Abstract
Objective:
Clinical reports in children implicate restless legs syndrome (RLS) with sleep and behavior problems. However, population-based studies on this association in adolescents and young adults are limited. Furthermore, few studies have evaluated the association between symptoms consistent with RLS and quality of life (QoL).
Study Design:
This cross-sectional study included 214 Caucasian and Hispanic adolescents and young adults aged 12-20 years. Symptoms consistent with RLS were based on four essential criteria and if the symptoms occurred ≥ 5 days/ month. Trouble falling asleep was present if reported “yes, still have the problem.” Quality of life (QoL) was assessed using the Pediatric QoL Inventory. Three summary QoL scores ranging from 0-100 were evaluated; higher scores indicated better QoL.
Results:
Participants were 50% male and 68.1% Caucasian. Prevalence of RLS was 8.4% (n = 18). RLS was associated with trouble falling asleep (OR = 3.1, p = 0.049), and trouble falling asleep was associated with worse Psychosocial Health scores (Coeff. −5.6, p = 0.004) and Total Scale scores for quality of life (Coeff. −4.6, p = 0.007).
Conclusions:
The prevalence of symptoms consistent with RLS in this community-based sample of adolescents and young adults, aged 12-20, is comparable to rates reported in older cohorts. Symptoms consistent with RLS may be associated with trouble falling asleep and psychosocial distress that may contribute to a lower health-related quality of life.
Citation:
Silva GE, Goodwin JL, Vana KD, Vasquez MM, Wilcox PG, Quan SF. Restless legs syndrome, sleep, and quality of life among adolescents and young adults. J Clin Sleep Med 2014;10(7):779-786.
Keywords: restless legs syndrome, quality of life, adolescents, young adults, and sleep
Restless legs syndrome (RLS) is defined as a sensorimotor disorder that can have a pronounced disturbance on sleep with symptom severity ranging from mild and occasional to nightly and severe with complete disruption of sleep. Four essential criteria have been identified and are required for the identification of RLS.1 These are: (1) an urge to move the legs often accompanied by unpleasant sensations; (2) the urge is worsened during rest or inactivity; (3) the urge is improved with leg movement; and (4) the urge is worsened in the evening or night. The prevalence of RLS in adults is approximately 10% and has been associated with iron deficiency, pregnancy, end-stage renal disease, and family history of RLS.2,3 RLS was first described in children by Walters in 1994,4 and the prevalence of RLS has been reported to be between 2% and 6%,5,6 although relatively few studies of RLS have been conducted in the pediatric and adolescent populations. In adults, RLS has been associated with depression.7 However, little information is available on the impact of RLS on quality of life. In one study, RLS was found to have a significant impact on health-related quality of life, measured using the SF-36 (Medical Outcomes Study 36-Item Short Form health survey), in 85 adult subjects with RLS as compared to 2,474 subjects from the general population.8 Subjects with RLS reported significant deficits in health-related quality of life when compared to subjects with hypertension, cardiovascular conditions, diabetes, and those with osteoarthritis. Similarly in another study including 3,433 older men and women, those with RLS had lower health-related quality of life in all physical domains of the SF-36 compared to subjects with no RLS.9
BRIEF SUMMARY
Current Knowledge/Study Rationale: Clinical reports in children implicate restless legs syndrome (RLS) with sleep and behavior problems. The purpose of this study is to investigate the prevalence of symptoms consistent with RLS in a community sample of adolescents and young adults and its association with sleep and health-related quality of life.
Study Impact: Results from this study show that RLS symptoms in adolescents and young adults are similar to previously published RLS prevalence rates in adults. RLS symptoms were significantly with greater odds of having trouble falling asleep, and trouble falling asleep was associated with lower health-related quality of life.
In children, RLS has been associated with attention deficit hyperactivity disorder (ADHD), growing pains, behavioral disorders, and low ferritin levels.10–13 However, only a small number of studies have evaluated RLS in the adolescent population, and fewer have assessed RLS and its correlates including quality of life in community pediatric populations. The aim of this study is to investigate the prevalence of symptoms consistent with RLS in a community sample of adolescents and young adults and its association with sleep and health-related quality of life.
METHODS
Design and Protocol
The Tucson Children's Assessment of Sleep Apnea Study (TuCASA) is a prospective cohort study designed to investigate the natural history of sleep disordered breathing and its impact on school and neurocognitive performances. At its initial baseline assessment, 503 Hispanic and Caucasian children aged 6 to 12 years were recruited to undergo unattended home polysomnograms (PSGs), perform neurocognitive assessments, and complete a sleep habits questionnaire (SHQ).14 Excluded were children whose parents reported them to have a history of tonsillectomy, ADHD, mental retardation, or other mental or physiological conditions that would affect neurocognitive or sleep testing. Included were Hispanic or Caucasian children who returned the screening questionnaire with recruitment information and did not meet exclusion criteria. A second assessment was conducted approximately 5 years after the first examination.
