Abstract
Objectives:
To assess the effectiveness of school-based interventions program in reducing the prevalence of overweight or obesity among schoolchildren.
Data source:
Ovid Medline (1950-December 2012), Embase (1980-2012), CINAHL (1982-2012), secondary references, review articles, and expert in the field.
Study selection:
All published clinical trials were eligible for study if were randomized, methodologically strong-based on a validity assessment, aimed to evaluate a school-based intervention for childhood overweight or obesity, and measured outcome in term of prevalence/incidence difference in overweight and obesity among both groups. Studies involved in cost-effective analysis of school-based intervention have been excluded. Data from eligible studies abstracted and pooled for relative risk.
Results:
Five trials with 3,904 schoolchildren were included. Mean age of the students (boys and girls) ranges 8.6-12.6 years. Meta-analysis showed a statistical significance beneficial effect of school-based intervention programs on obesity status of schoolchildren (risk ratio (RR) 0.58, 95% confidence interval (CI) 0.43-0.78) and suggested 42% reduction in prevalence of obesity among schoolchildren through school-based intervention programs. Individual studies also showed effectiveness of these school-based interventions.
Conclusion:
School-based intervention programs are effective in prevention of childhood overweight and obesity problem and our results quantitatively supported this argument.
Keywords: Children, obesity, overweight, school-based intervention
Introduction
Childhood overweight and obesity is a global public health problem that is responsible for childhood morbidity and mortality and also increase the risk of obesity, cardiovascular disease (CVD), diabetes mellitus (DM), osteoarthritis, and many types of cancers in adulthood.(1,2,3,4) The prevalence of overweight was 17% among the US children (2-19 years).(5) Similarly, 10-35% prevalence of overweight and obesity among children has been reported from the European countries.(6,7,8,9) This problem is no longer detained to the developed world as its rising trend has been observed now in the developing part of the world.(10,11,12,13)
It has potential adverse health consequences, that is, insulin resistance, cardiovascular diseases (CVD) risk factors, and early progression of atherosclerosis which lead to premature deaths.(14,15,16,17) Therefore, preventing childhood overweight and obesity may be an effective means to reduce the risk of undesirable health outcomes.
It has been recognized that schools can be an avenue for interventions directing childhood obesity.(4) Legislation and guidelines have been approved in a few countries for implementation of school-based intervention such as the US.(18,19) Many of the studies(20,21,22,23,24,25,26) have shown effectiveness of school-based interventions whereas other reported contrast results.(27,28,29,30,31) Hence, so far no conclusion has been drawn. The objective of this review is to assess the effectiveness of school-based interventions program compared to routine curriculum in reducing the prevalence of overweight or obesity among schoolchildren.
Materials and Methods
Searches
Terminologies such as overweight, obesity, physical activity, exercise, diet, schoolchildren etc., have been used for search. Main search engines were Ovid Medline (1950-December 2012), Embase (1980-2012), CINAHL (1982-2012), and PubMed. Secondary references and review articles were also scanned for thematic review. Hand search of the journal was also done. Language of studies was restricted to the English only.
Selection of studies
All published clinical trials were eligible for study if were randomized, aimed to evaluate a school-based intervention for childhood overweight and obesity, and measured outcome in terms of prevalence/incidence difference in overweight and obesity among both groups. There was no strict criterion applied for the control group. Studies involved in cost effective analysis, or done on high risk population only, or objectives were focused on physical activity/diet and not on overweight/obesity have been excluded.
Assessment of validity
According to Cochrane Collaboration's recommendations, the quality of the included studies was assessed for the appropriateness of randomization, intervention allocation, blindness, follow up, sample size, and intention-to-treat analysis based on criterion of Guyatt et al.(32)
Extraction of data
Data was extracted for the year of publication, journal's name, study's objectives, design, place, population, age, gender, type and duration of intervention, control group, randomization, blindness, sample size, power calculation, outcome, type of analysis, and results. Double data entry was done in Review Manager 5.
