Abstract
Objective:
To evaluate the upper airway dimensions in adolescents treated for bimaxillary proclination with first premolar extraction.
Materials and Methods:
A retrospective cephalometric evaluation was carried out on the available pre and post orthodontic treatment records of 150 patients (12-18 years of age) who had bimaxillary proclination and were treated with fixed orthodontic therapy. Cephalometric landmarks for sagittal airway measurements and hyoid bone were identified; linear and angular measurements were obtained. Descriptive statistics using paired t-test was used to assess changes in pre and post treatment values and Pearson's correlation coefficient was calculated to evaluate the reliability of observations. The method error calculations were performed using the Dahlberg formula.
Results:
It was observed that the mean values of nasopharyngeal dimension and Total Airway Length (TAL) showed no statistically significant difference in pre and post treatment groups. All other airway and hyoid parameters showed statistically significant difference. Pearson's correlation coefficient showed statistically significant correlations in all the airway and hyoid parameters.
Conclusions:
In the present study, the nasopharyngeal dimension and TAL were not found to be directly affected by the retraction of anterior teeth, This can be attributed to the fact that nasopharyngeal dimension and TAL are not under direct influence of tongue position. The other findings also indicated direct correlation of tongue position to oropharynx and hypopharynx. Consequently, we emphasize clinically relevant anatomic risk factors that should be given prime importance and serious consideration on the decision whether to extract or not in growing patients.
Keywords: Airway, cephalometrics, premolar extraction
Introduction
It is predictable that bone cannot be stimulated to grow beyond its inherent potential, and consequently, extractions are sometimes necessary to treat certain malocclusions. The extraction controversy still continues from the early 20th century. Malocclusions can be treated by several means, according to the characteristics associated with the problem, such as antero-posterior discrepancy, age, and patient compliance. Methods include extra-oral appliances, functional appliances and fixed appliances associated with inter-maxillary elastics. The treatment plan might also involve extractions. In addition to correcting the dental relationship, an objective of these treatment approaches is to provide good facial balance.
Dental arch expansion is associated with airway dimensional changes.[1] The effect of extraction treatment will be reflected on the arch dimensions, and since most of the extraction spaces in patients with bimaxillary proclination would be used for incisor retroclination and correction of lip procumbency, it is imperative to assume that altering incisor and soft-tissue position and arch dimension could affect tongue position, and therefore, the upper airway dimensions.[2] This especially holds good in young adolescent growing patients who may be put to risk for airway incumbency.
It is well-accepted that, during orthodontic treatment involving the extraction of teeth, arch dimensional changes occur and that these dimensions continue to change following active treatment.[3] Quantification of these changes in the maxillary arch, however, has only recently been provided.[4] Furthermore, the ability for maxillary extraction spaces to be used in a predictable fashion has not yet been widely presented in the literature. It is reported that in cases involving the extraction of four first premolars, approximately 66.5% of the available extraction space was taken up by the retraction of the anterior segment. In cases involving extractions of maxillary first and mandibular second premolars, 56.3% of the available extraction space was taken up by the retraction of the anterior segment.[5]
The effect of premolar extraction on dental arch dimensions has been studied before,[6] however, changes in the upper airway dimensions that may occur because of the extraction of first premolar teeth in a sample of young adolescent patients still needs further research. The purpose of this study was to evaluate the upper airway dimensions in adolescents treated for bimaxillary proclination with first premolar extraction.
Materials and Methods
The study protocol was in accordance with the Helsinki Declaration of Human Rights and was approved by the Ethical Committee. A retrospective cephalometric evaluation was carried out on the available pre and post orthodontic treatment records of 164 patients (12-18 years of age) who had bimaxillary proclination and were treated at the Department of Orthodontics, SPDC, Wardha between 2008 and 2012 with fixed orthodontic treatment by extraction of upper and lower first premolar teeth.
