Abstract
Objective
To form a normative set of responses to the GHABP questionnaire from a large regional dataset.
Design
Participants were asked to rate their hearing disability, handicap, hearing-aid (HA) use, HA benefit, HA satisfaction and residual (aided) disability on a five-point scale for four situations: quiet conversation, television (TV) listening, noisy conversation and group conversation. A subset of participants also estimated the time spent in these situations.
Study sample
1574 adults with normal to profound hearing thresholds participated.
Results
There was a significant relationship between increasing perceived disability and increasing hearing loss as given by the better-ear audiometric average (BEA). Responses for HA measures did not vary greatly with hearing loss: HA use was reported as high, whereas residual disability, HA benefit and satisfaction were all reported on average as moderate.
Conclusions
The results can be used as a normative dataset with which to evaluate individual responses in the clinic, where the GHABP provides a useful short-form questionnaire to engage the patient. The lack of systematic changes in hearing-aid related responses shows room for improvement in the benefit afforded by amplification.
Keywords: Hearing impairment, disability, handicap
1. INTRODUCTION
The Glasgow hearing-aid benefit profile (GHABP) questionnaire was designed to assess disability, handicap and hearing-aid (HA) benefit for operational management, both at the systematic and clinical levels (Gatehouse, 1999a). The GHABP asks respondents to consider four situations involving speech and to rate on a five-point scale their perceived initial (i.e., unaided) hearing disability, initial handicap, aided benefit, aided handicap, HA use and HA satisfaction (see Section 2.2 for a complete description of the questionnaire). The GHABP has played an important role in the UK-wide modernisation of the hearing-aid service (Davis et al., 2007). Our laboratory has been routinely administering the GHABP to all of our participants for about a decade, whether they wore no, one or two hearing aids. This data provides a large dataset on the GHABP as a clinical appraisal tool given a patient’s loss; that is, these results provide normative data on which individual responses can be better appraised. The data also provides important information on the perceived benefit of and satisfaction with hearing aids across a broad range of losses.
2. METHODS
2.1. Participants
A group of 1574 participants (788 female), aged 14-88 years (median 63 years), was recruited by post from attendees at clinics of the local hospitals from February 2002 to December 2011. Of these, 577 were unaided, 737 were unilaterally aided and 260 were bilaterally aided at the time of testing. Pure-tone air conduction thresholds were assessed, along with other audiometric measures. To classify participants based on hearing loss, we opted for the variable pure-tone threshold average as an improved means to classifying severity of impairment (Clark, 1981). It is computed from the three greatest (worse) of the four pure-tone thresholds in each ear at 500, 1000, 2000 and 4000 Hz. The better-ear variable pure-tone threshold average (BEA) was the lower of the two averages. For analysis, participants were divided into nine groups based on their BEAs in intervals of 10 dB HL. The distribution of participants is shown in Table 1. To eliminate BEA × HA groups with small n, all no-HA participants with BEA > 40 dB HL, unilateral participants with BEA ≤ 30 dB HL and bilateral participants with BEA ≤ 40 dB HL were combined into one group. While the number of participants in each group still varied from 72 to 301, the gender distribution and median age (with the exception of the lowest two BEA groups with no HAs) was well matched across groups.
Table 1.
Distribution of participants in study in groups based on number of hearing aids worn at time of response and their better-ear variable pure-tone average (BEA), showing number of participants, number of female participants in parentheses and median age of each group.
