Abstract
Objectives:
The purpose of this case series was to compare the clinical, radiographic, and histopathologic features of 11 cases of ameloblastoma that reported to the Goa Dental College and Hospital over a period of 4 years from January 2008 to December 2012.
Study Design:
Data with respect to the patients’ ages, sex, location of lesions, radiographic features, histopathologic features and surgical treatment and follow-up, was analyzed.
Results:
The mean age in males was 23.25 ± 6.99 years, while that in females was 43.43 ± 17.13 years. Seven (63.63%) of the 11 subjects were females, and four (36.36%) were males. 10 (90.9%) of the 11 ameloblastomas were located in the mandible. Swelling was noted in all 11 patients. 10 cases showed radiographic findings, while one case was a peripheral soft-tissue variant. Seven (70%) of the 10 tumors were multilocular with a well-demarcated corticated border, and three cases (30%) were unilocular. Two cases showed a soap-bubble appearance. Histologically, five cases were unicystic, four were multicystic, one was desmoplastic and one was a peripheral variant. Follow-up ranged from 12 to 34 months and there were no signs of recurrence in any of the patients.
Conclusions:
Ameloblastomas more commonly occur in females at an older age, as compared with males. Radiographic features that could help in diagnosing ameloblastomas include its predominant occurrence in the mandible, multilocular radiolucency with well-defined, corticated, scalloped margins, expansion of buccal and lingual cortical plates, root resorption and tooth displacement.
Keywords: Ameloblastoma, desmoplastic, multilocular, peripheral, unilocular
Introduction
Ameloblastoma is a neoplasm of odontogenic epithelium, and represents 11-13% of all odontogenic tumors.[1] It is a persistent and locally invasive tumor that has aggressive but benign growth characteristics.[2] There are three different clinicoradiographic types: The conventional solid/multicystic intra-osseous ameloblastoma, the unicystic ameloblastoma and the peripheral ameloblastoma. In addition, the desmoplastic ameloblastoma is regarded as a fourth subtype of ameloblastoma because of its biological behavior, radiographic appearance and unique histology. Ameloblastomas are tumors of odontogenic epithelial origin. They may arise from any of the following: Rest cells of the dental lamina, developing enamel organ, epithelial lining of odontogenic cysts, basal cells of oral mucosa, heterotopic epithelium in other parts of the body (e.g., pituitary gland).[3]
Conventional ameloblastomas are usually seen between 20 and 50 years of age, with an average age of discovery of about 40 years,[1,2] while the unicystic variant may occur in younger patients (20-30 years of age). Some authors state a male predilection,[1,2] while others describe it as being more common in females.[4] Lesions grow slowly, with few, if any, symptoms in early stages. Patients most commonly present with a painless swelling or expansion of the jaw causing facial asymmetry. Ameloblastomas are about 5 times more common in the mandible than in the maxilla.[5] Radiographically, the tumor may be unilocular or multilocular, with a tendency for expansion.[6] Unicystic lesions however, present more commonly as unilocular radiolucencies. The internal structure varies from totally radiolucent to a mixed radiolucent-radiopaque caused by presence of bony septae creating internal compartments, which may give rise to soap bubble, honeycomb, spider-like[4] or mother-and-daughter cell[4] appearances. The appearance of septae on the radiograph usually represents differential resorption of the cortical plate by the tumor and not actual separation of tumor portions.[7] Ameloblastomas have a tendency to cause extensive root resorption and teeth may be displaced apically.
There are several histopathological subtypes-follicular, acanthomatous, plexiform, desmoplastic, granular cell, and basal cell pattern, which may exist singly or as a combination of two or more types.[8] A difference in aggressiveness or tendency to recur does not appear to vary according to histopathologic type. Treatment options range from conservative surgical therapy (enucleation, curettage, excision, and marsupialization) to radical surgery (marginal resection, segmental resection and total resection of the jaw (maxilla/mandible) with wide margins).[5] Peripheral lesions are usually excised with a small margin of normal tissue, and the surgical site re-examined periodically.[9,10]
The aim of this work was to review a series of eleven cases of ameloblastomas that presented to our department in the last 4 years and attempt to correlate the clinico-radiographic-histopathologic features of these lesions, to help in diagnosing ameloblastomas based on their clinical and radiographic characteristics.
