Abstract
AIM
To assess the consecutive recurrence following early success of intermittent exotropia surgery and to determine the clinical factors that affect the survival.
METHODS
One hundred and thirty-five patients who underwent intermittent exotropia surgery and experienced early surgical success [≤5 prism diopters (PD) esophoria (E) to ≤10 PD exophoria (X) on the postoperative sixth month] were enrolled in this study. Their consecutive survival on the postoperative first year, second year and third year and at the last visit of fourth year or more, and the factors that might affect their survival, were analyzed. The final surgical outcomes after the postoperative fourth year were also investigated by dividing the patients into the success group (≤5 PD E to ≤10 PD X) and the failure group (>5 PD esodeviation or >10 PD exodeviation)
RESULTS
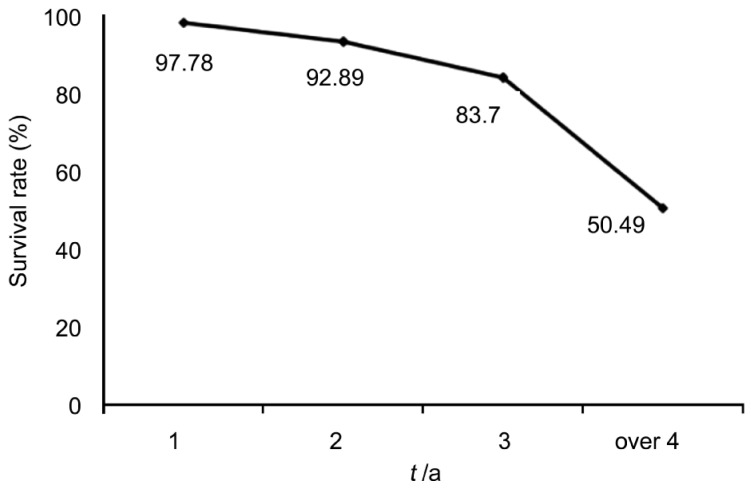
The survival rates from the Kaplan-Meier analysis were 97.78%, 92.89%, 83.70% and 50.49% on the postoperative first, second and third years and fourth year or more, respectively. None of the clinical factors was determined to have affected the survival. The amount of the exodrift was largest (2.29 PD) between the first year and the second year, and smallest (1.47 PD) between the fourth year and the last visit. Sixty-three patients had their final visit after the postoperative fourth year, and 29 of them were in the failure group. Twenty-five patients in the failure group had an intermittent exotropia (IXT) of <20 PD with good to fair distant fusion; two had an IXT of <20 PD with poor distant fusion; one had an IXT of ≥20 PD with fair distant fusion; and another had delayed-onset consecutive esotropia. The exodeviation on the postoperative sixth month was smaller in the success group than in the failure group (2.81 PD vs 5.86 PD, P=0.012). The reoperation rate for recurrent IXT was 3.7%.
CONCLUSION
The survival rate steadily decreases with the exodrift, but the amount of the exodrift decreases with long-term follow-up. The final outcomes demonstrate favorable results via surgical success or small-angle IXT with good fusion in most of the patients. A smaller deviation on the postoperative sixth month is associated with long-term survival.
Keywords: long-term outcome, survival analysis, intermittent exotropia surgery
INTRODUCTION
Intermittent exotropia (IXT) is a major primary comitant strabismus in childhood[1]. It has variable nonsurgical treatment options such as patching, orthoptic therapy and over-minus lenses[2],[3], but surgical correction is the only curative therapy for IXT. Although surgery for IXT is an easy procedure and highly satisfying for both surgeons and patients during the early postoperative period, many reports have indicated a decrease in the rate of surgical success after the progress of an exotropic drift[4],[5].
