Abstract
Objective:
The objective of this study is to investigate the influence of flap design on visibility and accessibility during removal of impacted third molar and hematoma formation, wound gaping and healing of flap post-operatively.
Study Design:
The randomized prospective comparative study included 30 patients with impacted mandibular third molars. Two flap designs namely envelope flap (Koener's incision) and ‘triangular flap’ (Ward's incision) were used. After 7 days, sutures were removed and status of wound, periodontal health, and progress of healing was assessed. Patients were followed through 15 days to judge the incidence of post-operative complications in both groups.
Results:
No statistical differences were noted between the groups in terms of visibility, accessibility, excessive bleeding during surgery, healing of flap, sensitivity of adjacent teeth, and dry socket. A statistically significant difference was observed in post-operative hematoma, wound gaping, and distal pocket in adjacent tooth, which was significant in Ward's triangular incision group in comparison to Koeiner's envelope incision group.
Conclusion:
The selection of the flap design is dependent on needs of the case and preference of the operating surgeon and does not seem to have a significant influence on the health of tissues. In order to avoid wide area of exposure of bone, the operating surgeon should clinically and radiographically assess the designing of incision and mucoperiosteal flap, the clinical relevance is still debatable.
Keywords: Envelope flap, impacted mandibular third molar, Koener's incision, triangular flap, Ward's incision
Introduction
Surgical removal of an impacted mandibular third molar is one of the most frequently performed minor oral surgical procedures and demands sound understanding of surgical principles to perform it as atraumatically as possible. Incisions are placed to gain access to the surgical site for adequate accessibility to perform a clean surgical procedure and for proper visibility of the surgical field. The effect of impacted third molar extraction and different flap techniques on periodontal health distal to the adjacent second molar has been investigated with conflicting results in several studies.[1,2,3] Different designs for the raising of a mucoperiosteal flap to expose an impacted lower third molar have been advocated by various authors, the most common designs being the modified triangle flap and the envelope flap.[4] The presence of various important anatomical structures in the adjacent area around the surgical site has made many surgeons to design an incision, ranging from envelope (Koener's) incision, triangular (Ward's) incision, and its’ modification, L shaped incision, bayonet shaped incision, comma incision, and “S” shaped incision,[5] which would allow proper access and visibility with consideration and protection of the vital anatomical structures. A comparative study was carried out between two basic incision designs namely envelope (Koener's) and triangular (Ward's) incision used in surgical removal of impacted third molar in terms of visibility, accessibility, hematoma formation, wound gaping, and healing of flap.
Materials and Methods
A randomized comparative prospective study was done which included a total of 30 patients aged between 20 and 30 years (mean age of 25 years), and were included in this comparative study, irrespective of gender, who reported to and were treated at the Department of Oral and Maxillofacial Surgery, K. M. Shah Dental College and Hospital, Vadodara, with the clinical and radiographic diagnosis of impacted mandibular third molar.
Inclusion criteria consisted of patients with no medical history of any illness or prolonged medication that could influence the course of post-operative wound healing. Patients with healthy dental and periodontal status with no evidence of local inflammation or pathology at the time of removal of impacted tooth. Pre-operatively, intraoral periapical, occlusal, and panoramic radiographs were obtained. An informed consent was duly signed by the participants. Ethical approval was also obtained from the local ethical committee.
A standard surgical protocol was followed. While one investigator who is experienced in the use of both the flap designs performed the surgery the other investigator carried out the evaluation.
Prophylactic antibiotics amoxicillin 500 mg t.d.s. was started orally 24 h before surgery. Intraoral flushing was done with 5% betadine followed by flushing with normal saline. For local anesthesia, 2% lignocaine hydrochloride with 1:80,000 adrenaline was used.
