of preservation may vary greatly, from dry bones to a complete putrefied, charred or mummified body. Examination can be requested in a variety of contexts: exhumation, museum research, mass disasters, contemporary bodies, ancient bodies, humanoid fossils and other such requests. The forensic pathologist, the forensic anthropologist and the anthropologist encounter a wide range of situations.
Just as when working with patients in clinical practice, one of the central issues is benefit/risk: what does the investigation add in terms of anthropological study? What do the anthropologist, the forensic anthropologist or the forensic pathologist who request the radiological examination expect? This must be discussed between the physician requesting the examination and the radiologist who performs it. Concerns relating to imaging of the bones and teeth of deceased persons are not very different from the concerns of clinical practice: the radiologist must always be aware of the reasons behind the examinations to use an appropriate CT image acquisition protocol.
MSCT can be used for (1) comparative identification, (2) reconstructive identification and (3) lesion identification. We look here at some of the possibilities offered by this new radiological subspeciality that adds a new dimension to the work of the forensic radiologist.
COMPARATIVE IDENTIFICATION
When a body is not identified or is unidentifiable, as with skeletal, charred, putrefied or mutilated individuals, radiological investigation is necessary. It has two major aims: identification of the person and identification of the injuries. This can be important in hidden crimes (such as a person first killed by gunshot and then burnt in their home). Comparison of ante-mortem radiographs or MSCT images with post-mortem MSCT images can be vital for positive identification of the deceased: this is the goal of comparative identification.
Among the various tools and methods used as an aid to identification, radiography is considered as a simple method (identifying scars, tattoos, morphological characteristics and fingerprints).7 Autopsy, like anthropological study, is considered as a tool of intermediate complexity. Clearly, cross-sectional imaging represents the passage from a simple to an intermediate level of complexity. For Ciaffi et al,8 in view of developments in radiographic technologies and the increasing number of studies on their application to the forensic setting, in the future, radiology will become one of the most useful tools in the field of personal identification. The deceased is identified by a number of features, either alone or in conjunction. As with plain radiographs, identification may be based on the detection of surgical material, variants of normal radiological appearance or pre-existing abnormalities (congenital or acquired).9,10 There is no consensus on the specific number of concordant traits required to establish an identity. The lack of a standard ruling on which, and how many, features and matching points are needed for positive identification makes the process difficult. Some authors consider that one to four concordant features and no discrepancies usually establish positive identification. However, others state that, in some cases, the combined presence of numerous common and non-specific features are required.11–13 Others believe that several concordant traits in at least two different body areas are necessary to determine a positive identity.14 It is obvious that with comparative identification, error rates and standard deviations are not easily quantifiable.
Comparative bone identification
Like plain radiographs, ante- and post-mortem MSCT images can be compared. More and more investigations are carried out in clinical and surgical situations making such comparisons more and more frequent. According to Murphy et al,15 radiographic comparisons of ante- and post-mortem images lead to positive identification in 42% of cases. Few data are available on the potential advantages of MSCT for comparative identification. It is estimated to provide positive identification in about 5% of cases.4,16 Although, at the present time, CT is less used than plain radiography, this will change because of the increasing number of CT examinations performed routinely in radiology departments. Nevertheless, it is interesting to compare radiographic data used for the identification because the same reasoning is used with CT.11 For practical radiographic comparative identification, the chest is the most informative anatomical region (53%), followed ex aequo by the skull and the extremities (20%), the lumbar spine (17%), cervical spine (10%) and pelvis (3%). The features used for positive identification are chest calcifications (29%), normal variations (24%), surgical devices (18%), fractures (14%), followed ex aequo by congenital abnormalities, and abdominal calcifications and arthritic lesions (5%).
In current forensic practice, foreign material is of great value for identification.9,10 As osteosynthesis and endoprosthesis techniques are now widely used, a considerable amount of foreign material may be detected in unidentified corpses (Figures 2 and 3). Normally, use of these surgical techniques means that ante-mortem radiographs or MSCT documentation is available. The main difficulty is of course the recovery of these ante-mortem data!
Figure 2.
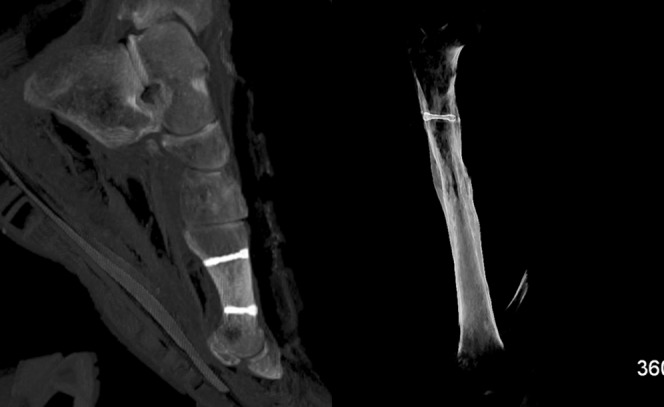
Surgical material in unidentified bodies. (Left image) maximum intensity projection (MIP) reconstruction of the left first metatarsal showing two surgical screws, with evidence of osteotomy of the head of the metatarsal. (Right image) MIP reconstruction of a right femur (skeletal remains) with a surgical screw at the upper femoral diaphysis.
Figure 3.
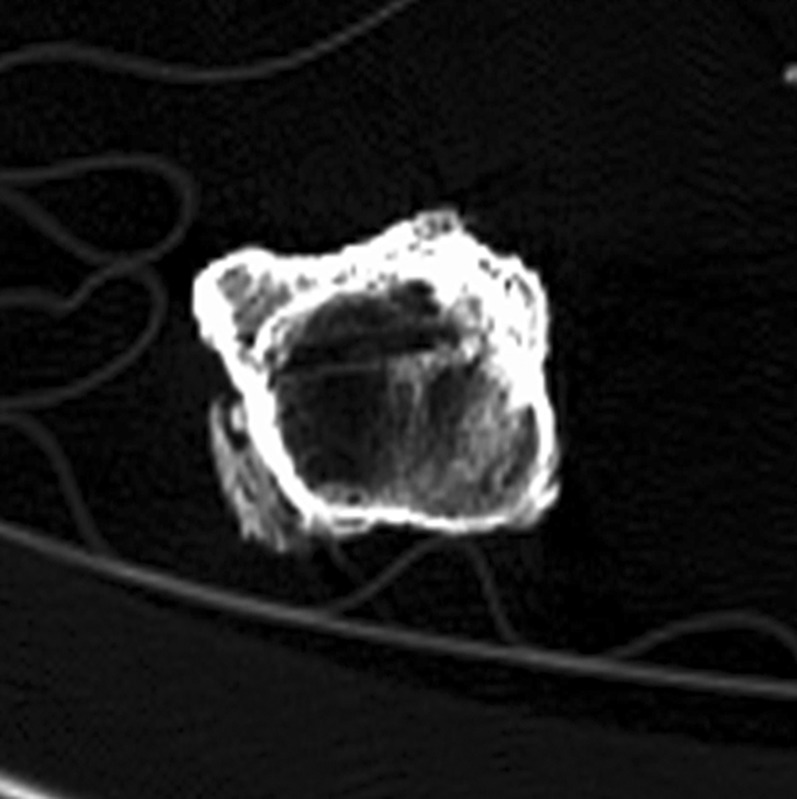
Bone stigmata of surgical material removal. Axial slice of the upper right femoral diaphysis. Linear bone defect with condensation of the edges because of removal of a surgical screw.
Knowledge of normal bone variations is also pertinent (Figure 4). The reference textbook for radiologists on this subject is Keats and Anderson's17 “Atlas of normal roentgen variants that may simulate disease”.
Figure 4.

Normal bone variations useful for comparative identification. (Left image) volume rendering technique reconstruction of skeletal remains. Calcification of the transverse superior ligament of the scapula (arrow). (Right image) Coronal maximum intensity projection reconstruction of the sternum. Presence of a superior episternal bone (arrow).
