Abstract
Objective
To assess the barriers to uptake of eye care services among those with avoidable impairment in the population aged ≥40 years in the South Indian state of Andhra Pradesh.
Design
Cross-sectional study.
Setting
Community setting.
Participants
Of 7800 participants recruited from one urban and two rural locations using a two-stage cluster random sampling methodology, 7378 (95%) were examined. Eye examinations were conducted using a rapid assessment protocol. Visual impairment (VI) was defined as presenting visual acuity <6/18 in the better eye. For the purpose of this study, VI caused due to cataract or uncorrected refractive error was considered avoidable VI. A validated questionnaire was used to collect information on barriers for uptake of services among those who had avoidable VI.
Primary outcome
Barriers to uptake of services among those with avoidable VI.
Results
The prevalence of avoidable VI was 11.8% (95% CI 11.0% to 12.5%; n=868). Among these, 71.1% (n=617) individuals reported ‘person-related’ barriers whereas 28.9% (n=251) individuals reported ‘service-related’ barriers to uptake of services. Among the ‘person-related’ barriers, the leading barrier was ‘lack of perceived need’ (61.1%; n=377) for reasons such as old age, good vision in the other eye. This was followed by ‘no one to accompany’ (20.3%; n=125). Of the 251 individuals who had ‘service-related’ barriers, lack of affordability was the major barrier (76.1%; n=191) followed by lack of accessibility (12.7%; n=32). Over 11% (n=28) of the individuals were advised to wait for cataract surgery.
Conclusions
Person-related barriers are more common than service-related barriers in Andhra Pradesh. As the barriers trend more towards ‘person-related’ phenomenon such as person's attitude and ‘felt need’ to improve vision, newer and much intensive awareness campaigns are needed to bring about an attitudinal/behavioural change among individuals to improve the uptake of services.
Keywords: PUBLIC HEALTH, EPIDEMIOLOGY
Strengths and limitations of this study.
Large representative sample from three districts, a good response rate and sound methodology are the strengths of the study.
The division of barriers into ‘person-related’ and ‘service-related’ is arbitrary and subject to discussion.
Our data present the pointers that can help service providers plan strategies to address them but by no means provide in-depth analysis on health-seeking behaviours of the people.
With over 285 million visually impaired people worldwide, visual impairment is a major global public health challenge.1 Over 80% of the blindness is due to cataract and uncorrected refractive errors, both of which have cost-effective solutions.1 2 While technological advances have rendered cataract surgery safe, resulting in excellent outcomes, this technology needs to be accessible to people in remote rural areas in developing nations where visual impairment is more prevalent.1 Making services available is only a part of the larger solution to the global problem of visual impairment. Even in places where services are available and accessible,3 the uptake of services is determined by several factors or barriers that must be addressed if we are to improve the uptake of services and thereby reduce the prevalence of visual impairment. Research has shown that the barriers to uptake of services tend to change over time due to several factors.4 5 Hence research on changing trends is necessary to guide service delivery programmes for planning strategies to address avoidable visual impairment in the community.
Andhra Pradesh is one of the largest states in India with an estimated population of 84 million in 2011.6 It is administratively divided into 23 districts which are further divided into subdistricts (mandals which are rural) and municipalities (urban).6 The literacy rate is around 68% and nearly one-third of the population resides in urban areas as per census 2011.6 Similar to other parts of the country, eye care services are provided by several non-government organisations, private hospitals and clinics, especially in urban areas and by government hospitals.7 In rural areas, several non-government organisations conduct outreach screening programmes to identify people with cataract who are then transported to a base eye hospital where cataract surgery is performed at ‘no cost’ to the people and expenses are reimbursed by National Programme for Control of Blindness (NPCB), India.