The postoperative change in the IXT is variable during the several early months after the surgery. Most cases show an initial overcorrection and then a change to orthotropia or undercorrection according to the exodrift[6],[7]. Consecutive esotropia could occasionally develop[8]. As for the postoperative course of IXT, Ruttum[9] suggested the almost unpredictability of the initial postoperative alignment and occasionally, even of the direction of the early postoperative drift. These short-term events would be related to the preoperative conditions that cause erroneous determination of the target angle, dynamic changes in the postoperative wound healing process and re-adopted convergence/divergence tonus during the initial postoperative period. It was considered that the short-term changes would stabilize in about six months after the surgery and that the surgical results would be either early surgical failure (consecutive esotropia and undercorrected exotropia) or surgical success (postoperative orthophoria). Recurrence with time is a noticeable and frustrating phenomenon in intermittent exotropia surgery, and there is still insufficient information on the long-term outcomes[4]. Besides, if the recurrence rate was calculated with the inclusion of the patients who had variable early results without clear discrimination of the cases of early surgical failure (especially of undercorrected exotropia after the stabilization of the initial postoperative change), it could enhance the recurrence rate in the long-term results.
This study was conducted to assess the recurrence of intermittent exotropia surgery after the postoperative sixth month and to find the clinical factors that affect its long-term outcome. Patients who had experienced early surgical success were selected to assess the recurrence with time, and survival analysis was performed with investigation of the factors that might affect the survival. The final long-term outcomes after the postoperative fourth year were also investigated.
SUBJECTS AND METHODS
This retrospective, single-center study included 135 patients who underwent intermittent exotropia surgery by a single surgeon between January 2001 and March 2006 and experienced early surgical success. We reviewed and analyzed the data from January to June in 2012. Early surgical success was defined as an eye alignment of ≤5 prism diopters (PD) esophoria (E) and ≤10 PD exophoria (X) on the postoperative sixth month. Patients with neurological or medical abnormalities, amblyopia or ocular disease, except for eye deviation, were excluded. This study was conducted following the tenets of the Declaration of Helsinki.
The target angle at the time of the surgery was the distant exodeviation that was measured with the fixation target at 6 m. To determine the target angle, one-hour occlusion was performed on the nondominant eye and an alternate prism cover test was performed before the patients were allowed to see with both eyes. The routine follow-up schedule after the surgery was on the first day, fourteenth day, first month, third month, sixth month and first year; and after the postoperative first year, every six months. In each postoperative visit, a visual acuity test, refractive correction, angle measurement with an alternate prism cover test, and a near stereoacuity test were performed. The fusion control grade of the exodeviation (FCGX) was checked preoperatively and recorded in the cases of a recurrent exotropia of more than 10 PD, and was graded as good, fair or poor fusion control, with the fixation target at 6 m. In the office, good control was when the patient “broke” only after the cover test and resumed the fusion rapidly without the need to blink or have a refixation. Patients who blinked or had a refixation to control the deviation after the disruption with the cover test were deemed to have had fair control, and patients who “broke” spontaneously without any form of fusion disruption, poor control[10],[11].
The surgeon measured the deviation angle and assessed the FCGX. The postoperative findings were collected from the medical records at the visits on the sixth month, first year, second year and third year, and at the last visit of fourth year or more. The data for the visits of “fourth year or more” were defined as those on the last visit at postoperative fourth year or after the postoperative fourth year. By defining “survival” as the maintenance of the surgical success (≤5 PD E and ≤10 PD X), survival analysis was performed on each postoperative visit from the first year to fourth year or more. The patients who showed angle of deviaition at distance ≥20 PD and who showed poor fusion control of distant deviation with angle of deviation at distance >10 PD to <20 PD were recommended reoperation during follow up after surgery. If the patients underwent reoperation during the study period, termination of follow-up for this study was considered. Consequently, they were excluded from the calculation of survival rate for the subsequent terms after the reoperation. Their reoperation was not considered in this study, so they were not classified with the subjects who had secondary surgery for analysis. The patients who had a final follow-up of four years or more were divided into the success group (≤5 PD E to ≤10 PD X) and the failure group (>5 PD esodeviation or >10 PD exodeviation), and their eye alignments and FCGX were further investigated and the amounts of their early postoperative deviation were compared.
