Abstract
Background.
Low literacy is common among the elderly and possibly more reflective of educational attainment than years of school completed. We examined the association between literacy and risk of likely dementia in older adults.
Methods.
Participants were 2,458 black and white elders (aged 71–82) from the Health, Aging and Body Composition study, who completed the Rapid Estimate of Adult Literacy in Medicine and were followed for 8 years. Participants were free of dementia at baseline; incidence of likely dementia was defined by hospital records, prescription for dementia medication, or decline in Modified Mini-Mental State Examination score. We conducted Cox proportional hazard models to evaluate the association between literacy and incidence of likely dementia. Demographics, education, income, comorbidities, lifestyle variables, and apolipoprotein E (APOE) ε4 status were included in adjusted analyses.
Results.
Twenty-three percent of participants had limited literacy (<9th-grade level). Limited literacy, as opposed to adequate literacy (≥9th-grade level), was associated with greater incidence of likely dementia (25.5% vs17.0%; unadjusted hazard ratio [HR] = 1.75, 95% confidence interval 1.44–2.13); this association remained significant after adjustment. There was a trend for an interaction between literacy and APOE ε4 status (p = .07); the association between limited literacy and greater incidence of likely dementia was strong among ε4 noncarriers (unadjusted HR = 1.85) but nonsignificant among ε4 carriers (unadjusted HR = 1.25).
Conclusions.
Limited literacy is an important risk factor for likely dementia, especially among APOE ε4-negative older adults, and may prove fruitful to target in interventions aimed at reducing dementia risk.
Key Words: Cognitive aging, Risk factors, Epidemiology.
Low educational attainment, generally measured by years of school completed, is a well-established risk factor for dementia among older adults, with higher education being thought to contribute to cognitive reserve (1). Literacy may be more reflective of educational attainment than years of school completed and thus a more sensitive indicator of risk for the development of dementia. Low literacy is common among elderly adults compared with other age groups (2). In the 2003 National Assessment of Adult Literacy, about one-quarter of older adults were unable to use information presented in text form to accomplish common tasks (2). Further, the association between older age and lower literacy is not merely explained by age differences in years of school completed (3,4).
Cross-sectional studies of older adults have shown positive relationships between literacy and global cognition (5–7), memory (6,7), verbal fluency (6,7), and working memory (8) and other executive skills (7), above and beyond the effects of education. Cross-sectional associations between literacy and cognitive performance are not entirely surprising, as reading ability is considered a proxy measure for premorbid intelligence (9). Longitudinal analysis is needed to ascertain whether low literacy might predict cognitive decline or the development of dementia. Two longitudinal studies evaluated the association between literacy and cognitive decline in aging while controlling for education effects (10,11) and found that individuals with lower literacy showed greater decline in memory, language, and executive functioning. Further, literacy has been shown to help explain racial discrepancies in cognitive performance (12) and rates of cognitive decline (13) between black and white elders independent of education. However, few studies have specifically investigated the association between literacy and the development of dementia. Most have been conducted outside of the United States and focused on developing countries by comparing illiterate versus literate individuals (14–16). In a recent study of dementia incidence among older adults in six “middle-income” countries (China, Cuba, the Dominican Republic, Mexico, Peru, and Venezuela) by Prince and coworkers (17), self-reported ability to read a newspaper was associated with lower dementia incidence even after controlling for education and other measures of socioeconomic status.
In the present study, we examined the association between literacy and incidence of likely dementia in a biracial cohort of older adults residing in two U.S. cities followed prospectively. We hypothesized that limited literacy, as opposed to adequate literacy, would be associated with greater incidence of likely dementia and that literacy would be predictive above and beyond the effects of education and other participant characteristics.
Methods
Population
Participants were from the Health, Aging, and Body Composition (Health ABC) study, a prospective cohort study of community-dwelling, Medicare-eligible older adults conducted at study centers in Pittsburgh, Pennsylvania, and Memphis, Tennessee. Health ABC methods are detailed elsewhere (18–20). Briefly, a random sample of white and all black Medicare-eligible older adults aged between 70 and 79 residing within specified zip codes were contacted, and 3,075 individuals were enrolled. Inclusion criteria required that participants report no difficulty performing activities of daily living, climbing 10 steps without resting, or walking a quarter of a mile. Institutional review boards at the University of Pittsburgh, the University of Tennessee, Memphis, and the University of California, San Francisco, approved the study, and all participants provided written informed consent. Participants’ first study visit (Year 1) took place between 1997 and 1998. At Year 3, participants were administered a measure of literacy (described below); thus, Year 3 is treated as “baseline” for the present analyses, and only individuals who completed the literacy measure in Year 3 are included. Of these 2,512 individuals, we excluded 54 participants who met criteria for prevalent likely dementia (detailed below) on or before Year 3, leaving a total of 2,458 participants in our study.
