Abstract
Although poor parenting practices place youth living in under resourced communities at heightened risk for adjustment difficulties, less is known about what influences parenting practices in those communities. The present study examines prospective linkages between three latent constructs: parental strain, mental health problems and parenting practices. Parental victimization by community violence and life stressors were indicative of parental strain; depressive, anxious, and hostile symptoms were indicators of parental mental health; and parental knowledge of their child's activities and child disclosure were indicators of parenting practices. Interviews were conducted annually for 3 waves with 316 female caregivers (92% African American) parenting youth in low-income inner-city communities. Structural equation modeling revealed that parental strain, assessed at Wave 1, predicted changes in mental health problems one year later, which in turn predicted parenting practices at Wave 3. These results suggest that parental strain can compromise a caregiver's ability to parent effectively by impacting their mental health. Opportunities for intervention include helping caregivers process trauma and mental health problems associated with parental strain.
Keywords: African American female caregivers, parental strain, mental health, parenting
Parenting children in high-risk contexts is the common experience for millions of adults living in the United States (Ceballo, Kennedy, Bregman,& Epstein-Ngo, 2012). Living in high-risk contexts, such as neighborhoods with high levels of violence, noise, and crowding can take a toll on parenting practices, ranging from excessive and restrictive control of children's activities (Weir, Etelson, & Brand, 2006) to various forms of mistreatment and abuse (Zhang, & Anderson, 2010). These alterations in parenting and family processes, in turn, can impact youth adjustment (White & Roosa, 2012). Due to the significant effect parenting behavior has on children's development (Furstenberg, Cook, Eccles, Elder, & Sameroff, 1999; Sroufe, Egeland, Carlson, & Collins, 2005) ), it is important to understand the pathways through which parents' own experiences in hazardous neighborhoods impact their parenting practices. The present study examines prospective linkages between three latent constructs: parental strain, assessed through victimization by community violence and life stressors; parental mental health, assessed through depressive, anxious and hostile symptoms; and subsequent parenting practices assessed through parental knowledge of their child's activities and child voluntary disclosure of activities (see Figure 1).
Figure 1.
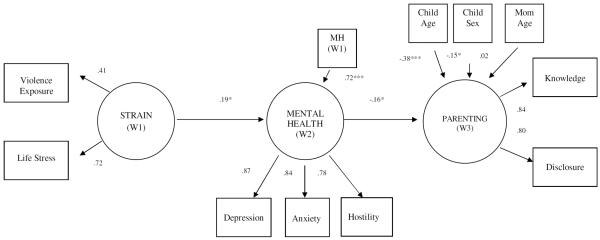
Structural model with standardized estimates. MH = Mental Health. W1 = Wave 1. W2 = Wave 2. W3 = Wave 3. * p < .05; ** p < .01; *** p < .001.
Parental Strain, Mental health and Parenting Practices
Neighborhood poverty can negatively impact parenting: it can affect the nature and extent of stressors to which parents are exposed, parental coping strategies, parental health, and the extent to which parents are warm and responsive to their children (Ernst, 2001; Klebanov, Brooks-Gunn, & Duncan, 1994). Many impoverished neighborhoods also are filled with danger and violence, including drug dealing, gang activity, robberies, and assaults. Although exposure to this type of community violence has documented effects on the well-being of youth (see Fowler et al., 2009, for a review), less is known about how parents' exposure to community violence and the life stressors that co-occur in these environments may affect their mental health (Franco, Pottick, & Huang, 2010; Klebanov et al., 1994; McDonell, 2007), which in turn affects their parenting practices.
