Abstract
Background:
There are limited primary data on the number of urban health care providers in private practice in developing countries like India. These data are needed to construct and test models that measure the efficacy of public stewardship of private sector health services.
Objective:
This study reports the number and characteristics of health resources in a 200 000 urban population in Pune.
Materials and Methods:
Data on health providers were collected by walking through the 15.46 sq km study area. Enumerated data were compared with existing data sources. Mapping was carried out using a Global Positioning System device. Metrics and characteristics of health resources were analyzed using ArcGIS 10.0 and Statistical Package for the Social Sciences, Version 16.0 software.
Results:
Private sector health facilities constituted the majority (424/426, 99.5%) of health care services. Official data sources were only 39% complete. Doctor to population ratios were 2.8 and 0.03 per 1000 persons respectively in the private and public sector, and the nurse to doctor ratio was 0.24 and 0.71, respectively. There was an uneven distribution of private sector health services across the area (2-118 clinics per square kilometre). Bed strength was forty-fold higher in the private sector.
Conclusions:
Mandatory registration of private sector health services needs to be implemented which will provide an opportunity for public health planners to utilize these health resources to achieve urban health goals.
Keywords: India, mixed health system, private sector services, regulation, urban health system
Introduction
Urban health systems of many developing countries including India are characterized by under-funded public services and large-scale proliferation of private sector health services. In most instances, the private sector services develop without appropriate regulation or stewardship from the public sector.(1,2) As such, the potential capability of such mixed public-private health systems in working cohesively to achieve national health goals remains underutilized.(3) In India, urban areas have a range of health services working with little or no coordination among them. Government run maternity hospitals and outpatient centers (referred to as urban health posts) provide free or subsidized health services. Publicly funded preschools (anganwadis), situated mostly within or near slums, offer health and education facilities to children aged 0-6 years and pregnant and lactating mothers. Privately owned health facilities deliver services on payment and range from clinics of general practitioners to large hospitals. Practitioners may belong to modern or traditional systems of medicine. A few health care facilities run by charitable organizations may also be present. Pharmacies assume importance due to their use by the community for a range of ailments. The magnitude and spectrum of these private sector services often remain unknown to public health services as the regulatory guidelines for registration with public health authorities have been voluntary in many developing countries, including India.(4) In India, as a first step toward regulation of this sector, the Clinical Establishments (Registration and Regulation) Act has been mandated.(5) This Act essentially aims at mandatory registration of all health facilities. The Act also mandates infrastructural standards for provision of health services by private sector practitioners. This Act has, however, not been implemented in most states across the country, due to dissent from within the private sector, arguing mainly against the mandatory infrastructural standards. Without a formal system to record the number of private sector health providers, there are considerable differences in official estimates and data obtained from large-scale surveys like the Census or the National Sample Survey Organization.(6,7,8)
There is, thus, a need to increase the comprehensiveness and reliability of the official data including maintenance of updated data on the health workforce. Although there are several commentaries on mixed health systems,(1,2,9) primary data measuring the actual number of providers within defined areas are few in number.(2,10) The lack of information is a constraint toward developing models by which the health benefits of public stewardship of private sector services can be measured.(11,12) As a first step toward testing a public-stewardship model, we report primary data on the health facilities and health workforce in a 200 000 population of Pune, India, which is the 8th largest city in India. We refer to the metrics of the health facilities and health workforce as the health resources since they have the potential to contribute toward improving population health.
Materials and Methods
Study setting
The Karve Road ward, area 15.46 sq km, population 210, 946 was randomly selected out of the 14 administrative wards of Pune city.(13) This ward is subdivided into nine electoral wards.
Data collection
Data collection was done by walking through the entire study area. As ward boundaries were not delineated on street maps, we first defined the ward boundaries by superimposing digital boundaries of the administrative and electoral wards from census data on satellite imagery using Google Earth 6.0.1.2032 software. This helped in identifying streets and other landmarks that delineated the boundaries of wards and defined our study area and study population. Using defined outlines, every street and building of the study area was visited and inquiries made on the availability of any health facilities. All health facilities were mapped using a Global Positioning System (GPS) device, Garmin GPSMAP 76CS×, and data analyzed using ArcGIS 10.0. Data on characteristics of health facilities (that is the physical location) and health workforce (individuals working at the facility in medical or paramedical activities) were collected using a structured format. Enumerated data were compared with existing data sources. The data were entered in Microsoft Excel 2007 and analyzed in Statistical Package for the Social Sciences (SPSS) version 16.0 software.
Categorization of health resources
Health facilities were categorized as (a) medical facilities which included hospitals (defined as any facility offering in-patient facilities), consultation clinics of individual doctors (private clinics), polyclinics (a unit of multiple consulting rooms used on fixed hour basis by different doctors), government health posts (outpatient facilities offering primary health services free or at a subsidized cost); (b) Paramedical facilities which included pharmacies and diagnostic laboratories; and (c) Allied health facilities which included the government anganwadis. Health workforce included doctors, nurses, and community health workers. Permission was obtained from the Medical Officer (Health) of the Pune Municipal Corporation and the relevant authorities were kept updated during the course of the study.