Measures
Literacy.—
Literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine, an instrument for which individuals read common health-related words aloud (eg, germs, prescription, diagnosis); this measure is highly correlated with other standard, non-health-focused measures of reading ability (21). The Rapid Estimate of Adult Literacy in Medicine total score (0–66), based on correct pronunciation of the words, corresponds to grade-level equivalents with scores between 0 and 18 indicating literacy at or below a 3rd grade reading level, scores between 19 and 44 indicating between a 4th- and 6th-grade reading level, scores between 45 and 60 indicating a 7th- to 8th-grade reading level, and scores above 60 indicating a reading level at or above 9th grade (21). Previous analysis of the Health ABC cohort has shown that about one-quarter of individuals demonstrated literacy below a 9th-grade reading level on the Rapid Estimate of Adult Literacy in Medicine (22,23); this level is considered to reflect limited literacy, meaning that one’s reading ability is likely insufficient to interpret written materials commonly provided in health care settings (21). As previously done in Health ABC, we focused on comparing individuals considered to have limited literacy (<9th-grade reading level) to individuals with adequate literacy (≥9th-grade reading level) (21). We chose this literacy cutoff for our primary analyses to enable investigation of whether relatively subtle differences in literacy are associated with dementia incidence. We also conducted a sensitivity analysis, comparing dementia incidence between individuals at less than or equal to 6th grade, 7th–8th grade, versus greater than or equal to 9th-grade reading levels, to explore whether risk for dementia might be greater among those with even lower literacy.
Likely dementia.—
Participants were administered the Modified Mini-Mental State Exam (3MS) at Years 1, 3, 5, 8, 10, and 11. The 3MS (24) is a cognitive screening instrument assessing orientation, attention, praxis, language, and memory, extended from the traditional Mini-Mental State Exam with scores ranging from 0 to 100. Hospitalization records and medication prescription records were obtained. Participants were interviewed every 6 months about possible hospitalizations, and, if reported, Health ABC staff requested records. Participants were asked to bring in their medications to each clinic visit, and these were recorded by study staff.
Individuals were classified as having developed “likely” dementia if any of the following criteria were met: (a) record of a hospitalization with dementia listed as a primary or secondary diagnosis, determined through Health ABC adjudication to reflect a chronic, progressive decline rather than an acute change (eg, delirium), (b) a documented prescription for dementia medication, or (c) ≥ 1.5 SD decline in 3MS score from participants’ baseline to last visit compared with the mean 3MS change exhibited by their race-matched peers within the cohort. The date of “diagnosis” was recorded as the date on which any of the previous criteria were first met, and this was used to estimate time to the development of likely dementia in our statistical models. This method of measuring likely dementia has been used previously for the Health ABC study (25).
Covariates.—
Demographics (age, sex, and race), education, and household income were obtained at participants’ Year 1 visit. At Year 3, comorbidities, including hypertension, myocardial infarction, diabetes mellitus, stroke, or transient ischemic attack, were determined from a combination of self-report data, physician diagnosis, medications, and laboratory values. Body mass index was calculated from participants’ height and weight, and obesity was defined as a body mass index more than 30. Participants reported their cigarette and alcohol use. Apolipoprotein E (APOE) genotype was obtained via standard single nucleotide polymorphism analyses to determine if participants were APOE ε4 allele carriers.
Statistical Analysis
T-tests and chi-square analyses were used to compare baseline characteristics between individuals with limited versus adequate literacy. To investigate whether literacy predicted incidence of likely dementia, we calculated Kaplan–Meier survival curves and conducted a series of Cox proportional hazard models. Model 1 was unadjusted; Model 2 adjusted for age, sex, and race; Model 3 added adjustments for education and household income; Model 4 added adjustments for comorbidities (hypertension, myocardial infarction, diabetes, stroke/transient ischemic attack, obesity) and lifestyle variables (>1 alcoholic drink per day, current smoker); and Model 5 added adjustment for APOE ε4 status. We tested for interactions between literacy and sex and literacy and race in predicting incidence of likely dementia by adding these interaction terms to Model 2 and Model 5. We tested for interactions between literacy and education and literacy and household income by adding these interaction terms to Model 3 and Model 5. We also tested for an interaction between literacy and APOE ε4 status by adding this interaction term to Model 5. Analyses were conducted with SAS software (version 9.2; SAS Institute Inc, Cary, NC). Statistical significance was set at p < .05 (two-tailed).