The effect of the preoperative and operative clinical factors on the survival was assessed. The factors included the patient's age at the surgery, the experience of orthoptic treatment via part-time patching therapy or convergence exercise, the wearing of myopic glasses, the surgery sequence and the accompanying vertical strabismus surgery. The surgeon prescribed patching therapy and/or a convergence exercise by judging whether the postoperative angle tended to increase or the bifoveal fusion tended to weaken on each follow-up visit. The occlusion was performed on the dominant eye or on two eyes in alternate fashion if the dominant eye could not be defined. Fully corrected or -0.25 diopter over-corrected glasses were prescribed for the patients who had a myopic refractive error (a ≥0.75 diopter spherical equivalent), and the effect of the patient's myopic spectacle wear was also investigated. The patients who had secondary surgery for recurrent IXT were also included. The patients who underwent the surgery on their cyclovertical muscles at the time of their exotropia surgery were also included. The effects of the surgery sequence (primary surgery or secondary surgery) and the accompanying vertical strabismus surgery on the survival were also assessed.
The statistical analysis was performed with the SPSS 12.0 statistical program. The survival rate was analyzed via Kaplan-Meier survival analysis, and the clinical risk factors that affected the survival were evaluated using Cox's proportional hazard model with survival analysis. Kaplan-Meier survival analysis is a widely used method of assessing the survival pattern in a group of subjects who had variable follow-up periods[5],[12]. The independent t test was used to compare the deviation angles.
RESULTS
Table 1 shows the clinical characteristics of the 135 subjects. Seventy-two of them were female, and their average age at their surgery was 9.37±5.68 (3-37)y. The mean follow-up time was 3.86±1.89y (range: 1-8y). The mean preoperative angle of the exotropia was 25.71±7.02 (12-60) PD. A total of 126 patients had primary surgery. Among them, 114 patients underwent unilateral or bilateral rectus recession; ten, unilateral recess-resect surgery; and two, three horizontal muscle surgeries. Among the nine patients who had secondary surgery, five had bilateral medial rectus resection; three, unilateral recess-resect surgery; and one, three horizontal muscle surgeries. Nineteen patients had vertical muscle surgery with their exotropia surgery. Sixteen of them underwent bilateral inferior oblique muscle recession and three, unilateral superior rectus recession.
Table 1. Clinical characteristics of the 135 patients.
| Clinical characteristics | n (%) | |
| Age at surgery (a) | ||
| 3-6 | 37 (27.4) | |
| 7-10 | 73 (54.1) | |
| 11-20 | 18 (13.3) | |
| 20-37 | 7 (5.2) | |
| Preoperative angles | ||
| <20 PD | 43 (31.8) | |
| ≥20 PD or <30 PD | 71 (52.3) | |
| ≥30 PD | 21 (15.9) | |
| Surgery sequence | ||
| Primary surgery | 126 (93.4) | |
| Secondary surgery | 9 (6.6) | |
| Last follow-up(a) | ||
| 1 | 135 (100) | |
| 2 | 131 (97.3) | |
| 3 | 88 (65.2) | |
| ≥4 | 63 (46.7) | |
PD: prism diopter.
The Kaplan-Meier survival rate was 97.78% on the first year, 92.89% on the second year, 83.70% on the third year and 50.49% on fourth years or more (Figure 1). Table 2 shows the amounts of the postoperative angle changes in time in the patients who underwent the postoperative examinations on their postoperative visits in the corresponding period to calculate the angle change. Most of the patients had an exodrift, but some showed an esodrift. The mean change in the exodrift was largest between the first and second years, and smallest between the fourth year and the last follow-up. Conversely, the amount of the esodrift was largest between the fourth year and the last follow-up (P=0.045, ANOVA), and the proportion of the patients with esodrift was also highest in that period (P=0.026, Chi-square test). Throughout the study period, five patients (3.7%) underwent reoperation for recurrent IXT.
Figure 1. Kaplan-Meier survival curve after intermittent exotropia surgery.