Research supports the relation between parental exposure to community violence, compromised coping, and subsequent mental health problems (Aisenberg, 2001; Kliewer & Zaharakis, 2013; Weir et al., 2006). In general parents raising their children in communities where the sense of safety is compromised and crime is prevalent tend to present higher levels of anxiety regarding neighborhood safety (Kliewer, in press) and are at higher risk for depression compared to parents raising their children in communities where the sense of safety is not compromised. Certainly poverty and community violence contribute to the context of parenting. Parents' direct or indirect exposure to community violence contributes to mental health problems like anxiety, depression, and hostility; all of which have the potential to affect a parent's ability to effectively monitor and connect with their child (Aisenberg, 2001; McLoyd, 1998; Ross, 2000; Wandersman & Nation, 1998). As noted by Kotchick and Forehand (2002), parenting practices that include adequate monitoring and supervision of children's activities serve as protective factors for children growing up in neighborhoods characterized by poverty and danger. Adequate parental monitoring of child activities has been identified as an essential parenting skill that relates to better youth adjustment (Kerr & Stattin, 2000), and parental monitoring builds upon both parental knowledge and child's disclosure. Stattin and Kerr (2000) described how adequate parental monitoring involves parental solicitation of information as well as parental control, and/or voluntary child disclosure of information. These factors contribute to parental knowledge of the child's activities and whereabouts.
Because closeness to parents decreases while the importance of peers increase as children transition from childhood to adolescence, promoting voluntary child disclosure of information is key for optimizing parents' monitoring efforts (Kerr & Stattin, 2000). Furthermore, a child's voluntary disclosure of information is associated with parental acceptance, responsiveness and warmth in the parent–child relationship (Blodgett-Salafia, Gondoli, & Grundy, 2009; Smetana, Metzger, Gettman, & Campione-Barr, 2006), and all these factors are related to youth adjustment (Scott et al., 2011). These data suggest that a better understanding of the factors that influence parenting practices, such as parental monitoring in under resourced communities, have important implications for enhancing optimal parenting.
Evidence suggests that in an effort to better protect their children, parents living in violent neighborhoods adapt their parenting strategies. For example, in response to community violence, parental awareness of their child's whereabouts increases, leading to higher monitoring and an increase in communication with children about safety issues (Ceballo et al., 2012; Kimbro & Schachter, 2011; Letiecq & Koblinsky, 2004). Nevertheless, parental efforts to protect their children do not guarantee effective parenting practices; for instance, Byrnes, Miller, Chen, and Grube (2011) found that mothers who perceived higher levels of neighborhood problems used more rule-setting strategies, but also showed lower levels of awareness regarding their children's whereabouts, indicating evidence of less effective monitoring strategies.
Exposure to community violence – directly or indirectly – is stressful, and not all parents cope adaptively with this exposure. Echoing work cited earlier, Pinderhughes et al. (2001) noted that the chronic stress faced by parents living in neighborhoods characterized by limited economic resources and public services, and high violence and crime rates, may impact a parent's ability to be warm, appropriate, consistent, and non-harsh. Along those lines, White and Roosa (2012) in their study with Mexican American fathers and adolescents found that neighborhood danger was associated with disruptions in parenting and family processes, which in turn led to elevated levels of internalizing symptoms for the youth.
Some work exists linking exposure to violence and life stressors to psychological vulnerability and disciplinary practices among African American women (Jarrett & Jefferson, 2004; Jenkins, 2002; Mitcell et al, 2010). However, to our knowledge this is the first study that examines the prospective relations between parental strain, mental health, and parenting practices measured by parental knowledge and children voluntary disclosure of information.
The present study augments the literature on influences on parenting practices in underresourced neighborhoods by testing a longitudinal model linking parental strain (exposure to violence and life stressors), parent mental health problems (depressive, anxious, and hostile symptoms), and parenting practices (parental knowledge and child disclosure). It is hypothesized that parental strain would affect their parenting practices indirectly via mental health problems. That is, parents' exposure to violence and experience of life stress would be positively and prospectively associated with mental health problems, which in turn would be associated with lower levels of parental knowledge and child disclosure.