Results
Of the 2,458 participants, 76.7% (n = 1886) had adequate literacy (≥9th-grade level), and 23.3% (n = 572) had limited literacy (<9th-grade level). As shown in Table 1, individuals with limited compared to those with adequate literacy were more likely to be male (p < .001), black (p < .001), to have less education (p < .001), and lower income (p < .001). Individuals with limited literacy were more likely to have hypertension (p = .001), diabetes (p < .001), obesity (p < .001), to be current smokers (p = .006), and APOE ε4 carriers (p = .02), and were less likely to consume alcohol (p = .001).
Table 1.
Baseline Characteristics by Literacy Level
| Characteristics, Mean (SD) or % | Limited Literacy (n = 572) | Adequate Literacy (n = 1886) | p |
|---|---|---|---|
| Age, years | 76.2 (2.9) | 76.1 (2.8) | .43 |
| Sex, female | 43.0 | 54.7 | <.001 |
| Race, black | 72.2 | 27.5 | <.001 |
| Education | |||
| <High school | 59.4 | 10.5 | <.001 |
| High school/some college | 35.2 | 56.9 | |
| ≥Bachelor’s degree | 5.5 | 32.6 | |
| Household income | |||
| ≤$25k | 76.6 | 41.0 | <.001 |
| >$25k | 23.4 | 59.0 | |
| Hypertension | 66.4 | 58.9 | .001 |
| Myocardial infarction | 22.9 | 20.5 | .22 |
| Diabetes | 30.0 | 17.8 | <.001 |
| Stroke/transient ischemic attack | 9.4 | 9.5 | .97 |
| Obesity | 32.9 | 21.9 | <.001 |
| Current smoker | 10.0 | 6.5 | .006 |
| >1 Alcoholic drink per day | 4.4 | 8.5 | .001 |
| Apolipoprotein E-ε4 carrier | 31.9 | 26.5 | .02 |
| Baseline Modified Mini-Mental State Exam | 82.6 | 92.8 | <.001 |
Participants were followed for a mean of 7.3 years (SD = 1.9), with 29.4% of participants dropping out prior to completing the full 8 years of follow-up. Of the total 2,458 participants, 20.2% (n = 496) were classified as having developed likely dementia. Of those individuals, 73.2% met the hospitalization criterion, 34.5% met the dementia medication criterion, and 44.6% met the 3MS decline criterion; 41.3% of individuals classified with likely dementia met two or more of the criteria. Of 291 individuals who met only one of the criteria, most (60.8%) met only the hospitalization criteria. On average, the 3MS performance of participants who met criteria for likely dementia declined by −15.4 points (SD = 11.4), whereas participants who did not meet criteria for likely dementia declined on average by −4.4 points (SD = 3.1).
Literacy and Dementia Incidence
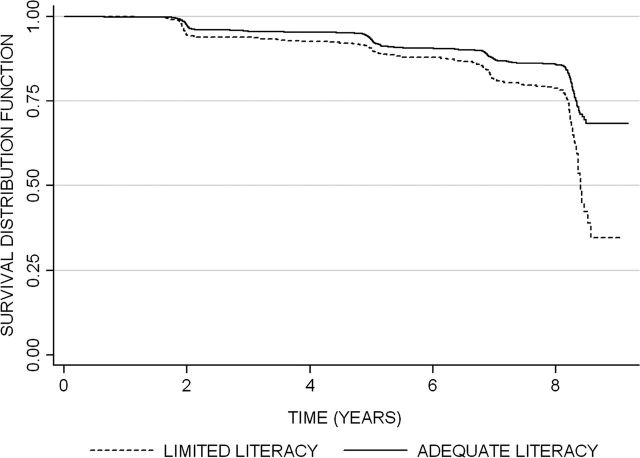
Kaplan–Meier survival curves for the development of likely dementia by literacy level (limited vs adequate) are shown in Figure 1. Of those with limited literacy, 25.5% developed likely dementia over the 8-year follow-up, in comparison with 17.0% of those with adequate literacy (p < .001).