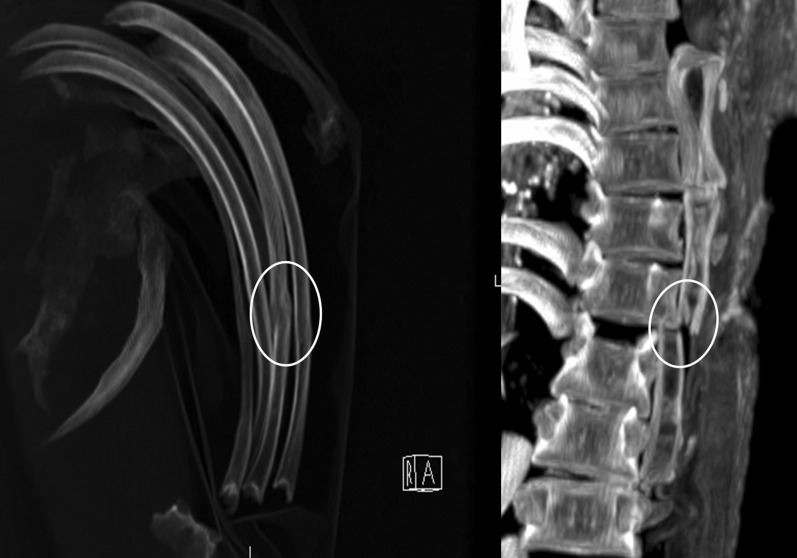
Arthropathies of the appendicular and axial skeleton enable the radiologist to diagnose some degenerative changes, diffuse idiopathic skeletal hyperostosis and ankylosing spondylitis, among other diseases (Figure 5).18
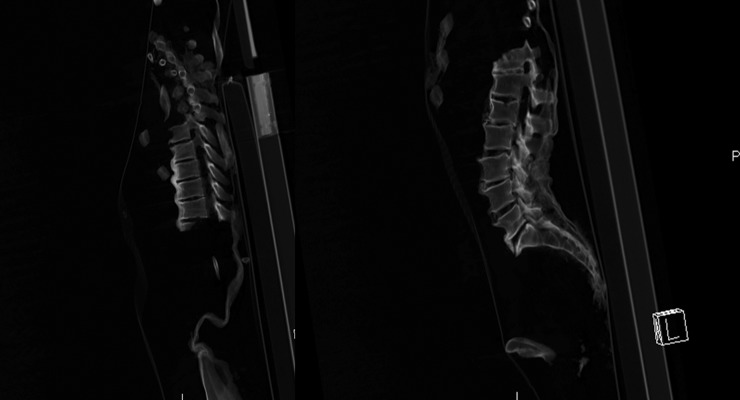
Figure 5.
Spinal arthropathic changes on skeletal remains. (Left image) Sagittal maximum intensity projection (MIP) reconstruction of the thoracic spine. Ossification of the anterior longitudinal spinal ligament affecting >4 contiguous vertebrae, without sacroiliitis. Intervertebral disc spaces and apophyseal joints are preserved. These changes suggest diffuse idiopathic skeletal hyperostosis. (Right image) Sagittal MIP reconstruction of the lumbar spine. Osteophytic spurring of the superior and inferior plates of numerous vertebrae. L, left.
When only a single bone is available, the potential identification criteria are the presence of anomalous or unusual development, disease or degeneration, tumours, trauma, iatrogenic interference, some particular vascular grooves and trabecular patterns.11
Obviously, the expert who bases identification on a trait that they consider to be rare is making a subjective judgment. Caution is always needed because some authors have demonstrated that some morphological characteristics of bone, such as fractures, pathological conditions and surgical material, supposed to be rather rare, may in fact be quite common.19
Comparative dental identification
When comparing ante-mortem and post-mortem dental radiographs, the forensic radiologist observes similarities and differences.7,11 In most cases, the ante-mortem dental radiographs were obtained some months or even years before the comparisons are made. Some similarities are commonplace or non-specific and are of low discriminant value. Others may be so distinctive as to ensure uniqueness. Likewise, apparent differences between ante-mortem and post-mortem radiographs may have a reasonable explanation, whereas others are incompatible and rule out the putative victim as the decedent. For example, the major incompatible inconsistencies in adults between ante- and post-mortem radiographs are the absence of a tooth on the ante-mortem radiograph which is present on the post-mortem radiograph, the presence of a tooth filling on the ante-mortem radiograph which is virgin on the post-mortem radiograph or a fully formed tooth on the ante-mortem radiograph, which is incompletely formed on the post-mortem radiograph. On the contrary, some discrepancies observed in adults are due only to the time elapsed between ante- and post-mortem radiographs. For example, the presence of a tooth on the ante-mortem radiograph, which is absent on the post-mortem radiograph because of extraction; the presence of a virgin tooth on the ante-mortem radiograph, which is filled or shows caries on the post-mortem radiograph; or an incompletely formed tooth on the ante-mortem radiograph, which is fully formed on the post-mortem radiograph.
Identification from dental radiographs relies on a number of points of comparison (Figure 6):
– the number and arrangement of teeth (missing teeth, rotated teeth, spacing, extra teeth and impacted teeth)
– caries and periodontal bone loss
– coronal restorations
– hidden restorations (bases under fillings, pins, root canal fillings, posts and implants) seen only radiographically
– bony pathology
– dental anatomy
– trabecular bone pattern and crestal bone topography
– nutrient canals
– anatomical bony landmarks
– maxillary sinus and nasal aperture size and morphology
– frontal sinus size and morphology.
Figure 6.
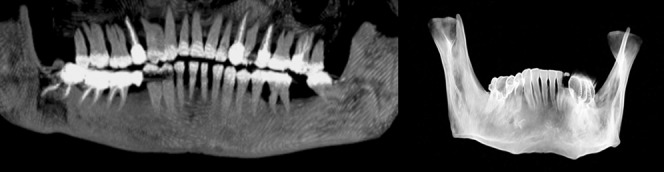
Dental reconstructions performed for identification purposes. (Left image) Panoramic maximum intensity projection reconstruction. Root canal fillings, metallic crowns, bridges and missing teeth can be detected on a single reconstruction. (Right image) Volume rendering technique reconstruction of a mandible, with coloured dental structures corresponding to metal crowns.
MSCT or cone beam images require post-treatment processing to obtain the equivalent of a panoramic radiograph.20 It is also possible to study the development of each tooth or to demonstrate dental restoration work by generating oblique MPR or MIP slices.21 Unfortunately, dental restorations cause streak artefacts because of their increased radio-opacity, which can make comparison difficult or impossible between ante-mortem radiographs and post-mortem MSCT reconstructions.21
RECONSTRUCTIVE IDENTIFICATION
Reconstructive identification is a considerable challenge for the radiologist. The deceased is identified by determining a biological profile, whose most important features are sex, geographical origin, stature and age at death. Obviously, DNA (deoxyribonucleic acid) analysis is now also extremely valuable for positive personal identification. This has perhaps made a difference to the workload of forensic anthropologists and odontologists, but, fortunately, it has not completely replaced other methods. In practice, even when DNA is recoverable, analysis is limited by the need for appropriate comparisons to allow a positive identification.
The first step is to determine the bone or dental maturity of the individuals studied. In prepubertal juveniles, many criteria such as geographic origin, stature and sex determination are in reality unavailable, although certain points may be debated in some articles or textbooks. However, age at death can always be assessed.
An important point regarding all metric studies, whether of population ancestry, age at death or stature, is that the osteometric measurements must be repeatable, and there must be no significant difference between traditional and MSCT osteometric measurements. Many authors have demonstrated these crucial points of methodology.22,23
Sex assessment
Sex can be assessed with both metric and visual data. As in physical anthropology, the most dimorphic elements are the skull and the innominate bone.