Method
Participants
Participants included 316 female caregivers (M = 39.42 yrs, SD = 7.62; range = 23–67; 91.8% African American) enrolled with one of their children in a longitudinal study of community violence exposure, coping, and adjustment. Most (87.1%) caregivers were the biological mother of a child also enrolled in the study; adopted mothers (2.2%), stepmothers (0.9%), grandmothers (6.3%), father's girlfriends (0.3%) and other female relatives (3.2%) also participated. All caregivers will be referred to as “parents” hereafter. Youth in the study ranged in age from 10 to 17 (M = 13.10 yrs, SD = 1.63) and 47% were male. Most (39.4%) of these women had never married, 33.4% were married or cohabitating, 25.2% were separated or divorced, and 1.9% were widowed. Approximately a quarter of the sample (23.1%) had not completed high school. Another 27.9% completed high school or earned a general education degree (GED), 25.0% had some college, and 24.0% had a vocational degree, associate's degree or higher. Approximately half of the sample had household incomes of $400/week or less; 30% of the sample had household incomes of $601 per week or more.
Measures
Strain
Strain was assessed at baseline with a two measures: victimization by community violence and life stressors. Parent victimization (10 items; e.g., been threatened with serious physical harm) was assessed with Richters and Saltzman's (1990) Survey of Exposure to Community Violence. Parents reported on their lifetime exposure using a scale from (0) never to (4) every day. Richters and Saltzman's (1990) measure has been widely used and validated. Stressors were assessed with the 20-item Life Stress Scale that taps a variety of life stressors that adults may have experienced in the past year. A sample item is “Have you had a loss of income?” This measure has been used in the Multisite Violence Prevention Project (Miller-Johnson, Sullivan, Simon, & Multisite Violence Prevention Project, 2004). Respondents rated each item on a 3-point scale (“0 = did not occur”, “1 = caused minor stress”, or “2 = caused major stress”). Item scores were averaged to obtain a mean severity rating, with high scores reflecting higher levels of stress. The victimization and stressor measure were used as manifest indicators of the latent construct Strain.
Mental health problems
Parent mental health problems were reported at the first and second wave of the study using anxiety (6 items; e.g., “nervousness or shakiness inside”), depression (6 items; e.g., “feeling hopeless about the future”), and hostility (5 items; e.g., “feeling easily annoyed or irritated”) subscales of the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983). Items are rated on a 5-point scale from (1) not at all to (5) extremely, with higher scale scores indicating higher symptom levels.The BSI, a brief form of the Symptom Checklist (SCL-90), is a valid and reliable measure of symptomatology (Derogatis & Melisaratos, 1983). Cronbach alphas in the current sample were .87 and .86 for depressive symptoms at waves 1 and 2; .81 and .82 for anxious symptoms at waves 1 and 2; and .75 and .74 for hostility at waves 1 and 2.
Parenting practices
Parent parenting practices were self reported at Wave 3 using the parental knowledge (9 items) and child disclosure (5 items) subscales of Kerr and Stattin's parenting measure (Stattin & Kerr, 2000). The parental knowledge scale assesses information parents have about their child's activities (i.e., where they are, what they are doing, and who they are with). The child disclosure scale assesses the extent to which children volunteer information about their activities to their parents (e.g., “does your child usually tell you how school was when s/he gets home [how s/he did on different exams, his/her relationships with teachers, etc.”]?) Items are rated on a 5-point scale and reverse coded so that higher values indicate greater knowledge or disclosure. Kerr and Stattin (2000; Stattin & Kerr, 2000) report adequate internal consistencies and good validity of the measure. Cronbach alphas in the current sample were .85 for parental knowledge and .78 for child disclosure.
