Dear Sir,
I am Dr. Yin-Hung Chang from the Department of Otolaryngology, Taipei Tzu Chi Hospital, the Buddhist Tzu Chi Medical Foundation. I would like to present a case of inverted papilloma with carcinoma change of lacrimal drainage apparatus and nasal cavity that had been successfully treated by endoscopic surgery.
Lacrimal drainage apparatus tumors are rare but important because of their high rate of malignancy and life-threatening potentiality. There are about 73% primary epithelial tumors, of which 75% are malignant[1]. However, delayed or misdiagnosis of the lacrimal drainage apparatus tumors is noted as more than 50% due to the gradual onset symptoms and a low suspicion of these tumors[2]. A prompt and adequate diagnosis and management are essential to the local control of these tumors and patients' long term survival. Otorhinolaryngologists can play a role in helping ophthalmologists to make the accurate diagnosis in time and offer an adequate therapy for these lesions. Recently, ophthalmologists have tried to establish a management protocol for lacrimal drainage apparatus tumors. According to the protocol, extensive papillomas were managed with complete excision of the lacrimal drainage apparatus by lateral rhinotomy or a combined open and endoscopic approach directed against its local invasion and high recurrence rate[2]. For an inverted papilloma with carcinoma change of lacrimal drainage apparatus origin, whether or not a pure endoscopic surgical approach is feasible has been explored in this case.
A 57-year-old woman visited our ophthalmological outpatient department for the first time in August 2008 with chief complaints of epiphora from the right eye for 3mo. On ophthalmological examination, the visual acuity was 1.0 in right eye without correction and there was no relative afferent pupillary defect. The probing and nasolacrimal duct irrigation were performed by our ophthalmologist and no nasolacrimal duct obstruction or bloody reflux was noted. However, one year later, this patient returned to our hospital due to the symptoms of reddening, oedema and induration overlying the nasolacrimal sac. Besides, relapsed epiphora and purulent discharge through the right lacrimal punctum were also observed. Therefore, right side acute dacryocystitis due to nasolacrimal duct obstruction was diagnosed and empirical antibiotics treatment was given. After this patient's symptoms of acute dacryocystitis partial relieved, lacrimal probing and Silastic monocanalicular intubation (Monoka tube, FCI, Issy-Les-Moulineaux Cedex, France) were performed for the treatment of her nasolacrimal duct obstruction. Her symptoms improved due to intubation persisting with the monocanalicular tube. However, after removal of Monoka tube at our ophthalmological outpatient department in an office setting, nasolacrimal duct obstruction relapsed immediately. This unusual sign accompanied with the new symptom of nasal obstruction alerted our ophthalmologist to take sinonasal or lacrimal drainage apparatus tumors into consideration. So she was referred to our otorhinolaryngologic department for further examination and a granular tumor at right side inferior meatus was noted by the nasopharyngoscope examination (Figure 1A). Computed tomography revealed a huge heterogeneously enhancing tumor that involved the enlarged right side nasolacrimal sac and duct and protruded into the nasal cavity (Figure 2A). Punch biopsy of this tumor was done and its histopathology revealed inverted papilloma with moderate dysplasia. Dacryocystography showed contrast medium accumulation at junction between nasal cavity and orifice of nasolacrimal duct. When dealing with the inverted papilloma, we followed strictly the therapeutic principle of radical resection since the overall recurrence rate of inverted papillomas, regardless of its subtypes, is up to 40%[3], [4]. In the beginning, the main bulk of tumor was excised endoscopically to identify its origin. After the tumor was totally removed from the nasal cavity, we traced the residual papilloma to the nasolacrimal duct. Then the endoscopic medial maxillectomy and dacryocystorhinostomy were performed for the tumor removal. When the lacrimal sac was opened, we removed this tumor by microdebrider (Medtronic, Fridley, Minnesota, USA) and dissected the lacrimal sac to the orbital side. There was no tumor invasion into orbital cavity endoscopically. Final histopathology revealed inverted papilloma with carcinoma change (Figure 3). Although we advised this patient to receive post-operation radiotherapy, she declined the radiotherapy due to personal consideration. We followed up this patient at our outpatient department more than 3y by sinoscope and computed tomography exam. There was no evidence of cancer recurrence or distant metastasis till now (Figure 1B, 2B).