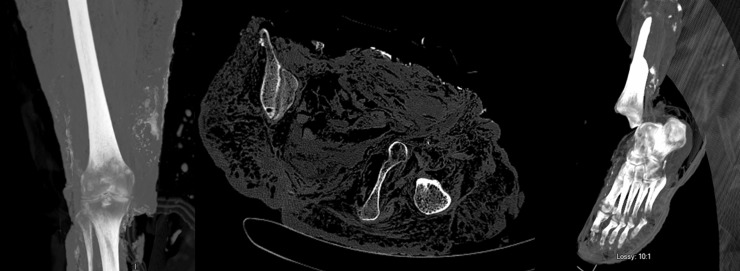
Morphological study
This is similar to classic dry bone study. However, 3D reconstructions in VRT mode with adequate filters offer added possibilities. The bone can be rotated in the same way as an anthropologist rotates a dry bone. The major advantage is that the bone can be cut virtually, which the anthropologist often cannot do with high-value specimens such as hominid fossils. Many criteria have been described, and it is not possible to cite them all.7,24,25 Some useful classic criteria for the forensic radiologist are the following (Figure 7):
– on the innominate bone: analysis of the ventral arch, the subpubic concavity, the shape of the ischiopubic ramus and the great sciatic notch7,24,25
– on the skull: analysis of the appearance of the forehead, the general shape of the skull, the appearance of the mastoid process and the mandibular ramus7,24,25
– on costal cartilage calcifications: superior and inferior edge calcifications for males and central calcifications for females.26
Figure 7.
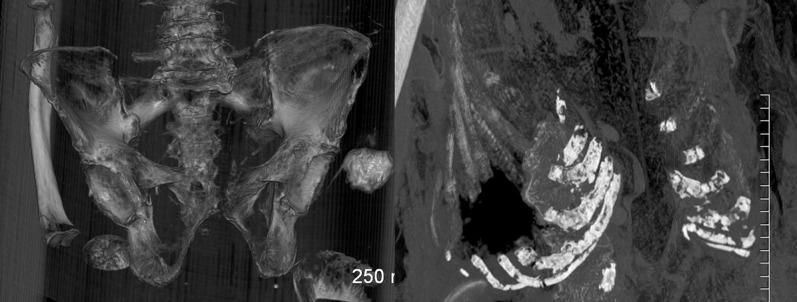
Morphological dimorphism. (Left image) Volume rendering technique reconstruction of the pelvis, skeletal remains. The wide subpubic angle is a female trait. (Right image) Maximum intensity projection reconstruction of the costal cartilages. Central costal cartilage calcifications, which are a female trait.
Metric study
Once again, many criteria have been described, and they cannot all be cited. Some useful classic criteria for the forensic radiologist are:
– measurement of certain epiphyseal widths
– craniometric analysis, which requires the positioning of various landmarks on the skull. The principle is the same as for population determination, based on discriminant function analysis of the different measurements and giving results for two functions27
– study of foramen magnum size and angles of the laryngeal laminae of the thyroid cartilage.28,29
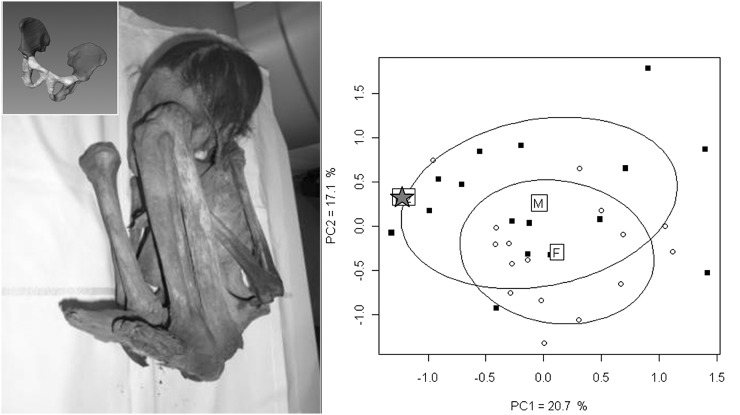
Another method known as morphometric geometrical analysis with procrustes superimpositions is also interesting for the forensic radiologist, but requires specific software.30–32 With this technique, landmarks or semi-landmarks are placed on 2D or 3D CT reconstructions of the innominate bone and, secondarily, these coordinates are projected on a panel of a previously studied population and of individuals (Figure 8).33,34 This can be useful when direct examination of dry bones is not possible, as with mummified individuals. One of the advantages of this technique in anthropology is that features contributing to shape differences and size differences can be identified and analysed.
Figure 8.
Use of morphometric geometrical analysis with procrustes superimposition on the pelvis. (Left image) Photograph of the individual with damaged pelvic soft tissue, making sex estimation visually impossible [left upper image: three-dimensional (3D) reconstruction of the pelvis after segmentation of both innominate bones]. (Right image) Principal component analysis giving a projection of the subject (star), based on the analysis of some 3D landmarks, within population data, in favour of a male subject. F, females; M, males; PC, principal component.
Age at death can be assessed through dental and bone examination
Radiological images merely reflect biological age. It is important to be aware that skeletal age, bone age and dental age are also the reflection of biological age, which is not always related to chronological age or official age and is subject to interindividual variations.35 Estimation of age is based on biological changes that take place throughout life. There is a high statistical correlation between a person's chronological age and their biological stage of growth and development. Assessment of biological age is usually most accurate in the early phases of development and decreases as the individual gets older.7 In children, females show advanced skeletal maturation compared with males. Therefore, when possible, sex should be determined before attempting to assess age at death. In juvenile individuals, when only bones are preserved with no soft tissue or when the state of preservation is poor, it is not possible to obtain information on sex.
Bone age
For juvenile individuals, many methods based on bone analysis are possible (Figures 9 and 10):
-
○ the presence/absence of primary ossification centres
-
○ the presence/absence of secondary ossification centres
-
– Metric methods
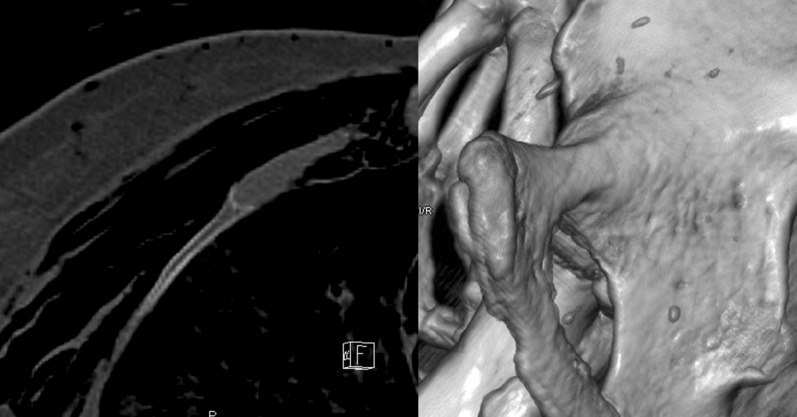
Figure 9.
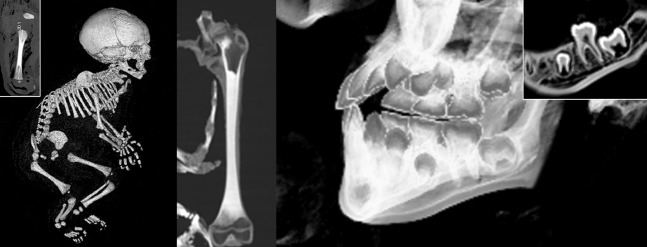
Age assessment in juveniles. (Left image) Volume rendering technique (VRT) skeletal reconstruction in a case of infanticide, with late discovery of the body (3 weeks) [left upper image: maximum intensity projection (MIP) reconstruction enables measurement of the left femoral diaphysis]. (Middle image) MIP reconstructions of the left femur of a mummified juvenile, showing the absence of epiphyseal fusion. (Right image) VRT reconstruction of the left mandible of a mummified juvenile (right upper image: multiplanar reconstruction of the posterior part of the mandible). Dental age can be estimated by analyses of the development of the crown and the apex.
Figure 10.
Age assessment in adults. (Left image) Axial multiplanar reconstruction of the sternal extremity of the right fourth rib. Appearance suggesting Phase 4 of the iScan™ system. (Right image) Volume rendering technique reconstruction of the right pubic symphysis. Appearance suggesting Suchey–Brooks Phase VI. F, front.