Procedures
Participants were recruited from neighborhoods within (city and state blinded for review) and the neighboring counties with high levels of violence and/or poverty according to police statistics and 2000 census data. The study was advertised through community agencies and events, and by canvassing qualifying neighborhoods via flyers posted door-to-door. Interviews were scheduled annually for four waves, and were conducted primarily in participants' homes by trained research staff. It was never the case than more than one child in the household was eligible to participate in the study, thus parents always reported on the child participating in the study. Sixty-three percent of eligible participants agreed to be in the study, which is consistent with studies using similar designs and populations. Sixty nine percent of the original sample retained across the entire study. Only data from parents collected during the 2nd, 3rd, and 4th waves is used in the current study because data on parent exposure to violence was not collected in Wave 1. However, to reduce confusion we refer to data in the current study as Waves 1, 2 and 3. Interviewers thoroughly reviewed the parent consent forms with the family. A Certificate of Confidentiality was obtained from the National Institutes of Health (NIH) to protect families' responses. Tests for the effects of interviewer race and gender revealed no systematic biases, ps > .10. Interviews lasted approximately 2.5 h and participants received $50 in gift cards per family at each wave.
Results
Attrition analyses
Participants who completed two waves of data were compared with participants who were missing the final wave of data on victimization, life stressors, and mental health problems. There were no significant differences on any of the t-tests (ps > .10) indicating no systematic biases in attrition.
Descriptive information on the study variables
Table 1 presents descriptive information on and correlations among the study variables. As seen in the table, both victimization and life stressors, assessed at baseline, were associated with concurrent and future mental health symptoms. Depressive and anxious symptoms were significantly associated with lower levels of parental knowledge and child disclosure the following year; hostility was not prospectively associated with parenting behaviors. Child age (not shown in Table 1) was associated with lower levels of parental knowledge (r = −.30, p< .001) and child disclosure (r = -.29, p< .001). Parents reporting knowing less about the activities of sons (M = 37.42, SD = 5.87) than daughters (M = 39.08, SD = 5.06), t(244) = 2.37, p< .05. Child disclosure did not differ by gender, t(244) = 1.58, n.s. Parent age was not associated with parental knowledge (r = −.02) or child disclosure (r = .01).
Table 1.
Descriptive Information on and Correlations Among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Victimization (W1) | -- | .30*** | .16** | .20*** | .17*** | .18*** | .27*** | .26*** | −.01 | .01 |
| 2. Life stressors (W1) | -- | .38*** | .33*** | .29*** | .31*** | .30*** | .36*** | −.07 | −.08 | |
| 3. Depressive sym (W1) | -- | .69*** | .65*** | .53*** | .57*** | .46*** | −.09 | −.10 | ||
| 4. Depressive sym (W2) | -- | .51*** | .74*** | .46*** | .65*** | −.14* | −.14* | |||
| 5. Anxious sym (W1) | -- | .60*** | .60*** | .45*** | −.07 | −.03 | ||||
| 6. Anxious sym(W2) | -- | .45*** | .68*** | −.16* | −.15* | |||||
| 7. Hostility (W1) | -- | .59*** | −.05 | −.07 | ||||||
| 8. Hostility (W2) | -- | −.11 | −.10 | |||||||
| 9. Knowledge (W3) | -- | .68*** | ||||||||
| 10. Child disclosure (W3) | -- | |||||||||
| M | 3.94 | 8.28 | 9.22 | 8.73 | 9.04 | 8.96 | 7.87 | 7.76 | 38.35 | 20.31 |
| SD | 3.77 | 5.28 | 4.17 | 3.84 | 3.58 | 3.70 | 3.04 | 3.12 | 5.47 | 3.86 |
Note. W1 = Wave 1; W2 = Wave 2; W3 = Wave 3.
p < .05;
p < .01;
p < .001.
Structural equation model testing main hypotheses
The main study hypotheses were tested using a structural equation model in Mplus 6.11 (Muthen& Muthen, 2010). As seen in Figure 1, paths were specified from the latent construct of strain, assessed at baseline, to the latent construct of mental health symptoms, assessed one year later, to the latent construct of parenting assessed at the final wave. Baseline levels of mental health symptoms as well as child age, child gender, and parent age were controlled in the analyses. The model fit the data adequately (N = 316, X2 (36) = 82.23, p< .001; RMSEA = .064; CFI = .945). As seen in Figure 1, strain was associated with increases in mental health symptoms over time, which in turn was associated with lower levels of parental knowledge and child disclosure.