A third assessment of the participants was undertaken when participants were aged to 12-20 years, consisting of a follow-up sleep and health-related quality of life questionnaire only. This questionnaire was mailed to all participants who completed the baseline and second phase assessments and comprised 43 questions that were used in the SHQ and the addition of 23 questions from the Pediatric Quality of Life (PedsQL) questionnaire. Participants were asked to complete the questionnaire themselves. A total of 218 subjects returned the follow-up questionnaire; 4 of these had missing RLS-related questions and thus were excluded from further analyses. The present analysis is based on the 214 subjects with complete RLS-related questions. The TuCASA study was approved by the University of Arizona Institutional Review Board, as well as the Tucson Unified School District Research Committee. Complete details of the TuCASA study design have been published previously.14,15
Excessive daytime sleepiness (EDS) was defined as present if affirmative answers were given to any of the following questions: Are you sleepy during the daytime? Do you fall asleep at school or while working? or Do you fall asleep while watching television? Participants were classified as having learning problems or snoring if they answered frequently or almost always to the following questions: Do you have learning problems? or How often do you snore now? Reports of never, rarely, or occasionally were considered negative. Sleepwalking and sleep talking were present if participants reported having these symptoms ≥ 3 times per month and absent if participants answered having the symptoms < 3 times per month. Diagnosed sleep apnea was present if participants noted that health-care providers had told them that they had sleep apnea, and witnessed apnea was present if participants answered affirmative to the question, Based on what household members have told you, are there times when you stop breathing during your sleep? Difficulty initiating and maintaining sleep (DIMS) was present if participants answered yes, and still have the problem for having trouble falling asleep, trouble staying asleep, or waking up too early and not being able to get back to sleep and was negative for answers of yes, but no longer have the problem or no, do not have the problem. Sleep onset latency (SOL) was computed from the question, How long does it usually take you to fall asleep after going to bed? Total sleep time (TST) was computed from the question, How many hours of sleep do you usually get on week nights or school nights? The body mass index (BMI) was computed as kg/m2 from self-reports of height in inches and weight in pounds. The amount of time playing video games or games on a computer per day and the amount of time watching television per day also were asked.
Symptoms consistent with restless legs syndrome were determined using the International Restless Legs Syndrome Study Group rating scale (IRSSG),1 consisting of 4 essential criteria for the identification of RLS. Criterion 1 was present if participants endorsed having an urge to move their legs or unpleasant or uncomfortable feelings in their legs during the past year. Criterion 2 was present if participants reported that the symptoms were most likely to occur when they were resting, sitting, or lying down. Criterion 3 was present if participants reported that the symptoms improved if they got up and started walking. Criterion 4 was present if the symptoms occurred in the evening or nighttime, or if the symptoms persisted both day and night, but worsened in the evening or night. In addition, RLS was considered present if symptoms were reported ≥ 5 days per month and considered negative if symptoms were reported ≤ 4 times per month in order to identify participants with significant RLS symptoms.
Health-related quality of life was assessed using the Pediatric Quality of Life Inventory (PedsQL).16–19 The PedsQL is a 23-item self-report scale for children aged 2-18 that uses 4 subscales to evaluate: (1) Physical Functioning (8 items), (2) Emotional Functioning (5 items), (3) Social Functioning (5 items), and (4) School Functioning (5 items). The instructions ask how much of a problem each item has been during the past one month. A 5-point response scale is utilized (0 = never a problem; 1 = almost never a problem; 2 = sometimes a problem; 3 = often a problem; 4 = almost always a problem). Items were reverse-scored and linearly transformed to a 0 to 100 scale (0 = 100, 1 = 75, 2 = 50, 3 = 25, 4 = 0), so that higher scores indicated better health-related quality of life. Subscale scores were computed as the sum of the items divided by the number of items answered, which accounted for missing data. If > 50% of the items in the subscale were missing, the subscale score was not computed. For this study, > 99% of respondents were included in the subscale score analyses. The Total Scale Score was computed as the sum of all the items over the number of answered items on all scales. To create the Psychosocial Health Summary Score (15 items), the mean was computed as the sum of the items divided by the number of answered items in the Emotional, Social, and School Functioning subscales. The Physical Health Summary Score (8 items) was the subscale score for the Physical Functioning subscale.
Analyses
The Fisher exact test was used to compare differences in proportions between each of the categorical variables by status of symptoms consistent with RLS and between each variable and gender. The Student t-test was used to compare differences in mean values for continuous variables by status of symptoms consistent with RLS and by gender. Multivariate logistic regressions were fitted to evaluate odds of having trouble falling asleep by status of symptoms consistent with RLS. Models were adjusted for diagnosed sleep apnea, EDS, and learning problems. Models also were adjusted for DIMS, witnessed apnea, snoring, gender, ethnicity, and hours of television or video watching; however, these additional variables were not significant and were excluded from the final model.
Separate multiple linear regression models were fitted to estimate the effect of having trouble falling asleep as the independent variable on health-related quality of life summary scores for Physical Function, Psychosocial Health, and Total Score as dependent variables. Models were adjusted for gender, ethnicity, diagnosed sleep apnea, EDS, and learning problems. Models also were adjusted for snoring, witnessed apnea, sleepwalking, sleep talking, and television or video watching; these additional variables, however, were not significant and were not kept in the final models. Variables tested in the logistic and linear models were selected in accordance with possible biologic associations, significance, or in accordance with previously published studies. Statistical analyses were conducted using Intercooled Stata version 12.0 statistical software (Stata Corp, College Station, TX). A significance level of p < 0.05 was used for all statistical tests.