In one group, Koener's incision was used in 15 patients. Incision was given with the distal extension commencing near the external oblique ridge on the lateral aspect of the mandible. The incision is brought forward and medially towards the middle of the distal surface of mandibular second molar, which was 0.75 inch long with distal incision. The incision was drawn anteriorly along the free margin of the second molar, which terminated at the mesiobuccal line angle of that tooth.
In other group, Ward's incision was used in 15 patients. The incision starts about 6 mm inferiorly in the buccal sulcus at a point corresponding to the junction of anterior 2/3rd and distal 1/3rd of mandibular second molar. The cut is then taken vertically upwards to the neck of the second molar, passes around the gingival margin of posterior 1/3rd of the tooth and continues cervically on the distal aspect to approximately the midpoint of the tooth. From this point, the incision runs posteriorly and buccally along the line of external oblique ridge.
After exposing the surgical site, osteotomy was carried out using a bur technique and the tooth was sectioned as necessary. The flap was approximated with interrupted 3-0 silk suture. In case of wards incision, one suture was taken on the releasing incision.
After 7 days, sutures were removed and status of wound, periodontal health, and healing was assessed. Patients were followed up through 15 days to judge the incidence of post-operative complications in both groups.
Results
This prospective randomized comparative study was conducted at the Department of Oral and Maxillofacial Surgery and consisted of 30 healthy patients with impacted mandibular third molars. The age range was 20-30 years with the mean age being 25 years. There were no significant differences regarding the demographic data between the subjects who were enrolled. The side of surgery and order of surgery exerted no significant effect on the results (P > 0.05). There existed no significant difference (P > 0.05) between the two groups of Ward's triangular incision and Koener's envelope incision in respect to visibility, accessibility, excessive bleeding, healing of flap, sensitivity, and dry socket.
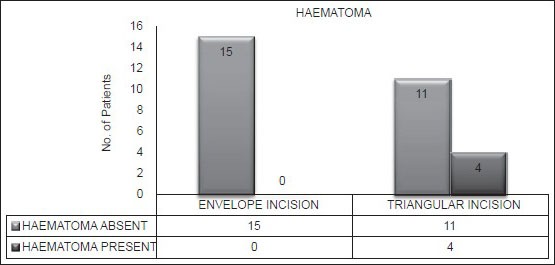
There exists a significant difference (P < 0.05) between the two groups of Ward's triangular incision and Koener's envelope incision in respect to hematoma [Tables 1a and b, Graph 1], wound gaping [Tables 2a and b, Graph 2], distal pocket [Tables 3a and b, Graph 3], which was significant in Ward's triangular incision group in comparison to Koener's envelope incision group.
Table 1a.
Haematoma : Number of incidents
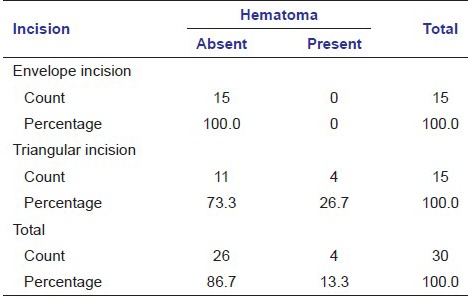
Table 1b.
Hematoma : Statistical evaluation
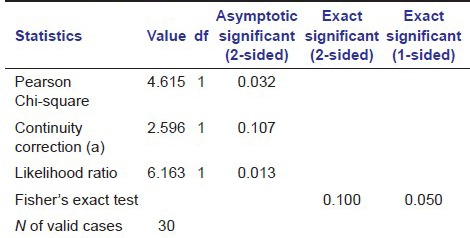
Graph 1.
Hematoma
Table 2a.
Wound gaping : Number of incidents
Table 2b.
Wound gaping : Statistical evaluation
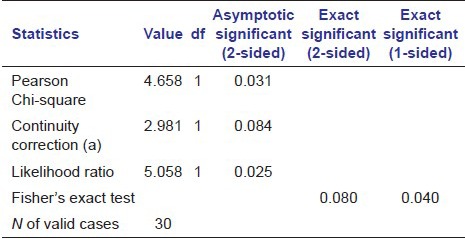
Graph 2.