Patients and Methods
This study was carried out on 11 cases of ameloblastoma that were diagnosed and treated at our institution in the last 4 years. The cases were examined clinically and radiographically and were confirmed by preoperative incisional biopsies. All cases were documented radiographically with orthopantomograms, while intra-oral periapical and occlusal radiographs were also taken, depending on the location of the lesions. The patients were treated conservatively (i.e., with enucleation and curettage, or both) or radically (i.e., with partial or complete jaw resection) depending on the location and size of the tumor. All postoperative surgical specimens were submitted for histopathologic examination.
Results
Age and gender
Of the 11 cases of ameloblastoma in our series, seven cases were diagnosed in females and four in males, with a male-to-female ratio of 1:1.75. The youngest patient was a 15-year-old, while the eldest was 69 years of age. The mean age in males was 23.25 years, while that in females was 43.43 years [Table 1] with a standard deviation of 6.99 in males and 17.13 in females. A statistically significant difference (with P = 0.024) in the mean age of occurrence in males as compared to that in females was observed.
Table 1.
Gender, age, clinical symptoms and histopathologic appearance of eleven cases histopathologically diagnosed as ameloblastoma in the present case series
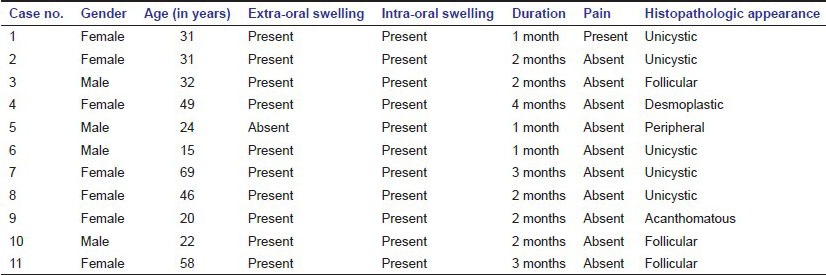
Location
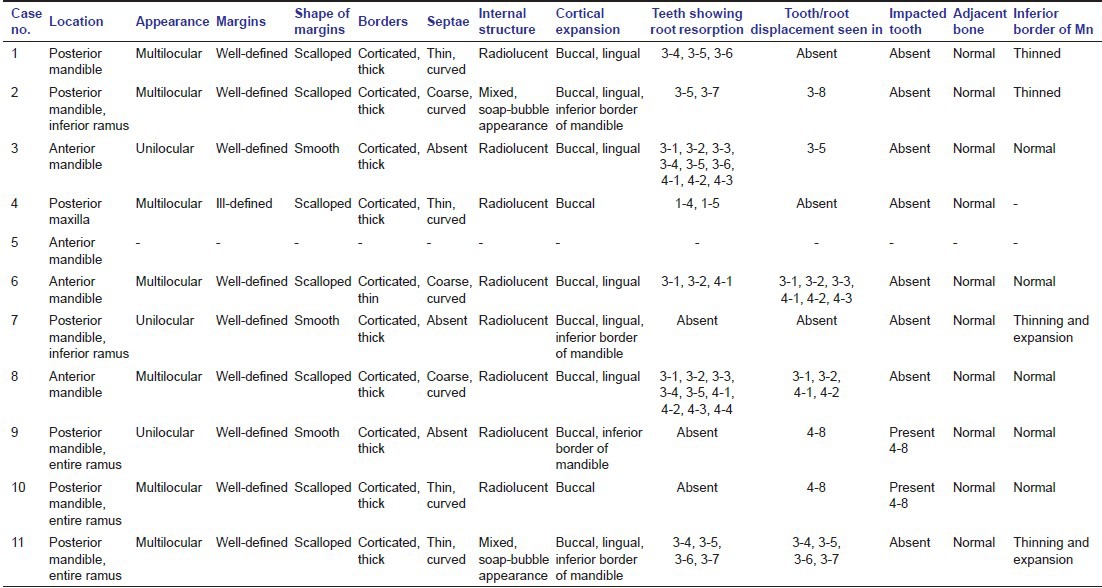
Ten out of eleven cases were seen in the mandible, with six of these occurring in the posterior mandible. One case involved only the molar region while five cases involved both the molar and ramus regions. Involvement of the entire ramus of mandible was observed in three cases [Table 2].