RESULTS
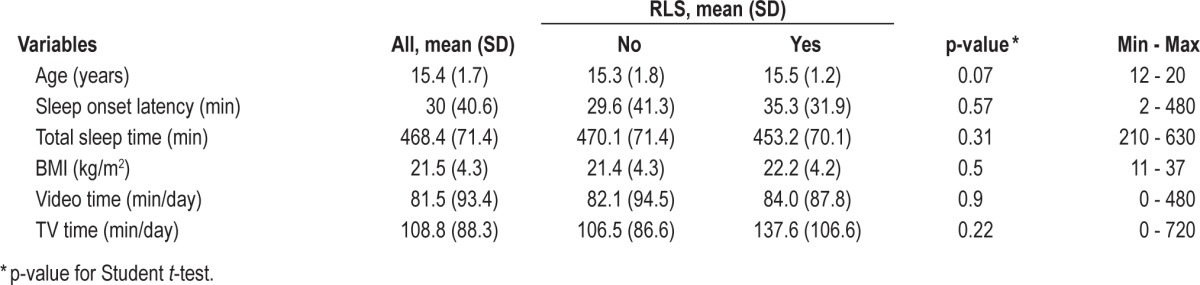
Participants had the following demographics: mean age of 15.4 years (SD 1.7), 50% male and 50% female, 68.1% Caucasian, and 31.9% Hispanic. Eighteen participants (8.4%) were classified as having symptoms consistent with RLS (8 males and 10 females). Trouble falling asleep was present in 35% (68 of 196) of those without RLS symptoms and in 67% (12 of 18) of those with RLS symptoms (p = 0.001). Diagnosed sleep apnea was present in 5% (9 of 187) of those without RLS symptoms and in 16.7% (3 of 18) of those with RLS symptoms (p = 0.06; Table 1). No significant differences, however, were observed for SOL, TST, BMI, or video or television time (Table 2). In this study, SOL was a self-reported measure of the usual amount of time that was required for participants to fall asleep, whereas trouble falling asleep referred to the participant's perceived distress with falling asleep, so that there is no direct correlation between these two variables. Comparing the subset of subjects who participated in the questionnaire follow-up with those in the second assessment we found no difference in gender (p = 0.545). However, a lower proportion of Hispanics (25.4%) than Caucasians (42.2%, p < 0.001) and those who were slightly younger (mean difference 0.53 years, p = 0.005, data not shown) participated in the follow-up study.
Table 1.
Descriptive characteristics by RLS symptom status for dichotomous variables**
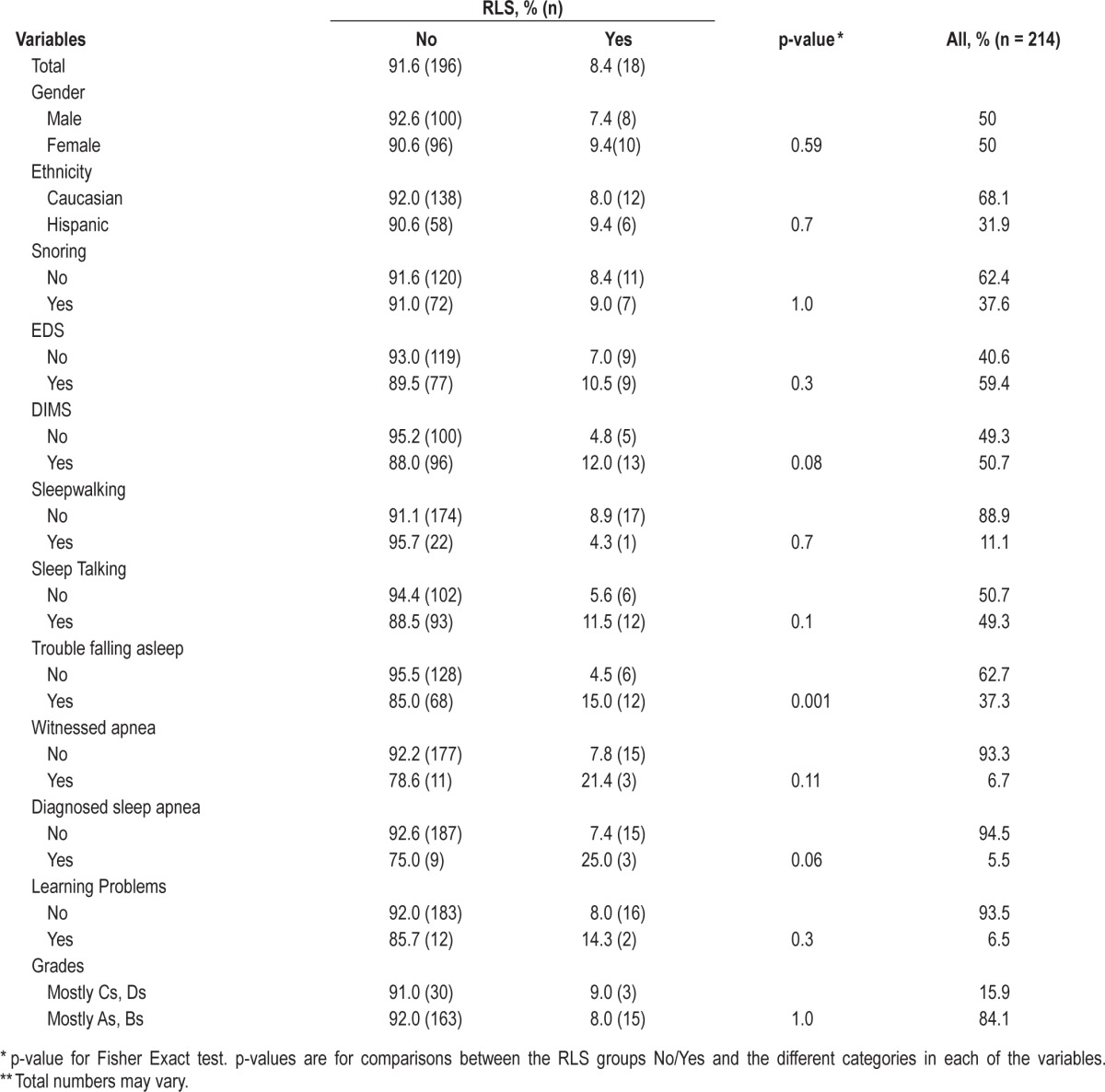
Table 2.