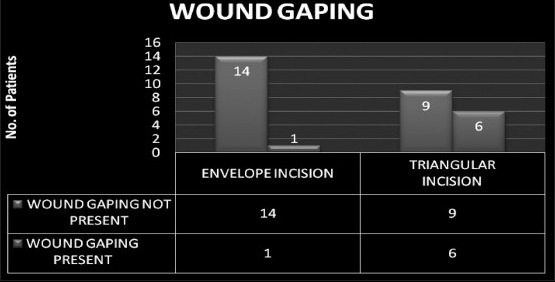
Wound gaping
Table 3a.
Distal pocket : Number of incidents
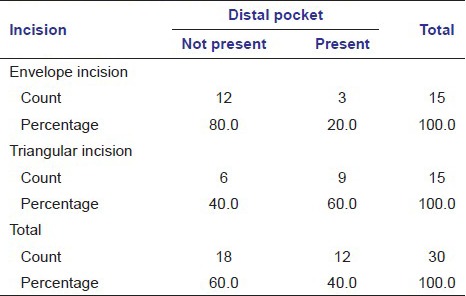
Table 3b.
Distal pocket : Statistical evaluation
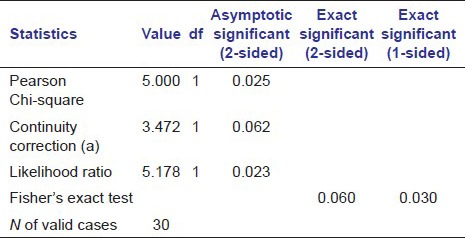
Graph 3.
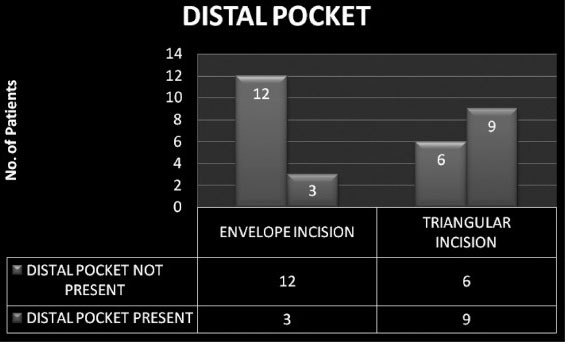
Distal pocket
Discussion
The envelope flap allows good exposure of the surgical site and the sulcular incision can be extended anteriorly if required. Owing to the broad base, blood supply is excellent, and the design facilitates easy closure and reapproximation. Potential problems of the envelope flap have been discussed in the literature and includes (1) damage to the periodontal ligament when creating a sulcular incision around a tooth, (2) increased osteoclastic activity when raising a mucoperiosteal flap with potential local bone loss, and (3) a higher risk of wound dehiscence in the post-operative period compared with the triangular flap.[1,6]
The triangular flap is regarded as more conservative owing to a lesser degree of tissue reflection, because it avoids the raising of soft-tissue from the buccal aspect of the second molar. It is simple to close and allows a relatively tension-free closure. However, unlike the envelope flap, it cannot be readily extended. The literature reports no difference in the periodontal status of the adjacent second molar at 6 months that can be attributed to using an envelope flap compared with using a triangular flap.[7] Stephens et al.[7] compared the periodontal status of mandibular second molars after third molar surgery using either the envelope flap design or the triangular flap design and concluded that, within the limits of the study, flap design did not influence the health of the second molar periodontium, and therefore flap design becomes a matter of individual preference.