| BEA GROUP (dB HL) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 < BEA ≤ 10 | 10 < BEA ≤ 20 | 20 < BEA ≤ 30 | 30 < BEA ≤ 40 | 40 < BEA ≤ 50 | 50 < BEA ≤ 60 | 60 < BEA ≤ 70 | 70 < BEA ≤ 80 | 80 < BEA ≤ 125 | |
| None |
69 (35) 46 yrs |
169 (98) 55 yrs |
144 (65) 60 yrs |
97 (33) 62 yrs |
98 (41) 66 yrs |
||||
| Unilateral |
88 (38) 66 yrs |
145 (83) 62 yrs |
199 (96) 68 yrs |
145 (73) 66 yrs |
90 (47) 67 yrs |
70 (35) 65 yrs |
|||
| Bilateral |
26 (13) 66 yrs |
43 (23) 67 yrs |
57 (26) 66 yrs |
54 (31) 66 yrs |
41 (28) 67 yrs |
39 (23) 62 yrs |
|||
2.2. Questionnaire
There are four pre-specified elements or environments of the GHABP: (1) listening to the television when the volume is adjusted for others, (2) having a conversation with one person in quiet, (3) having a conversation on a busy street or in a shop, and (4) having a conversation with several people in a group. For each element, there is the initial yes/no question, “does this situation happen in your life?” If the response is yes (i.e., the situation did occur), the participant was then asked six questions for that environment about their (1) initial disability, (2) handicap, and if they wore hearing aids (997 of the 1574 participants), (3) HA use, (4) HA benefit, (5) residual disability and (6) HA satisfaction. For each of the six questions, scoring used the integers 1-5, with one representing “none” and five representing “all.”
To assess initial disability in each situation, the question was “how much difficulty do you have in this situation?” Participants selected one of five possible responses ranging from “no difficulty” to “cannot manage at all.” If their response was “no difficulty,” the remaining five questions were marked as “not applicable” for that environment; if they responded with anything greater than “no difficulty,” responses were obtained for the five remaining questions. To assess (initial) handicap, the question was “how much does any difficulty in this situation worry, annoy or upset you?” with responses ranging from “not at all” to “very much indeed.” To assess HA use, the question was “in this situation, what proportion of the time do you wear your hearing aid?” with responses ranging from “never/not at all” to “all the time.” To assess HA benefit, the question was “in this situation, how much does your hearing aid help you?” with responses ranging from “no use at all” to “hearing is perfect with aid.” To assess residual (aided) disability, the question was “in this situation, with your hearing aid, how much difficulty do you now have?” with responses ranging from “no difficulty” to “cannot manage at all” (i.e., same as the initial-disability responses). Finally, to assess HA satisfaction, the question was “for this situation, how satisfied are you with your hearing aid?” with responses ranging from “not satisfied at all” to “delighted with aid.”
2.3 Procedure
After completing audiometric assessment, each participant was given a series of short questionnaires on their hearing, including the GHABP. All questionnaires were administered verbally by a trained member of the Institute staff. Most questionnaires (n = 1326) were recorded on paper; later questionnaires (n = 248) were recorded digitally using a laptop computer. The paper versions of the GHABP included entries on the estimate of time spent, in hours per week, in each situation. The paper versions also included optional, additional entries for situations of interest to the individual. Only 73 of the 1326 participants who were asked for additional entries gave any examples. Given the small number of additional entries, we did not analyze the responses to these entries.
3. RESULTS
For all questions within a hearing-aid group (none, unilateral or bilateral), results were analysed with a repeated-measures analysis of variance with situation and BEA as within- and between-group factors, respectively. The numerical results of these analyses are shown in Table 2. Given the large sample size, most analyses yield statistically significant results. We have therefore included estimates of effect size (partial η2). Effect sizes were deemed small, medium or large based on the conventional criteria set by Cohen (1988) – 0.01, 0.06 and 0.14, respectively – though it is arguably more instructive to compare the effect sizes within these results (Lenth, 2001). Also, as sphericity could not be assumed, within-subject effects were based on the Greenhouse-Geisser correction for degrees of freedom.
Table 2.