We recently conducted a large population-based cross-sectional study among adults 40 years and older in three locations (one urban and two rural) in Andhra Pradesh and reported an age-adjusted and gender-adjusted prevalence of visual impairment of 14.3% (95% CI 13.5% to 15.0%) including a blindness prevalence of 5.5% (95% CI 5.0% to 6.0%).8 Refractive errors were the leading cause of visual impairment accounting for 47.6% followed by cataract (43.7%).8 In this paper, we report the reasons for poor uptake of eye care services among those who are visually impaired due to cataract or refractive errors in this study cohort and suggest strategies to address these barriers.
Methods
Ethics approval
This study adhered to the tenets of the Declaration of Helsinki. Verbal informed consent was obtained from each participant after explaining the study procedures and before starting the eye examination. The studies were carried out during 2011 and 2012.
Data collection
The sampling process and the study protocol are described in detail elsewhere.8 In brief, a two-stage cluster random sampling was used to select 7800 participants from 156 study clusters across three districts, Krishna (urban area), Khammam (rural) and Warangal (rural) in Andhra Pradesh. In each randomly selected cluster, the study teams comprising of a vision technician and a community eye health worker visited the selected households and conducted eye examinations that included visual acuity assessment. Those with visual impairment, defined as presenting visual acuity worse than 6/18 in the better eye were identified. The investigators asked the question: ‘Why were services not sought despite having visual impairment?’. It was an open-ended question and was asked in the local language. The response given by the participants was matched with the responses that were prelisted on the data collection form and the response that was the closest was marked. If a participant gave a response that was different to those listed, then it was fully documented in the forms as ‘others’. If the participant gave multiple responses, then a follow-up questioning was asked to prioritise the response and the most important one was documented. The responses used in the form were based on the questionnaire used in the previous studies in India and were available in the local language.3 9 10 To suggest strategies to increase uptake of services, the responses were further categorised into two groups: (A) person-related barriers and (B) service-related barriers. The proportion of visual impairment caused due to cataract and refractive errors was considered as avoidable visual impairment in this study.
Data analysis was performed using STATA statistical software V.12.11 χ2 Tests were conducted to assess the association between the barriers quoted by the individuals and sociodemographic variables. The point prevalence estimate for prevalence of avoidable blindness was calculated and reported along with 95% CIs. A p value of 0.05 (two-tailed) was considered as statistically significant for all the estimates.
Results
Among the 7800 enumerated from the three districts, 7378 (95%) individuals were available for examination. Of those examined, 46.4% (n=3421) were men, 62% (n=4562) had no education and 66.7% (n=4923) were from rural location. The mean age of those examined was 51.7 years (SD 10.9 years) compared with 52.8 years (SD 9.9 years) of those not examined. The mean difference in age among those examined and not examined was of borderline statistical significance (p=0.05). Women were more likely to be examined compared with men (95.6% vs 93.5%; p<0.01).8
The overall prevalence of avoidable visual impairment was 11.8% (95% CI 11.0% to 12.5%; n=868). It was 9.5% (95% CI 8.4% to 10.8%) and 12.9% (95% CI 12.0% to 13.8%) in urban and rural areas, respectively. The most common reason quoted for not seeking eye care services were ‘old age need not felt’ (29.6%; n=257) followed by ‘unable to afford the cost of services’ (22%; n=191) and no one to accompany (14.4%; n=125) followed by ‘aware of the problem, but can manage ‘(11.2%, n=97; table 1). ‘No one to accompany’ was quoted by 15.9% (n=101) of the participants in the rural area compared with 10.3% (n=24) in the urban area (p=0.04). ‘Unaware of the problem’ and ‘no time available/other priorities’ was quoted more frequently by urban participants compared with their rural peers (p<0.01). Other health reasons were significantly higher among rural residents (p<0.01). The other reasons for not seeking eye care services were similar between the groups (table 1).
Table 1.