In mature individuals, bone growth is replaced by degenerative changes. Anthropological methods are based on these changes, which affect bones, teeth and cartilage. The anthropological use of MSCT principally relies either on specific MSCT criteria and characteristics or on the transposition of techniques applied on dry bones in physical anthropology (Figure 10).46,47 Consequently, the radiologist who performs these investigations must be familiar with the techniques of physical anthropology. It is not possible to cite all the different methods transposed. However, the most important and the most often used are the appearance of the right fourth rib according to the iScan™ classification, the pubic symphysis, using the Suchey–Brooks classification and the auricular surface according to Lovejoy's classification.48–50 Some other methods defined with MSCT may also be helpful, such as the appearance of the trabecular bone of the auricular surface, the right first rib and the clavicle.8,51–53 The forensic radiologist needs to be aware of the limitations of these methods and to know the different average ages, standard deviations of the state variables used and intra- and interobserver variabilities, and should present the results in terms of probability.
Dental age
Dental age is generally estimated by evaluation of the degree of mineralization or eruption of the teeth. Classically, dental age is closer to chronological age than skeletal age.54 One of the most likely explanations is that the development of all the deciduous dentition and part of the permanent dentition takes place before birth in a relatively protected environment, whereas skeletal growth and development, although having a strong genetic basis, are influenced for a longer time by external factors such as nutrition and disease.7
For juvenile individuals, numerous methods for dental age estimation are possible (Figure 9):
For young adults dental age estimation is possible using the third molar (method of Mincer et al).64
MSCT or cone beam images require post-treatment processing to obtain the equivalent of a panoramic radiograph. The development of each tooth can be studied or dental restoration work can be demonstrated by generating oblique MPR or MIP slices.
Population ancestry
When determining population ancestry or geographical origin, also termed ethnic affiliation or racial phenotype by some authors, the skull is critical to the evaluation. Geographical origins are conventionally divided into three major populations: Caucasoid, Negroid and Mongoloid.24 Two different approaches are possible: visual and scopic, or morphological and metric.
Typical visual descriptions can be found in every textbook of anthropology.7,24,25 However, it is important for the radiologist to be aware that these evaluations have limitations and must be made with great caution. In reality, determination of population ancestry is complicated by every kind of admixture, as well as by the variability that exists within every general geographical group.
For craniometric analysis, a number of landmarks are positioned on the skull. The principle is based on a discriminant function analysis of the different measurements, giving results for two functions. The individual studied can therefore be assigned to one of the three major geographical groups. Beside descriptions of the methods by classic authors like Howells65 or Krogman and Iscan,66 and others,67,68 softwares such as Fordisc v. 3.0 (Knoxville, TN) and Cranid v. 6 (Sydney, Australia) provide useful information and are practical and easy to use.
Stature determination
For stature determination, the two principal methods are anatomical and mathematical.
The anatomical method involves measuring all of the skeletal elements that contribute to height and then adding a constant.69,70 Unfortunately, it requires a completely undamaged skeleton.
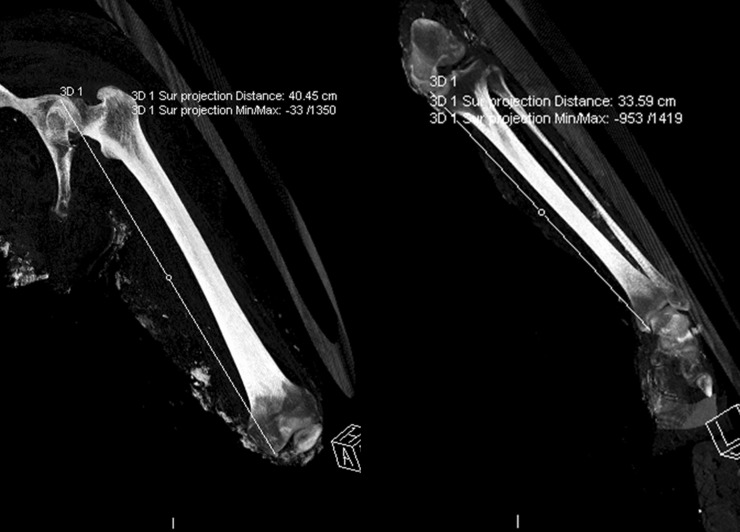
The mathematical method is based on the correlation between bones and body parts and stature (Figure 11).7 Multiple regression formulas exist for a number of single bones or combinations of bones. It is important that sex and geographical origin are known before estimating stature, so that the appropriate formula can be used.71–74
Figure 11.
Maximum intensity projection reconstructions of the left lower limb of a putrefied unidentified body performed for stature determination. (Left image) Measurement of the maximum length of the femur. (Right image) Measurement of the total length of the tibia. 3D, three-dimensional; A, anterior; L, left; max, maximum; min, minimum.
IDENTIFICATION OF LESIONS ON SKELETAL REMAINS
Lesion identification is an important feature common to virtual autopsy and virtual anthropology. MSCT can be applied to the palaeopathological examination of bones and teeth. Palaeopathology is the study of ancient diseases, and the application of radiology to palaeopathology is known as palaeoradiology.18 However, palaeoradiology is also very useful on forensic and recent skeletal remains. Human osteopathology is classified into several general groups: arthropathy, infection, oral pathology, trauma, tumours, haematological disorders, stress indicators, occupational stress.
The first step in lesion identification consists in differentiating lethal and non-lethal pathological lesions.
Bone is an excellent indicator of the type of trauma: gunshot wound, or injury with a sharp or blunt instrument. Sometimes, bone is the only element that remains if there have been major putrefactive changes. Knowledge of the type of fracture can define the nature of the trauma or of the wounding agent. Of course, pseudarthrosis may be seen as a complication of fracture. In some cases, the fracture may mimic the shape of the instrument. Other particularities are laryngeal fracture secondary to hanging or strangulation, which may be detected on putrefied or mummified bodies.
Dating of bone trauma is not an exact science.75,76 Description of the fractures is most important, to determine if different stages of bone consolidation are acquired or not (Figures 12 and 13). This reasoning is the same as in clinical radiology.77
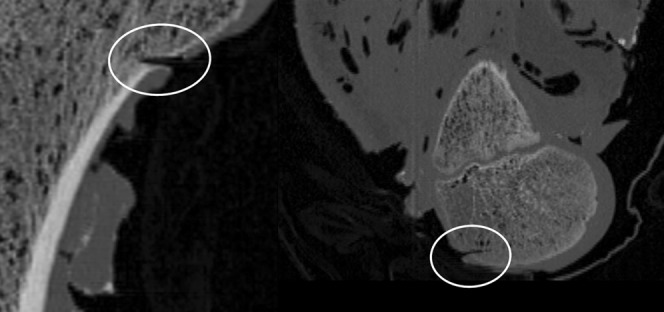
Figure 12.
Axial maximum intensity projection reconstructions. (Left image) Reconstruction of the left ribs of skeletal remains, showing bone consolidation with a hard callus of the anterior arch of one rib (circle). (Right image) Reconstruction of the sternum of a mummified individual, showing the absence of bone consolidation with displacement of the fracture (circle). A, anterior; R, right.
Figure 13.

Volume rendering technique reconstructions of a skull (dry bones) which had been restored, visually masking all the fracture lines. (Left image) Complete volume. (Right image) Virtual section of the right part, increasing the contrast of the traumatic lesions of the left part. The most important finding is the left parietal injury with numerous radiating fractures, giving a stellate appearance.