Analyses of variance results for each participant group (those without aids, aided unilaterally and aided bilaterally) showing the degrees of freedom (factor, error), F statistic and partial η2 (estimate of effect size) of hearing loss (HL), situation (S) and interaction (HL×S) factors for each question. The number of asterisks (1, 2 or 3) indicates factors that were statistically significant at the p < 0.05, 0.01 and 0.001 levels, respectively.
| Group | Factor | Initial disability | Handicap | HA use | HA benefit | Residual disability | HA satisfaction |
|---|---|---|---|---|---|---|---|
| None | HL |
df = 4, 502 F = 40.86*** η2 = 0.25 |
4, 260 12.34*** 0.16 |
||||
| S |
df = 2.9, 1441.6 F = 262.53*** η2 = 0.34 |
2.6, 695.4 41.40*** 0.14 |
|||||
| HL×S |
df = 11.5, 1441.6 F = 4.00*** η2 = 0.03 |
10.7, 695.4 1.99* 0.03 |
|||||
| Unilateral | HL |
df = 6, 615 F = 33.92*** η2 = 0.25 |
6, 505 7.33*** 0.08 |
6, 425 7.08*** 0.09 |
6, 370 1.28 |
6, 371 3.24** 0.05 |
2.7, 990.6 33.73*** 0.08 |
| S |
df = 2.8, 1720.2 F = 209.12*** η2 = 0.25 |
2.8, 1417.3 55.16*** 0.10 |
2.8, 1196.6 4.23* 0.01 |
2.9, 1058.2 49.48*** 0.12 |
2.8, 1056.3 76.24*** 0.17 |
6, 369 2.53* 0.04 |
|
| HL×S |
df = 16.8, 1720.2 F = 4.45*** η2 = 0.04 |
16.8, 1417.3 2.93*** 0.03 |
16.9, 1196.6 1.576 |
17.2, 1058.2 1.86* 0.03 |
17.1, 1056.3 1.27 |
16.1, 990.6 1.21 |
|
| Bilateral | HL |
df = 5, 215 F = 21.89*** η2 = 0.34 |
5, 191 3.03* 0.07 |
5, 192 2.50* 0.06 |
5, 187 1.27 |
5, 186 1.96 |
5, 187 1.07 |
| S |
df = 2.4, 521.7 F = 85.18*** η2 = 0.28 |
2.6, 499.8 15.47*** 0.07 |
2.6, 504.2 1.41 |
2.9, 547.2 71.75*** 0.28 |
2.8, 518.5 98.71*** 0.35 |
2.9, 538 66.44*** 0.26 |
|
| HL×S |
df = 12.1, 521.7 F = 2.87*** η2 = 0.04 |
13.1, 499.8 1.96* 0.05 |
13.1, 504.2 1.13 |
14.6, 547.2 1.41 |
13.9, 518.5 1.08 |
14.4, 538 1.21 |
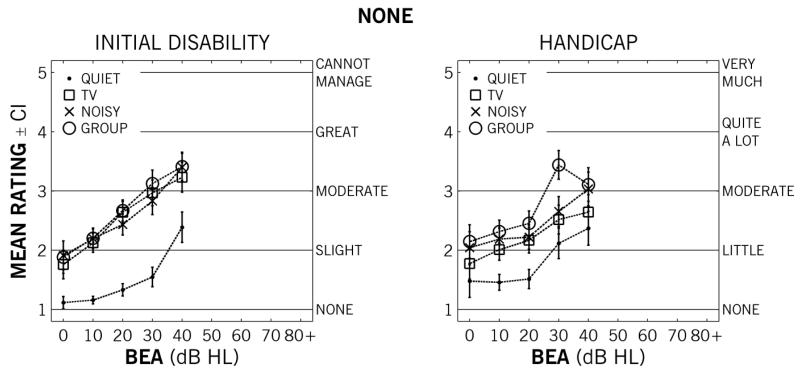
3.1. Unaided results
Figure 1 shows the mean ratings for those without hearing aids of initial disability and handicap – the only questions asked of those without aids – as a function of hearing loss. For the initial-disability ratings (left panel), there were large, statistically significant main effects of hearing loss and situation, and a small significant interaction between situation and hearing loss. Post-hoc comparisons indicated that ratings significantly increased from the lowest two BEAs (0-20 dB HL), and ratings were significantly higher by approximately one scale point for the complex situations – TV, noisy and group conversation – compared to the quiet conversation. That is, mean disability ratings for unaided respondents increased from none to slight difficulty for quiet conversation and slight to moderate difficulty for complex situations as a function of hearing loss. For the handicap ratings (right panel), there were also statistically significant, medium-sized main effects of hearing loss and situation, and a small, significant interaction. The handicap ratings for the lower three BEA groups (0-30 dB HL) were significantly lower (p < 0.01) than those with greater (worse) BEAs. In terms of situations, handicap ratings were lowest for quiet conversation, a half point greater for TV and noisy conversation, and a point greater for group conversation.
