Abstract
Background:
In March 2013, cases of acute hepatitis were reported from Lalkuan, Nainital district. We investigated the outbreak to identify the source of infection and to facilitate control measures.
Objectives:
To study the distribution of hepatitis cases, to find the source of infection, and to initiate the control measures in the affected area.
Materials and Methods:
We defined a case of acute hepatitis as those cases that had jaundice with at least one of the following symptoms: Dark urine, fever, pain in abdomen, vomiting, and loss of appetite in the affected area between January and March 2013. Door-to-door survey was carried out. Thirteen blood samples were randomly collected from jaundice cases for immunoglobulin M (IgM) antibody for hepatitis A virus (HAV) and hepatitis E virus (HEV). Water samples were collected to test residual chlorine.
Results:
Total 2,785 individuals were surveyed; of which 240 were suffering from acute viral hepatitis (attack rate (AR) = 8.61%). Out of 13 serum samples, 10 were found positive for HEV IgM antibodies and three cases had IgM antibodies for both HAV and HEV, which confirmed a hepatitis E outbreak. The difference in attack rate of hepatitis of both the sexes was statistically significant (P < 0.001). The attack rate was significantly higher in age groups >12 years of age (P < 0.001). Environmental investigation also confirmed the sewage contamination of drinking water in the distribution system. The attack rate was much higher (29.4%) among those who were exposed to the leaking pipeline than the nonexposed (χ2 = 574.26, P < 0.01).
Conclusion:
HEV was confirmed as the major etiological agent in this outbreak that was transmitted by contaminated drinking water. The recognition of early warning signals, timely investigation, and application of specific control measures can contain the outbreak.
Keywords: Epidemiological investigation, environmental sanitation, infective hepatitis E, feco-oral route, serological examination
Introduction
Hepatitis E virus (HEV) is the agent largely responsible for epidemic as well as sporadic hepatitis in the developing countries.(1,2) The virus is transmitted by the feco-oral route, often through contaminated water. Acute viral hepatitis is a major public health issue in the developing nations that have inadequate sanitary conditions, inadequate safe drinking water, and sewage disposal problems.(2,3,4) Recognition of early warning signals, timely investigation and application of specific control measures can limit the spread of the outbreak and prevent deaths.
In March 2013, we received the information from medical officer in-charge, Lalkuan Primary Health Center (PHC), that several people were presenting to the hospital with acute hepatitis from ward no-5, of Lalkuan. An investigation team visited the affected area immediately because an epidemiological investigation was required in this situation to determine the existence of epidemic of jaundice if any, to identify the source, and to recommend and adopt control measures.
Materials and Methods
A criterion for diagnosis of acute hepatitis was defined as those cases that have/had jaundice with at least one of the following symptoms: Dark urine, fever, pain in abdomen, vomiting, and loss of appetite between January and March 2013. Intensive door-to-door survey was carried out. For all cases, information on personal details, time of onset, and source of drinking water were obtained. Randomly 13 sera from cases were collected for immunoglobulin M (IgM) antibodies for hepatitis A virus (HAV) and HEV by enzyme-linked immunosorbent assay (ELISA; DSI, Italy provided by IDSP, Uttarakhand).
Information regarding water quality, source of water supply, and drainage system were collected. Estimation of residual chlorine was performed at distribution level and from randomly collected consumer levels of the water distribution system. However, coliform count could not be performed due to logistic problem.
Results
Ward no-5 in Lalkuan has a population 2,785 as per PHC record. A total of 240 cases of jaundice (overall attack rate 8.62%) were reported in March 2013. There was an initial cluster in the last week of February 2013 followed by a peak in the 3rd week of March 2013 and then a gradual decline in the number of cases was observed. The epidemic curve showed no secondary peaks of incidence [Figure 1].
Figure 1.