Figure 1.
Literacy level and the development of likely dementia over 8 years. Kaplan–Meier survival curves for the development of likely dementia by literacy level (limited vs adequate). Limited literacy was associated with greater incidence of likely dementia (25.5% vs 17.0%; p < .001).
In an unadjusted Cox proportional hazard model, individuals with limited literacy, compared to those with adequate literacy, were more likely to develop likely dementia (unadjusted hazard ratio [HR] = 1.75, 95% confidence interval [CI] 1.44–2.13, p < .001). As shown in Table 2, this difference remained significant after adjustment for demographics, education, income, comorbidities, lifestyle variables, and APOE ε4 status. Of note, education was not associated with likely dementia incidence in this fully adjusted model (see Supplementary Table 1). There were no significant interactions between literacy and the race, sex, education, or household income variables in predicting incidence of likely dementia. In race-stratified analyses, the association between limited literacy and likely dementia was similar in blacks (unadjusted HR = 1.62, 95% CI 1.24–2.13, p < .001) and whites (unadjusted HR = 1.50, 95% CI 1.05–2.14, p = .026). There was a trend for an interaction between literacy and APOE ε4 status in predicting incidence of likely dementia (p = .07) in the fully adjusted model. To explore this trend, we calculated Models 1 through 4 stratified by APOE-ε4 carriers versus noncarriers. As shown in Table 2, there was a strong and significant association between limited literacy and greater incidence of likely dementia among APOE-ε4 noncarriers, but this association was nonsignificant among APOE-ε4 carriers.
Table 2.
Limited Literacy and Risk of Likely Dementia
| Effect of Limited Literacy | ||||||
|---|---|---|---|---|---|---|
| All Individuals (n = 2458) | APOE-ε4 Noncarriers (n = 1677) | APOE-ε4 Carriers (n = 645) | ||||
| Model | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p |
| Unadjusted model | 1.75 (1.44–2.13) | <.001 | 1.85 (1.41–2.42) | <.001 | 1.25 (0.91–1.73) | .16 |
| Models adjusted for | ||||||
| Age, sex, race | 1.57 (1.26–1.95) | <.001 | 1.80 (1.32–2.45) | <.001 | 1.12 (0.79–1.59) | .52 |
| +Education, household income | 1.53 (1.17–2.00) | .002 | 1.84 (1.26–2.67) | .002 | 1.07 (0.70–1.64) | .76 |
| +Hypertension, myocardial infarction, diabetes, stroke/transient ischemic attack, obesity, smoking, alcohol consumption | 1.49 (1.13–1.96) | .004 | 1.80 (1.23–2.64) | .003 | 1.03 (0.66–1.59) | .91 |
| +APOE ε4 | 1.39 (1.04–1.85) | .03 | — | — | — | — |
Note: APOE = Apolipoprotein E; CI = confidence interval; HR = hazard ratio.
Sensitivity Analysis
To explore whether risk for likely dementia might be greatest among those with the lowest literacy, we conducted a sensitivity analysis by dividing individuals into three literacy groups: less than or equal to 6th grade (n = 206), 7th–8th grade (n = 366), and greater than or equal to 9th-grade level (n = 1886), and results were similar. Both lower literacy groups had greater incidence of likely dementia than the greater than or equal to 9th-grade group (≤6th grade: 27.2%, 7th–8th grade: 24.6%, ≥9th grade: 17.0%; ≤6th grade vs ≥9th grade: unadjusted HR = 1.98, 95% CI 1.49–2.62, p < .001; 7th–8th grade vs ≥9th grade: unadjusted HR = 1.63, 95% CI 1.29–2.07, p < .001), and the two lowest literacy groups did not significantly differ from each other with respect to risk for likely dementia (≤6th grade vs 7th–8th grade: unadjusted HR = 1.23, 95% CI 0.88–1.71, p = .23).