Reasons for not utilising care services (n=868)
| Responses | Category | Urban (n=234) | Rural (n=634) | Total (n=868) | Statistical significance |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Old age and need not felt | P | 70 (29.9) | 187 (29.5) | 257 (29.6) | 0.13 |
| Cannot afford | S | 48 (20.5) | 143 (22.6) | 191 (22.0) | 0.52 |
| No one to accompany | P | 24 (10.3) | 101 (15.9) | 125 (14.4) | 0.04 |
| Aware of the problem, but can manage | P | 25 (10.7) | 72 (11.4) | 97 (11.2) | 0.78 |
| Fear of losing eyesight/operation/consultation | P | 6 (2.6) | 35 (5.5) | 41 (4.7) | 0.07 |
| Services not available or very far | S | 11 (4.7) | 21 (3.3) | 32 (3.7) | 0.34 |
| Waiting for cataract to mature | S | 10 (4.3) | 18 (2.8) | 28 (3.2) | 0.29 |
| Other health reasons | P | 1 (0.4) | 27 (4.3) | 28 (3.2) | <0.01 |
| Unaware of the problem | P | 21 (9.0) | 4 (0.6) | 25 (2.9) | <0.01 |
| No time available/other priorities | P | 15 (6.4) | 6 (0.9) | 21 (2.4) | <0.01 |
| One eye adequate vision/need not felt | P | 3 (1.3) | 20 (3.2) | 23 (2.6) | 0.13 |
| Total | 234 (100) | 634 (100) | 868 (100) |
Italics are statistically significant.
P, person-related barrier; S, service-related barrier.
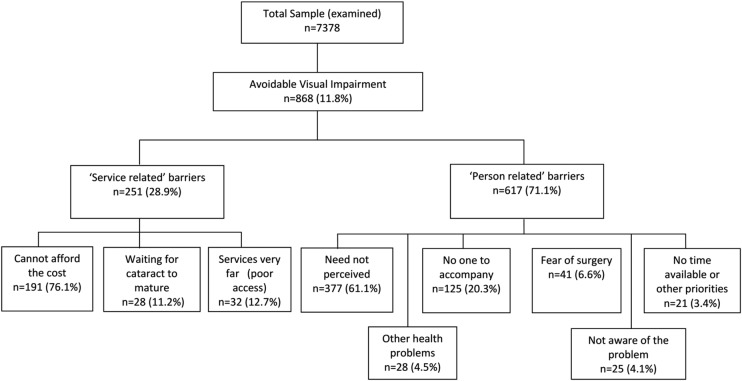
When the above quoted reasons for not seeking eye care services were categorised into ‘person-related’ and ‘service-related’ barriers, of 868 individuals who had avoidable visual impairment, 71.1% (n=617) individuals reported ‘person-related’ barriers while 28.9% (n=251) individuals reported ‘service-related’ barriers for uptake of services. Among the ‘person-related’ barriers, the leading barrier was ‘lack of perceived need’ (61.1%; n=377) for reasons such as old age, good vision in the other eye. This was followed by ‘no one to accompany’ (20.3%; n=125) and ‘fear of surgery or consultation’ (6.6%; n=41) (figure 1).
Figure 1.
Classification of barriers for not utilising eye care services among those with avoidable visual impairment.
Of the 251 individuals who had ‘service-related’ barriers, lack of affordability was the major barrier (76.1%; n=191) followed by lack of accessibility (12.7%; n=32). Over 11% (n=28) of the individuals were advised by an eye care service provider to ‘wait for cataract surgery’ or ‘waiting for cataract to mature’ (figure 1). Except for age groups, the service-related and person-related barriers were similar with respect to all other characteristics such as gender, education, area of residence, level and cause of visual impairment (table 2).
Table 2.