Table 2.
Radiographic features of ameloblastoma of eleven cases histopathologically diagnosed as ameloblastoma in the present case series
Clinical presentation
In 10 patients, the initial chief complaint was a swelling of the lower jaw and/or face, for a period ranging from 1 to 4 months. Pain was a feature only in one case. An extra-oral swelling was noted in 10 patients while all 11 cases presented with an intra-oral swelling. None of the patients complained of any tooth mobility or paresthesia [Table 1].
Radiographic features
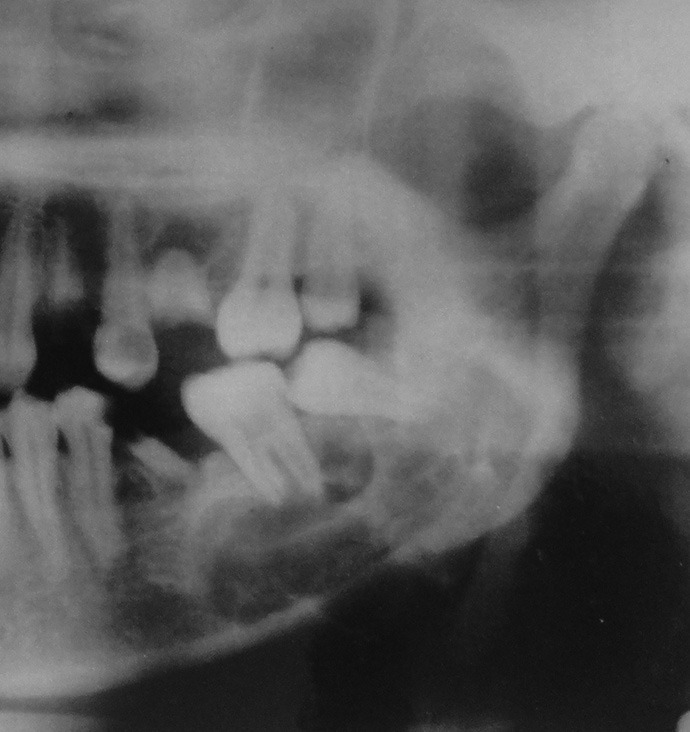
Out of the 11 cases, 10 cases showed radiographic findings. The peripheral variant (Case no. 5) did not show any radiographic evidence of bone involvement. Seven of the cases appeared as multilocular radiolucencies [Figures 1–4] with well-defined, scalloped margins. Three tumors were found to be large unilocular radiolucencies [Figures 5 and 6] with well-defined borders. Nine out of 10 cases showed a predominantly radiolucent internal structure (five of these showed presence of septae), while two cases had a “soap-bubble” appearance. 10 out of 10 cases showed expansion of buccal cortical plate, seven out of 10 cases showed lingual cortical expansion. Four cases showed thinning of inferior border of mandible, while expansion of the lower border of mandible was noted in two cases. However, no perforation of cortical margins of the inferior and/or posterior border (s) of the mandibular body/ramus was noted. The bone adjacent to the lesions showed a normal appearance in all the cases. Root resorption of involved teeth was seen in seven cases, and displacement of teeth in seven cases. Two cases were associated with impacted mandibular third molars [Table 2].
Figure 1.

Multilocular lesion in left posterior mandible with well-demarcated corticated borders (Case no. 1)
Figure 4.