Discussion
We found that limited literacy was associated with greater incidence of likely dementia among a biracial cohort of older adults followed over 8 years, an association which did not differ by race, sex, education level, or household income. Our study is novel in showing that the relationship between limited literacy and increased risk for likely dementia is particularly strong among APOE ε4-negative elders. Specifically, limited literacy predicted the development of likely dementia beyond the effects of education and comorbidities among APOE ε4 noncarriers. In contrast, among APOE ε4 carriers, there was no association between literacy and incidence of likely dementia before or after adjustment for other participant characteristics. Although the interaction between literacy and APOE ε4 status was of borderline significance in our cohort, the effect size differences were striking. This pattern of results is not without precedent as Seeman and coworkers (26) reported a significant interaction in the same direction between APOE ε4 status and years of education in predicting cognitive decline. However, these findings differ from Ngandu and coworkers (27), who found that low education was associated with greater dementia risk among both ε4 carriers and noncarriers. The discrepancy between these results is unclear and warrants further study.
Possession of at least one APOE ε4 allele is a well-established risk factor for the development of dementia, with possession of two ε4 alleles placing individuals at even greater risk (28,29). It may be that the impact of this genetic risk factor is so great, relatively speaking, that other individual characteristics, such as literacy level, have less potential to influence the development of dementia. Consistent with this explanation, associations between other risk factors and the development of dementia also differ by APOE ε4 status. For example, studies linking smoking (30), physical activity (31), and diet (32,33) to dementia risk have found that these relationships are stronger or occur only among APOE ε4 noncarriers.
Our findings indicate that, at least among APOE ε4 noncarriers, lower literacy is associated with greater risk for likely dementia independent of the effects of education. Indeed, our results indicate that it is not just individuals with the lowest literacy or illiterate individuals who are at greater risk for dementia; rather, even more subtle weaknesses in literacy (ie, 7th- to 8th-grade reading level vs 9th-grade reading level) among this cohort of older adults predicted greater incidence of likely dementia. Higher literacy may be a more sensitive marker of cognitive reserve than higher education such that an individual’s reading level may be more reflective of the “protection” from dementia built up earlier in life through the attainment of academic skills. Older adults with better literacy may also more readily and comfortably interact with written material in their daily lives, which could serve to facilitate the maintenance of cognition. We cannot fully rule out the possibility that limited literacy may have been a marker for the beginnings of a cognitive decline process in some individuals; however, this possibility would be a less likely explanation for our results. Reading ability has been shown to remain relatively stable even in individuals who have converted to mild dementia (34) such that reading tests are commonly used to estimate premorbid functioning in cognitively impaired individuals (9).
One strength of this study concerns the ability to control for factors not previously accounted for, including comorbidities (eg, cardiovascular disease and vascular risk factors). As these factors are also linked to the development of dementia (35), they are important to consider when evaluating limited literacy as a potential risk factor in its own right. After adjusting for comorbidities, ε4 noncarriers with limited literacy were still more likely to develop likely dementia. This finding is further evidence of the importance of limited literacy as a risk factor, yet another aspect of a patient’s presentation that clinical providers should consider in the assessment and care of older adults. The clinical importance of literacy among older adults is supported in other domains by associations between lower literacy and worse health outcomes, including poorer physical health (22,36), greater depression (22,36), less access to and/or utilization of health care (22,37), and increased risk of mortality(23,36,38,39).
Other study strengths include the prospective follow-up of a large cohort of black and white older adults over 8 years. Further, unlike some previous studies that based analyses on differentiating between illiterate versus literate individuals or based literacy on an individual’s self-report, we utilized an objective literacy measure that enabled us to conclude that even individuals with up to a 7th- to 8th-grade reading level were more likely to develop likely dementia than those with higher literacy. There are limitations to consider, however, including the “likely” dementia outcome. This outcome was determined using an algorithm rather than a comprehensive dementia work-up tailored to each individual. Although we believe the criteria we used are relatively sensitive to the diagnosis of dementia, our algorithm likely has less specificity than would a full clinical evaluation. We may have misclassified some individuals as having likely dementia that did not and perhaps may have failed to identify some individuals who truly did develop dementia. If or how misclassification may have affected the association between limited literacy and likely dementia is unclear. It also remains unknown whether the relationship between literacy and the development of dementia might be specific to a particular dementia etiology. Further, we cannot rule out the possibility that limited literacy may be associated with factors we did not measure, such as socioeconomic disadvantage earlier in life or lifelong learning disorders, which may in themselves be risk factors for dementia. Finally, a few of our covariates were based solely on self-report (eg, income), a limitation common in observational studies.