Quantitative data synthesis
Meta-analysis was based on post-intervention prevalence of overweight and obesity in both groups. Relative risks were used as the measure of risk along with 95% confidence intervals. Mantel-Haenszel (statistical method), fixed effects (analysis model), and risk ratio (effect measure) were used to make comparison among studies. Heterogeneity among studies was assessed by I2 statistics, chi2, and a P-value. I2 > 50% and P-value of chi2 < 0.05 was considered as high level of heterogeneity. The effect of an individual study on an overall summary measure was assessed by Jackknife analysis.
Results
Search identified 325 citations from Ovid Medline, 275 from Embase, 468 from CINAHL, and 213 from PubMed. Additional studies were found by hand searched (n = 3) and secondary references (n = 5). The total number of citations was 1,289 which reduced to 156 after title screening. After removing 37 duplicate studies, a total of 119 studies were left. Abstract screening excluded 76 nonexperimental studies, and 28 studies were either community-based, both school- and community-based, or involved parents as well. The remaining 15 potentially appropriate studies were examined for inclusion/exclusion criteria and quality assessment. Ten of clinical trials were excluded because; involved cost effectiveness analysis of an intervention (n = 1),(33) outcome was other than overweight/obesity reduction (n = 6),(34,35,36,37,38,39) conducted among the high risk population only (n = 1),(40) and nonrandomized clinical trials (n = 2).(41,42) Prisma flow diagram shows the summary of study selection process [Figure 1]. Table 1 summarizes the characteristics of the excluded studies.
Figure 1.
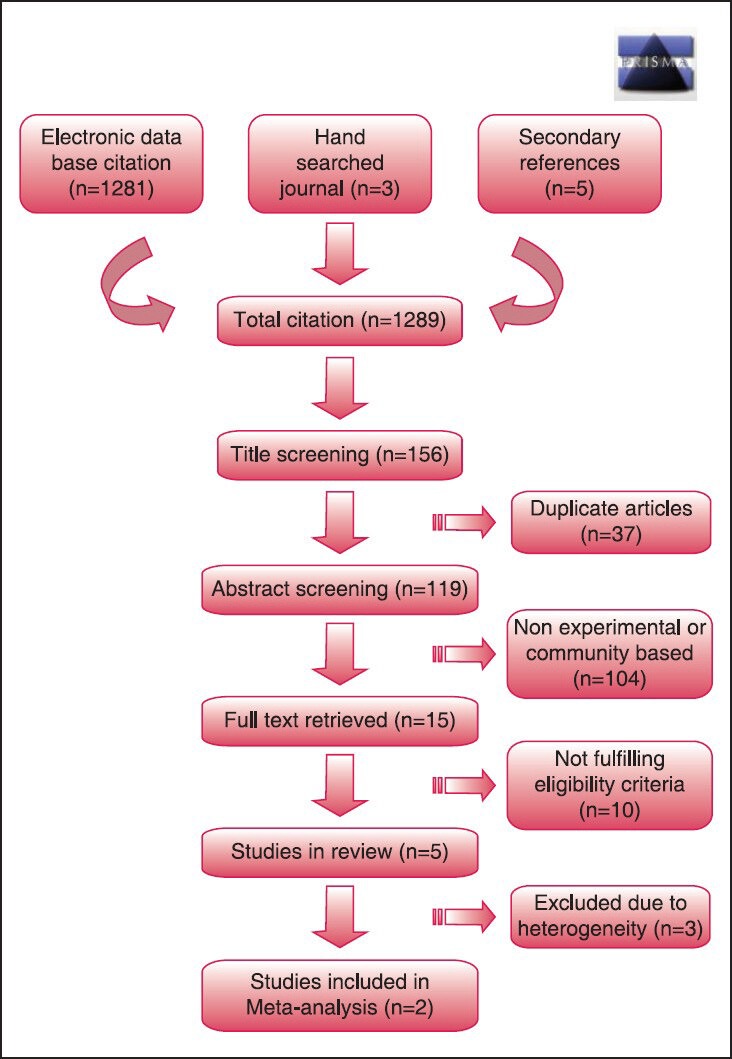
Prisma flow diagram
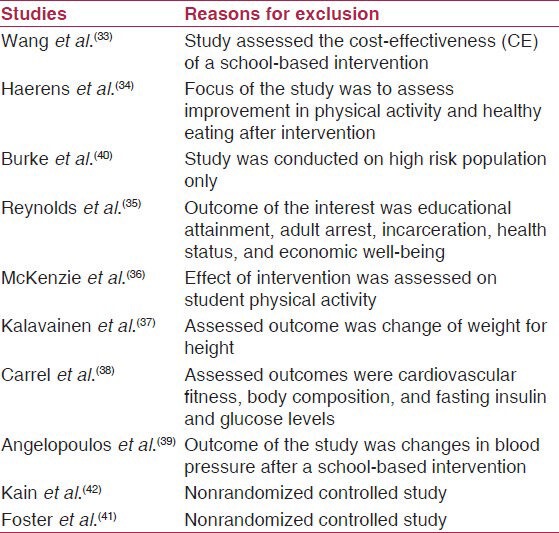
Table 1.