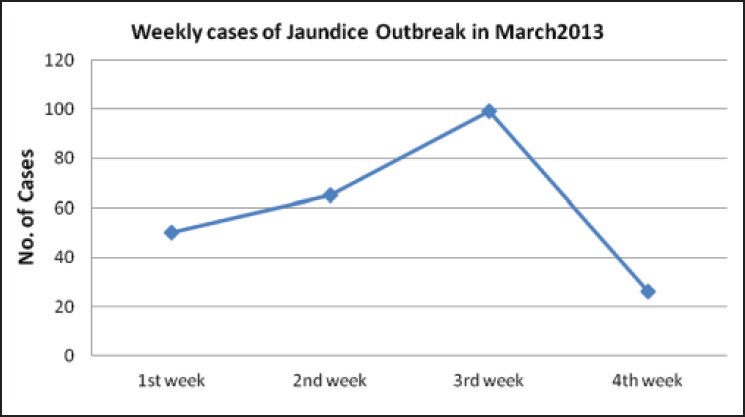
Epidemic curve of acute hepatitis cases in Lalkuana, Nainital District, 2013
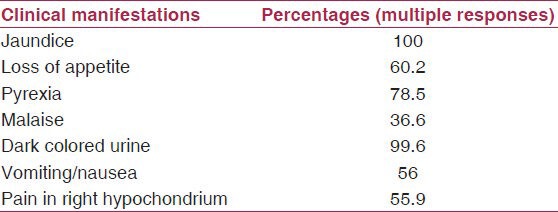
The signs and symptoms of the affected persons included jaundice (100%), loss of appetite (60.2%), pyrexia (78.5%), malaise (36.6%), high colored urine (99.6%), vomiting/nausea (56%), and pain in right hypochondria (55.9%) [Table 1].
Table 1.
Clinical profile in acute viral hepatitis cases (n = 240) in Lalkuan, Nainital
There were 135 males and 105 females affected. The attack rate in males was 10.21% and 7.18% for females and the difference was statistically significant (P < 0.001) [Table 2].
Table 2.
Age and sex wise distribution of cases of acute hepatitis in Lalkuan, Nainital
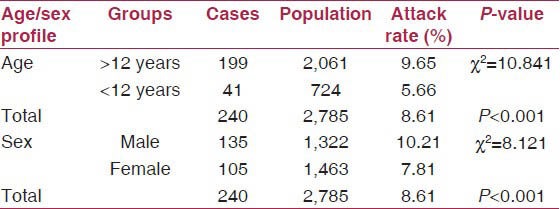
The disease affected all the age groups, but the attack rate was much more among the age group of >12 years (9.65%) and the difference was statistically significant (P < 0.001) [Table 2].
Out of the 13 sera collected, 10 were found positive for the hepatitis E IgM antibody and rest three were positive for both HEV and HAV IgM antibodies by ELISA (DSI, Italy).
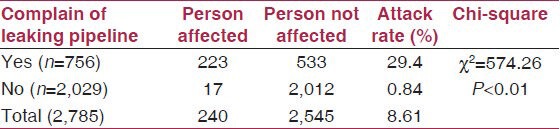
The higher attack rates of viral hepatitis was found in those, consuming water supplied from the leaking water pipelines passing adjacent to sewage pipeline, as compared to those who consumed water supplied from other pipelines indicating that the present outbreak was due to sewage contamination of drinking water supply. The difference in the attack rate was also found to be statistically significant (χ2 = 574.26, degrees of freedom (df) = 1, P < 0.01) [Table 3].
Table 3.
Attack rates in persons complaining of leaking water pipeline
Discussion
This study confirms the fact that there was an epidemic of infective hepatitis E in Lalkuan, Nainital District in March 2013. HEV causes a major public health issue in India. Similarly other studies reported HEV as the most important cause of all the clinical types of hepatitis commonly found in India.(5,6,7,8,9,10,11,12)
Out of the 13 sera collected, 10 were found positive for the hepatitis E IgM antibody and rest three were positive for both HEV and HAV IgM antibodies by ELISA (DSI, Italy). In other studies also hepatitis E was the major cause of the outbreak.(7,11,12)
Attack rate of acute viral hepatitis ranging from 1.9 to 17% have been reported from various studies from India.(8,9,10,11,12,13,14) The overall attack rate in the present study was 8.61%, comparable with the other studies.(9)
Similar to other studies in India,(15,16) we also found that all cases had jaundice, 78.5% had history of fever and 99.6% had dark colored urine.