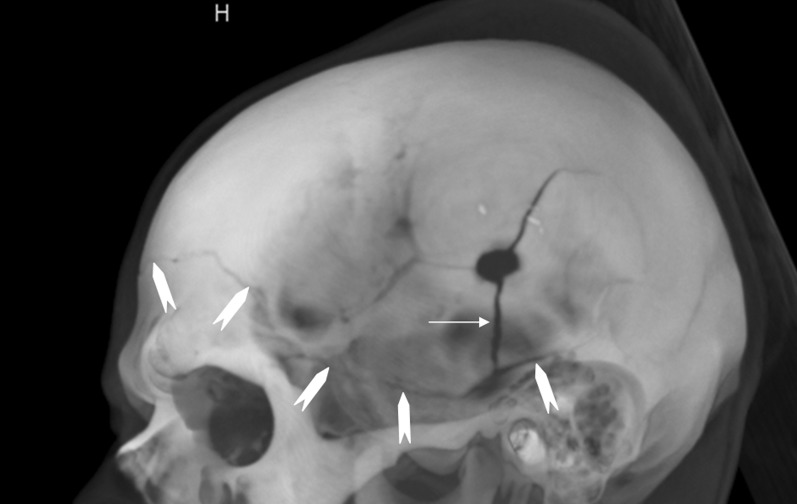
Some helpful rules should be borne in mind by the forensic radiologist when interpreting skull trauma:
– Puppe's rule, which applies when two blunt force injuries with intersecting fractures are visible.78,79 It states that the fractures from the first injury develop normally, whereas those caused by the subsequent injury are stopped where the structure of the skull has already been damaged. Although multiple gunshot wounds of the skull are much more difficult to analyse than blunt-instrument wounds, the sequence of the shots can sometimes be determined from the pattern of radial fracture lines. If a fracture related to an entrance hole passes another entrance hole and is not terminated, the entrance hole causing that fracture must have been inflicted first (Figure 14).
– The hat brim line rule.80 The hat brim line corresponds to a band-like area of approximately 3 cm whose lower limit runs from the top of the eyebrows, around the upper margin of the auricle and along the occipital pole at the back. Classically, an injury located above the hat brim line is more likely the result of a blow, whereas a fall would generally produce a wound at the level of the hat brim line. Recent studies have yielded additional information and criteria that can be helpful to differentiate blows from a fall, even if some do not exclusively concern bone.81–83 The following criteria were found to be suggestive of blows: more than three lacerations, laceration length of 7 cm or more, comminuted or depressed calvarial fractures, lacerations or fractures located above the hat brim line, left-side lateralization of lacerations or fractures, more than four facial contusions or lacerations, the presence of ear lacerations, the presence of facial fractures and the presence of post-cranial osseous and/or visceral trauma.
Figure 14.
Volume rendering technique reconstruction of a skull with gunshot trauma, left view. Illustration of Puppe's rule. The radial inferior fracture (arrow) originating from the bone defect (exit wound) ends where it meets another fracture originating from the contralateral entry wound (arrowheads). H, head.
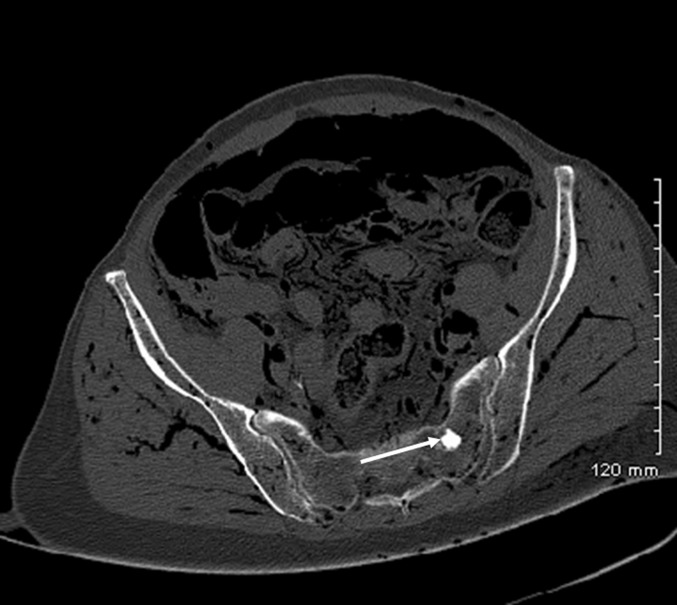
In ballistic trauma, MSCT is helpful in determining criteria such as location of the projectile(s), determination of the direction of fire and entry and exit bone wounds.84–88 Ricochets may also be detected by imaging. The same is true of sharp trauma, with visualization of deep bone laceration or of cartilage section in some cases (Figure 15).89
Figure 15.
Sagittal multiplanar reconstructions of an immature human femur. (Left image) Proximal part. (Right image) Distal part. Visualization of cuts in cortical bone and trabecular bone (circles) after use of a blade in a case of dismemberment.
MSCT is effective in identifying infectious lesions and is more informative than plain radiography (Figure 16).68 Infectious processes can affect bones, teeth and also soft tissues, so MSCT can be very helpful in the study of mummies. More rarely, bone tumours may be observed, or features secondary to metabolic changes or anaemia, such as cribra orbitalia, Harris lines, osteopenia or osteoporosis (Figure 17).18 Foreign bodies may also be detected within bones. Another advantage is the detection of the stigmata of occupational stress or cultural artefacts, such as intentional or artificial cranial deformations (Figure 18). Other bone lesions may be diagnosed, such as arthropathies, that may be important for comparative identification.
Figure 16.
Bone infection complications. Volume rendering technique reconstruction of the right femur (right upper image: axial aspect of the femoral diaphysis). Periosteal apposition secondary to osteomyelitis. H, head.
Figure 17.
Axial slice of an unidentified putrefied body. Hyperdense appearance of the trabecular bone, in favour of a benign tumour of the left sacrum (enostosis) (arrow).
Figure 18.

Volume rendering technique reconstruction of the skull of a mummified South American child (pre-Columbian epoch); right view, presenting an intentional cranial deformation. Some Wormian bones are also visible.
Taphonomy and pseudopathology should not be forgotten! Forensic taphonomy is the interdisciplinary study and interpretation of post-mortem processes of human remains in their depositional context.90 Taphonomic details are critically important for estimating time since death and differentiating injuries from post-mortem changes (Figure 19). The radiologist who performs post-mortem MSCT must be familiar with late post-mortem changes, to avoid misinterpreting normal changes as traumatic injuries. Such confusion, especially when exhumed bodies are concerned, could potentially have significant judicial consequences. Many anatomical parts may be involved: post-mortem changes of the ossicular chain of the middle ear, and axial and appendicular joint disarticulations.68,91 Owing to the loss of soft tissues and costal cartilages, the ribs, sternum and clavicles may collapse into the chest cavity. The hyoid bone may fall near the spine. The mandible may be disarticulated and some teeth may be absent because they have fallen after death. This must not be confused with post-traumatic lesions.
Figure 19.
Taphonomical appearance after long immersion in water, with adipocere changes. (Left image) Coronal maximum intensity projection (MIP) reconstruction of the right lower limb. (Middle image) Axial slice. Multiple spontaneous cutaneous and subcutaneous hyperdense areas can be seen because of adipocere changes. Gaseous dissection within the muscular tissues is also visible. (Right image) MIP reconstruction of the right lower limb, with disarticulation of the ankle because of taphonomical processes.
CONCLUSION
For current anthropological purposes, MSCT has many advantages over dry bone analysis. One of its major assets in forensic anthropology is the elimination of lengthy bone preparation, which may damage fragile bone. This can be particularly useful when bones are very burned or charred. Documentation by radiological imaging is classically described as observer-independent, objective and non-invasive. Another advantage of MSCT is the virtual access to bones, where physical access is impossible, such as bones embedded in sediment or concrete blocks.18,92 Also, of major interest is the conservation of images and the reconstructions. Further studies can be carried out on the object scanned, independently of its state of preservation. This opens up a new approach to quality control and expert supervision, as well as image transmission and use in forensic telemedicine. Additionally, MSCT can be performed in the country where the bones or body were discovered, whereas further work on image analysis and reconstructions can be continued in another country. Image and data processing offer objective visualization and recapitulation of forensic results, with the high spatial resolution of MSCT. Unfortunately, the main drawbacks to routine use of MSCT in anthropology are the limited accessibility of such systems, their cost and the real need for the radiologist to be familiar with anthropological techniques.