Subjects were selected according to the following criteria:
Pretreatment bimaxillary proclination (upper incisor to maxillary plane angle, UI/Max > 115°), lower incisor to mandibular plane angle (LI/Mand > 99°), and inter-incisal angle less than 125°
No medical history, that is, the selected patients did not suffer from any medical disease. Patients with medical history of pharyngeal pathology and/or nasal obstruction, snoring, obstructive sleep apnea, adenoidectomy, and tonsillectomy were excluded
Pre and post orthodontic treatment lateral cephalograms of adequate diagnostic quality
Treatment consisted of fixed orthodontic appliances only.
Out of the cephalometric records, 14 cephalograms were excluded from the evaluation due to poor diagnostic value and poor image quality.
Cephalometric tracing and analysis
Pre and post treatment lateral cephalograms were manually traced using acetate tracing paper carefully attached to the radiographs. During tracing, the room was darkened and the viewing screen was blanked off, showing only the radiograph. Magnification of radiographs was corrected and calibrated according to the magnification factor and using the radiopaque ruler (calibration marker). The same investigator performed all lateral cephalometric measurements. Landmarks for sagittal airway measurements and hyoid bone position were identified for each cephalogram, yielding 11 linear measurements [Figure 1]. Definition of the different landmarks and measurements used are shown in Tables 1 and 2. All cephalometric measurements were performed manually using a ruler to the nearest 0.1 mm to measure the linear distance between the two points, making the measurement and protractor to the nearest 0.5° to measure the angular measurements.
Figure 1.
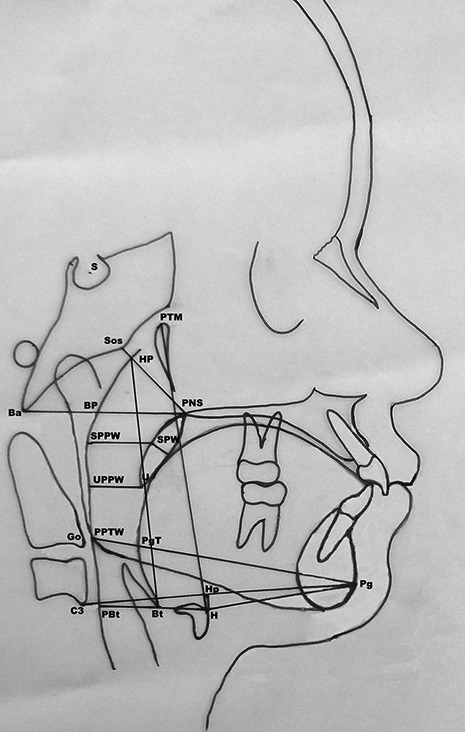
Landmarks for sagittal airway measurements and hyoid bone position on cephalogram
Table 1.
Definition of various landmarks identified for sagittal airway measurements and hyoid bone position on cephalogram
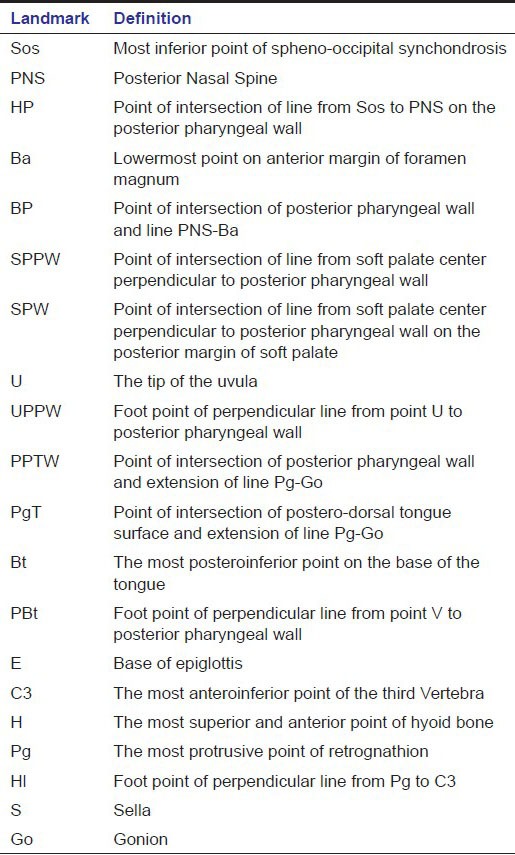
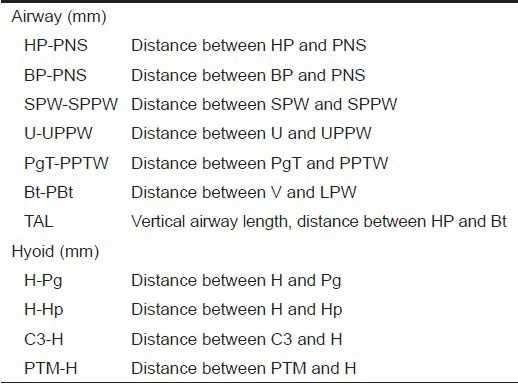
Table 2.