Table 2. Postoperative angle change with time.
| Duration interval | Mean change±standard deviation (PD) |
| 6thmo-1sta (1n=131) | Exodrift (n=114) 1.90±2.21 |
| Esodrift (n=17) 3.65±1.71 | |
| 1sta-2nda (1n=119) | Exodrift (n=105) 2.29±2.91 |
| Esodrift (n=14) 3.07±1.87 | |
| 2nda-3rda (1n=86) | Exodrift (n=70) 1.97±3.87 |
| Esodrift (n=16) 3.06±2.16 | |
| 3rda-4tha (1n=56) | Exodrift (n=49) 1.68±3.13 |
| Esodrift (n=7) 4.56±2.99 | |
| 4tha-2last visit (1n=50) | Exodrift (n=38) 1.47±2.23 |
| Esodrift (n=12) 5.08±6.41 |
1Number of patients who took the postoperative examinations at either postoperative visit in the corresponding period to calculate the angle change; 2Average number of years in the last follow-up =5.63±1.12 (range: 4-8y).
For the final long-term outcomes, a total of 63 patients had their last follow-up at fourth year or more. The average number of the last follow-up years was 5.63±1.12 (range: 4-8y). Among the 63 patients, 50 made the visits more than once between the fourth year and the last follow-up, and two patients were counted in the success group on the postoperative fourth year and dropped out on the following visit (Table 2). One patient showed survival with 8 PD exophoria up to the postoperative sixth year and dropped out on the postoperative seventh year with a recurrent IXT of 16 PD. Another patient wore fresnel prism glasses for the delayed-onset consecutive esotropia on the postoperative seventh year. In that case, a 3 PD esophoria occurred in the exam on the fourth-year visit, and the angle of the esotropia increased with diplopia. The other 48 patients did not experience a change in their status between the fourth year and the last follow-up. The mean exodeviation angle on the the final visit was 10.14±6.24 PD. In the last examination, 34 patients were counted in the success group and 29, in the failure group. Twenty-seven patients in the failure group demonstrated a recurrent IXT of ≥10 PD and <20 PD. Twenty of them had a good FCGX; five, a fair FCGX; and two, a poor FCGX. One patient showed a recurrent IXT of ≥20 PD and a fair FCGX. Another patient had delayed-onset consecutive esotropia, as mentioned previously.
Table 3 compares the early postoperative eye alignments of the two groups in the final outcomes. The amounts of the initial overcorrection on the postoperative first day of the success group and the failure group (P=0.823) did not significantly differ. The exodeviation on the postoperative sixth month was significantly smaller in the success group than in the failure group (P=0.012).
Table 3. Comparison of the angle of deviation at the postoperative first day and the sixth month between the success group and the failure group in the final surgical outcomes after the postoperative fourth year.
| Group | Postoperative angle of deviation |
|
| 1std | 6thmo | |
| Success (n=34) | 9.23±6.26 E | 2.81±3.52 X |
| Failure (n=29) | 9.82±8.66 E | 5.86±3.71 X |
| P | 0.823 | 0.012 |
SD: standard deviation; E: esodeviation; X: exodeviation.
x±s
None of the preoperative and operative factors was determined to have significantly affected the survival (Table 4).
Table 4. Relative risk according to the clinical factors.
| Characteristics | 1Odds Ratio | P |
| Age at surgery | ||
| ≥10a (n=38) | 1.633 | 0.268 |
| <10a (n=97) | ||
| Preoperative angle | ||
| ≥20 PD (n=92) | 1.095 | 0.690 |
| <20 PD (n=43) | ||
| Preoperative FCGX | ||
| Good to fair (n=66) | 1.720 | 0.182 |
| Poor (n=69) | ||
| Accompanied vertical strabismus surgery | ||
| - (n=117) | 1.120 | 0.807 |
| + (n=18) | ||
| Surgery sequence | ||
| Secondary surgery (n=9) | 1.143 | 0.862 |
| Primary surgery (n=126) | ||
| Type of surgery | ||
| BLR recession (n=114) | 1.136 | 0.834 |
| R&R (n=21) | ||
| Orthoptic treatment | ||
| - (n=10) | 1.303 | 0.726 |
| + (n=125) | ||
| Myopic refractive error with spectacle wear | ||
| - (n=61) | 1.772 | 0.081 |
| + (n=74) |
PD: prism diopter; FCGX: fusion control grade of the exodeviation; BLR: bilateral lateral rectus recession; R&R: monocular recess-resect surgery;1Cox proportional hazard model.