To conclude, a multidisciplinary approach is crucial in such work, as it involves communication and data exchange between radiologists, forensic pathologists, anthropologists and radiographers.
Acknowledgments
ACKNOWLEDGMENTS
Sincere appreciation is expressed to Nina Crowte for her assistance in the preparation of this manuscript.
REFERENCES
- 1.Rutty GN, Brogdon G, Dedouit F, Grabherr S, Hatch GM, Jackowski C, et al. Terminology used in publications for post-mortem cross-sectional imaging. Int J Legal Med 2013; 127: 465–6. doi: 10.1007/s00414-012-0782-7 [DOI] [PubMed] [Google Scholar]
- 2.Dedouit F, Otal P, Costagliola R, Loubes Lacroix F, Telmon N, Rouge D, et al. Role of modern cross-sectional imaging in thanatology: a pictorial essay. [in French.] J Radiol 2006; 87: 619–38. [DOI] [PubMed] [Google Scholar]
- 3.Grabherr S, Doenz F, Steger B, Dirnhofer R, Dominguez A, Sollberger B, et al. Multi-phase post-mortem CT angiography: development of a standardized protocol. Int J Legal Med 2011; 125: 791–802. doi: 10.1007/s00414-010-0526-5 [DOI] [PubMed] [Google Scholar]
- 4.Dedouit F, Telmon N, Costagliola R, Otal P, Florence LL, Joffre F, et al. New identification possibilities with postmortem multislice computed tomography. Int J Legal Med 2007; 121: 507–10. doi: 10.1007/s00414-007-0200-8 [DOI] [PubMed] [Google Scholar]
- 5.Dedouit F, Auriol J, Rousseau H, Rougé D, Crubézy E, Telmon N. Age assessment by magnetic resonance imaging of the knee: a preliminary study. Forensic Sci Int 2012; 217:232. e1–7. doi: 10.1016/j.forsciint.2011.11.013 [DOI] [PubMed] [Google Scholar]
- 6.Saint-Martin P, Rerolle C, Dedouit F, Bouilleau L, Rousseau H, Rougé D, et al. Age estimation by magnetic resonance imaging of the distal tibial epiphysis and the calcaneum. Int J Legal Med 2013; 127: 1023–30. doi: 10.1007/s00414-013-0844-5 [DOI] [PubMed] [Google Scholar]
- 7.Beauthier JP. Traité de médecine légale. Bruxelles, Belgium: De Boeck; 2008. [Google Scholar]
- 8.Ciaffi R, Gibelli D, Cattaneo C. Forensic radiology and personal identification of unidentified bodies: a review. Radiol Med 2011; 116: 960–8. doi: 10.1007/s11547-011-0677-6 [DOI] [PubMed] [Google Scholar]
- 9.Pfaeffli M, Vock P, Dirnhofer R, Braun M, Bolliger SA, Thali MJ. Post-mortem radiological CT identification based on classical ante-mortem X-ray examinations. Forensic Sci Int 2007; 171: 111–17. doi: 10.1016/j.forsciint.2006.10.009 [DOI] [PubMed] [Google Scholar]
- 10.Sidler M, Jackowski C, Dirnhofer R, Vock P, Thali M. Use of multislice computed tomography in disaster victim identification—advantages and limitations. Forensic Sci Int 2007; 169: 118–28. doi: 10.1016/j.forsciint.2006.08.004 [DOI] [PubMed] [Google Scholar]
- 11.Brogdon BG. Forensic radiology. Boca Raton, FL: CRC Press; 1998. [Google Scholar]
- 12.Fischman SL. The use of medical and dental radiographs in identification. Int Dent J 1985; 35: 301–6. [PubMed] [Google Scholar]
- 13.Fischman SL. The identification process. Alpha Omegan 2002; 95: 13–16. [PubMed] [Google Scholar]
- 14.Kuehn CM, Taylor KM, Mann FA, Wilson AJ, Harruff RC. Validation of chest X-ray comparisons for unknown decedent identification. J Forensic Sci 2002; 47: 725–9. [PubMed] [Google Scholar]
- 15.Murphy WA, Spruill FG, Gantner GE. Radiologic identification of unknown human remains. J Forensic Sci 1980; 25: 727–35. [PubMed] [Google Scholar]
- 16.Ruder TD, Kraehenbuehl M, Gotsmy WF, Mathier S, Ebert LC, Thali MJ, et al. Radiologic identification of disaster victims: a simple and reliable method using CT of the paranasal sinuses. Eur J Radiol 2012; 81: e132–8. doi: 10.1016/j.ejrad.2011.01.060 [DOI] [PubMed] [Google Scholar]
- 17.Keats TE, Anderson MW. Atlas of normal roentgen variants that may simulate disease. 9th edn. Philadelphia, PA: Elsevier/Saunders, 2012. [Google Scholar]
- 18.Chhem R. Paleoradiology: imaging mummies and fossils. Berlin, Germany: Springer; 2008. [Google Scholar]
- 19.Komar D, Lathrop S. Frequencies of morphological characteristics in two contemporary forensic collections: implications for identification. J Forensic Sci 2006; 51: 974–8. doi: 10.1111/j.1556-4029.2006.00210.x [DOI] [PubMed] [Google Scholar]
- 20.Maret D, Peters OA, Dedouit F, Telmon N, Sixou M. Cone-Beam computed tomography: a useful tool for dental age estimation? Med Hypotheses 2011; 76: 700–2. doi: 10.1016/j.mehy.2011.01.039 [DOI] [PubMed] [Google Scholar]
- 21.Thali MJ, Markwalder T, Jackowski C, Sonnenschein M, Dirnhofer R. Dental CT imaging as a screening tool for dental profiling: advantages and limitations. J Forensic Sci 2006; 51: 113–19. doi: 10.1111/j.1556-4029.2005.00019.x [DOI] [PubMed] [Google Scholar]
- 22.Robinson C, Eisma R, Morgan B, Jeffery A, Graham EA, Black S, et al. Anthropological measurement of lower limb and foot bones using multi-detector computed tomography. J Forensic Sci 2008; 53: 1289–95. doi: 10.1111/j.1556-4029.2008.00875.x [DOI] [PubMed] [Google Scholar]
- 23.Verhoff MA, Ramsthaler F, Krähahn J, Deml U, Gille RJ, Grabherr S, et al. Digital forensic osteology—possibilities in cooperation with the Virtopsy project. Forensic Sci Int 2008; 174: 152–6. doi: 10.1016/j.forsciint.2007.03.017 [DOI] [PubMed] [Google Scholar]
- 24.Bass WM, Missouri Archaeological Society. Human osteology: a laboratory and field manual. 5th edn. Columbia, MO: Missouri Archaeological Society; 2005. [Google Scholar]
- 25.Ubelaker DH. Human skeletal remains: excavation, analysis, interpretation. Chicago, IL: Aldine Publishing; 1978. [Google Scholar]
- 26.McCormick WF, Stewart JH, Langford LA. Sex determination from chest plate roentgenograms. Am J Phys Anthropol 1985; 68: 173–95. [DOI] [PubMed] [Google Scholar]
- 27.Giles E, Elliot O. Sex determination by discriminant function analysis of crania. Am J Phys Anthropol 1963; 21: 53–68. [DOI] [PubMed] [Google Scholar]
- 28.Dang-Tran KD, Dedouit F, Joffre F, Rougé D, Rousseau H, Telmon N. Thyroid cartilage ossification and multislice computed tomography examination: a useful tool for age assessment? J Forensic Sci 2010; 55: 677–83. doi: 10.1111/j.1556-4029.2010.01318.x [DOI] [PubMed] [Google Scholar]
- 29.Uysal S, Gokharman D, Kacar M, Tuncbilek I, Kosa U. Estimation of sex by 3D CT measurements of the foramen magnum. J Forensic Sci 2005; 50: 1310–14. [PubMed] [Google Scholar]
- 30.Bookstein FL. Morphometric tools for landmark data: geometry and biology. Cambridge, England/New York, NY: Cambridge University Press; 1991. [Google Scholar]