Descriptive characteristics by RLS symptom status for continuous variables
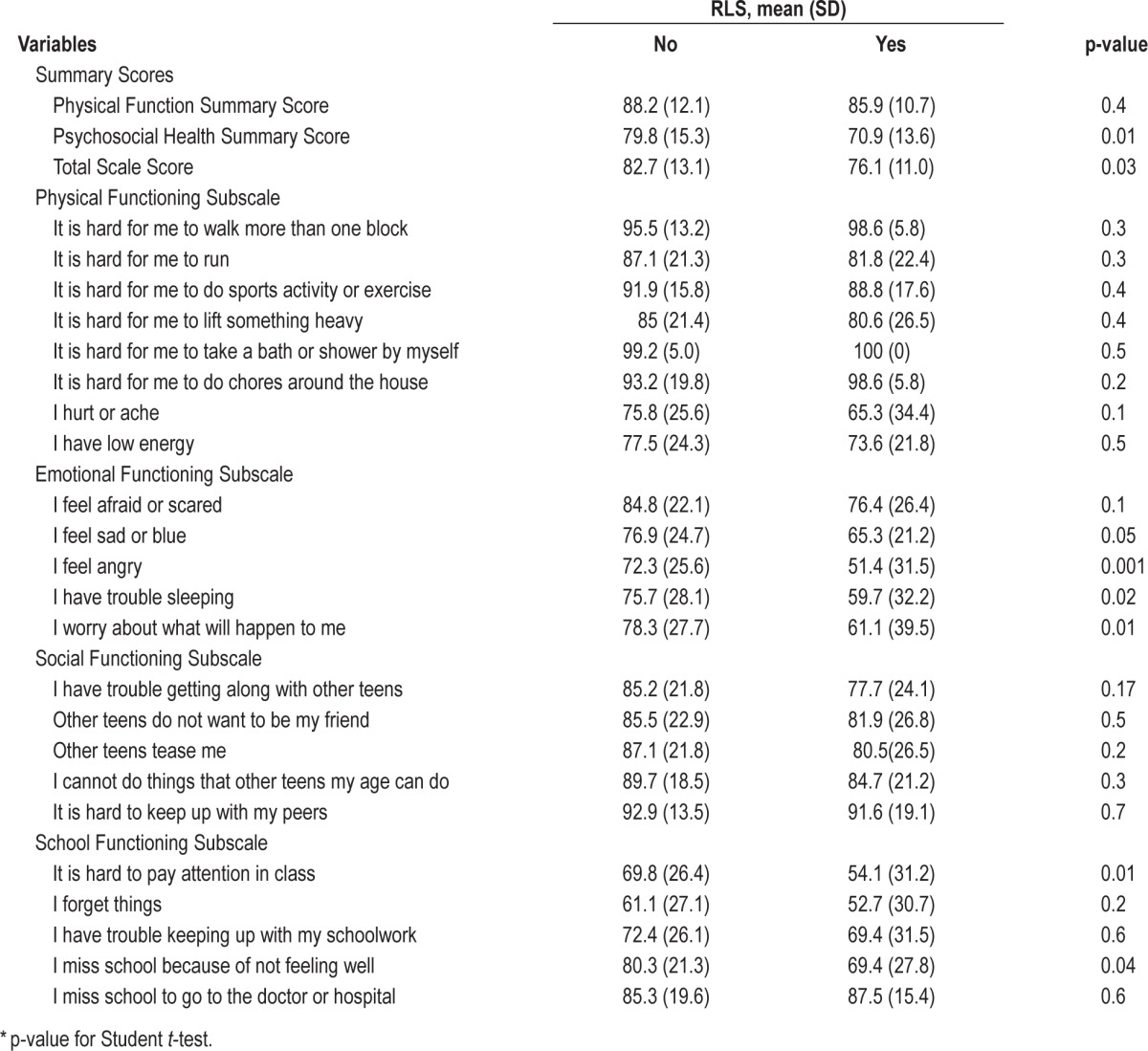
Mean Psychosocial Health Summary Scores were significantly lower for participants with RLS symptoms (70.9) than for those without RLS symptoms (79.8, p = 0.01). Likewise, the Total Scale Scores were lower for participants with RLS symptoms (76.1) than for those without RLS symptoms (82.7, p = 0.03; Figure 1). Individual items in the Emotional Functioning subscale were lower for those with RLS symptoms than for those without RLS symptoms with significant differences for those reporting feeling blue, angry, having trouble sleeping, and worrying about what will happen to them. In the School Functioning subscale, the item scores for hard to pay attention in class and missing school because of not feeling well were significantly lower for participants with RLS symptoms than for those without RLS symptoms (54.1 vs. 69.8, p = 0.01 and 69.4 vs. 80.3, p = 0.04, respectively; Table 3). Individual items in the Social Functioning Subscale and most items on the Physical Functioning Subscale also were lower for subjects with RLS symptoms than for those without RLS symptoms; however, the differences did not achieve statistical significance.