DISCUSSION
In most previous studies, IXT showed a tendency to demonstrate an exotropic drift over time and had a high recurrence rate after surgery[9],[12]–[14]. The natural course of untreated IXT also showed an aggravation[15],[16]. Nusz et al[16] followed cases of IXT without surgical correction for 20y and observed the progression in more than half of the patients. The generally progressive nature has a meaningful implication with regard to the importance of surgical correction in IXT. However, the long-term recurrence has been a serious phenomenon in intermittent exotropia surgery, and the high recurrence rate might be a cause for skepticism over the effectiveness of surgical treatment for this relatively benign disease.
The recurrence rate after intermittent exotropia surgery varies from approximately 40%-80% in published articles[6],[12],[17],[18]. This study showed that the survival rate of patients with early surgical success was 97.78% on the first year, 83.70% on the third year and 50.49% on fourth year or more (such that the calculated recurrence rate was 2.22% on the first year, 16.30% on the third year and 49.51% on fourth year or more). These results demonstrate relatively lower recurrence rates with relatively long-term follow-up compared with previous reports. We thought that the lower recurrence rate was mainly due to the exclusion of patients with early surgical failure. The advantage of this study is that a line was drawn between early surgical failure and the long-term recurrence to avoid overconcern with the patients who experienced early surgical success. The reoperation rate was also as low as 3.7% (for five of the 135 patients) throughout the study period. This means that even though the survival rate steadily decreased, few patients underwent reoperation for a poorly controlled distant IXT or a large-angle IXT of ≥20 PD. Actually, in the patients who had a follow-up of more than four years, most cases of recurrent IXT showed a small angle (<20 PD). It was also found that the yearly amount of the exodrift decreased and slightly stabilized in the eye alignment with a longer follow-up time. In the period after the postoperative fourth year, the magnitude of the exotropic drift was 1.47 PD, and only one patient dropped out of the success group based on the recurrence during this period. Therefore, steady follow-up seems important until the postoperative fourth year. Interestingly, it was found that an esodrift also occurred in some patients and the amount of the esodrift increased in the long-term follow-up. One patient dropped out of success group due to delayed occurrence of consecutive esotropia (>5 PD esodeviation) on the postoperative seventh year. No other patients dropped out of the success with the occurrence of esotropia within the other follow-up time in the raw data. When the natural course of the IXT that is generally believed to progress without treatment was considered, the results showed that intermittent exotropia surgery was strong enough to achieve a long-term outcome[15],[16]. The attainment of stable central fusion from surgery can keep the eyes well-aligned after IXT surgery[19]. The surgical correction would confine it to a small-angle IXT and help maintain binocularity despite the steady exodrift in the deviating angle.
Many studies have been conducted on the factors related to recurrence. Ruttum[9] suggested that such clinical factors as the preoperative angle of deviation, the difference between far and near exodeviation, and the patient's age at the time of the surgery are associated with surgical success. Lim et al[6] said the recurrence rate decreases in older people at the onset and at the time of the surgery. However, in this study, no preoperative factors were correlated with the sustainability of the surgical success. As for the preoperative fusion, Hatt et al[20] preoperative distant stereoacuity using the Frisby Davis Distance stereo test was not correlated to angle deviation after surgery. In the patients in this study, the preoperative FCGX was likewise not associated with the survival. Gezer et al[21] reported that preoperative refractive error was a prognostic factor of surgical success. Preoperative refractive error was also expected to be associated with recurrence. In the case of myopic patients, it was hypothesized that postoperative myopic glasses with full correction or small overcorrection functions could have greater ability to maintain binocular vision than in patients with hyperopia or emmetropia. However, the results showed that myopic refractive error with spectacle wear was not associated with survival. For the surgery sequence, it was presumed that patients who had secondary surgery might have an individual propensity for recurrence. On the other hand, it was also suspected that secondary surgery could reduce the long-term recurrence rate due to the greater weakening of the anatomical factors of the exodrift because of the two operations. Hahm et al[22] reported that the recurrence rate more significantly decreased after the secondary surgery than after the primary surgery in IXT. In this study, there was no difference between the primary surgery and the secondary surgery.