- 31.Slice DE. Modern morphometrics in physical anthropology. New York, NY: Kluwer Academic/Plenum Publishers; 2005. [Google Scholar]
- 32.Zelditch M. Geometric morphometrics for biologists: a primer. Amsterdam, Netherlands: Elsevier Academic Press; 2004. [Google Scholar]
- 33.Bilfeld MF, Dedouit F, Rousseau H, Sans N, Braga J, Rougé D, et al. Human coxal bone sexual dimorphism and multislice computed tomography: geometric morphometric analysis of 65 adults. J Forensic Sci 2012; 57: 578–88. doi: 10.1111/j.1556-4029.2011.02009.x [DOI] [PubMed] [Google Scholar]
- 34.Bilfeld MF, Dedouit F, Sans N, Rousseau H, Rougé D, Telmon N. Ontogeny of size and shape sexual dimorphism in the ilium: a multislice computed tomography study by geometric morphometry. J Forensic Sci 2013; 58: 303–10. doi: 10.1111/1556-4029.12037 [DOI] [PubMed] [Google Scholar]
- 35.Simpson DE, Dontu VS, Stephens SE, Archbold LJ, Lowe V, O'Doherty MJ, et al. Large variations occur in bone density measurements of children when using different software. Nucl Med Commun 2005; 26: 483–7. [DOI] [PubMed] [Google Scholar]
- 36.Brogdon BG. Scope of forensic radiology. Crit Rev Diagn Imaging 2000; 41: 43–67. [PubMed] [Google Scholar]
- 37.Scheuer L, Black SM. The juvenile skeleton. Amsterdam, Netherlands: Elsevier Academic Press; 2004. [Google Scholar]
- 38.Sauvegrain J, Nahum H, Bronstein H. Study of bone maturation of the elbow. [in French.] Ann Radiol (Paris) 1962; 5: 542–50. [PubMed] [Google Scholar]
- 39.Sauvegrain J, Nahum H, Carle F. Bone maturation. Importance of the determination of the bone age. Methods of evaluation (general review). [in French.] Ann Radiol (Paris) 1962; 5: 535–41. [PubMed] [Google Scholar]
- 40.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2nd edn. Stanford, CA: Stanford University Press; 1959. [Google Scholar]
- 41.Pyle SI, Hoerr NL. A radiographic standard of reference for the growing knee. Springfield, IL: CC Thomas; 1969. [Google Scholar]
- 42.Fazekas IG, Kâosa F. Forensic fetal osteology. Budapest, Hungary: Akadâemiai Kiadâo; 1978. [Google Scholar]
- 43.Maresh MM. Variations in patterns of linear growth and skeletal maturation. Phys Ther 1964; 44: 881–90. [PubMed] [Google Scholar]
- 44.Adalian P, Piercecchi-Marti MD, Bourliere-Najean B, Panuel M, Fredouille C, Dutour O, et al. Postmortem assessment of fetal diaphyseal femoral length: validation of a radiographic methodology. J Forensic Sci 2001; 46: 215–19. [PubMed] [Google Scholar]
- 45.Adalian P, Piercecchi-Marti MD, Bourliére-Najean B, Panuel M, Leonetti G, Dutour O. New formula for the determination of fetal age. [In French]. C R Biol 2002; 325: 261–9. [DOI] [PubMed] [Google Scholar]
- 46.Dedouit F, Telmon N, Guilbeau-Frugier C, Gainza D, Otal P, Joffre F, et al. Virtual autopsy and forensic identification-practical application: a report of one case. J Forensic Sci 2007; 52: 960–4. doi: 10.1111/j.1556-4029.2007.00475.x [DOI] [PubMed] [Google Scholar]
- 47.Grabherr S, Cooper C, Ulrich-Bochsler S, Uldin T, Ross S, Oesterhelweg L, et al. Estimation of sex and age of “virtual skeletons”—a feasibility study. Eur Radiol 2009; 19: 419–29. doi: 10.1007/s00330-008-1155-y [DOI] [PubMed] [Google Scholar]
- 48.Barrier P, Dedouit F, Braga J, Joffre F, Rougé D, Rousseau H, et al. Age at death estimation using multislice computed tomography reconstructions of the posterior pelvis. J Forensic Sci 2009; 54: 773–8. doi: 10.1111/j.1556-4029.2009.01074.x [DOI] [PubMed] [Google Scholar]
- 49.Dedouit F, Bindel S, Gainza D, Blanc A, Joffre F, Rougé D, et al. Application of the Iscan method to two- and three-dimensional imaging of the sternal end of the right fourth rib. J Forensic Sci 2008; 53: 288–95. doi: 10.1111/j.1556-4029.2007.00642.x [DOI] [PubMed] [Google Scholar]
- 50.Telmon N, Gaston A, Chemla P, Blanc A, Joffre F, Rougé D. Application of the Suchey-Brooks method to three-dimensional imaging of the pubic symphysis. J Forensic Sci 2005; 50: 507–12. [PubMed] [Google Scholar]
- 51.Moskovitch G, Dedouit F, Braga J, Rougé D, Rousseau H, Telmon N. Multislice computed tomography of the first rib: a useful technique for bone age assessment. J Forensic Sci 2010; 55: 865–70. doi: 10.1111/j.1556-4029.2010.01390.x [DOI] [PubMed] [Google Scholar]
- 52.Schulz R, Muhler M, Mutze S, Schmidt S, Reisinger W, Schmeling A. Studies on the time frame for ossification of the medial epiphysis of the clavicle as revealed by CT scans. Int J Legal Med 2005; 119: 142–5. doi: 10.1007/s00414-005-0529-9 [DOI] [PubMed] [Google Scholar]
- 53.Schulze D, Rother U, Fuhrmann A, Richel S, Faulmann G, Heiland M. Correlation of age and ossification of the medial clavicular epiphysis using computed tomography. Forensic Sci Int 2006; 158: 184–9. doi: 10.1016/j.forsciint.2005.05.033 [DOI] [PubMed] [Google Scholar]
- 54.Schaefer M, Scheuer L, Black SM. Juvenile osteology: a laboratory and field manual. London, UK: Academic Press; 2009. [Google Scholar]
- 55.Schour I, Massler M. Rate and gradient of growth in human deciduous teeth with special reference to neonatal ring. J Dent Res 1937; 16: 349–50. [Google Scholar]
- 56.Moorrees CF. Dental development—a growth study based on tooth eruption as a measure of physiologic age. Rep Congr Eur Orthod Soc 1964; 40: 92–106. [PubMed] [Google Scholar]
- 57.Moorrees CF, Fanning EA, Hunt EE Jr. Age variation of formation stages for ten permanent teeth. J Dent Res 1963; 42: 1490–502. [DOI] [PubMed] [Google Scholar]
- 58.Moorrees CF, Fanning EA, Hunt EE Jr. Formation and resorption of three deciduous teeth in children. Am J Phys Anthropol 1963; 21: 205–13. [DOI] [PubMed] [Google Scholar]
- 59.Demirjian A. Dental development: index of physiologic maturation. [In French.] Med Hyg (Geneve) 1978; 36: 3154–9. [PubMed] [Google Scholar]
- 60.Demirjian A. Dental development: an index of physiological maturity. [In French.] Union Med Can 1980; 109: 832–9. [PubMed] [Google Scholar]
- 61.Demirjian A, Goldstein H. New systems for dental maturity based on seven and four teeth. Ann Hum Biol 1976; 3: 411–21. [DOI] [PubMed] [Google Scholar]
- 62.Willems G. A review of the most commonly used dental age estimation techniques. J Forensic Odontostomatol 2001; 19: 9–17. [PubMed] [Google Scholar]
- 63.Willems G, Van Olmen A, Spiessens B, Carels C. Dental age estimation in Belgian children: Demirjian's technique revisited. J Forensic Sci 2001; 46: 893–5. doi: 10.1016/j.forsciint.2006.02.019 [DOI] [PubMed] [Google Scholar]