Characteristics of the excluded studies
Study characteristics
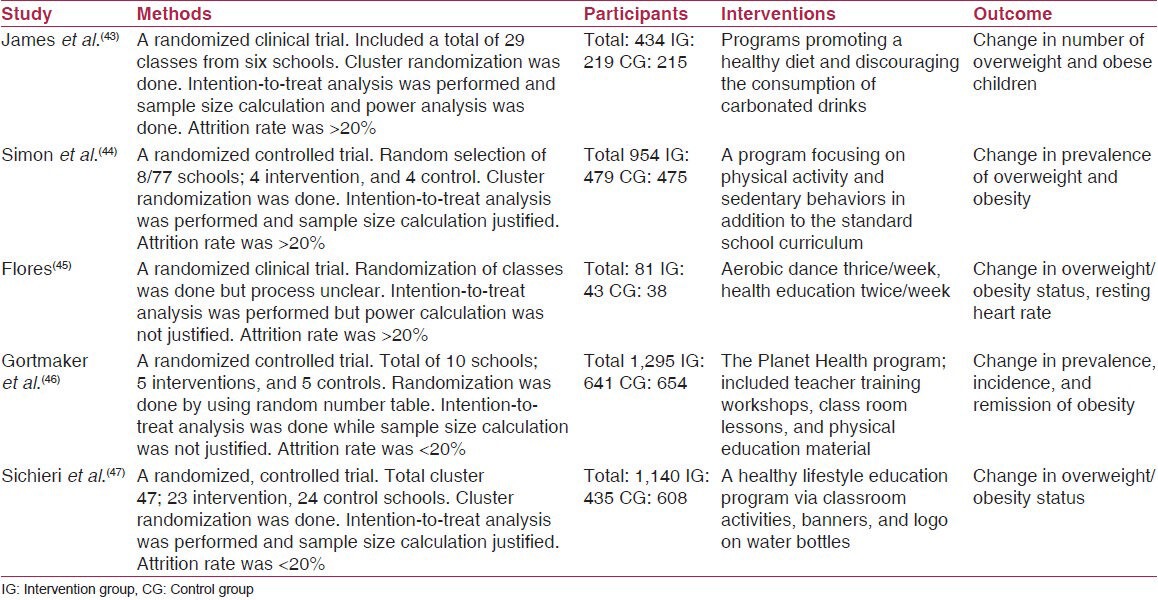
Table 2 shows the five trials included in the review with a total of 3,904 schoolchildren, published between 1995 and 2009 [Table 2]. These trials were conducted in England,(43) France,(44) Canada,(45) US,(46) and Brazil.(47) All included trials were school-based and intervention duration ranged from 1 to 4 years.
Table 2.
Characteristics of the included studies
Population characteristics
Study population was schoolchildren and it included both boys and girls. Mean age of the children ranged from 8.6 to 12.6 years.
Types of interventions
There was variation among trials in terms of type of interventions. These interventions included; planet health program which included teacher training workshops, classroom lessons, physical education material,(46) education program focused on improving physical activity and discouraging sedentary lifestyle,(44) program contained classroom activities, banners and logo on water bottles for promoting healthy lifestyle,(47) program promoting healthy diet and discouraging consumption of carbonated drinks,(43) and aerobic dance.(45) Although, no strict criterion applied for the control group during selection of studies, the usual school curriculum promoting healthy lifestyle was considered as control in found studies.