Previous studies had different conclusions on whether or not the initial alignments after surgery could be determining factors of surgical success. Ruttum[9] and Leow et al[14] reported that postoperative overcorrection had no correlation with the final outcome. However, most other studies reported that postoperative overcorrection was related to a higher success rate, and this has been widely accepted[12],[13],[23]. However, in the present study, the angle of esodeviation on the first day after the surgery was not associated with the final outcomes four years after the operation, so it was thought that initial overcorrection does not inhibit long-term recurrence in our patients who achieved early surgical success. However, there was a significant difference in the amount of the exodeviation angle on the postoperative sixth month between the 2.70 PD of the success group and the 6.29 PD of the failure group. These results suggest that the angle of deviation on the postoperative sixth month may be highly correlated with the long-term outcome. Therefore, a successful long-term result might be expected in case the angle of deviation on the sixth month is close to zero in the alternate prism cover test. This is consistent with the report of Leow et al[14] that the preoperative clinical characteristics were not predictors of success, but the alignment on the the sixth month was highly correlated with consecutive good alignment.
This study had limitations. The performance of the Cox proportional hazard model was statistically biased due to the insufficient number of patients and the large differences in the sizes of the groups according to each clinical factor. In addition, because this was a retrospective study, the application of the orthoptic treatment did not follow established guidelines, and compliance with the prescribed therapy was not evaluated. Finally, we guess the patients who were followed up for a relatively long period had the presence of symptoms or some other individual reasons. For example, some glasses wearer for the prescription of glasses and some who had the presence of symptoms such as headache or asthenopia were supposed to have longer follow-up after surgery.
In conclusion, the survival rate steadily decreased with the exodrift, but there was little change in the eye alignment after the postoperative fourth year. Early overcorrection was not correlated with long-term outcomes, but a smaller deviation on the postoperative sixth month was significantly associated long-term survival with surgical success after the postoperative fourth year. In the over-fourth-year follow-up, the most recurrent IXT had a small angle of <20 PD and good distant fusion based on its demonstration of a low reoperation rate. This could indicate the long-term effectiveness of the surgery in maintaining binocularity and avoiding IXT deterioration with time. IXT is a common strabismus, and there is currently no consensus on its management. Surgery can be undertaken, but there is concern over the correction or recurrence of the deviation. Information on the long-term outcome of surgery is very helpful to clinicians. This study is helpful for clinicians because it investigated patients who experienced operative success on the postoperative sixth month by giving them a set of practical expectations on the outcomes after early intermittent exotropia surgery success.
Acknowledgments
Conflicts of Interest: Lee JY, None; Ko SJ, None; Baek SU, None
REFERENCES
- 1.Chia A, Dirani M, Chan YH, Gazzard G, Au Eong KG, Selvaraj P, Ling Y, Quah BL, Young TL, Mitchell P, Varma R, Wong TY, Saw SM. Prevalence of amblyopia and strabismus in young singaporean chinese children. Invest Ophthalmol Vis Sci. 2010;51(7):3411–3417. doi: 10.1167/iovs.09-4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman RS, Isenberg SJ. The use of part-time occlusion for early onset unilateral exotropia. J Pediatr Ophthalmol Strabismus. 1989;26(2):94–96. doi: 10.3928/0191-3913-19890301-14. [DOI] [PubMed] [Google Scholar]
- 3.Rowe FJ, Noonan CP, Freeman G, Debell J. Intervention for intermittent distance exotropia with overcorrecting minus lenses. Eye. 2009;23(2):320–325. doi: 10.1038/sj.eye.6703057. [DOI] [PubMed] [Google Scholar]