The attack rate in males was 10.21% and 7.18% for females and the difference was statistically significant (P < 0.001), higher attack rates in males have also been reported in other studies from India.(11,17)
This study showed that population of >12 years showed significantly more number of cases as compared to <12 years of age [Table 2]. The age distribution of HEV cases in our study was similar to previously described studies.(7,8,9,12,15) In developing countries HEV is maintained as sporadic cases in the community and children acquire the infection in early life making them immune to another attack.(7)
This outbreak started in last week of February 2013, reached peaked in 3rd week of March 2013 and then started declining. No secondary peak was observed, similar finding were reported by varied studies.(6,10,15) Hepatitis E epidemics are frequently unimodal and short-lasting. Some have been multimodal, but even in such epidemics, new cases stopped appearing soon after water contamination was controlled.(18)
Hepatitis E outbreaks have been reported in urban areas whenever there is a break in the quality of water supplied including water chlorination.(6,7,8,9,10,11,17,19,20) In the present study out of 756 persons who gave the history of turbid water supply and leakage in water supply pipelines, 29.4% of them suffered from acute viral hepatitis. Whereas, rest 2,029 person who had not given the history of turbid water supply suffered less (0.84%) and this difference was statistically highly significant (χ2 = 574.26, P < 0.01). Hence, clear association was observed between turbid water supply and occurrence of cases of hepatitis in the present study. Residual chlorine was also found less in most of the water sample tested in various affected areas during the time of outbreak investigation.
The main source of water supply in Lalkuan area is tap water supplied by the Jal Sansthan for 1-2 h in the morning and 1 h in evening. Complains of turbid water supply were received from affected area. There was also a history of leakages in drinking water pipelines and overflowing drains in the area. Old dilapidated network in town, develop leakages. This result in entry of polluted water into the pipes when supply is closed.(21) We also confirmed the finding with the help of management staff at the Jal Sansthan in the affected areas. It was observed by the investigating team that many of the affected households had installed the electric motor system directly in the municipal water supply system as the pressure of the water was low during the supply hours.
As soon as the epidemic was noted, safe water supply was made available to the inhabitants through mobile Jal Sansthan water tanks and the local people were advised to boil the drinking water. Chlorine tablets were distributed to all houses in the affected areas. Simultaneously, extensive health education was provided. A meeting was held with the district magistrate in which the local elected representative, officials from Nagarpalika, Jal Sansthan, and health department participated. The appropriate authority (Nagarpalika, Jal Sansthan) were requested to repair the leaking water pipe line. Nagarpalika, Jal Sansthan took initiative to repair the leaking pipe. Due to active intervention like health education, provision for safe water by tanks and chlorination, the outbreak subsided.
Conclusions
Based on the above observations, it was concluded that, the present outbreak was due to fecal contamination of drinking water supplied to the affected areas, which occurred due to old and corroded leaking pipelines passing close to old leaking sewage lines.
The recognition of early warning signals, timely investigation, and application of specific control measures can contain the outbreak and decrease morbidity and mortality. Recommendations based on the outbreak investigation would also prevent future outbreaks.
Limitations
Water samples were not tested for the coliform count which could have further supported our findings in this study. Only 13 blood samples were tested for markers of hepatitis due to limited resources.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Khuroo MS, Duermeyer W, Zarger SA, Ahanger MA, Shah MA. Acute sporadic non-A, non-B in India. Am J Epidemiol. 1983;118:360–4. doi: 10.1093/oxfordjournals.aje.a113643. [DOI] [PubMed] [Google Scholar]