Outcome (reduction in overweight or obesity) assessment
Reduction in overweight or obesity status has been assessed by change in body mass index (BMI),(43,44,45,46,47) triceps skin fold (TSF) thickness,(46) and BMI Z-score change.(43)
Methodological quality
All of the included studies were randomized clinical trial (RCT).(43,44,45,46,47) Randomization was done with random number table;(46) three of the trials used cluster randomization;(43,44,47) while in one it was not clear.(45) Due to nature of intervention, blinding was not possible in any of the trials.(43,44,45,46,47) Three of the trials showed sample size calculation and power analysis,(43,44,47) whereas remaining two did not.(45,46) All of the trials analyzed their data by using intention-to-treat analysis.(43,44,45,46,47) Two of the studies had attrition rate <20%,(46,47) whereas in the remaining three it was >20%.(43,44,45)
Narrative data synthesis
Description of included RCTs is summarized below in context of their intervention:
Promotion of healthy diet and discouraging of carbonated drinks
It was a RCT conducted in Christchurch, Dorset, England to assess the long-term effects of school-based intervention program on childhood obesity.(43) Mean age of students was 8.6 years. The intervention program had four sessions to promote healthy diet and to discourage the carbonated drinks. The main outcome was change in BMI Z-score. Intention-to-treat analysis was performed. There was a decrease of -0.01 (SD 0.58) in BMI Z-score in intervention group, but increased in the control group by 0.10 (SD 0.53), with a significant mean difference of 0.10 (95% confidence interval (CI), 0.00-0.21; P-value = 0.06) at 12 months of intervention. However, there was no difference in both groups after 3 years of intervention.
Promotion of physical activity
It was a RCT conducted in Ban-Rhin, France to assess the effect of an intervention (promotion of physical activity) which integrate environmental changes to prevent obesity among schoolchildren through.(44) Mean age of students was 11.7 years. The focus of the intervention program was physical activity and sedentary lifestyle along with routine curriculum. The outcome was change in the prevalence of overweight and obesity. After 4th year of intervention, 4.2% of the initially normal weight children were overweight in intervention group, compared to 9.8% in control group (OR, 0.41; 95% CI 0.22-0.75; P-value = 0.01). Similarly, there was significant improvement in physical activity (P-value = 0.0001) of participants with reduction in duration of watching TV/video (P-value = 0.01) in intervention group.
Aerobic dance and health education
It was a RCT conducted in East Palo Alto to assess the effect of dance on students’ aerobic capacity, weight reduction, level of physical fitness.(45) Mean age of students (boys and girls) was 12.6 years. There was a 50 min class thrice a week, 10 min for warm up, and 40 min for aerobic dance. For health education class students met twice/week. Main outcome of the studies included; number of mile run, resting heart rate, BMI change, and attitude towards physical activity. Intention-to-treat analysis was performed. Intervention significantly reduces BMI and heart rate among girls, but not in boys.
The Planet Health program
It was a RCT conducted in Boston, USA to assess the effect of school-based health behavior intervention (Planet Health program) on childhood obesity students of grades 6-8 years.(46) Mean age of the students was 11.7 years. This program contained teacher training workshops, class room lessons, and physical education material. The main outcome was change in prevalence, incidence, and remission of obesity. Intention-to-treat analysis was done. Intervention significantly reduced prevalence of obesity among girls compared with controls (OR 0.47, 95% CI 0.24-0.93, P-value = 0.03), while among boys there was no difference.
A healthy lifestyle education program
It was a RCT conducted in Rio de Janeiro, Brazil, to assess the effect of an intervention program which discourages students from drinking sugar-sweetened drinks to reduce obesity.(47) Mean age of the students was 10.9 years. Main outcome was change in overweight/obesity status. In intervention group there was significant reduction in daily usage of sugar-sweetened drinks than control group (mean difference = −56 ml, 95% CI −19 to −7 ml), but without significant reduction in BMI (P-value = 0.33). However, there was a significant BMI reduction (P-value = 0.009) among girls.