- 4.Pineles SL, Ela-Dalman N, Zvansky AG, Yu F, Rosenbaum AL. Long-term results of the surgical management of intermittent exotropia. J AAPOS. 2010;14(4):298–304. doi: 10.1016/j.jaapos.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 5.Choi J, Chang JW, Kim SJ, Yu YS. The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession-resection for intermittent exotropia. Am J Ophthalmol. 2012;153(2):343–351. doi: 10.1016/j.ajo.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 6.Lim SH, Hong JS, Kim MM. Prognostic factors for recurrence with R&R procedure in intermittent exotropia. Eye. 2011;25(4):449–454. doi: 10.1038/eye.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pukrushpan P, Isenberg SJ. Drift of ocular alignment following strabismus surgery. Part 1: using fixed scleral sutures. Br J Ophthalmol. 2009;93(4):439–442. doi: 10.1136/bjo.2007.136390. [DOI] [PubMed] [Google Scholar]
- 8.Jang JH, Park JM, Lee SJ. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefes Arch Clin Exp Ophthalmol. 2012;250(10):1485–1490. doi: 10.1007/s00417-012-1991-y. [DOI] [PubMed] [Google Scholar]
- 9.Ruttum MS. Initial versus subsequent postoperative motor alignment in intermittent exotropia. J AAPOS. 1997;1(2):88–91. doi: 10.1016/s1091-8531(97)90004-5. [DOI] [PubMed] [Google Scholar]
- 10.Rosenbaum AL, Santiago A. Intermittent Exotropia: Clinical Strabismus Management. Philadelphia: WB Saunders; 1999. pp. 163–178. [Google Scholar]
- 11.Rosenbaum AL, Stathacopoulos RA. Subjective and objective criteria for recommending surgery in intermittent exotropia. Am Orthopt J. 1992;42:46. [Google Scholar]
- 12.Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye. 2006;20(11):1268–1272. doi: 10.1038/sj.eye.6702091. [DOI] [PubMed] [Google Scholar]
- 13.Cho YA, Kim SH. Postoperative minimal overcorrection in the surgical management of intermittent exotropia. Br J Ophthalmol. 2013;97(7):866–869. doi: 10.1136/bjophthalmol-2013-303253. [DOI] [PubMed] [Google Scholar]
- 14.Leow PL, Ko ST, Wu PK, Chan CW. Exotropic drift and ocular alignment after surgical correction for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2010;47(1):12–16. doi: 10.3928/01913913-20100106-04. [DOI] [PubMed] [Google Scholar]
- 15.Jampolsky A. Characteristics of suppression in strabismus. AMA Arch Ophthalmol. 1955;54(5):683–696. doi: 10.1001/archopht.1955.00930020689010. [DOI] [PubMed] [Google Scholar]
- 16.Nusz KJ, Mohney BG, Diehl NN. The Course of Intermittent Exotropia in a Population-Based Cohort. Ophthalmology. 2006;113(7):1154–1158. doi: 10.1016/j.ophtha.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 17.Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a populationbased cohort. JAAPOS. 2009;13(1):4–7. doi: 10.1016/j.jaapos.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faridi UA, Saleh TA, Ewings P, Twomey JM. Factors affecting the surgical outcome of primary exotropia. Strabismus. 2007;15(3):127–131. doi: 10.1080/09273970701506086. [DOI] [PubMed] [Google Scholar]
- 19.Morrison D, McSwain W, Donahue S. Comparison of sensory outcomes in patients with monofixation versus bifoveal fusion after surgery for intermittent exotropia. J AAPOS. 2010;14(1):47–51. doi: 10.1016/j.jaapos.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 20.Hatt SR, Haggerty H, Buck D, Adams W, Strong NP, Clarke MP. Distance stereoacuity in intermittent exotropia. Br J Ophthalmol. 2007;91(2):219–221. doi: 10.1136/bjo.2006.099465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gezer A, Sezen F, Nasri N, Gözüm N. Factors influencing the outcome of strabismus surgery in patient with exotropia. J AAPOS. 2004;8(1):56–60. doi: 10.1016/j.jaapos.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Hahm IR, Yoon SW, Baek SH, Kong SM. The clinical course of recurrent exotropia after reoperation for exodeviation. Korean J Ophthalmo. 2005;19(2):140–144. doi: 10.3341/kjo.2005.19.2.140. [DOI] [PubMed] [Google Scholar]
- 23.Kim TW, Kim JH, Hwang JM. Long-term outcome of patients with large overcorrection following surgery for exotropia. Ophthalmologica. 2005;219(4):237–242. doi: 10.1159/000085734. [DOI] [PubMed] [Google Scholar]