Definition of the different airway and hyoid measurements for sagittal airway and hyoid bone position
Results
Descriptive statistics using paired t-test was used to assess changes in pre and post treatment values [Tables 3 and 4] and Pearson's correlation coefficient was calculated to evaluate the reliability of observations [Tables 5 and 6]. 50 lateral cephalograms were randomly selected and reanalyzed after 8-week interval. Dahlberg's formula for was used to calculate the error of the method of measurements [Tables 3 and 4].
Table 3.
Descriptive statistics, method error calculations and paired t test analysis for airway parameters
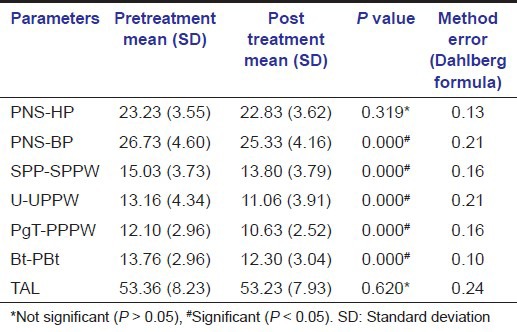
Table 4.
Descriptive statistics, method error calculations and paired t test analysis for hyoid parameters
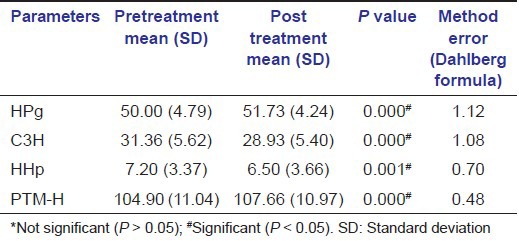
Table 5.
Reliability of airway parameters using Pearson's correlation coefficient (n=150)
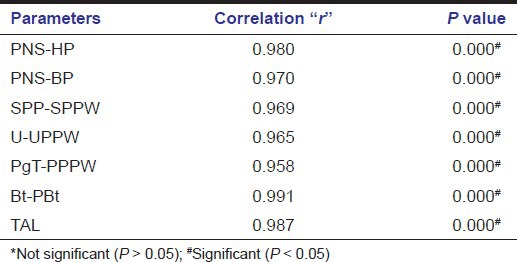
Table 6.
Reliability of hyoid parameters using Pearson's correlation coefficient (n=150)
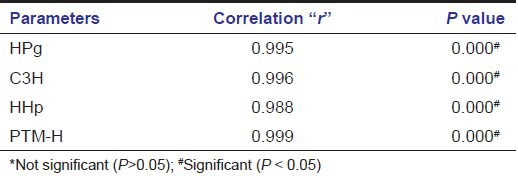
It was observed that the mean values of PNS-HP and TAL showed no statistically significant difference in pre and post treatment groups. Mean values of PNS-BP, SPP-SPPW, U-UPPW, PgT-PPTW and Bt-PBt showed statistically significant difference in pre treatment and post treatment groups. Mean values of HPg, C3H, HHp and PTM-H showed statistically significant difference in pre and post treatment groups. Pearson's correlation coefficient showed statistically significant correlations in all the airway and hyoid parameters. A significant range of 0.95 to 0.99 was observed with airway parameters whereas for hyoid it was found to be ranging from 0.98 to 0.99 [Tables 1–6].