Figure 1. Health-Related Quality of Life Summary Scores by RLS Symptom Status.
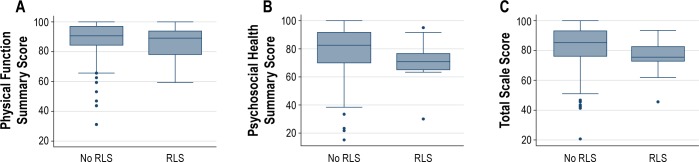
Box graphs showing distributions for Physical Function Summary Score (A), Psychosocial Health Summary Score (B), and Total Scale Score (C) by RLS symptom status. The line in the middle of each box graph represents the median values for the scores. The boxes show lower medians for participants with RLS symptoms than those without RLS symptoms for Physical Function (89.1 vs. 90.62), Psychosocial Health (70.8 vs. 82.5), and Total Scale (75.5 vs. 85.3) scores. The boxes extend from the 25th to the 75th percentiles of the data. Outliers are represented by circles and are shown outside the whisker lines. The whisker lines extend to the most extreme observations that are not more than 1.5 times the height of the box beyond either quartile.
Table 3.
Health-Related Quality of Life by RLS symptom status
When health-related quality of life scales were compared by gender, females had lower mean Physical Function Summary Scores (86.3) than males (89.5, p = 0.05). Females also had lower scores for most individual items in the Physical Functioning and Emotional Functioning subscales than males. Males reported lower scores (83.6) than females (90.0, p = 0.03) to the Social Functioning Subscale question, other teens tease me. Males also spent more time playing video games (107 min) than females (53 min, p < 0.001, data not shown). Analyses by ethnicity showed that Hispanics spent more time watching television (130 min) and had higher BMIs (22.8 kg/m2) than Caucasians (99 min, p = 0.02, and 20.9 kg/m2, p = 0.005, respectively). No other differences were noted by gender or ethnicity (data not shown).
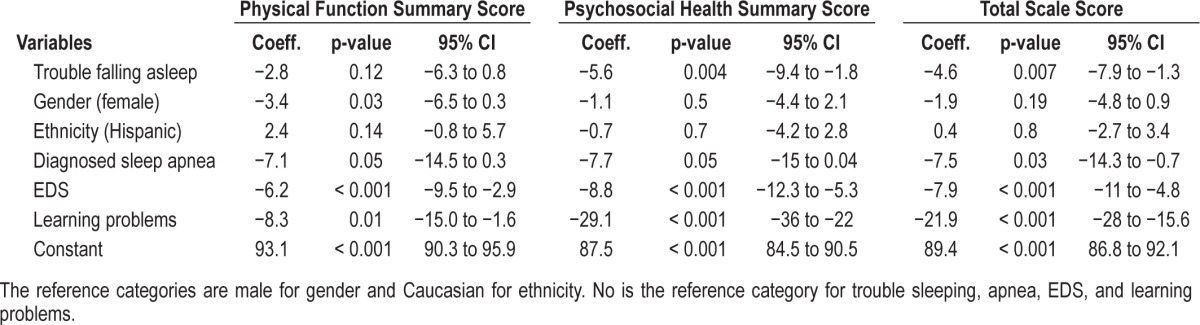
Logistic regression models showed that the odds of experiencing trouble falling asleep for participants with RLS symptoms were 3.1 (p = 0.049, 95% CI: 1.01–9.6) as compared to those without RLS symptoms (Table 4). The odds of having trouble falling asleep for participants with diagnosed sleep apnea were 6.5 (p = 0.009, 95% CI: 1.6–26.6) and 2.9 for those participants with EDS (p = 0.001, 95% CI: 1.5–5.4), while the odds of experiencing trouble falling asleep for those participants with learning problems were 22.6 (p = 0.003, 95% CI: 2.8–181.6, the large CI being a result of small number of subject with learning problems). Multiple linear regressions predicting health-related quality of life summary scores showed a significant inverse association between trouble falling asleep and Psychosocial Health Summary Scores (coeff. = −5.6, p = 0.004) and between trouble falling asleep and the Total Scale Scores (coeff. = −4.6, p = 0.007) when adjusted for other covariates (Table 5). No associations were found between trouble falling asleep and Physical Function Summary Scores. Diagnosed sleep apnea, EDS, and learning problems were significant predictors for lower health-related quality of life scores.