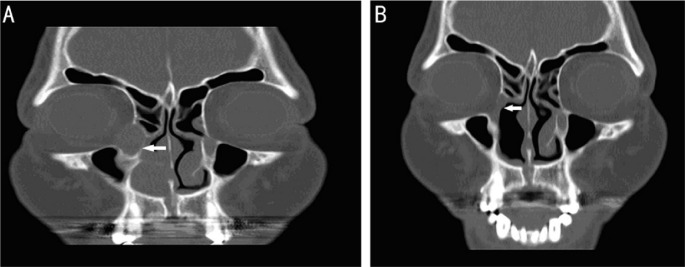
Figure 1. Pictures of pre-op and post-op of right nasal cavity and lacrimal drainage apparatus.
A: Inverted papilloma protruded into right side inferior meatus under sinoscopic examination before the operation; B: There was no recurrence sign or residual tumor at right side nasolacrimal sac and nasal cavity under sinoscopic examination after a three-year follow up.
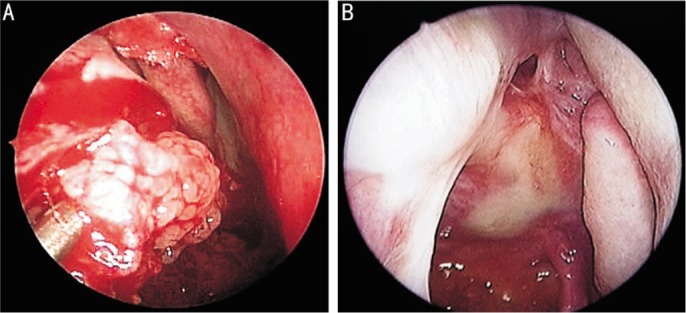
Figure 2. Pictures of pre-op and post-op of computed tomography.
A: Sinus CT coronal view (the patient): Inverted papilloma widening right side nasolacrimal sac and duct and protruding into right side nasal cavity; B: Sinus CT coronal view (the patient): There was no recurrence sign or residual tumor at right side nasolacrimal sac and nasal cavity after a three-year follow-up.
Figure 3. Pictures of final histopathological examination.
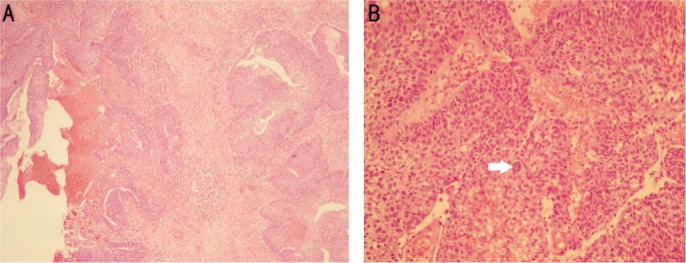
A: Histopathological examination revealed inverted nests of papillary, nonkeratinizing and transitional cell like epithelium into a polypoid edematous stroma, presenting a feature of an inverted papilloma (hematoxylin-eosin stain × 100); B: Histopathological examination demonstrated marked nuclear pleomorphism and numerous mitoses indicating carcinomatous changes arising from an inverted papilloma (hematoxylin-eosin stain × 400).
Delayed or misdiagnosis of lacrimal drainage apparatus tumors can be attributed to three causes. First, primary tumors of the lacrimal drainage system are very rare. Only approximately 300 lacrimal tumors have been reported to date[1],[5]. Second, gradual onset of lacrimal drainage system's obstructive symptoms like epiphora often lead to the dacryocystitis as the first impression. But lacrimal drainage system's tumors can also contribute to the same symptoms. So once obstructive symptoms of lacrimal drainage system caused by tumors was suspected clinically, otorhinolaryngologists and radiologist can assist to identify the tumors arising from paranasal sinus, nasal cavity or lacrimal drainage system. Nonetheless, if the tumor is confined in the lacrimal drainage system, endoscopic examination by otorhinolaryngologists barely helps to eliminate the delayed or misdiagnosis. In this case, the lacrimal drainage apparatus tumors were not suspected initially because bloody reflux was not noted when irrigation was performed. However, lacrimal drainage system irrigation with antibiotics and normal saline maybe increase the risk of cancer spread. Therefore, when managing lacrimal drainage system obstruction without identified etiology, the close cooperation among the ophthalmologists, otorhinolaryngologists and radiologists is required to achieve accurate diagnosis and appropriate therapy in time [6],[7].