Studies included in the review suggest the effectiveness of school-based programs for prevention of obesity among children especially among girls. The study that promoted physical activity reported 61% less risk of being obese in intervention group than control.(44) Another study which conducted 40 min aerobic dance thrice a week and health education class twice/week reported significant reduction in BMI and heart rate among girls only.(45) Similarly, the study with Planet Health program showed 53% risk reduction of being obese in intervention group as compare to control, but only among girls.(46) Discouraging of sugar-sweetened drinks use, although reduced uptake of drinks but failed to reduce significant BMI change of the students. However, this intervention causes significant BMI reduction among girls.(47) A similar study, which discouraged carbonated drinks along with promoting healthy diet showed promising results in term of reducing BMI Z-score at 12 months, however these results were not sustained in long run (at 3 years).(43)
Quantitative data synthesis
Effectiveness of a school-based intervention was based on producing statistical significant differences between the intervention and control groups in terms of prevalence of overweight and obesity at the end of study. Meta-analysis was done on only two of the studies(43,44) included in review. Heterogeneity was more than 50% if any of the remaining three studies were included,(45,46,47) evident by I2 > 50% and P-value of chi2 < 0.05. Removal of trials at risk of bias reduced heterogeneity and improved significance of our results. The studies included in meta-analysis showed a statistical significance beneficial effect of school-based intervention programs on obesity status of schoolchildren (two trials, n = 1,166; risk ratio (RR) 0.58, 95% CI 0.43-0.78) (Figure 2). These results suggested 42% reduction in prevalence of obesity among schoolchildren through school-based interventions.
Figure 2.
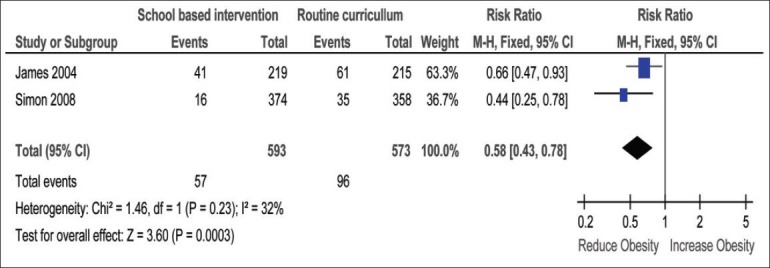
Meta-analysis output graph
Discussion
The narrative review of school-based programs shows effectiveness of intervention targeted towards childhood obesity. It is important to note that the included studies in review were diverse in term of type of interventions, duration, and outcome assessment. Due to heterogeneity, 2/5 studies could be included in meta-analysis. Although meta-analysis result are in the favor of interventions, have limited generalizability due to small number of studies.
Our results are consistent with other studies reporting effectiveness of school-based interventions for childhood obesity.(20,21,22,23,24,25,26) Contrarily, there are studies which reported ineffectiveness of school-based interventions.(27,28,29,30,31) The success and failure of interventions depend upon multiple factors such as duration of intervention, quality of education or diet programs, and more importantly adherence rate of schoolchildren to those interventions. Individual studies showed that these intervention work well in girls as compared to boys.(45,46,47) This difference in effectiveness may be due to variation in casual factors among both gender, however there is dearth of knowledge to support this hypothesis. On the other hand, girls could be more accustomed to issue of weight, body shape, physical activity, and diet consequently more quickly responding to these interventions.(45,46,47,48) As far as other success factors are concerned, a positive role of family has been acknowledged as a success factor for school-based interventions. Similarly, involvement of school teachers and staffs can also enhance and sustain the effect of interventions as recommended earlier.(49)
Recommendations
Despite lack of rigorous data to support specific intervention, we would recommend that school-based intervention programs be placed for intervention of childhood obesity. An intervention might work differently across gender and there may be need to use different gender specific techniques to enhance effectiveness, especially in context of developing countries such as India, Pakistan, and Bangladesh where higher proportion of boys than girls are studying in schools. Along with school-based interventions, attention should also be paid on environments and cultural practices, that is, involvement of parents, teachers, and school staff that could support and encourage children. More importantly, interventions need to be developed and implement into existing operating systems, instead of demanding extra resources. Further researches should include home component along with school-based interventions to address overall health behavior of children especially of younger age group (< 3 years).