- 2.Sreenivasan MA, Banerjee K, Pandya PG, Kotak RR, Pandya PM, Desai NJ, et al. Epidemiological investigation of the outbreak of infectious hepatitis in Ahmedabad city during 1975- 1976. Indian J Med Res. 1978;67:197–206. [PubMed] [Google Scholar]
- 3.Singh S, Mohanty A, Joshi YK, Deka D, Mohanty S, Panda KS. Mother to child transmission of Hepatitis E virus. Indian J Pediatr. 2003;30:37–9. doi: 10.1007/BF02722743. [DOI] [PubMed] [Google Scholar]
- 4.Park K. 21th ed. Jabalpur: Bhanot Publisher; 2011. Park's text book of preventive and social medicine; p. 198. [Google Scholar]
- 5.Tandon BN, Gandhi MB, Joshi YK, Irshad M, Gupta H. Hepatitis virus-non-A and non B-the cause of a major public Health problem in India. Bull WHO. 1985;63:931–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Das P, Adhikary KK, Gupta PK. An Outbreak investigation of Viral Hepatitis E in South Dumdum Municipality of Kolkata. Indian J Community Med. 2007;32:84–5. [Google Scholar]
- 7.Sarguna P, Rao A, Sudha Ramana KN. Outbreak of acute viral hepatitis due to hepatitis E virus in Hyderabad. Indian J Med Microbiol. 2007;25:378–82. doi: 10.4103/0255-0857.37343. [DOI] [PubMed] [Google Scholar]
- 8.Chauhan NT, Prajapati P, Trivedi AV, Bhagyalaxmi A. Epidemic investigation of the jaundice outbreak in Girdharnagar, Ahmedabad, Gujarat, India, 2008. Indian J Community Med. 2010;35:294–7. doi: 10.4103/0970-0218.66864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vyas S, Parikh S, Kapoor R, Patel V, Solanki A. Investigation of an epidemic of hepatitis in Ahmedabad city. National J Community Med. 2010;1:27–9. [Google Scholar]
- 10.Singh PM, Handa SK, Banerjee A. Epidemiological Investigation of an Outbreak of Viral Hepatitis. MJAFI. 2006;62:332–4. doi: 10.1016/S0377-1237(06)80100-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raval DA, Chauhan NT, Katara RS, Mishra PP, Zankar DV. Outbreak of hepatitis E with bimodal peak in rural area of Bhavnagar, India, 2010. Ann Trop Med Public Health. 2012;5:190–4. [Google Scholar]
- 12.Martolia HC, Hutin Y, Ramachandran V, Manickam P, Murhekar M, Gupte M. An outbreak of hepatitis E tracked to a spring in the foothills of the Himalayas, India, 2005. Indian J Gastroenterol. 2009;28:99–101. doi: 10.1007/s12664-009-0036-x. [DOI] [PubMed] [Google Scholar]
- 13.Das DK, Biswas R, Pal D. An Epidemiological Investigation of Jaundice Outbreak in A Slum Area of Chetla, Kolkata. Ind J Pub Health. 2005;48:151–6. [PubMed] [Google Scholar]
- 14.Singh V, Raje M, Nain CK, Singh K. Routes of transmission in the hepatitis E epidemic of Saharanpur. Trop Gastroenterol. 1998;19:107–9. [PubMed] [Google Scholar]
- 15.Gurav YK, Kakade SV, Kakade RV, Kadam YR, Durgawale PM. A study of hepatitis E outbreak in rural area of Western Maharashtra. Indian J Community Med. 2007;32:1828–4. [Google Scholar]
- 16.Jain P, Prakash S, Gupta S, Singh KP, Shrivastava S, Singh DD, et al. Prevalence of hepatitis A virus, hepatitis B virus, hepatitis C virus, hepatitis D virus, and hepatitis E virus as a cause of acute viral hepatitis in North India: A hospital based study. Indian J Med Microbiol. 2013;31:261–5. doi: 10.4103/0255-0857.115631. [DOI] [PubMed] [Google Scholar]
- 17.Bhagyalaxmi A, Gadhvi M, Bhavsar BS. Epidemiological investigation of an outbreak of infectious hepatitis in Dakor town. Indian J Community Med. 2007;32:277–9. [Google Scholar]
- 18.Somani SK, Aggarwal R, Naik SR, Srivastava S, Naik S. A Serological Study of Intrafamilial Spread From Patients With Sporadic Hepatitis E Virus. Infection J Viral Hepat. 2003;10:446–9. doi: 10.1046/j.1365-2893.2003.00458.x. [DOI] [PubMed] [Google Scholar]
- 19.WHO, Hepatits E, WHO/CSR Web site. 2001. [Last accessed on 2013 Aug 9]. Available from: http://www.who.int/emc .
- 20.Banerji A, Sahni AK, Rajiva, Nagendra A, Saiprasad GS. Outbreak of viral hepatitis E in a regimental training. Med J Armed Forces India. 2005;61:326–9. doi: 10.1016/S0377-1237(05)80055-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rawat V, Jha SK, Bag A, Singhai M, Rawat CM. The Bacteriological Quality of Drinking Water in Haldwani Block of Nainital District, Uttarakhand, India. J Water Health. 2012;10:465–70. doi: 10.2166/wh.2012.035. [DOI] [PubMed] [Google Scholar]