Figure 1.
Mean ratings for respondents not wearing hearing aids (n = 577) of initial disability (left panel) and handicap (right panel) as a function of better-ear (variable pure-tone threshold) average in each situation: quiet conversation (dots), TV listening (squares), noisy conversation (crosses) and group conversation (circles). The scale labels for each question are shown to the right of each panel. Error bars show 95% confidence intervals.
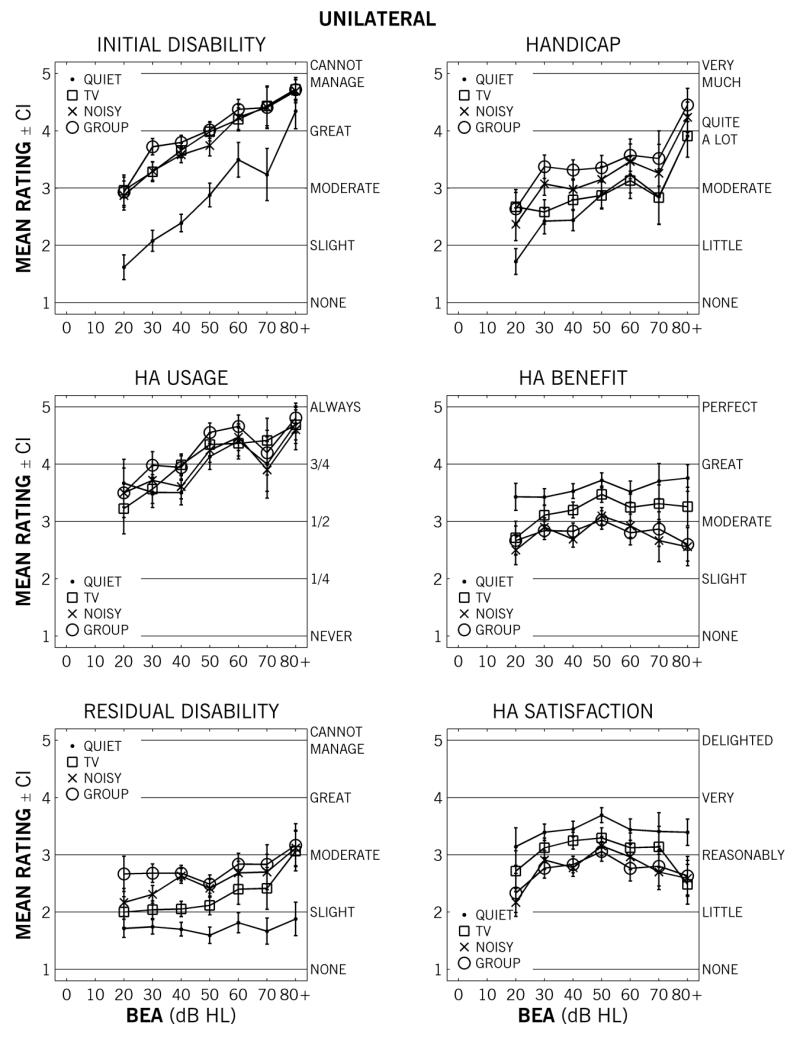
3.2. Unilateral results
Figure 2 shows the mean ratings for those wearing one hearing aid as a function of hearing loss. For initial disability (top left panel), there were relatively large, significant main effects of hearing loss and situation, as well as an interaction. The disability ratings increased from none-to-slight to just above great difficulty for quiet conversation and from moderate difficulty to just below cannot manage at all for the non-quiet situations. For (initial) handicap (top right panel), there were medium-sized, significant main effects of hearing loss and situation, and also a small, significant interaction. Handicap ratings increased with BEA from little to moderate annoyance to quite a lot; handicap increased roughly a quarter of a scale point from quiet to TV to noisy to group situations. For HA use (middle left panel), there was a smaller, significant main effect of hearing loss and a very small, significant main effect of situation but no interaction. Across situations, self-rated HA use increased – except for a slight dip for the 70-80 dB HL participants – from 54% to 95%. For HA benefit (middle right panel), there was a significant main effect of situation and a small, significant interaction with hearing loss, but no main effect of hearing loss. HA benefit increased from slight-to-moderate for noisy and group conversations, moderate for the TV conversation and moderate-to-great for quiet conversation. For residual (aided) disability (bottom left panel), there was a small significant main effect of hearing loss and a large main effect of situation, but no significant interaction. Finally, for ratings of HA satisfaction (bottom right panel), there was a medium-sized significant main effect of situation, a smaller, significant main effect of hearing loss, and no significant interaction.