Limitations
There are certain limitations of review which should be considered during interpretation of results. Inclusion of studies published in English only might have induced the reporting bias. Though, selected studies were of good methodological quality, but often not included details of training, qualifications of intervention provider, and the extent to which they followed the protocol. Moreover, the variation in school-based interventions and end points of studies, represent a significant challenge to meaningfully evaluate these interventions as a whole especially in meta-analysis.
Conclusion
Childhood overweight and obesity is a global public health issue that needs urgent attention of health policy makers. Schools are the best avenue to address this global problem and our results quantitatively supported this argument. The best school-based intervention program will be one which will reduce incidence and prevalence of overweight/obesity across gender without initiating an inappropriate weight controlling behaviors. Public health persons especially health services researchers have to lead in identifying pragmatic and cost effective school-based programs.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Guo SS. The predictive value of childhood body mass index values for overweight at age of 35 years. Am J Clin Nutr. 1999;59:810–9. doi: 10.1093/ajcn/59.4.810. [DOI] [PubMed] [Google Scholar]
- 2.Mahoney LT, Burns TL, Stanford W, Thompson BH, Witt JD, Rost CA, et al. Coronary risk factors measured in childhood and young adult life are associated with coronary artery calcification in young adults: The Muscatine Study. J Am Coll Cardiol. 1996;27:277–84. doi: 10.1016/0735-1097(95)00461-0. [DOI] [PubMed] [Google Scholar]
- 3.Srinivasan SR. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: The Bogalusa Heart Study. Metabolism. 1996;45:235–40. doi: 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 4.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: An evidence-based review. Obesity. 2008;16:1009–18. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 6.Apfelbacher CJ, Cairns J, Bruckner T, Mohrenschlager M, Behrendt H, Ring J, et al. Prevalence of overweight and obesity in East and West German children in the decade after reunification: Population-based series of cross-sectional studies. J Epidemiol Community Health. 2008;62:125–30. doi: 10.1136/jech.2007.062117. [DOI] [PubMed] [Google Scholar]
- 7.Lobstein T, James WP, Cole TJ. Increasing levels of excess weight among children in England. Int J Obes Relat Metab Disord. 2003;27:1136–8. doi: 10.1038/sj.ijo.0802324. [DOI] [PubMed] [Google Scholar]
- 8.Karayiannis D, Yannakoulia M, Terzidou M, Sidossis LS, Kokkevi A. Prevalence of overweight and prevalence in Greek school-aged children and adolescent. Eur J Clin Nutr. 2003;57:1189–92. doi: 10.1038/sj.ejcn.1601743. [DOI] [PubMed] [Google Scholar]
- 9.Moreno LA, Sarria A, Popkin BM. The nutrition transition in Spain: A European Mediterranean country. Eur J Clin Nutr. 2002;56:992–1003. doi: 10.1038/sj.ejcn.1601414. [DOI] [PubMed] [Google Scholar]
- 10.Caprio S, Genel M. Confronting the epidemic of childhood obesity. Pediatrics. 2005;115:494–5. doi: 10.1542/peds.2004-2165. [DOI] [PubMed] [Google Scholar]
- 11.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: Public-health crisis, common sense cure. Lancet. 2002;360:473–82. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- 12.Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Hosseini M, Gouya MM, et al. Caspian Study Group. Thinness, overweight and obesity in a national sample of Iranian children and adolescents: CASPIAN Study. Child Care Health Dev. 2008;34:44–54. doi: 10.1111/j.1365-2214.2007.00744.x. [DOI] [PubMed] [Google Scholar]
- 13.Misra A, Vikram NK, Sharma R, Basit A. High prevalence of obesity and associated risk factors in urban children in India and Pakistan highlights immediate need to initiate primary prevention program for diabetes and coronary heart disease in schools. Diabetes Res Clin Pract. 2006;71:101–2. doi: 10.1016/j.diabres.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;38:1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 15.Davis PH, Dawson JD, Riley WA, Lauer RM. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: The Muscatine Study. Circulation. 2001;104:2815–9. doi: 10.1161/hc4601.099486. [DOI] [PubMed] [Google Scholar]
- 16.Kiess W, Galler A, Reich A, Muller G, Kapellen T, Deutscher J, et al. Clinical aspects of obesity in childhood and adolescence. Obes Rev. 2001;2:29–36. doi: 10.1046/j.1467-789x.2001.00017.x. [DOI] [PubMed] [Google Scholar]
- 17.Smoak CG, Burke GL, Webber LS, Harsha DW, Srinivasan SR, Berenson GS. Relation of obesity to clustering of cardiovascular disease risk factors in children and young adults. The Bogalusa Heart Study. Am J Epidemiol. 1987;125:364–72. doi: 10.1093/oxfordjournals.aje.a114543. [DOI] [PubMed] [Google Scholar]
- 18.State Actions to Promote Nutrition, Increase Physical Activity and Prevent Obesity: A Legislative Overview. Health Policy Tracking Service 2005. [Online] [Last accessed on 2013 Jan 15]. Available from: www.rwjf.org/files/publications/State_Obesity_Action_October_2005.pdf .