Multilocular radiolucency with well-demarcated corticated borders in posterior mandible (Case no. 8)
Figure 5.

Unilocular radiolucency with well-demarcated corticated borders in posterior mandible, causing expansion and thinning of inferior border of mandible (Case no. 7)
Figure 6.

Unilocular lesion in right mandibular ramus with well-defined corticated borders (Case no. 9)
Figure 2.
Multilocular lesion in left posterior mandible showing soap bubble appearance (Case no. 2)
Figure 3.

Multilocular radiolucency with well-demarcated corticated borders in anterior mandible (Case no. 6)
Histopathological features
Four cases were diagnosed as solid/multicystic ameloblastomas (three follicular, one acanthomatous). Five cases showed histological features of unicystic ameloblastomas, while one case was a desmoplastic variant with one lesion being a peripheral ameloblastoma [Table 1].
Treatment and follow-up
Large lesions, including those that involved the ramus of mandible, were treated by radical surgery which included marginal resection, segmental or total resection of the mandible with wide margins. Four cases were treated with conservative surgical therapy including enucleation. Follow-up ranged from 12 to 34 months until date. Healing was satisfactory in all the patients and there are currently no signs of recurrence in any of the patients.
Discussion
Conventional ameloblastomas are usually seen between 20 and 50 years of age, while the unicystic variant may occur in younger patients (20-30 years of age).[2] In the present case series, six of the 11 cases were seen in the 2-3rd decade of life, which is in agreement with previous studies by White and Pharoah,[2] Reichart et al.,[5] and Cosola et al.[11] We found a male-to-female ratio of 1:1.75, which is similar to that reported by Al-Khateeb and Ababneh.[8] In this case series, we documented the occurrence of ameloblastomas at a significantly younger age in males (mean age of 23.3 years), when compared to that in females (mean age of 41 years), which differs from previously reported cases in the literature.
Most ameloblastomas develop in the mandible (up to 75%), usually in the molar-ascending ramus region, and 15% in maxilla (usually in third molar area).[2,5] 10 out of our 11 cases occurred in the mandible (90.9%), with seven cases occurring in the posterior mandible (ramus and molar region), which corroborates with the findings obtained by Cosola et al.[11] and Kim and Jang.[12] The only maxillary ameloblastoma that we found turned out to be a desmoplastic variant. 10 of our cases presented with a chief complaint of a painless extra-oral swelling, which is similar to what has been reported by White and Pharoah[2] and Al-Khateeb and Ababneh,[8] with pain being a feature in only one case. According to Worth,[4] the most common radiographic appearance of ameloblastoma is a multilocular radiolucency with a corticated border, and margins, which usually show irregular scalloping. In the present series, a multilocular appearance was seen in 70% cases, while 30% cases showed a unilocular appearance. This is in contrast to Reichart, et al.,[5] who found a multilocular appearance in 51% cases and a unilocular appearance in 49% cases. This difference can be attributed to the relatively small number of cases in our study. However, four of the five cases of unicystic ameloblastoma (80%) in the present series showed a multilocular radiographic appearance, which differs with previous literature. The single desmoplastic case appeared as a multilocular radiolucency, similar to the conventional ameloblastoma. A typical soap-bubble appearance was noted in only two cases in our series. Two out of the five unicystic cases (40%) appeared as pericoronal radiolucencies similar to dentigerous cysts, with both being associated with an impacted mandibular third molar, which was displaced apically. All the cases (100%) in the present series showed expansion of the buccal cortical plate, while lingual cortical expansion was seen in 70% cases, with thinning of the inferior border of mandible in 40% of the cases.
Ameloblastomas are thought to have a pronounced tendency to cause extensive root resorption and tooth migration, tipping, and displacement is common.[10] Root resorption was seen in 70% cases, with displacement of teeth also noted in 70% of our cases. According to White and Pharoah[2] and Kim and Jang,[12] around 10-15% may be associated with a non-erupted tooth, often a mandibular third molar. Two of our cases (22.22%) were associated with impacted mandibular third molars. Unicystic types of ameloblastoma may cause extreme expansion of the mandibular ramus and often the anterior border of the ramus is no longer visible on the panoramic image.[2] This feature was noted in two of the unicystic cases in this series.