Figure 2.
Mean ratings for respondents wearing one hearing aid (n = 737) of initial disability (top left panel), handicap (top right panel), hearing-aid use (middle left panel), hearing-aid benefit (middle right panel), residual disability (bottom left panel) and hearing-aid satisfaction (bottom right panel) as a function of better-ear (variable pure-tone threshold) average in each situation: quiet conversation (dots), TV listening (squares), noisy conversation (crosses) and group conversation (circles). The scale labels for each question are shown to the right of each panel. Error bars show 95% confidence intervals.
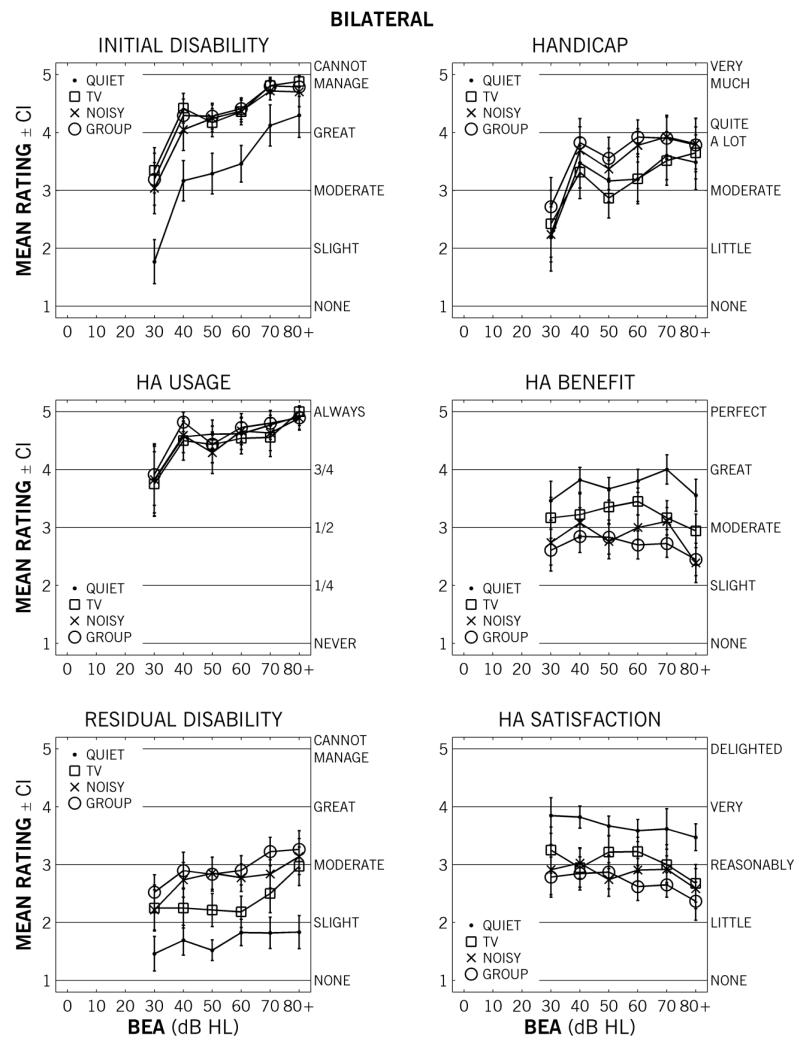
3.3. Bilateral results
Figure 3 shows mean ratings for those wearing two hearing aids as a function of hearing loss. The data are similar to those for unilateral responses. For initial disability, there were relatively large, significant main effects of hearing loss and situation, as well as a smaller, significant interaction. For quiet conversation, initial disability increased from slight for those with less than 40 dB HL to great for those with greater than 70 dB HL; for TV, street and group conversation, ratings increased from moderate to cannot manage. For handicap, there were relatively small, significant main effects of hearing loss and situation, as well as an interaction. Handicap ratings increased from little-to-moderate annoyance for those with BEAs ≤ 40 dB HL, to moderate-to-quite-a-lot annoyance for all participants with BEAs > 40 dB HL. For HA use, there was only a small, significant main effect of hearing loss, increasing with BEA from 78% to 100%. For HA benefit, there was only a relatively large significant main effect of situation; benefit for quiet conversation was rated, on average, half a point higher than TV listening and a point higher than noisy or group conversation. For residual disability, there was only a relatively large significant main effect of situation. Residual disability was between none and slight difficulty for quiet conversation, between slight and moderate difficulty for