Table 4.
Logistic regression predicting trouble falling asleep by RLS symptoms adjusting for covariates
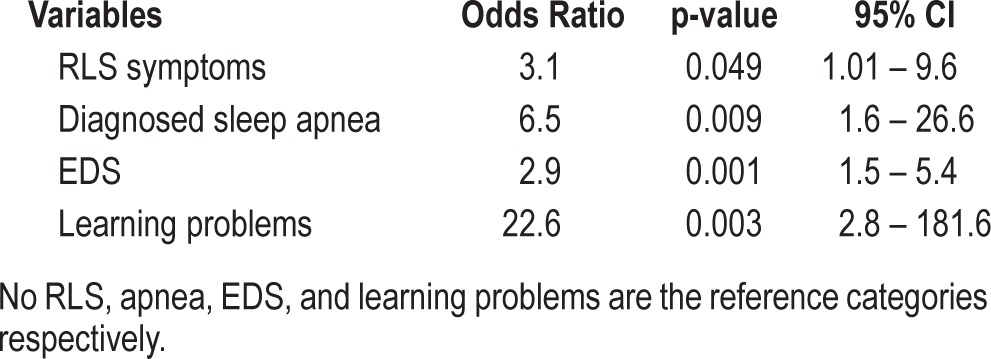
Table 5.
Linear regressions predicting Health-Related Quality of Life scores by trouble sleeping and adjusted for covariates
DISCUSSION
Results from this study showed that prevalence of symptoms consistent with RLS among this cohort of adolescents and young adults is comparable to RLS prevalence rates previously reported in adults,9,20 and that a large percentage of these adolescents and young adults with RLS symptoms had trouble falling asleep, which may have affected their health-related quality of life scores. Participants with RLS symptoms had significantly lower Psychosocial Health Summary scores and lower Total Scale scores than participants without RLS symptoms.
Adolescents and young adults with RLS symptoms also were more likely to have trouble falling asleep than participants without RLS symptoms, as well as to admit to EDS; the odds for experiencing trouble falling asleep for participants with RLS symptoms were 3.1 and the odds for trouble falling asleep were 2.9 for those participants with EDS and no RLS symptoms. Previous studies in children and adolescents have reported similar findings.6,21 Yilmaz and associates noted that adolescents with RLS were more likely to experience difficulty falling asleep than those adolescents without RLS (47% vs. 32%) and that adolescents with RLS had generally higher Epworth Sleepiness Scale scores.22 Arbuckle et al. noted that 79% of children and adolescents with RLS had problems falling asleep and 70% felt tired or sleepy during the day.23 However, the direction of the association between EDS and trouble falling asleep cannot be determined in a cross-sectional design.
While not all subjects with RLS are reported to experience EDS,24 some studies suggest a correlation between RLS, trouble falling asleep, EDS, and impaired concentration and learning. Picchietti et al. noted that 40% of adolescents with RLS were unable to concentrate on their studies.6 Picchietti also noted that 48% of children and adolescents with RLS (n = 16), aged 6-17, suffered cognitively, which affected schoolwork or homework, and that 45% (n = 15) of these children and adolescents had difficulty concentrating.25 However, almost half of the subjects in Picchietti's study were diagnosed with ADHD. Associations between RLS and ADHD have been noted previously.1,26,27 RLS prevalence has been found to be higher in pediatric and adolescent subjects with ADHD than those not diagnosed with ADHD.12,28 Yilmaz et al. noted that the RLS prevalence rate was almost two-fold greater in adolescents aged 15-18 years with ADHD than in those adolescents without ADHD (6.3% vs. 3.2%).22 In the present study, univariate analyses showed that participants with symptoms consistent with RLS were more likely to admit to learning problems (14.3%) than those without RLS symptoms (8.0%), although the difference did not reach statistical significance. Potential participants with ADHD were excluded from the initial TuCASA study to avoid the effects of ADHD on home PSGs. Therefore, our data suggest that RLS symptoms have an adverse effect on cognition in adolescents and young adults independent of the presence of ADHD.
A small number of studies in adults have shown associations between RLS and health-related quality of life.8,20,29 Abetz et al. compared scores from the Medical Outcomes Study 36-Item Short Form (SF-36)30 between 85 adults with RLS and 2,474 subjects from the general population.8 Subjects with RLS had significantly lower scores for all SF-36 scales than subjects in the general population, including physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health, (p < 0.001 for all). The Physical and Mental Component summary scores (PCS and MCS) similarly were lower for subjects with RLS (p < 0.001 and p < 0.01, respectively). Fewer studies, however, have looked at RLS and health-related quality of life in children and adolescents, with most of these studies evaluating the association between RLS and psychiatric, anxiety, or depression comorbidities.28,31,32 For example, in a study by Pullen et al., comorbid psychiatric problems such as anxiety (11.5%), behavioral (10.9%), and mood disturbances (29.1%) were prevalent among 374 children and adolescents with RLS.28 In our study, adolescents and young adults with RLS symptoms had significantly lower scores for Psychosocial Health Summary and Total Scale scores than adolescents and young adults without RLS symptoms. Furthermore, lower Psychosocial Health Summary and Total Scale scores were significantly associated with trouble falling asleep; thus, trouble falling asleep may be one mediating sleep factor between RLS symptoms and reduced health-related quality of life.