Discussion
The dental, skeletal, and soft tissue effects of extraction and nonextraction treatment continue to be contemplated in the orthodontic literature, just as they have been for over a century. The choice whether or not to extract premolars is intricate, often involving relationships between arch size, occlusion, vertical control, and esthetics. Recently, it has been asserted that airway health should also be a primary consideration before initiating orthodontic treatment with premolar extractions. An existing strife is that orthodontic treatment can move the denture back in the mouth, reducing oral space and restricting pharyngeal volume. The present study probed this assertion, and analysis shows that the extraction of premolars has a detrimental effect on oropharyngeal structures.
Owing to the close relationship between the pharynx and the dentofacial structures, a mutual interaction has long been assumed and studies on the subject have been performed.[7,8] The upper airway in patients with retrognathism or prognathism with physiological breathing showed that the type of malocclusion did not influence the measurements of the airway. The transverse dimension of the nasopharynx is significantly decreased in patients with distoclusion.[9] Joseph et al.[10] assumed that skeletal factors, such as a retrognathic maxilla, can lead to narrowing of the anteroposterior dimensions of the airway. Furthermore, the study showed that hyperdivergent growth of the facial cranium or excessively vertical growth of the maxilla can result in narrowing of the anteroposterior dimensions of the airway.
An important role in securing the pharyngeal airway is also attributed to the hyoid and its musculature. Various studies have demonstrated that changes in the hyoid position can result in changes to the mandibular position. It is reported that in patients with mandibular retrognathism, there was a posterior position of the hyoid associated with narrowing of the upper airway.[11] Abu Allhaija and Al-Khateeb[12] found a significant correlation between jaw relation, hyoid position and width of the pharyngeal cavity. Studies on the influence of surgical advancement or setback of the mandible on the hyoid position and the pharyngeal airway showed that mandibular advancement resulted in forward displacement of the hyoid with widening of the minimum pharyngeal airway (minimum pharyngeal airway: the minimal distance between the base of the tongue and the posterior pharyngeal wall), whereas the opposite was true in the case of the surgical mandibular setback.[13]
Previous studies have shown a possible relationship between pharyngeal airway and skeletal structures, soft tissues, and musculature. Nasopharyngeal airway was increased with maxillary protraction in skeletal Class III children.[14] Changes in the size of nasopharyngeal airway dimension have been reported following rapid maxillary expansion. In addition, controversial findings on the relationship between vertical craniofacial pattern and pharyngeal airway were also demonstrated.[15,16] However, the effects of orthodontic treatment, specifically the effects of anterior tooth retraction on pharyngeal airway after extraction of four premolars in the young adolescents with bimaxillary protrusion, have seldom been discussed.
A recent study indicated that orthodontic treatment with extraction of four premolars did not influence oropharyngeal airway volume in adolescents.[17] However, specific changes of the pharyngeal airway and hyoid bone position were not investigated. Another study reported a decrease of airway space behind the tip of soft palate and tongue in 13 subjects with extraction orthodontic treatment.[18] Other sections of the pharynx, such as nasopharynx, hypopharynx, and airway length were not evaluated. It is well-documented that significant dentofacial changes exist after such orthodontic treatment, including soft-tissue profile and incisor angulation. An alteration of incisors and soft tissue position could potentially affect tongue position and pharyngeal airway.