- 19.National Institute for Health and Clinical Excellence. CG43 obesity: full guideline section 3-prevention: evidence statements and reviews. [Online] [Last accessed on 2013 Jan 17]. Available from: http://guidance.nice.org.uk/CG43 .
- 20.Robinson TN. Reducing children's television viewing to prevent obesity: A randomized controlled trial. JAMA. 1999;282:1561–7. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 21.Lee IM. Dose-response relation between physical activity and fitness: Even a little is good; more is better. JAMA. 2007;297:2137–9. doi: 10.1001/jama.297.19.2137. [DOI] [PubMed] [Google Scholar]
- 22.Harrell JS, McMurray RG, Bangdiwala SI, Frauman AC, Gansky SA, Bradley CB. Effects of a school-based intervention to reduce cardiovascular disease risk factors in elementary-school children: The Cardiovascular Health in Children (CHIC) study. J Pediatr. 1996;28:797–805. doi: 10.1016/s0022-3476(96)70332-3. [DOI] [PubMed] [Google Scholar]
- 23.McMurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adolesc Health. 2002;31:125–32. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 24.Kain J, Uauy R, Albala, Vio F, Cerda R, Leyton B. School-based obesity prevention in Chilean primary school children: Methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord. 2004;28:483–93. doi: 10.1038/sj.ijo.0802611. [DOI] [PubMed] [Google Scholar]
- 25.Austin SB, Field AE, Wiecha J, Peterson KE, Gortmaker SL. The impact of a school-based obesity prevention trial on disordered weight-control behaviors in early adolescent girls. Arch Pediatr Adolesc Med. 2005;159:225–30. doi: 10.1001/archpedi.159.3.225. [DOI] [PubMed] [Google Scholar]
- 26.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005:CD001871. doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA. 1996;275:768–76. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- 28.MacKelvie KJ, Khan KM, Petit MA, Janssen PA, McKay HA. A school-based exercise intervention elicits substantial bone health benefits: A 2-year randomized controlled trial in girls. Pediatrics. 2003;112:e447. doi: 10.1542/peds.112.6.e447. [DOI] [PubMed] [Google Scholar]
- 29.Lohman T, Thompson J, Going S, Himes JH, Caballero B, Norman J, et al. Indices of changes in adiposity in American Indian children. Prev Med. 2003;37:S91–6. doi: 10.1016/j.ypmed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Coleman KJ, Tiller CL, Sanchez J, Heath EM, Sy O, Milliken G, et al. Prevention of the epidemic increase in child risk of overweight in low-income schools: The El Paso coordinated approach to child health. Arch Pediatr Adolesc Med. 2005;159:217–24. doi: 10.1001/archpedi.159.3.217. [DOI] [PubMed] [Google Scholar]
- 31.Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, et al. TAAG Collaborative Research Group. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008;34:173–84. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guyatt GH, Sackett DL, Cook DJ. Users’ guides to the medical literature. II. How to use an article about therapy or prevention. B What were the results and will they help me in caring for my patients? Evidence-Based Medicine Working Group. JAMA. 1994;271:59–63. doi: 10.1001/jama.271.1.59. [DOI] [PubMed] [Google Scholar]
- 33.Wang LY, Gutin B, Barbeau P, Moore JB, Hanes J, Jr, Johnson MH, et al. Cost-effectiveness of a school-based obesity prevention program. J Sch Health. 2008;78:619–24. doi: 10.1111/j.1746-1561.2008.00357.x. [DOI] [PubMed] [Google Scholar]