There are several limitations to our study. First, the number of respondents to the follow-up sleep assessment was less than 50% of the original study population, raising the possibility that those respondents returning surveys were not fully representative of the initial cohort. Second, the number of cases identified as having symptoms consistent with RLS was relatively small. Nevertheless, the relatively low power of this study makes the statistically significant differences in health-related quality of life and trouble falling asleep between participants with symptoms consistent with RLS and no RLS more striking. Third, classification of RLS was determined by the sleep assessment questionnaire and not by in-person interviewing raising the possibility of case misclassification. However, we believe that any misclassification would be nondifferential, meaning that because symptoms were self-reported, and thus some may have over- or under-reported their symptoms, participants would have equal probability of being classified as either having symptoms consistent with RLS or no RLS. In addition, our classification for excessive daytime sleepiness (EDS) was done using questions that were more age-appropriate for a pediatric population and thus may not be comparable to those studies which have used the Epworth Sleepiness Scale,33 which is more suitable for an adult population. Because this third assessment was designed to be only a self-completed questionnaire, we were not able to obtain polysomnography data. We previously found that self-reports of sleep times were overestimated34 and that parental sleep-time reports35 overestimated their children's actual total sleep time; this fact might have contributed to the nonsignificant difference we saw with self-reported sleep onset latency and total sleep time by RLS status in this study. Similarly, we did not ask about prescribed medications that might induce or exacerbate RLS symptoms. Despite these limitations, the strengths of this analysis are a well-characterized general population of adolescents and young adults and a validated pediatric specific health-related quality of life instrument.
In summary, results from this study show that RLS symptoms were prevalent in 8.4% of adolescents and young adults, which is similar to previously published RLS prevalence rates in adults. RLS symptoms were significantly associated with greater odds of having trouble falling asleep and trouble falling asleep was associated with lower health-related quality of life. RLS symptoms also were associated positively with EDS. EDS may impact negatively health-related quality of life and concentration, which may contribute to learning problems. Further longitudinal studies are warranted to determine possible causal associations between RLS, EDS, and health-related quality of life.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest. This work was performed at the University of Arizona College of Nursing.
ACKNOWLEDGMENTS
The TuCASA study was supported by NHLBI grant HL 62373. Silva, G.E. was supported by NHLBI grant HL 62373-05A2S1.
REFERENCES
- 1.Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 2.Hening W, Walters AS, Allen RP, et al. Impact, diagnosis and treatment of restless legs syndrome (RLS) in a primary care population: the REST (RLS epidemiology, symptoms, and treatment) primary care study. Sleep Med. 2004;5:237–46. doi: 10.1016/j.sleep.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Trenkwalder C, Paulus W. Restless legs syndrome: pathophysiology, clinical presentation and management. Nat Rev Neurol. 2010;6:337–46. doi: 10.1038/nrneurol.2010.55. [DOI] [PubMed] [Google Scholar]
- 4.Walters AS, Picchietti DL, Ehrenberg BL, et al. Restless legs syndrome in childhood and adolescence. Pediatr Neurol. 1994;11:241–5. doi: 10.1016/0887-8994(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 5.Kotagal S, Silber MH. Childhood-onset restless legs syndrome. Ann Neurol. 2004;56:803–7. doi: 10.1002/ana.20292. [DOI] [PubMed] [Google Scholar]
- 6.Picchietti D, Allen RP, Walters AS, et al. Restless legs syndrome: prevalence and impact in children and adolescents--the Peds REST study. Pediatrics. 2007;120:253–66. doi: 10.1542/peds.2006-2767. [DOI] [PubMed] [Google Scholar]
- 7.Hornyak M, Kopasz M, Berger M, et al. Impact of sleep-related complaints on depressive symptoms in patients with restless legs syndrome. J Clin Psychiatry. 2005;66:1139–45. doi: 10.4088/jcp.v66n0909. [DOI] [PubMed] [Google Scholar]
- 8.Abetz L, Allen R, Follet A, et al. Evaluating the quality of life of patients with restless legs syndrome. Clin Ther. 2004;26:925–35. doi: 10.1016/s0149-2918(04)90136-1. [DOI] [PubMed] [Google Scholar]
- 9.Winkelman JW, Redline S, Baldwin CM, et al. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32:772–8. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chervin RD, Archbold KH, Dillon JE, et al. Associations between symptoms of inattention, hyperactivity, restless legs, and periodic leg movements. Sleep. 2002;25:213–8. [PubMed] [Google Scholar]