At the post-operative examination after 7 days, the probing depth was statistically greater in the first and second molars on the side on which an envelope flap was used. These findings could be related to the deficient initial regeneration of the connective-tissue attachment, which was formed perfectly 3 months post-operatively, as demonstrated on post-extraction probing. The post-operative examinations 3 and 6 months after extraction showed perfect healing with both flaps. We believe that this follow-up period was adequate, and was similar to the follow-up periods in most studies of this type. A longer duration runs the risk of losing some patients to follow-up.[8,9,10] With regard to operating times, a triangular flap facilitated extractions compared with an envelope flap, although the difference was not statistically significant. However, this might be an important factor with less cooperative patients or with those who cannot open their mouths fully for anatomical reasons. Difficulty in opening the mouth (distance between the mandibular and maxillary incisors of - 30 mm) can hinder the use of bur method for osteotomy and sectioning of tooth, complicating the surgical procedure. In such cases, the use of a triangular flap might be advisable.
Conclusion
In this study, the two groups were assessed for visibility, accessibility, healing and pre-and post-operative complications. In our present study Koener's envelope flap was found to be better in terms of post-operative healing as compared to Ward's incision. It has advantage of (1) good adaptation of gingival margins, (2) no pocket formation distal to mandibular second molar, (3) avoidance of difficult suturing in vestibule, (4) no chances of injury to facial artery and vein, (5) no food lodgment and thus chances of infection are reduced. Ward's incision enjoys advantages like better accessibly and visibility especially in deep seated impactions. It is easy to retract flap margins away from surgical area.
The selection of the flap design is dependent on needs of case and preference of surgeon and does not seem to have a lasting effect on the health of tissues. In order to avoid wide area of exposure of bone, the surgeon should clinically and radiographically assess the designing of incision and mucoperiosteal flap.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jakse N, Bankaoglu V, Wimmer G, Eskici A, Pertl C. Primary wound healing after lower third molar surgery: Evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:7–12. doi: 10.1067/moe.2002.119519. [DOI] [PubMed] [Google Scholar]
- 2.Ash MM, Costich ER, Hayward JR. A study of periodontal hazards of third molars. J Periodontol. 1962;33:209. [Google Scholar]
- 3.Schofield ID, Kogon SL, Donner A. Long-term comparison of two surgical flap designs for third molar surgery on the health of the periodontal tissue of the second molar tooth. J Can Dent Assoc. 1988;54:689–91. [PubMed] [Google Scholar]
- 4.Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–6. doi: 10.1016/j.tripleo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 5.Baqain ZH, Al-Shafii A, Hamdan AA, Sawair FA. Flap design and mandibular third molar surgery: A split mouth randomized clinical study. Int J Oral Maxillofac Surg. 2012;41:1020–4. doi: 10.1016/j.ijom.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Wood DL, Hoag PM, Donnenfeld W, Rosenfeld LD. Alveolar crest reduction following full and partial thickness flaps. J Periodontol. 1994;65:79–83. doi: 10.1902/jop.1972.43.3.141. [DOI] [PubMed] [Google Scholar]
- 7.Stephens RJ, App GR, Foreman DW. Periodontal evaluation of two mucoperiosteal flaps used in removing impacted mandibular third molars. J Oral Maxillofac Surg. 1983;41:719–24. doi: 10.1016/0278-2391(83)90188-x. [DOI] [PubMed] [Google Scholar]
- 8.Quee TA, Gosselin D, Millar EP, Stamm JW. Surgical removal of the fully impacted mandibular third molar. The influence of flap design and alveolar bone height on the periodontal status of the second molar. J Periodontol. 1985;56:625–30. doi: 10.1902/jop.1985.56.10.625. [DOI] [PubMed] [Google Scholar]
- 9.Rosa AL, Carneiro MG, Lavrador MA, Novaes AB., Jr Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:404–7. doi: 10.1067/moe.2002.122823. [DOI] [PubMed] [Google Scholar]
- 10.Dodson TB. Management of mandibular third molar extraction sites to prevent periodontal defects. J Oral Maxillofac Surg. 2004;62:1213–24. doi: 10.1016/j.joms.2004.06.035. [DOI] [PubMed] [Google Scholar]