TV listening, and moderate difficulty for noisy and group conversation. For HA satisfaction – similar to HA benefit and residual disability – there was only a relatively large, significant main effect of situation. Across hearing losses, mean responses were between reasonably and very satisfied for quiet conversation, and between little and reasonably satisfied for the other three, non-quiet situations.
Figure 3.
Mean ratings for respondents wearing two hearing aids (n = 260) of initial disability (top left panel), handicap (top right panel), hearing-aid use (middle left panel), hearing-aid benefit (middle right panel), residual disability (bottom left panel) and hearing-aid satisfaction (bottom right panel) as a function of better-ear (variable pure-tone threshold) average in each situation: quiet conversation (dots), TV listening (squares), noisy conversation (crosses) and group conversation (circles). The scale labels for each question are shown to the right of each panel. Error bars show 95% confidence intervals.
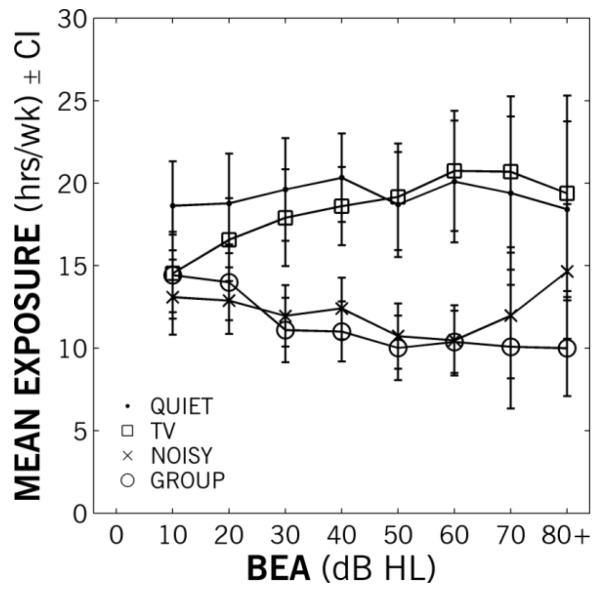
3.4. Exposure time
In the original paper version of the GHABP completed by 1326 of the 1574 total participants, the participant was also asked how much time they estimated they spent in each of the situations. Of the 1326 participants who were asked, 902 of them gave response(s) greater than zero for at least one situation. The mean exposure time in hours per week are shown as a function of hearing-loss group in Figure 3. There were no significant differences in exposure-time reports between those without hearing aids (n = 317), with one hearing aid (n = 450) and those with two (n = 135); hence, results are shown collapsed across participant groups. There was only a small, significant main effect of hearing loss for the TV listening situation [F(8,1311) = 4.17; p < 0.001; η2 = 0.025]. Overall, the amount of time spent in quiet conversation or listening to TV (mean 18.7 hours/week) was significantly greater [t(901) = 13.03; p < 0.001] than the time spent in noisy or group conversation (mean 11.9 hours/week).