Discussion
Living in under resourced communities can be challenging for both parents and youth. While there is ample information regarding the effects of exposure to violence on youth, less is known about its effects on parents' mental health and/or parenting practices. Researchers have shown that parental experiences can impact parenting style and therefore the quality of the parent-child relationship. The present longitudinal study explored pathways between parental strain at year one, subsequent changes in parental mental health at year two, and general quality of parenting practices as assessed by parental knowledge and child disclosure at year three.
Maternal experiences of victimization and life stress were associated with changes in mental health problems one year later. Our data are consistent with that of Jordan, Campbell, and Follingstad (2010), who reported a relationship between experiences of victimization and subsequent PTSD, anxiety and depression among women, all negatively associated with quality of parenting. These results add to the evidence supporting the importance of addressing parental victimization experiences in prevention efforts, especially when taking into account the noted links between exposure to community violence and aggressive parenting practices (Zhang, & Anderson, 2010), which are known to be harmful to children's well-being and are related to aggressive child behaviors (Zhang, & Eamon, 2011). Indeed, poor maternal health consistently is linked to children's negative outcomes (Boyd & Waanders, 2013; Goodman, 2007), and harsh parenting is associated with increased relational aggression among youth (Kawabata, Alink, Tseng, IJzendoorn, & Crick, 2011) and children's academic problems (Barry, Lochman, Fite, Wells, & Colder, 2012).
Our results also showed that parents' mental health symptoms were significantly associated with lower levels of parental knowledge and child disclosure the following year. These results are important since they provide evidence that the impact of parental strain on mental health can influence parental behaviors beyond disciplinary practices. As noted earlier, parents' ability to adequately monitor their children's activities and whereabouts is a key protective factor that relates to better youth adjustment (Kerr & Stattin, 2000). Perhaps the elevated levels of depressive, anxious, and hostile symptoms observed among parents limited their ability to connect with their children and to instill the feeling of trust and confidence needed to promote children's voluntary disclosure of information. Moreover, it is likely that parents who are dealing with depression and anxiety are less effective at soliciting information and/or tracking their children's activities which impacts their parental knowledge.
Study Limitations
Although the present study contributes to an understanding of the prospective relations among parental strain, mental health problems, and parenting practices in a difficult to recruit sample of largely minority parents, some study limitations should be noted. First, information on the number of years parents resided in their neighborhood was not systematically collected; therefore this information could not be used in the present analysis. Second, the present study relies completely on parental self-report. Inclusion of data from other sources would strengthen the study findings. Third, the study focused on maternal perspectives. Although many of the participating parents were not partnered, future studies should attempt to include the perspectives of social or biological fathers if feasible, especially given the reported influence of African American fathers in the lives of at-risk youth (Caldwell et al., 2014; Mandara & Murray,2006; Rodney & Mupier,1999).
Study Implications
The present results highlight the relevance of improving community conditions, social support, and other resources that can contribute to reduced parental strain. For instance, Mapp (2006) stated that it is not as much parental strain that impacts parenting practices, but rather parents' ability to resolve the trauma associated with taxing life experiences. Indeed, even among families faced with considerable environmental risk, there is ample evidence that social support from family and friends can buffer the effects of this risk on parenting (Anderson, 2008; Cochran & Walker, 2005; Marshall, Noonan, McCartney, Marx, & Keefe, 2001). In addition, efforts should be oriented towards minimizing parental victimization experiences, helping parents to process past trauma experiences, and increasing and strengthening parents' social support networks for those living in under resourced neighborhoods, as mental health and parenting practices can be negatively affected by parental strain. Hence, there is an urgent need for evidence-based parenting programs that address the impact of parental strain on mental health and parenting.