Categories of reasons for not utilising eye care services stratified by sociodemographic variables and causes of visual impairment (VI)
| Total in the group with avoidable VI | Service-related barriers (n=251) |
Person-related barriers (n=617) |
p Value* | |||
|---|---|---|---|---|---|---|
| n | n | Per cent† | n | Per cent† | ||
| Age group (years) | <0.01 | |||||
| 40–49 | 55 | 25 | 10.0 | 30 | 4.9 | |
| 50–59 | 181 | 69 | 27.5 | 112 | 18.2 | |
| 60–69 | 330 | 97 | 38.6 | 233 | 37.8 | |
| 70 and above | 302 | 60 | 23.9 | 242 | 39.2 | |
| Gender | 0.63 | |||||
| Male | 381 | 107 | 42.6 | 274 | 44.6 | |
| Female | 487 | 144 | 57.4 | 343 | 55.6 | |
| Education | 0.58 | |||||
| No education | 720 | 211 | 84.1 | 509 | 82.5 | |
| Educated | 148 | 40 | 15.9 | 108 | 17.5 | |
| Area of residence | 0.82 | |||||
| Urban | 234 | 69 | 27.5 | 165 | 26.7 | |
| Rural | 634 | 182 | 72.5 | 452 | 73.3 | |
| Categories of VI | 0.44 | |||||
| <6/18–6/60 | 553 | 155 | 61.8 | 398 | 64.5 | |
| <6/60 | 315 | 96 | 38.2 | 219 | 35.5 | |
| Cause of VI | 0.54 | |||||
| Cataract | 401 | 120 | 47.8 | 281 | 45.5 | |
| Refractive error | 467 | 131 | 52.2 | 336 | 54.5 | |
| Total | 868 | 251 | 100.0 | 617 | 100.0 | |
Italics are statistically significant.
*p Values comparing the service-related and person-related barriers.
†Column percentages presented.
Discussion
We found an overwhelming predominance of ‘person-related’ barriers compared with ‘service-related’ barriers compared with previous studies suggestive of a clear change in trends in barriers over time.4 9 10 12–14 Earlier studies that were conducted about two decades ago revealed ‘service-related’ barriers such as availability, accessibility and affordability in sharp contrast to ‘person-related’ barriers found in this study.4 9 10 12–14 In 1995, Gupta and Murthy14 reported distance as the leading barrier for uptake of services followed by economic and other reasons whereas accessibility was not a major barrier in the current study.
In the past few decades, the availability of services has increased significantly due to efforts of several non-government agencies and the national programme for prevention of blindness. Despite this, lack of affordability continues to remain a concern and still is a leading barrier. Recent studies from Andhra Pradesh also reported economic reasons as one of the leading barriers for uptake of services.5 15 Affordability was a leading barrier (41%), similar to that found in Tamil Nadu16 (78.2%) and another study from an urban area in Andhra Pradesh.9 However, in the rural component of this study, it was not an important barrier.10 Although some services are provided at no cost, the indirect expenses such as lost wages, travel and other incidental expenses may be posing an economic hurdle for uptake of services.16 17 The service delivery programmes need to consider ways to address the issues related to ‘indirect costs’ by providing transport facilities.
Lack of escort was quoted more commonly in Karnataka (21.6%) and Tamil Nadu (58.2%) compared with 14.4% in the present study.4 16 However, ‘waiting or was told to wait for cataract surgery’ was the leading reasons in the Karnataka study whereas it was reported only by 3% of the respondents in our study.4 These differences are indicative of the changing trends in barriers for uptake of services over time. Similarly, the ‘fear of surgery or visual outcome after surgery’ was more commonly reported from Tamil Nadu17 and Karnataka,4 compared with less than 5% of the participants in the present study, again suggestive of a changing trend.
The reasons, such as ‘fear of surgery’ and ‘waiting or was told to wait for cataract to mature for surgery’, are reminiscent of the days when intracapsular cataract extraction was the commonly performed procedure in the camp settings. In fact, population-based studies that were conducted over a decade ago in several parts of India revealed poor outcomes after cataract surgery.18 19 However, technological advances and increase in availability of cataract surgical services support by NPCB are resulting in better outcomes as evidenced by recent publications.20 21 However, efforts are needed to pass this information on to the communities using effective information, education and communication tools so that these barriers are addressed. Similar is the case with those reporting about ‘other commitments’ that prevent them from undergoing cataract surgery and ‘old age’ and ‘need not felt’; there appears to be perception in the community on the need for long period of rest after cataract surgery that will keep them away from active work engagements for a considerable period of time. The quick visual rehabilitation that is now possible with better surgical techniques at a low cost even in small towns in India should be propagated more actively.