Figure 4.
Mean exposure time per week as a function of better-ear variable pure-tone average (BEA) group for quiet conversation (dots), television listening (squares), noisy conversation (crosses) and group conversation (circles). Error bars show 95% confidence intervals.
3.5. Results across participants
As all participants self-rated their initial hearing disability and handicap, we can examine the sensitivity and specificity of these self ratings compared to BEA. Neither the initial disability nor handicap question in the quiet situation had high sensitivity or specificity compared to previous results (Davis et al., 2007). Using BEA ≥ 30 dB HL and response of 2 for either initial disability (slight difficulty) or handicap (little annoyance) as the criteria for dichotomisation, the specificity was 73% and 70%, respectively, and the sensitivity was 81% and 72%, respectively. Averaging across situations and using a response of 3 for initial disability (moderate difficulty) yielded similar sensitivity and specificity. We do not believe that these sensitivities and specificities are high enough to warrant the use of these questions alone as a screening tool.
HA use was the only HA-related question where there were significant differences between unilateral and bilatereal HA wearers: bilaterally fitted respondents with milder losses (BEA ≤ 50 dB HL) rated their HA use – averaged across situations – significantly higher than unilateral cohorts (4.3 vs. 3.7; t(352) = 3.49; p < 0.001). The only significant gender response differences (across all participants) were higher initial-disability ratings in quiet conversation[t(1419) = 3.82; p < 0.001], TV listening [t(1524) = 3.72; p < 0.001] and group conversation [t(1532.9) = 2.46; p < 0.05], and handicap ratings in all situations for females [all t(1109-1405.5) > 4.1; all p < 0.001], though all of these differences were less than half a scale point. The only significant gender difference in exposure time was for TV listening [t(1297) = 2.68; p < 0.01], with males reporting 2.4 more hours per week in front of the TV.
4. DISCUSSION
The current study reports on a large dataset to assist in the interpretation of GHABP responses with individual patients. As Gatehouse stated in his original instructional package for the GHABP, “I believe that although the raw scores can be informative, it is by association with reference data gathered from one’s own clinical circumstance using the particular patients and hearing aids that are appropriate, that the maximum value from the GHABP is derived” (1999b, p. 38). While the current data is from one circumstance, it can be used as a simple reference for the clinician to better understand the individual patient’s perception of their disability, handicap and possibly HA benefit. There are no definitive answers on the best remediation given a particular response, but responses well outside these normative means for the patient’s hearing-loss group may indicate the need for another method of rehabilitation. If clinical time is at a premium, the test could be reduced to two situations: quiet conversation and noisy conversation, as there were clear response differences across questions for quiet and non-quiet situations, but few differences between noisy- and group-conversation situations.
In terms of the systematic responses to the HA-specific questions, the mean results shown here (Figures 2 and 3) can be interpreted as both positive and negative findings. As a positive, residual disability was reduced on average for those with more severe hearing losses. Another positive is that HA use was rated highly – from three-quarters to all of the time – although self-reported use has been previously shown to be inflated (Brooks, 1979). Also, residual disability on average was rated significantly lower than initial disability for all but the mildest hearing losses, whether unilaterally or bilaterally fitted. A negative is the lack of change in HA benefit with hearing loss. At issue is how much interpretation should be given to the relatively flat lines seen in the mean responses to residual disability, benefit and satisfaction as a function of hearing loss. It is important to consider that these responses were gathered after a clinical visit in a research laboratory, so that responses are tempered by an already established decision process. That is, each respondent has already made a choice on remediation, so some response homogenization – gravitation towards a central response – is possible. Furthermore, the GHABP is answered on a discrete five-point scale, which may be too insensitive for some systematic uses or revealing small effects. The GHABP as part of the modernized hearing-aid service in the UK is generally implemented during the first clinical visit (e.g., Davis et al., 2007). We believe that this questionnaire still has clear value in engaging the patient, and potentially comparing responses longitudinally, but, based on the hearing-aid related responses here, may not illuminate any issues if used to audit service (i.e., as a sensitive, stand-alone measure of hearing-aid benefit).