Highlights
Parental strain influenced parenting through changes in parental mental health
Parental strain was associated with concurrent and future mental health symptoms
Changes in parent mental health influenced parental knowledge and child disclosure
Acknowledgements
This study was supported by National Institutes of Health grants R21DA020086-02 and K01DA015442-01A1 awarded to Wendy Kliewer. We thank the many students and staff members who worked on Project COPE as well as the families who shared their lives with us over the course of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aisenberg E. The effects of exposure to community violence upon Latina mothers and preschool children. Hispanic Journal of Behavioral Sciences. 2001;23:378–398. doi: 10.1177/0739986301234003. [Google Scholar]
- Anderson LS. Predictors of parenting stress in a diverse sample of parents of early adolescents in high-risk communities. Nursing Research. 2008;57:340–350. doi: 10.1097/01.NNR.0000313502.92227.87. doi:10.1097/01.NNR.0000313502.92227.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry TD, Lochman JE, Fite PJ, Wells KC, Colder CR. The influence of neighborhood characteristics and parenting practices on academic problems and aggression outcomes among moderately to highly aggressive children. Journal of Community Psychology. 2012;40:372–379. [Google Scholar]
- Blodgett-Salafia EH, Gondoli DM, Grundy AM. The longitudinal interplay of maternal warmth and adolescents' self-disclosure in predicting maternal knowledge. Journal of Research on Adolescence. 2009;19:654–668. [Google Scholar]
- Boyd RC, Waanders C. Protective Factors for Depression Among African American Children of Predominantly Low-Income Mothers with Depression. Journal of Child and Family Studies. 2013;22:85–95. doi: 10.1007/s10826-012-9588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes HF, Miller BA, Chen MJ, Grube JW. The roles of mothers'neighborhood perceptions and specific monitoring strategies in youths' problem behavior. Journal of Youth Adolescence. 2011;40:347–360. doi: 10.1007/s10964-010-9538-1. doi: 10.1007/s10964-010-9538-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell CH, Antonakos CL, Assari S, Kruger D, De Loney EH, Njai R. Pathways to prevention: Improving nonresident African American fathers' parenting skills and behaviors to reduce sons' aggression. Child Development. 2014;85:308–325. doi: 10.1111/cdev.12127. doi: 10.1111/cdev.12127. [DOI] [PubMed] [Google Scholar]
- Ceballo R, Kennedy T, Bregman A, Epstein-Ngo Q. Always aware (Siemprependiente): Latina mothers' parenting in high-risk neighborhoods. Journal of Family Psychology. 2012;26:805–815. doi: 10.1037/a0029584. doi:10.1037/a0029584. [DOI] [PubMed] [Google Scholar]
- Cochran M, Walker S. Parenting and personal social networks. In: Luster T, Ogakaki L, editors. Parenting: An ecological perspective. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 2005. pp. 235–273. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Ernst JS. Community-level factors and child maltreatment in a suburban county. Social Work Research. 2001;25:133–142. [Google Scholar]
- Fowler PJ, Tompsett CJ, Braciszewski JM, Jacques-Tiura AJ, Baltes BB. Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychology. 2009;21:227–259. doi: 10.1017/S0954579409000145. doi: 10.1017/S0954579409000145. [DOI] [PubMed] [Google Scholar]
- Franco LM, Pottick KJ, Huang C. Early parenthood in a community context: Neighborhood conditions, race-ethnicity, and parenting stress. Journal of Community Psychoogy. 2010;38:574–590. doi: 10.1002/jcop.20382. [Google Scholar]
- Furstenberg FF, Cook TD, Eccles J, Elder GH, Sameroff A. Managing to make it: Urban families and adolescent success. University of Chicago Press; Chicago: 1999. [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Jarrett RL, Jefferson SM. Women's Danger Management Strategies in an Inner-City Housing Project. Family Relations. 2004;53:138–147. [Google Scholar]