Availability was reported by less than 5% of those with avoidable visual impairment in urban and rural areas in the present study suggesting increased availability of services. ‘Old age and need not felt’ was reported by nearly 30% of the respondents which relates to individual attitudes. A significantly higher proportion of rural residents reported ‘no one to accompany’ compared with their urban counterparts and overall it accounted for nearly 15% of the responses. This could be attributed to availability of services at much closer distances or better conveyance in urban locations compared with rural locations.
The individuals who are aware of their visual impairment but do not perceive the need for consultations owing to several reasons are more challenging for service providers to deal with as it is related to attitude. This finding was also reported in earlier studies in different parts of India.3 10 Only effective Information, education and communication (IEC) methods focused on relative ease and safety of cataract surgery that can be undertaken now, compared with yesteryear's strenuous planning and efforts, may induce a proportion of these people to utilise the services. The same holds true for those who do not perceive any eye problem despite having visual impairment.
We did not find any difference in ‘person-related’ and ‘service-related’ barriers among those with cataract and uncorrected refractive errors though they require a very different intervention. This could be possible as the barrier question was asked to all those with avoidable visual impairment and not specific to a cause. It is possible that a significant proportion of people may not have known the cause of their visual impairment. It is also possible that some of those who were visually impaired due to uncorrected refractive errors felt that their visual impairment was due to cataract and not refractive errors and vice versa.
Our study is not free from limitations. As the participants were aware of the affiliation of the study teams, the responses may have been biased (courtesy bias). Moreover, the earlier studies were focused on cataract compared with avoidable visual impairment in our study, though we found no difference in barriers with the avoidable causes of visual impairment. Our data present the pointers that can help service providers plan strategies to address them but by no means provide in-depth analysis on health-seeking behaviours.
In conclusion, as the barriers trend more towards ‘person-related’ phenomenon such as person's attitude and ‘felt need’ to improve vision, newer and much intensive awareness campaigns are needed to bring about an attitudinal/behavioural change among individuals to improve the uptake of services. Only such focused and innovative approaches can improve uptake of services through which the goal of eliminating avoidable visual impairment can be achieved.22–24
Supplementary Material
Acknowledgments
Authors thank S Narsaiah, K Eswara Rao, Ch Rajesh, D Susheel Kumar, N Raja Shekar Reddy, S Narahari, B Raghavendra and D Raghuswamy for their assistance in fieldwork and data collection. LVPEI acknowledges the volunteers for their participation in the study. Dr Sreedevi Yadavalli is acknowledged for her language inputs on earlier versions of the manuscript. Authors are thankful to Dr Usha Raman (University of Hyderabad) and Professor Jill Keeffe for their comments on the earlier versions of this manuscript.
Footnotes
Contributors: SM conceived the idea, and planned and implemented the study. RCK and GNR reviewed the earlier versions of the manuscript and provided inputs. KS helped in the data collection. All authors approved the final version of the manuscript.
Funding: The financial support for this study was provided by Hyderabad Eye Research Foundation, India.
Competing interests: None.