Besides, middle-aged male predominance may reduce our suspicion of lacrimal drainage apparatus tumor [2],[6]. To our otorhinolaryngologists, the techniques for the adequate radical excision of the sinonasal inverted papilloma improve with the age. The medial maxillectomy through lateral rhinotomy was established in the 1970s and 1980s as the gold standard for treatment of inverted papilloma and then midfacial degloving became the most popular approach for the management of inverted papilloma[8]. Nowadays, endoscopic resection of sinonasal inverted papilloma has been accepted as a favorable treatment option around the world[9]. Although it is not always possible for the endoscopic approaches to achieve an en bloc resection, the current concept of the management of inverted papilloma is dissection the involved mucosa along the subperiosteal plane and to drill the underlying bone whenever required by imaging and/or intraoperative findings[8]. The extent of the operation is dictated by the site of the lesion and the area of mucosa involved by the lesion[8]. However, the efficacy of exclusively endoscopic management for lacrimal drainage apparatus tumor is still controversial, especially when malignant change was confirmed by histopathological examination. In this case, we chose endoscopic endonasal approach to achieve complete removal of the inverted papilloma instead of lateral rhinotomy procedure for three reasons. First, malignant change of this tumor was not proved before the surgery. If a malignant tumor was confirmed before the operation, complete removal of the lacrimal drainage apparatus with surrounding bony structures by en bloc excision may provide the best choice for survival enhancement and against early recurrence[10]. However, in recent years, endoscopic surgery for sinonasal malignant tumors is gaining popularity. Endoscopic instruments and techniques not only provide excellent visualization of the tumor, but also greatly help in their removal. The lacrimal drainage apparatus tumors often obscure their origin site and areas of invasion. The microdebrider (Medtronic, Fridley, Minnesota, USA) can be used for rapid excision of the main bulk of the inverted papilloma so that the rest of residual tumor can then be identified endoscopically. Accordingly, complete resection of all visible tumor with clear surgical margin revealed by the microscopic view of endoscopic telescopes should be a reasonable goal. Nowadays, major resistance of exclusively endoscopic surgery for malignant tumor mainly lies in the concern that oncological principles may be compromised by the piecemeal technique that has been regarded as responsible for cancer spread through the vascular or lymphatic way[11]. Yet, in recent studies, there is no evidence indicating that the piecemeal resection increases the risk of tumor recurrence[ 12]–[14]. In contrast, the exclusively endoscopic resection of sinonasal cancer resulted in oncologic outcomes comparable to those of traditional open surgery with fewer perioperative complications in well-selected patients[11], [15]–[17]. In this case, we successfully resected the tumor without recurrence or cancer spread can be attributed to the tumor aggressiveness, a well-experienced surgeon and irrigation of the surgical field. Although the tumor extended from the lacrimal sac to the nasal cavity, its origin only confined to the medial wall of the lacrimal sac without invading the bony structure and that make endoscopic approach with minimal risk of cancer spread possible. Furthermore, we have a well-experienced surgeon who can make the minimal injury of the tumor sounding tissue during the endoscopic procedure that helps decrease the possibility of cancer spread into paranasal sinus. Finally, to keep the excellent visualization of the tumor, we would irrigate the surgical field from time to time that can also reduce the chances of tumor seeding. Second, the endoscopic surgery offers the precise determination of tumor extent and the preservation of normal mucosa and bony structures. In our case, the tumor extended from the lacrimal sac and duct to the nasal cavity without invading the bony structure and mucosal lining of nasal sinus, contributing to the increased feasibility of endoscopic surgery. Finally, for the cosmetic concern, most patients, especially women, prefer to choose endoscopic surgery to avoid the external facial scars. Adjuvant radiotherapy after complete resection of the malignant tumor with close margin was recommended by previous literatures[5],[6],[10].
In conclusion, consultation for the cases of chronic dacryocystitis or prolonged epiphora to the otorhinolaryngologists in time may avoid the delayed or misdiagnosis. The surgical strategy for the lacrimal drainage apparatus tumor must be highly individualized. Tumor grade, aggressiveness, histopathological pattern and patient's health status should all be taken into account when weighing treatment options. Exclusively endoscopic surgery in this case offers a successful experience in the management of lacrimal drainage apparatus inverted papilloma with carcinoma change. But more clinical evidence is still needed to support endoscopic surgery as one option to be considered in the management of lacrimal drainage apparatus tumors.
Acknowledgments
Dr. Chung-Tai Yue, of the Department of Pathology, Taipei Tzu Chi Hospital, contributed to the accurate histopathological diagnosis and perfect photos.
Foundation: Supported by Taipei Tzu Chi Hospital, the Buddhist Tzu Chi Medical Foundation.
Conflicts of Interest: Chang YH, None; Chiu TJ, None; Hsu WC, None.