Histopathologically, we found that the unicystic pattern was the most common (45.45%), followed by the follicular pattern (27.27% cases). Six ameloblastomas showed a variable extent of micro-cyst formation, while four tumors were entirely cystic (unicystic). These unicystic tumors contained mural and/or intraluminal thickenings that consisted of tumor cells. None of the cases showed infiltration beyond the cystic confines.
Conclusion
In contrast to other reports, we found that ameloblastomas were more common in females at an older age and occurred at a much younger age in males. The diagnosis of ameloblastoma can be based on the following radiographic features (starting with the most common): (1) Occurrence in the mandible, (2) multilocular radiolucency with well-defined, corticated, scalloped margins, (3) expansion of buccal cortical plate, (4) expansion of lingual cortical plate, (5) presence of curved septae within the lesion, (6) root resorption, (7) displacement of teeth, (8) involvement of ramus of mandible, (9) thinning of inferior border of mandible, and (10) non-erupted mandibular third molar.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wood NK, Goaz PW, editors. 5th ed. Missouri: Mosby-Elsevier; 2011. Differential Diagnosis of Oral and Maxillofacial Lesions; pp. 337–40. [Google Scholar]
- 2.White SC, Pharoah MJ, editors. 5th ed. New Delhi: Mosby-Elsevier; 2005. Oral Radiology: Principles and Interpretation; pp. 419–22. [Google Scholar]
- 3.Giraddi GB, Bimleshwar K, Singh C, Garg V, Anusha JS. Ameloblastoma: Series of 7 treated cases and review of literature. Arch Oral Sci Res. 2011;1:152–5. [Google Scholar]
- 4.Worth HM, editor. Chicago: Year Book Medical Publishers Inc; 1975. Principles and Practice of Oral Radiologic Interpretation; pp. 476–94. [Google Scholar]
- 5.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 6.Leider AS, Eversole LR, Barkin ME. Cystic ameloblastoma. A clinicopathologic analysis. Oral Surg Oral Med Oral Pathol. 1985;60:624–30. doi: 10.1016/0030-4220(85)90366-4. [DOI] [PubMed] [Google Scholar]
- 7.Gümgüm S, Hoºgören B. Clinical and radiologic behaviour of ameloblastoma in 4 cases. J Can Dent Assoc. 2005;71:481–4. [PubMed] [Google Scholar]
- 8.Al-Khateeb T, Ababneh KT. Ameloblastoma in young Jordanians: A review of the clinicopathologic features and treatment of 10 cases. J Oral Maxillofac Surg. 2003;61:13–8. doi: 10.1053/joms.2003.50002. [DOI] [PubMed] [Google Scholar]
- 9.Gardner DG. Peripheral ameloblastoma: A study of 21 cases, including 5 reported as basal cell carcinoma of the gingiva. Cancer. 1977;39:1625–33. doi: 10.1002/1097-0142(197704)39:4<1625::aid-cncr2820390437>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 10.Philipsen HP, Reichart PA, Nikai H, Takata T, Kudo Y. Peripheral ameloblastoma: Biological profile based on 160 cases from the literature. Oral Oncol. 2001;37:17–27. doi: 10.1016/s1368-8375(00)00064-6. [DOI] [PubMed] [Google Scholar]
- 11.Di Cosola M, Turco M, Bizzoca G, Tavoulari K, Capodiferro S, Escudero-Castano N, et al. Ameloblastoma of the jaw and maxillary bone: Clinical study and report of our experience. Av Odontoestomatol. 2007;23:367–73. [Google Scholar]
- 12.Kim SG, Jang HS. Ameloblastoma: A clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:649–53. doi: 10.1067/moe.2001.114160. [DOI] [PubMed] [Google Scholar]