- Jenkins EJ. Black women and community violence: Trauma, grief, and coping. Women & Therapy. 2002;25:29–44. doi: 10.1300/J015v25n03_03. [Google Scholar]
- Jordan CE, Campbell R, Follingstad D. Violence and women's mental health: The impact of physical, sexual, and psychological aggression. Annual Review of Clinical Psychology. 2010;6:607–628. doi: 10.1146/annurev-clinpsy-090209-151437. doi:10.1146/annurev-clinpsy-090209-151437. [DOI] [PubMed] [Google Scholar]
- Kawabata Y, Alink LRA, Tseng WL, van IJzendoorn MH, Crick NR. Maternal and paternal parenting styles associated with relational aggression in children and adolescents: A conceptual analysis and meta-analytic review. Developmental Review. 2011;31:240–278. [Google Scholar]
- Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Development Psychology. 2000;36:366–380. doi: 10.1037/0012-1649.36.3.366. [PubMed] [Google Scholar]
- Kimbro RT, Schachter A. Neighborhood poverty and maternal fears of children's outdoor play. Family Relations: An Interdisciplinary Journal of Applied Family Studies. 2011;60:461–475. doi: 10.1111/j.1741-3729.2011.00660.x. doi: 10.1111/j.1741-3729.2011.00660.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebanov PK, Brooks-Gunn J, Duncan GJ. Does neighborhood and family poverty affect mothers' parenting, mental health, and social support? Journal of Marriage and the Family. 1994;56:441–455. doi: 10.2307/353111. [Google Scholar]
- Kliewer W. The role of neighborhood collective efficacy and fear of crime in socialization of coping with violence in low-income communities. Journal of Community Psychology. doi: 10.1002/jcop.21573. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kliewer W, Zaharakis N. Community violence exposure, coping, and problematic alcohol and drug use among urban, female caregivers: A prospective study. Personality and Individual Differences. 2013;55:361–66. doi: 10.1016/j.paid.2013.03.020. doi: 10.1016/j.paid.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotchick BA, Forehand R. Putting parenting in perspective: A discussion of the contextual factors that shape parenting practices. Journal of Child and Family Studies. 2002;11:255–269. doi: 10.1023/A:1016863921662. [Google Scholar]
- Letiecq BL, Koblinsky SA. Parenting in violent neighborhoods: African-American fathers share strategies for keeping kids safe. Journal of Family Issues. 2004;25:715–734. doi: 10.1177/0192513X03259143. [Google Scholar]
- Mandara J, Murray CB. Father's absence and African American adolescent drug use. Journal of Divorce and Remarriage. 2006;46:1–12. doi: 10.1300/J087v46n01_01. [Google Scholar]
- Mapp SC. The effects of sexual abuse as a child on the risk of mothers physically abusing their children: a path analysis using systems theory. Child Abuse & Neglect. 2006;30:1293–1310. doi: 10.1016/j.chiabu.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Marshall N, Noonan A, McCartney K, Marx F, Keefe N. It takes an urban village: Parenting networks of urban families. Journal of Family Issues. 2001;22:163–182. doi:10.1177/019251301022002003. [Google Scholar]
- McDonell JR. Neighborhood characteristics, parenting, and children's safety. Social Indicators Research. 2007;83:177–199. doi: 10.1007/s11205-006-9063-5. [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. doi: 10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- Mitchell SJ, Lewin A, Horn IB, Valentine D, Sanders-Phillips K, Joseph JG. How does violence exposure affect the psychological health and parenting of young African-American mothers? Social Sciences and Medicine. 2009;70:526–533. doi: 10.1016/j.socscimed.2009.10.048. doi: 10.1016/j.socscimed.2009.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SJ, Lewin A, Horn IB, Valentine D, Sanders-Phillips K, Joseph JG. How does violence exposure affect the psychological health and parenting of young African-American mothers? Social Sciences and Medicine. 