- 11.Rajaram SS, Walters AS, England SJ, et al. Some children with growing pains may actually have restless legs syndrome. Sleep. 2004;27:767–73. [PubMed] [Google Scholar]
- 12.Picchietti DL, Underwood DJ, Farris WA, et al. Further studies on periodic limb movement disorder and restless legs syndrome in children with attention-deficit hyperactivity disorder. Mov Disord. 1999;14:1000–7. doi: 10.1002/1531-8257(199911)14:6<1000::aid-mds1014>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 13.Kryger MH, Otake K. Low body stores of iron and restless legs syndrome: a correctable cause of insomnia in adolescents and teenagers. Sleep Med. 2002;3:127–32. doi: 10.1016/s1389-9457(01)00160-5. [DOI] [PubMed] [Google Scholar]
- 14.Quan SF, Goodwin JL, Babar SI, et al. Sleep architecture in normal Caucasian and Hispanic children aged 6-11 years recorded during unattended home polysomnography: experience from the Tucson Children's Assessment of Sleep Apnea Study (TuCASA) Sleep Med. 2003;4:13–9. doi: 10.1016/s1389-9457(02)00235-6. [DOI] [PubMed] [Google Scholar]
- 15.Goodwin JL, Kaemingk KL, Fregosi RF, et al. Clinical outcomes associated with sleep-disordered breathing in Caucasian and Hispanic children--the Tucson Children's Assessment of Sleep Apnea study (TuCASA) Sleep. 2003;26:587–91. doi: 10.1093/sleep/26.5.587. [DOI] [PubMed] [Google Scholar]
- 16.Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–41. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Varni JW, Limbers CA. The PedsQL 4.0 Generic Core Scales Young Adult Version: feasibility, reliability and validity in a university student population. J Health Psychol. 2009;14:611–22. doi: 10.1177/1359105309103580. [DOI] [PubMed] [Google Scholar]
- 18.Varni JW, Seid M, Knight TS, et al. The PedsQL 4.0 Generic Core Scales: sensitivity, responsiveness, and impact on clinical decision-making. J Beh Med. 2002;25:175–93. doi: 10.1023/a:1014836921812. [DOI] [PubMed] [Google Scholar]
- 19.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med. 2005;165:1286–92. doi: 10.1001/archinte.165.11.1286. [DOI] [PubMed] [Google Scholar]
- 21.Owens JA. Update in pediatric sleep medicine. Curr Opin Pulm Med. 2011;17:425–30. doi: 10.1097/MCP.0b013e32834ba901. [DOI] [PubMed] [Google Scholar]
- 22.Yilmaz K, Kilincaslan A, Aydin N, et al. Prevalence and correlates of restless legs syndrome in adolescents. Dev Med Child Neurol. 2011;53:40–7. doi: 10.1111/j.1469-8749.2010.03796.x. [DOI] [PubMed] [Google Scholar]
- 23.Arbuckle R, Abetz L, Durmer JS, et al. Development of the Pediatric Restless Legs Syndrome Severity Scale (P-RLS-SS): a patient-reported outcome measure of pediatric RLS symptoms and impact. Sleep Med. 2010;11:897–906. doi: 10.1016/j.sleep.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 24.Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med. 2009;10:134–8. doi: 10.1016/j.sleep.2007.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Picchietti DL, Arbuckle RA, Abetz L, et al. Pediatric restless legs syndrome: analysis of symptom descriptions and drawings. J Child Neurol. 2011;26:1365–76. doi: 10.1177/0883073811405852. [DOI] [PubMed] [Google Scholar]
- 26.Durmer JS, Quraishi GH. Restless legs syndrome, periodic leg movements, and periodic limb movement disorder in children. Pediatr Clin North Am. 2011;58:591–620. doi: 10.1016/j.pcl.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 27.Picchietti MA, Picchietti DL. Advances in pediatric restless legs syndrome: Iron, genetics, diagnosis and treatment. Sleep Med. 2010;11:643–51. doi: 10.1016/j.sleep.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 28.Pullen SJ, Wall CA, Angstman ER, et al. Psychiatric comorbidity in children and adolescents with restless legs syndrome: a retrospective study. J Clin Sleep Med. 2011;7:587–96. doi: 10.5664/jcsm.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Happe S, Reese JP, Stiasny-Kolster K, et al. Assessing health-related quality of life in patients with restless legs syndrome. Sleep Med. 2009;10:295–305. doi: 10.1016/j.sleep.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Ware JE, Snow KK, Kosinski M, et al. Boston, MA: The Health Institute, New England Medical Center; 1993. SF-36 Health Survey-manual and interpretation guide. [Google Scholar]
- 31.Picchietti DL, Stevens HE. Early manifestations of restless legs syndrome in childhood and adolescence. Sleep Med. 2008;9:770–81. doi: 10.1016/j.sleep.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 32.Sevim S, Dogu O, Kaleagasi H, et al. Correlation of anxiety and depression symptoms in patients with restless legs syndrome: a population based survey. J Neurol Neurosurg Psychiatry. 2004;75:226–30. [PMC free article] [PubMed] [Google Scholar]
- 33.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 34.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS) J Clin Sleep Med. 2007;3:622–30. [PMC free article] [PubMed] [Google Scholar]
- 35.Goodwin JL, Silva GE, Kaemingk KL, et al. Comparison between reported and recorded total sleep time and sleep latency in 6- to 11-year-old children: the Tucson Children's Assessment of Sleep Apnea Study (TuCASA) Sleep Breath. 2007;11:85–92. doi: 10.1007/s11325-006-0086-6. [DOI] [PubMed] [Google Scholar]