However, our results differed from the result of a recent study by Valiathan et al.,[17] who demonstrated oropharyngeal volumes did not show significant change after orthodontic treatment with extraction of four premolars in adolescents. The authors attributed this negative finding to mandibular growth and the high variability of oropharyngeal volume. The assertion of some “nonextraction” orthodontists and orthotropists is that treatment, especially with premolar extractions, causes the retraction of anterior teeth, which decreases oral and pharyngeal space, thus impairing airflow. These arguments are of apprehension to patients and parents. The long-term effects of oxygen deprivation from “outdated” extraction treatment are purported to be ominous: developmental delays, migraine headaches, and even obstructive sleep apnea. However, there is only speculation that pharyngeal size is affected by position of the teeth, according to the orthotropists’ beliefs, which are without documentation. This has been addressed in the present study where we quantitatively tested the argument that the pharynx is reduced in size when premolars are extracted.
In addition, the present study also gave equal importance to the most important parameter of physiologic growth. This is that aspect of orthodontic treatment that cannot be ignored; as the majority of orthodontic patients are growing adolescents. In growing patients, structural dimensions expand as the face grows downward and forward.[19] Claims that orthotropic treatment produces downward- and-forward growth are just taking credit for natural growth trajectories and cannot be attributed to treatment. Growth is a powerful and often underrated component of orthodontic treatment and it can easily outweigh the effects of treatment mechanics. It has been found that a greater rate of changes in the soft-tissue measurements of the posterior pharyngeal wall occurred between 6 and 9 years.[7] In this study, the age range was 12-18 years.
In the present study, lateral cephalometric radiographs were used to measure airway dimensions. Using lateral cephalograms to assess the airway dimension is considered a reliable method.[20] Recent armamentaria like Cone Beam Computed Tomography (CBCT) could also be a valuable tool; however, its restricted accessibility in developing countries like India still poses challenges and hence cephalograms are still considered a dependable modus.
Conclusion
In our study, the nasopharyngeal dimension (PNS-HP) and Total Airway Length (TAL) were not found to be directly affected by the retraction of anterior teeth; this can be attributed to the fact that nasopharyngeal dimension and TAL are not under direct influence of tongue position.
In summary, it was observed that the pharyngeal airway size became narrower after the treatment. Extraction of four premolars did affect velopharyngeal, glossopharyngeal, hypopharyngeal, and hyoid position in bimaxillary protrusive young adolescents. The velopharyngeal, glossopharyngeal, and hypopharyngeal airway became narrower following orthodontic therapy. The hyoid bone tends to move in a posterior and inferior direction. The other findings of our study also proved direct correlation of tongue to oropharynx and hypopharynx. Postextraction tongue position directly influenced the hyoid; this again can be attributed to anatomical dependence of hyoid with the hyoglossal muscle. The findings of our study also emphasize clinically relevant anatomic factors that should be given prime importance and serious consideration on the decision whether to extract or not in growing patients. This gives further impetus to utilization of nonarch-length reducing modalities with early interceptive evaluation and treatment in growing children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Palaisa J, Ngan P, Martin C, Razmus T. Use of conventional tomography to evaluate changes in the nasal cavity with rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;132:458–66. doi: 10.1016/j.ajodo.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Al Maaitah E, El Said N, Alhaija Abu ES. First premolar extraction effects on upper airway dimension in bimaxillary proclination patients. Angle Orthod. 