Our study shows that, particularly among APOE ε4-negative elders, limited literacy predicts development of likely dementia independent of other factors, including education and comorbidities. This provides further evidence that low literacy, which is common among older adults, is an important public health problem. The development of interventions aimed at improving literacy among older adults appears warranted on several levels and as this study has shown it may serve to reduce the risk for dementia, a possibility that warrants further investigation. Future directions also include evaluating potential mechanisms that underlie the link between literacy and risk for dementia, such as how higher literacy might protect the aging brain.
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Funding
This work was supported by the National Institute on Aging (N01-AG-6-2101, N01-AG-6-2103, N01-AG-6-2106; R01-AG028050, K24AG031155 to K.Y.) and National Institute of Nursing Research (R01-NR012459). This work was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute on Aging. Writing of this manuscript was supported by Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the San Francisco Veterans Affairs Medical Center, and the Department of Veterans Affairs Sierra-Pacific Mental Illness Research, Education, and Clinical Center.
References
- 1. Meng X, D’Arcy C. Education and dementia in the context of the cognitive reserve hypothesis: a systematic review with meta-analyses and qualitative analyses. PLoS One. 2012;7:e38268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kutner M, Greenberg E, Baer J. National Assessment of Adult Literacy (NAAL): A first look at the literacy of America’s adults in the 21st Century 2005. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006470 Accessed August 20, 2012
- 3. Brown H, Prisuta R, Jacobs B, Campbell A. Literacy of Older Adults in America: Results From the National Adult Literacy Survey. Washington, DC: National Center for Education Statistics; 1996. http://nces.ed.gov/pubs97/97576.pdf Accessed August 8, 2012 [Google Scholar]
- 4. Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. J Gerontol B Psychol Sci Soc Sci. 2000;55:S368–S374 [DOI] [PubMed] [Google Scholar]
- 5. Albert SM, Teresi JA. Reading ability, education, and cognitive status assessment among older adults in Harlem, New York City. Am J Public Health. 1999;89:95–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Federman AD, Sano M, Wolf MS, Siu AL, Halm EA. Health literacy and cognitive performance in older adults. J Am Geriatr Soc. 2009;57:1475–1480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barnes DE, Tager IB, Satariano WA, Yaffe K. The relationship between literacy and cognition in well-educated elders. J Gerontol A Biol Sci Med Sci. 2004;59(4):M390–M395 [DOI] [PubMed] [Google Scholar]
- 8. Jefferson AL, Gibbons LE, Rentz DM, et al. A life course model of cognitive activities, socioeconomic status, education, reading ability, and cognition. J Am Geriatr Soc. 2011;59:1403–1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed New York: Oxford University Press; 2004 [Google Scholar]
- 10. Manly JJ, Schupf N, Tang MX, Stern Y. Cognitive decline and literacy among ethnically diverse elders. J Geriatr Psychiatry Neurol. 2005;18:213–217 [DOI] [PubMed] [Google Scholar]
- 11. Manly JJ, Touradji P, Tang MX, Stern Y. Literacy and memory decline among ethnically diverse elders. J Clin Exp Neuropsychol. 2003;25:680–690 [DOI] [PubMed] [Google Scholar]
- 12. Mehta KM, Simonsick EM, Rooks R, et al. Black and white differences in cognitive function test scores: what explains the difference? J Am Geriatr Soc. 2004;52:2120–2127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sachs-Ericsson N, Blazer DG. Racial differences in cognitive decline in a sample of community-dwelling older adults: the mediating role of education and literacy. Am J Geriatr Psychiatry. 2005;13:968–975 [DOI] [PubMed] [Google Scholar]
- 14. Nitrini R, Bottino CM, Albala C, et al. Prevalence of dementia in Latin America: a collaborative study of population-based cohorts. Int Psychogeriatr. 2009;21:622–630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nitrini R, Caramelli P, Herrera E, Jr, et al. Incidence of dementia in a community-dwelling Brazilian population. Alzheimer Dis Assoc Disord. 2004;18:241–246 [PubMed] [Google Scholar]