The exposure data – the time spent in each of the situation – showed no differences across hearing loss except for a significant rise in average time spent listening to TV. In a recent study of listening habits, Wu and Bentler (2012) found little difference in the time spent in various listening situations as self-reported by among middle-aged (40-65 yrs) and older (65-88 yrs) hearing-impaired individuals. They found instead that measures not directly linked to hearing (e.g., social networking indices) had significantly decreased for the older, more impaired group. Along with the current results, it appears as though self reports of listening activity do not vary across age or impairment. To better understand the variation in impact to the patient, the focus of subjective questioning may need to shift from listening to general socialization.
5. SUMMARY
In conclusion, the results provide a normative dataset on which to gauge individual responses to the GHABP questionnaire. The current results also show a clear relationship between the subjective estimate of hearing difficulty and the pure-tone audiogram. The lack of systematic changes in hearing-aid related responses show either room for improvement in the benefit afforded by amplification or a potential limit in the perceived benefit that warrants further, specific investigation. The hearing-aid responses, however, suggest caution in interpreting group-average outcomes. A subsequent questionnaire, the Speech, Spatial and Quality of Life Questionnaire, has shown utility in parsing systematic differences (Noble & Gatehouse, 2006), and it or its abbreviated version (Noble et al., 2013) is recommended when the group differences are under scrutiny. Nevertheless, as a short-form method to discuss intervention with an individual patient, the GHABP still has merit.
ACKNOWLEDGMENTS
The authors thank Dr. David Bagueley and two anonymous reviewers for their comments, Fiona Guy, Helen Lawson, Neil Kirk, David McShefferty and Sharon Suller for their invaluable assistance in the collection of data, and Oliver Zobay for insightful suggestions on an earlier draft. The Scottish Section of IHR is supported by intramural funding from the Medical Research Council (grant number U135097131) and the Chief Scientist Office of the Scottish Government.
LIST OF ABBREVIATIONS
- BEA
Better-ear pure-tone audiometric average
- GHABP
Glasgow Hearing-Aid Benefit Profile
- HA
Hearing aid
- HL
Hearing loss
7. REFERENCES
- Brooks D. Counselling and its effect on hearing aid use. Scand Audiol. 1979;8:101–107. doi: 10.3109/01050397909076308. [DOI] [PubMed] [Google Scholar]
- Clark J. Uses and abuses of hearing loss classification. ASHA. 1981;23:493–500. [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Lawrence Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I. Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models. Health Technol Assess. 2007;11 doi: 10.3310/hta11420. [DOI] [PubMed] [Google Scholar]
- Gatehouse S. Glasgow hearing aid benefit profile: Derivation and validation of a client-centered outcome measure for hearing aid services. J Am Acad Audiol. 1999a;10:80–103. [Google Scholar]
- Gatehouse S. The Glasgow hearing aid benefit profile - Information package. 1999b http://www.ihr.mrc.ac.uk/downloads/products/questionnaires/ghabp-ip.zip. [Google Scholar]
- Lenth R. Some practical guidelines for effective sample size determination. Am Stat. 2001;55:187–193. [Google Scholar]
- Noble W, Gatehouse S. Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the speech, spatial, and qualities of hearing scale (SSQ) Int J Audiol. 2006;45:172–181. doi: 10.1080/14992020500376933. [DOI] [PubMed] [Google Scholar]
- Noble W, Jensen N, Naylor G, Bhullar N, Akeroyd M. A short form of the Speech, Spatial and Qualities of Hearing scale suitable for clinical use: The SSQ 12. Int J Audiol. 2013;52:409–412. doi: 10.3109/14992027.2013.781278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Bentler R. Do older adults have social lifestyles that place fewer demands on hearing? J Am Acad Audiol. 2012;23:697–711. doi: 10.3766/jaaa.23.9.4. [DOI] [PubMed] [Google Scholar]