Ethics approval: Institutional Review Board (IRB) of Hyderabad Eye Research Foundation, L V Prasad Eye Institute, Hyderabad, India.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614–18 [DOI] [PubMed] [Google Scholar]
- 2.Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology 2007;114:1670–8 [DOI] [PubMed] [Google Scholar]
- 3.Marmamula S, Keeffe JE, Raman U, et al. Population-based cross-sectional study of barriers to utilisation of refraction services in South India: Rapid Assessment of Refractive Errors (RARE) Study. BMJ 2011;1:e000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vaidyanathan K, Limburg H, Foster A, et al. Changing trends in barriers to cataract surgery in India. Bull World Health Organ 1999;77:104–9 [PMC free article] [PubMed] [Google Scholar]
- 5.Finger RP, Ali M, Earnest J, et al. Cataract surgery in Andhra Pradesh state, India: an investigation into uptake following outreach screening camps. Ophthalmic Epidemiol 2007;14:327–32 [DOI] [PubMed] [Google Scholar]
- 6.Census 2011. Registrar General and Census Commissioner, Census of India 2011. New Delhi: Ministry of Home Affairs, Government of India, 2011 [Google Scholar]
- 7.Thomas R, Paul P, Rao GN, et al. Present status of eye care in India. Surv Ophthalmol 2005;50:85–101 [DOI] [PubMed] [Google Scholar]
- 8.Marmamula S, Narsaiah S, Shekhar K, et al. Visual impairment in the South Indian state of Andhra Pradesh: Andhra Pradesh—Rapid Assessment of Visual Impairment (AP-RAVI) project. PLoS ONE 2013;8:e70120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dandona R, Dandona L, Naduvilath TJ, et al. Utilisation of eyecare services in an urban population in southern India: the Andhra Pradesh eye disease study. Br J Ophthalmol 2000;84:22–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kovai V, Krishnaiah S, Shamanna BR, et al. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol 2007;55:365–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.StataCorp. Stata statistical software: release 12. College Station, TX: StataCorp LP, 2011 [Google Scholar]
- 12.Brilliant GE, Lepkowski JM, Zurita B, et al. Social determinants of cataract surgery utilization in south India. The operations research group. Arch Ophthalmol 1991;109:584–9 [DOI] [PubMed] [Google Scholar]
- 13.Finger RP. Cataracts in India: current situation, access, and barriers to services over time. Ophthalmic Epidemiol 2007;14:112–18 [DOI] [PubMed] [Google Scholar]
- 14.Gupta SK, Murthy GV. Where do persons with blindness caused by cataracts in rural areas of India seek treatment and why? Arch Ophthalmol 1995;113:1337–40 [DOI] [PubMed] [Google Scholar]
- 15.Marmamula S, Narsaiah S, Shekhar K, et al. Visual impairment among weaving communities in Prakasam district in South India. PLoS ONE 2013;8:e55924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nirmalan PK, Katz J, Robin AL, et al. Utilisation of eye care services in rural south India: the Aravind Comprehensive Eye Survey. Br J Ophthalmol 2004;88:1237–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher AE, Donoghue M, Devavaram J, et al. Low uptake of eye services in rural India: a challenge for programs of blindness prevention. Arch Ophthalmol 1999;117:1393–9 [DOI] [PubMed] [Google Scholar]
- 18.Anand R, Gupta A, Ram J, et al. Visual outcome following cataract surgery in rural Punjab. Indian J Ophthalmol 2000;48:153–8 [PubMed] [Google Scholar]
- 19.Dandona L, Dandona R, Anand R, et al. Outcome and number of cataract surgeries in India: policy issues for blindness control. Clin Experiment Ophthalmol 2003;31:23–31 [DOI] [PubMed] [Google Scholar]
- 20.Khanna RC, Marmamula S, Krishnaiah S, et al. Changing trends in the prevalence of blindness and visual impairment in a rural district of India: systematic observations over a decade. Indian J Ophthalmol 2012;60:492–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khanna RC, Pallerla SR, Eeda SS, et al. Population based outcomes of cataract surgery in three tribal areas of Andhra Pradesh, India: risk factors for poor outcomes. PLoS ONE 2012;7:e35701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khanna R, Raman U, Rao GN. Blindness and poverty in India: the way forward. Clin Exp Optom 2007;90:406–14 [DOI] [PubMed] [Google Scholar]
- 23.Rao GN. An infrastructure model for the implementation of VISION 2020: the right to sight. Can J Ophthalmol 2004;39:589–94 [DOI] [PubMed] [Google Scholar]
- 24.Rao GN, Khanna RC, Athota SM, et al. Integrated model of primary and secondary eye care for underserved rural areas: the L V Prasad Eye Institute experience. Indian J Ophthalmol 2012;60:396–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.