2009;70:526–533. doi: 10.1016/j.socscimed.2009.10.048. doi: 10.1016/j.socscimed.2009.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller-Johnson S, Sullivan TN, Simon TR. Multisite Violence Prevention Project. (2004). Evaluating the impact of interventions in the multisite violence prevention study: Samples, procedures, and measures. American Journal of Preventive Medicine. 26:48–61. doi: 10.1016/j.amepre.2003.09.015. doi: 10.1016/j.amepre.2003.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. MplusUser's Guide. Sixth Edition Muthen & Muthen; Los Angeles, CA: 2010. [Google Scholar]
- Pinderhughes EE, Nix R, Foster EM, Jones D, The Conduct Problems Prevention Research Group Parenting in context: Impact of neighborhood poverty, residential stability, public services, social networks, and danger on parental behaviors. Journal of Marriage and Family. 2001;63:941–953. doi: 10.1111/j.1741-3737.2001.00941.x. doi: 10.1111/j.1741-3737.2001.00941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, Saltzman W. Survey of exposure to community violence: Self report version. National Institute of Mental Health; Rockville, MD: 1990. [Google Scholar]
- Rodney HE, Mupier R. Behavioral differences between African American male adolescents with biological fathers and those without biological fathers in the home. Journal of Black Studies. 1999;30:45–61. doi: 10.1177/002193479903000103. [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior. 2000;41:177–187. doi: 10.2307/2676304. [Google Scholar]
- Scott S, Briskman J, Woolgar M, Humayun S, O'Connor TG. Attachment in adolescence: Overlap with parenting and unique prediction of behavioral adjustment. Journal of Child Psychology and Psychiatry. 2011;52:1052–1062. doi: 10.1111/j.1469-7610.2011.02453.x. [DOI] [PubMed] [Google Scholar]
- Smetana JG, Metzger A, Gettman DC, Campione-Barr N. Disclosure and secrecy in adolescent-parent relationships. Child Development. 2006;77:201–217. doi: 10.1111/j.1467-8624.2006.00865.x. [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Egeland B, Carlson EA, Collins WA. The Development of the Person: The Minnesota Study of Risk and Adaptation from Birth to Adulthood. Guilford Press; New York: 2005. [Google Scholar]
- Stattin H, Kerr M. Parental monitoring: A reinterpretation. Child Development. 2000;71:1072–1085. doi: 10.1111/1467-8624.00210. doi: 10.1111/1467-8624.00210. [DOI] [PubMed] [Google Scholar]
- Wandersman A, Nation M. Urban neighborhoods and mental health: Psychological contributions to understanding toxicity, resilience, and interventions. American Psychologist. 1998;53:647–656. doi: 10.1037/0003-066X.53.6.647. [PubMed] [Google Scholar]
- Weir LA, Etelson D, Brand DA. Parents' perceptions of neighborhood safety and children's physical activity. Preventive Medicine. 2006;43:212–217. doi: 10.1016/j.ypmed.2006.03.024. doi: 10.1016/j.ypmed.2006.03.024. [DOI] [PubMed] [Google Scholar]
- White RMB, Roosa M. Neighborhood contexts, fathers, and Mexican American young adolescents' internalizing symptoms. Journal of Marriage and Family. 2012;74:152–166. doi: 10.1111/j.1741-3737.2011.00878.x. doi: 10.1111/j.1741-3737.2011.00878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worthington EL, Wade NG, Hight TL, Ripley JS, et al. The Religious Commitment Inventory-10: Development, Refinement, and Validation of a Brief Scale for Research and Counseling. Journal of Counseling Psychology. 2003;50:84–96. doi:10.1037//0022-0167.50.1.84. [Google Scholar]
- Zhang SJ, Anderson SG. Low-income single mothers' community violence exposure and aggressive parenting practices. Children and Youth Services Review. 2010;32:889–895. doi: 10.1016/j.childyouth.2010.02.010. [Google Scholar]
- Zhang S, Eamon MK. Parenting practices as mediators of the effect of mothers' community violence exposure on young children's aggressive behavior. Families in Society. 2011;92:336–343. [Google Scholar]