REFERENCES
- 1.Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye. 2003;17(5):599–606. doi: 10.1038/sj.eye.6700516. [DOI] [PubMed] [Google Scholar]
- 2.Valenzuela AA, McNab AA, Selva D, O'Donnell BA, Whitehead KJ, Sullivan TJ. Clinical features and management of tumors affecting the lacrimal drainage apparatus. Ophthal Plast Reconstr Surg. 2006;22(2):96–101. doi: 10.1097/01.iop.0000198457.71173.7b. [DOI] [PubMed] [Google Scholar]
- 3.Callender DL. Carcinomas of the lacrimal drainage system. Head Neck. 1993;15(4):313–319. doi: 10.1002/hed.2880150408. [DOI] [PubMed] [Google Scholar]
- 4.Ryan SJ, RL Font. Primary epithelial neoplasms of the lacrimal sac. Am J Ophthalmol. 1973;76(1):73–88. doi: 10.1016/0002-9394(73)90014-7. [DOI] [PubMed] [Google Scholar]
- 5.Stefanyszyn MA. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994;10(3):169–184. doi: 10.1097/00002341-199409000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Ni C. Tumors of the lacrimal sac: a clinicopathological analysis of 82 cases. Int Ophthalmol Clin. 1982;22(1):121–140. doi: 10.1097/00004397-198202210-00010. [DOI] [PubMed] [Google Scholar]
- 7.Flanagan J, Stokes DP. Lacrimal sac tumors. Ophthalmology. 1978;85(12):1282–1287. doi: 10.1016/s0161-6420(78)35554-8. [DOI] [PubMed] [Google Scholar]
- 8.Piero Nicolai, Paolo Castelnuovo. CHAPTER 49 – Benign Tumors of the Sinonasal Tract. 5th ed Cummings Otolaryngology: Head & Neck Surgery; [Google Scholar]
- 9.Busquets JM, PH Hwang. Endoscopic resection of sinonasal inverted papilloma: a meta-analysis. Otolaryngol Head Neck Surg. 2006;134(3):476–482. doi: 10.1016/j.otohns.2005.11.038. [DOI] [PubMed] [Google Scholar]
- 10.Valenzuela AA. En bloc excision in malignant tumors of the lacrimal drainage apparatus. Ophthal Plast Reconstr Surg. 2006;22(5):356–360. doi: 10.1097/01.iop.0000235819.06507.b1. [DOI] [PubMed] [Google Scholar]
- 11.Suh JD. Outcomes and complications of endoscopic approaches for malignancies of the paranasal sinuses and anterior skull base. Ann Otol Rhinol Laryngol. 2013;122(1):54–59. doi: 10.1177/000348941312200110. [DOI] [PubMed] [Google Scholar]
- 12.Snyderman CH, Carrau RL, Kassam AB, Zanation A, Prevedello D, Gardner P, Mintz A. Endoscopic skull base surgery: principles of endonasal oncological surgery. J Surg Oncol. 2008;97(8):658–664. doi: 10.1002/jso.21020. [DOI] [PubMed] [Google Scholar]
- 13.Wellman BJ, Traynelis VC, McCulloch TM, Funk GF, Menezes AH, Hoffman HT. Midline anterior craniofacial approach for malignancy: results of en bloc versus piecemeal resections. Skull Base Surg. 1999;9(1):41–46. doi: 10.1055/s-2008-1058171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen MA, Liang J, Cohen IJ, Grady MS, O'Malley BW, Jr, Newman JG. Endoscopic resection of advanced anterior skull base lesions: oncologically safe? ORL J Otorhinolaryngol Relat Spec. 2009;71(3):123–128. doi: 10.1159/000209312. [DOI] [PubMed] [Google Scholar]
- 15.Hanna E. Endoscopic resection of sinonasal cancers with and without craniotomy: oncologic results. Arch Otolaryngol Head Neck Surg. 2009;135(12):1219–1224. doi: 10.1001/archoto.2009.173. [DOI] [PubMed] [Google Scholar]
- 16.Higgins TS, Thorp B, Rawlings BA, Han JK. Outcome results of endoscopic vs craniofacial resection of sinonasal malignancies: a systematic review and pooled-data analysis. Int Forum Allergy Rhinol. 2011;1(4):255–261. doi: 10.1002/alr.20051. [DOI] [PubMed] [Google Scholar]
- 17.Nicolai P, Battaglia P, Bignami M, Bolzoni Villaret A, Delù G, Khrais T, Lombardi D, Castelnuovo P. Endoscopic surgery for malignant tumors of the sinonasal tract and adjacent skull base: a 10-year experience. Am J Rhinol. 2008;22(3):308–316. doi: 10.2500/ajr.2008.22.3170. [DOI] [PubMed] [Google Scholar]