2012;82:853–9. doi: 10.2319/101711-646.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aksu M, Kocadereli I. Arch width changes in extraction and nonextraction treatment in class I patients. Angle Orthod. 2005;75:948–52. doi: 10.1043/0003-3219(2005)75[948:AWCIEA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Ong HB, Woods MG. An occlusal and cephalometric analysis of maxillary first and second premolar extraction effects. Angle Orthod. 2001;71:90–102. doi: 10.1043/0003-3219(2001)071<0090:AOACAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Williams R, Hosila FJ. The effect of different extraction sites upon incisor retraction. Am J Orthod. 1976;69:388–410. doi: 10.1016/0002-9416(76)90208-6. [DOI] [PubMed] [Google Scholar]
- 6.Saatci P, Yukay F. The effect of premolar extractions on tooth-size discrepancy. Am J Orthod Dentofacial Orthop. 1997;111:428–34. doi: 10.1016/s0889-5406(97)80025-x. [DOI] [PubMed] [Google Scholar]
- 7.Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1–132. [PubMed] [Google Scholar]
- 8.Solow B, Siersbaek-Nielsen S, Greve E. Airway adequacy, head posture, and craniofacial morphology. Am J Orthod. 1984;86:214–23. doi: 10.1016/0002-9416(84)90373-7. [DOI] [PubMed] [Google Scholar]
- 9.Alves PV, Zhao L, O’Gara M, Patel PK, Bolognese AM. Three-dimensional cephalometric study of upper airway space in skeletal class II and III healthy patients. J Craniofac Surg. 2008;19:1497–507. doi: 10.1097/SCS.0b013e31818972ef. [DOI] [PubMed] [Google Scholar]
- 10.Joseph AA, Elbaum J, Cisneros GJ, Eisig SB. A cephalometric comparative study of the soft tissue airway dimensions in persons with hyperdivergent and normodivergent facial patterns. J Oral Maxillofac Surg. 1998;56:135–9. doi: 10.1016/s0278-2391(98)90850-3. [DOI] [PubMed] [Google Scholar]
- 11.Battagel JM, Johal A, L’Estrange PR, Croft CB, Kotecha B. Changes in airway and hyoid position in response to mandibular protrusion in subjects with obstructive sleep apnoea (OSA) Eur J Orthod. 1999;21:363–76. doi: 10.1093/ejo/21.4.363. [DOI] [PubMed] [Google Scholar]
- 12.Abu Allhaija ES, Al-Khateeb SN. Uvulo-glosso-pharyngeal dimensions in different anteroposterior skeletal patterns. Angle Orthod. 2005;75:1012–8. doi: 10.1043/0003-3219(2005)75[1012:UDIDAS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Achilleos S, Krogstad O, Lyberg T. Surgical mandibular setback and changes in uvuloglossopharyngeal morphology and head posture: A short- and long-term cephalometric study in males. Eur J Orthod. 2000;22:383–94. doi: 10.1093/ejo/22.4.383. [DOI] [PubMed] [Google Scholar]
- 14.Lee JW, Park KH, Kim SH, Park YG, Kim SJ. Correlation between skeletal changes by maxillary protraction and upper airway dimensions. Angle Orthod. 2011;81:426–32. doi: 10.2319/082610-499.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ucar FI, Uysal T. Orofacial airway dimensions in subjects with Class I malocclusion and different growth patterns. Angle Orthod. 2011;81:460–8. doi: 10.2319/091910-545.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grauer D, Cevidanes LS, Styner MA, Ackerman JL, Proffit WR. Pharyngeal airway volume and shape from cone-beam computed tomography: Relationship to facial morphology. Am J Orthod Dentofacial Orthop. 2009;136:805–14. doi: 10.1016/j.ajodo.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valiathan M, El H, Hans MG, Palomo MJ. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–74. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Germec-Cakan D, Taner T, Akan S. Uvulo-glossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. Eur J Orthod. 2011;33:515–20. doi: 10.1093/ejo/cjq109. [DOI] [PubMed] [Google Scholar]
- 19.Enlow DH, Bang S. Growth and remodeling of the human maxilla. Am J Orthod. 1965;51:446–64. doi: 10.1016/0002-9416(65)90242-3. [DOI] [PubMed] [Google Scholar]
- 20.Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D. Comparison of airway space with conventional lateral headfilms and 3-dimensional reconstruction from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2009;135:468–79. doi: 10.1016/j.ajodo.2007.04.043. [DOI] [PubMed] [Google Scholar]