- 64.Mincer HH, Harris EF, Berryman HE. The A.B.F.O. study of third molar development and its use as an estimator of chronological age. J Forensic Sci 1993; 38: 379–90. doi: 10.1016/j.forsciint.2004.09.021 [DOI] [PubMed] [Google Scholar]
- 65.Howells WW. Criteria for selection of osteometric dimensions. Am J Phys Anthropol 1969; 30: 451–7. [DOI] [PubMed] [Google Scholar]
- 66.Krogman WM, Iscan MY. The human skeleton in forensic medicine. 2nd edn Springfield, IL: CC Thomas; 1986. [Google Scholar]
- 67.Kallenberger L, Pilbrow V. Using CRANID to test the population affinity of known crania. J Anat 2012; 221: 459–64. doi: 10.1111/j.1469-7580.2012.01558.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dedouit F, Géraut A, Baranov V, Ludes B, Rougé D, Telmon N, et al. Virtual and macroscopical studies of mummies—differences or complementarity? Report of a natural frozen Siberian mummy. Forensic Sci Int 2010; 200: e7–13. doi: 10.1016/j.forsciint.2010.03.028 [DOI] [PubMed] [Google Scholar]
- 69.Fully G. New method of determination of the height. [In French.] Ann Med Leg Criminol Police Sci Toxicol 1956; 36: 266–73. [PubMed] [Google Scholar]
- 70.Raxter MH, Auerbach BM, Ruff CB. Revision of the Fully technique for estimating statures. Am J Phys Anthropol 2006; 130: 374–84. doi: 10.1002/ajpa.20361 [DOI] [PubMed] [Google Scholar]
- 71.Gardner JC, Garvin G, Nelson AJ, Vascotto G, Conlogue G. Paleoradiology in mummy studies: the Sulman mummy project. Can Assoc Radiol J 2004; 55: 228–34. [PubMed] [Google Scholar]
- 72.Chan SS, Elias JP, Hysell ME, Hallowell MJ. CT of a Ptolemaic period mummy from the ancient Egyptian City of Akhmim. Radiographics 2008; 28: 2023–32. doi: 10.1148/rg.287085039 [DOI] [PubMed] [Google Scholar]
- 73.Cesarani F, Martina MC, Ferraris A, Grilletto R, Boano R, Marochetti EF, et al. Whole-body three-dimensional multidetector CT of 13 Egyptian human mummies. AJR Am J Roentgenol 2003; 180: 597–606. doi: 10.2214/ajr.180.3.1800597 [DOI] [PubMed] [Google Scholar]
- 74.Trotter M, Gleser GC. A re-evaluation of estimation of stature based on measurements of stature taken during life and of long bones after death. Am J Phys Anthropol 1958; 16: 79–123. [DOI] [PubMed] [Google Scholar]
- 75.Prosser I, Maguire S, Harrison SK, Mann M, Sibert JR, Kemp AM. How old is this fracture? Radiologic dating of fractures in children: a systematic review. AJR Am J Roentgenol 2005; 184: 1282–6. doi: 10.2214/ajr.184.4.01841282 [DOI] [PubMed] [Google Scholar]
- 76.Kleinman PK. Diagnostic imaging of child abuse. 2nd edn. St Louis, MO: Mosby; 1998. [Google Scholar]
- 77.Adamsbaum C, Méjean N, Merzoug V, Rey-Salmon C. How to explore and report children with suspected non-accidental trauma. Pediatr Radiol 2010; 40: 932–8. doi: 10.1007/s00247-010-1591-0 [DOI] [PubMed] [Google Scholar]
- 78.Madea B, Staak M. Determination of the sequence of gunshot wounds of the skull. J Forensic Sci Soc 1988; 28: 321–8. [DOI] [PubMed] [Google Scholar]
- 79.Viel G, Gehl A, Sperhake JP. Intersecting fractures of the skull and gunshot wounds. Case report and literature review. Forensic Sci Med Pathol 2009; 5: 22–7. doi: 10.1007/s12024-008-9062-8 [DOI] [PubMed] [Google Scholar]
- 80.Knight B, Knight BF, Saukko PJ. Knight's forensic pathology. 3rd edn. London, UK: Arnold; 2004. [Google Scholar]
- 81.Guyomarc'h P, Campagna-Vaillancourt M, Kremer C, Sauvageau A. Discrimination of falls and blows in blunt head trauma: a multi-criteria approach. J Forensic Sci 2010; 55: 423–7. doi: 10.1111/j.1556-4029.2009.01310.x [DOI] [PubMed] [Google Scholar]
- 82.Kremer C, Racette S, Dionne CA, Sauvageau A. Discrimination of falls and blows in blunt head trauma: systematic study of the hat brim line rule in relation to skull fractures. J Forensic Sci 2008; 53: 716–19. [DOI] [PubMed] [Google Scholar]
- 83.Kremer C, Sauvageau A. Discrimination of falls and blows in blunt head trauma: assessment of predictability through combined criteria. J Forensic Sci 2009; 54: 923–6. doi: 10.1111/j.1556-4029.2009.01072.x [DOI] [PubMed] [Google Scholar]
- 84.Andenmatten MA, Thali MJ, Kneubuehl BP, Oesterhelweg L, Ross S, Spendlove D, et al. Gunshot injuries detected by post-mortem multislice computed tomography (MSCT): a feasibility study. Leg Med (Tokyo) 2008; 10: 287–92. doi: 10.1016/j.legalmed.2008.03.005 [DOI] [PubMed] [Google Scholar]
- 85.Harcke HT, Levy AD, Abbott RM, Mallak CT, Getz JM, Champion HR, et al. Autopsy radiography: digital radiographs (DR) vs multidetector computed tomography (MDCT) in high-velocity gunshot-wound victims. Am J Forensic Med Pathol 2007; 28: 13–19. doi: 10.1097/01.paf.0000257419.92109.ce [DOI] [PubMed] [Google Scholar]
- 86.Harcke HT, Levy AD, Getz JM, Robinson SR. MDCT analysis of projectile injury in forensic investigation. AJR Am J Roentgenol 2008; 190: W106–11. doi: 10.2214/AJR.07.2754 [DOI] [PubMed] [Google Scholar]
- 87.Levy AD, Abbott RM, Mallak CT, Getz JM, Harcke HT, Champion HR, et al. Virtual autopsy: preliminary experience in high-velocity gunshot wound victims. Radiology 2006; 240: 522–8. doi: 10.1148/radiol.2402050972 [DOI] [PubMed] [Google Scholar]
- 88.Oehmichen M, Gehl HB, Meissner C, Petersen D, Hoche W, Gerling I, et al. Forensic pathological aspects of postmortem imaging of gunshot injury to the head: documentation and biometric data. Acta Neuropathol 2003; 105: 570–80. doi: 10.1007/s00401-003-0683-4 [DOI] [PubMed] [Google Scholar]
- 89.Schnider J, Thali MJ, Ross S, Oesterhelweg L, Spendlove D, Bolliger SA. Injuries due to sharp trauma detected by post-mortem multislice computed tomography (MSCT): a feasibility study. Leg Med (Tokyo) 2009; 11: 4–9. doi: 10.1016/j.legalmed.2008.07.001 [DOI] [PubMed] [Google Scholar]
- 90.Haglund WD, Sorg MH. Forensic taphonomy: the postmortem fate of human remains. Boca Raton, FL: CRC Press; 1997. [Google Scholar]
- 91.Dedouit F, Loubes-Lacroix F, Costagliola R, Guilbeau-Frugier C, Alengrin D, Otal P, et al. Post-mortem changes of the middle ear: multislice computed tomography study. Forensic Sci Int 2008; 175: 149–54. doi: 10.1016/j.forsciint.2007.06.004 [DOI] [PubMed] [Google Scholar]
- 92.Dedouit F, Gainza D, Franchitto N, Joffre F, Rousseau H, Rougé D, et al. Radiological, forensic, and anthropological studies of a concrete block containing bones. J Forensic Sci 2011; 56: 1328–33. doi: 10.1111/j.1556-4029.2011.01742.x [DOI] [PubMed] [Google Scholar]