- 16. Li G, Shen YC, Chen CH, Zhau YW, Li SR, Lu M. A three-year follow-up study of age-related dementia in an urban area of Beijing. Acta Psychiatr Scand. 1991;83:99–104 [DOI] [PubMed] [Google Scholar]
- 17. Prince M, Acosta D, Ferri CP, et al. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: a 10/66 Dementia Research Group population-based cohort study. Lancet. 2012;380:50–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harris TB, Visser M, Everhart J, et al. Waist circumference and sagittal diameter reflect total body fat better than visceral fat in older men and women. The Health, Aging and Body Composition study. Ann N Y Acad Sci. 2000;904:462–473 [DOI] [PubMed] [Google Scholar]
- 19. Rooks RN, Simonsick EM, Miles T, et al. The association of race and socioeconomic status with cardiovascular disease indicators among older adults in the health, aging, and body composition study. J Gerontol B Psychol Sci Soc Sci. 2002;57:S247–S256 [DOI] [PubMed] [Google Scholar]
- 20. Yaffe K, Barnes D, Lindquist K, et al. ; Health ABC Investigators. Endogenous sex hormone levels and risk of cognitive decline in an older biracial cohort. Neurobiol Aging. 2007;28:171–178 [DOI] [PubMed] [Google Scholar]
- 21. Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395 [PubMed] [Google Scholar]
- 22. Sudore RL, Mehta KM, Simonsick EM, et al. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54:770–776 [DOI] [PubMed] [Google Scholar]
- 23. Sudore RL, Yaffe K, Satterfield S, et al. Limited literacy and mortality in the elderly: the health, aging, and body composition study. J Gen Intern Med. 2006;21:806–812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Teng EL, Chui HC. The Modified Mini-Mental State Examination (3MS). Can J Psychiatry. 1987;41:114–121 [PubMed] [Google Scholar]
- 25. Hong CH, Falvey C, Harris TB, et al. Anemia and risk of dementia in older adults: findings from the Health ABC study. Neurology. 2013;81:528–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Seeman TE, Huang MH, Bretsky P, Crimmins E, Launer L, Guralnik JM. Education and APOE-e4 in longitudinal cognitive decline: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 2005;60:P74–P83 [DOI] [PubMed] [Google Scholar]
- 27. Ngandu T, von Strauss E, Helkala EL, et al. Education and dementia: what lies behind the association? Neurology. 2007;69:1442–1450 [DOI] [PubMed] [Google Scholar]
- 28. Slooter AJ, Cruts M, Kalmijn S, et al. Risk estimates of dementia by apolipoprotein E genotypes from a population-based incidence study: the Rotterdam Study. Arch Neurol. 1998;55:964–968 [DOI] [PubMed] [Google Scholar]
- 29. Rubinsztein DC, Easton DF. Apolipoprotein E genetic variation and Alzheimer’s disease: a meta-analysis. Dement Geriatr Cogn Disord. 1999;10:199–209 [DOI] [PubMed] [Google Scholar]
- 30. Ott A, Slooter AJ, Hofman A, et al. Smoking and risk of dementia and Alzheimer’s disease in a population-based cohort study: the Rotterdam Study. Lancet. 1998;351:1840–1843 [DOI] [PubMed] [Google Scholar]
- 31. Podewils LJ, Guallar E, Kuller LH, et al. Physical activity, APOE genotype, and dementia risk: findings from the Cardiovascular Health Cognition Study. Am J Epidemiol. 2005;161:639–651 [DOI] [PubMed] [Google Scholar]
- 32. Barberger-Gateau P, Raffaitin C, Letenneur L, et al. Dietary patterns and risk of dementia: the Three-City cohort study. Neurology. 2007;69:1921–1930 [DOI] [PubMed] [Google Scholar]
- 33. Huang TL, Zandi PP, Tucker KL, et al. Benefits of fatty fish on dementia risk are stronger for those without APOE epsilon4. Neurology. 2005;65:1409–1414 [DOI] [PubMed] [Google Scholar]
- 34. Schmand B, Geerlings MI, Jonker C, Lindeboom J. Reading ability as an estimator of premorbid intelligence: does it remain stable in emergent dementia? J Clin Exp Neuropsychol. 1998;20:42–51 [DOI] [PubMed] [Google Scholar]
- 35. Middleton LE, Yaffe K. Targets for the prevention of dementia. J Alzheimers Dis. 2010;20:915–924 [DOI] [PubMed] [Google Scholar]
- 36. Bostock S, Steptoe A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012;344:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404 [DOI] [PubMed] [Google Scholar]
- 38. Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–1509 [DOI] [PubMed] [Google Scholar]
- 39. Baker DW, Wolf MS, Feinglass J, Thompson JA. Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med. 2008;23:723–726 [DOI] [PMC free article] [PubMed] [Google Scholar]