- 34.Haerens L, Deforche B, Maes L, Cardon G, Stevens V, De Bourdeaudhuij I. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res. 2006;21:911–21. doi: 10.1093/her/cyl115. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds AJ, Temple JA, Ou SR, Robertson DL, Mersky JP, Topitzes JW, et al. Effects of a school-based, early childhood intervention on adult health and well-being: A 19-year follow-up of low-income families. Arch Pediatr Adolesc Med. 2007;161:730–9. doi: 10.1001/archpedi.161.8.730. [DOI] [PubMed] [Google Scholar]
- 36.McKenzie TL, Stone EJ, Feldman HA, Epping JN, Yang M, Strikmiller PK, et al. Effects of the CATCH physical education intervention: Teacher type and lesson location. Am J Prev Med. 2001;21:101–9. doi: 10.1016/s0749-3797(01)00335-x. [DOI] [PubMed] [Google Scholar]
- 37.Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes. 2007;31:1500–8. doi: 10.1038/sj.ijo.0803628. [DOI] [PubMed] [Google Scholar]
- 38.Carrel AL, Clark RR, Peterson SE, Nemeth BA, Sullivan J, Allen DB. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: A randomized, controlled study. Arch Pediatr Adolesc Med. 2005;159:963–8. doi: 10.1001/archpedi.159.10.963. [DOI] [PubMed] [Google Scholar]
- 39.Angelopoulos PD, Milionis HJ, Grammatikaki E, Moschonis G, Manios Y. Changes in BMI and blood pressure after a school based intervention: The CHILDREN study. Eur J Public Health. 2009;19:319–25. doi: 10.1093/eurpub/ckp004. [DOI] [PubMed] [Google Scholar]
- 40.Burke V, Milligan RA, Thompson C, Taggart AC, Dunbar DL, Spencer MJ, et al. A controlled trial of health promotion programs in 11-year-olds using physical activity “enrichment” for higher risk children. J Pediatr. 1998;132:840–8. doi: 10.1016/s0022-3476(98)70315-4. [DOI] [PubMed] [Google Scholar]
- 41.Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–802. doi: 10.1542/peds.2007-1365. [DOI] [PubMed] [Google Scholar]
- 42.Kain J, Leyton B, Cerda R, Vio F, Uauy R. Two-year controlled effectiveness trial of a school-based intervention to prevent obesity in Chilean children. Public Health Nutr. 2009;12:1451–61. doi: 10.1017/S136898000800428X. [DOI] [PubMed] [Google Scholar]
- 43.James J, Thomas P, Kerr D. Preventing childhood obesity: Two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS) BMJ. 2007;335:762. doi: 10.1136/bmj.39342.571806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: A 4-year randomized controlled intervention. Int J Obes. 2008;32:1489–98. doi: 10.1038/ijo.2008.99. [DOI] [PubMed] [Google Scholar]
- 45.Flores R. Dance for health: Improving fitness in African American and Hispanic adolescents. Public Health Rep. 1995;110:189–93. [PMC free article] [PubMed] [Google Scholar]
- 46.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 47.Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12:197–202. doi: 10.1017/S1368980008002644. [DOI] [PubMed] [Google Scholar]
- 48.Stone EJ, Baranowski T, Sallis JF, Cutler JA. Review of behavioral research for cardio-pulmonary health: Emphasis on youth, gender and ethnicity. J Health Educ. 1995;26:9–S17. [Google Scholar]
- 49.Waters E, de Silva-Sanigorski A, Burford BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children (Review) Cochrane Database Syst Rev. 2011:CD001871. doi: 10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]