Results
Sources and completeness of information
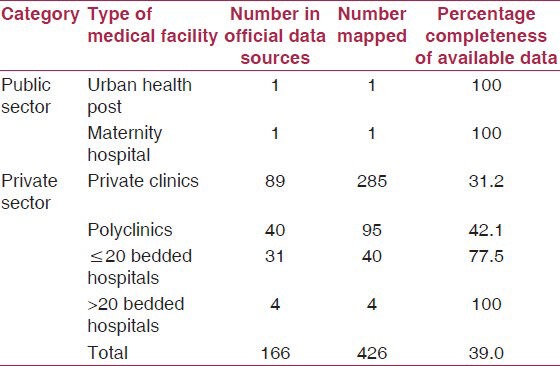
There is no single source for obtaining data on private health care providers in India. In Pune city, information on hospitals is available from the office of the Medical Officer (Health), while general practitioners and specialists have to register the clinic with the Office of the Shops and Establishments prior to initiating services. We obtained recent (2009) survey data from the Ward Medical Office and compared this data with those obtained through our field mapping exercise [Table 1]. The data were accurate for public sector facilities and hospitals with > 20 beds. There was a large discrepancy in the completeness of the data with respect to the number of private clinics (31.2% completeness), polyclinics (42.1% completeness), and small hospitals (77.5% completeness).
Table 1.
Completeness of available data
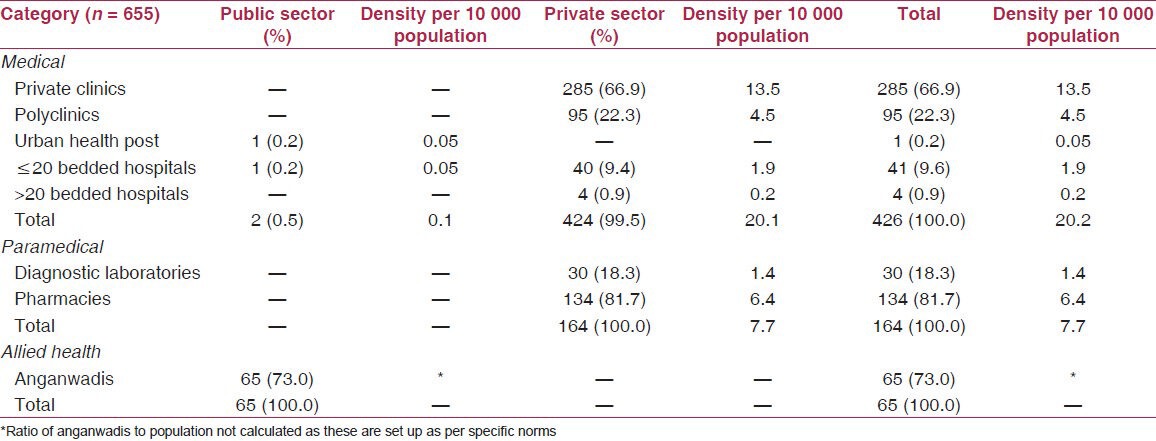
Types of health facilities
There were 655 medical, paramedical, and allied health institutions mapped in the 15.46 sq km study area [Figure 1]. Of these, 426 were medical facilities (424, 99.5% were private and two were government sector medical facilities); 164 were paramedical health facilities (134 pharmacies and 30 diagnostic laboratories); and 65 were allied health facilities (anganwadi centers). There was a higher density of private sector medical facilities (20.1 per 10 000 persons) as compared with public sector health facilities which was 0.1 per 10 000 persons). There were 1.4 diagnostic laboratories and 6.4 pharmacies per 10 000 population within the private sector [Table 2].
Figure 1.
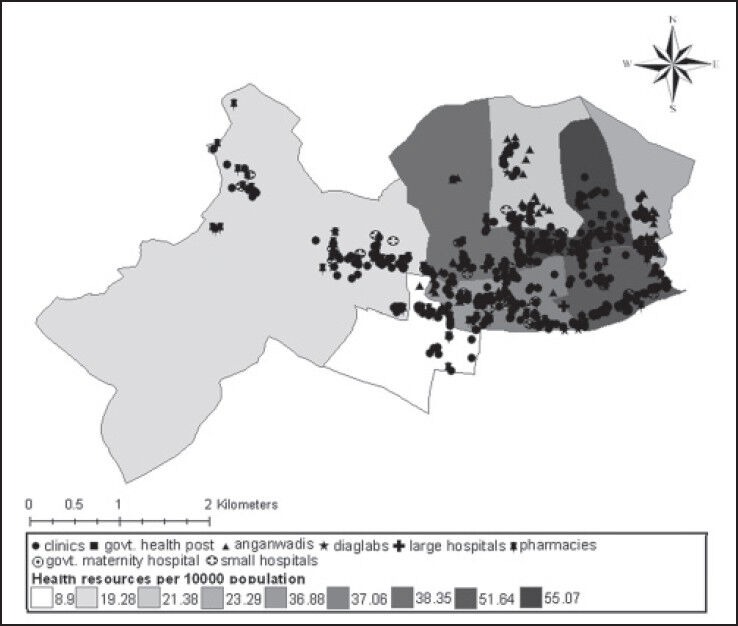
Distribution of health facilities and density per subward per 10 000 population
Table 2.
Medical, paramedical, and allied health institutions in the study area
Spatial distribution and density of health facilities
The spatial distribution of these health facilities varied between 55.1 per 10 000 population to 8.9 per 10 000 population [Figure 1]. Private sector health facilities, that is clinics, diagnostic laboratories, pharmacies, and hospitals were clustered along major roads, while government run anganwadis, clinics, and maternity hospitals were all situated within or near slums. Area-wise clustering of each type of health facility showed that the density of clinics ranged from 118 clinics per sq km to two clinics per sq km. The density of diagnostic laboratories ranged from 1 to 8 per sq km and the number of pharmacies ranged between 2 and 41 per sq km.
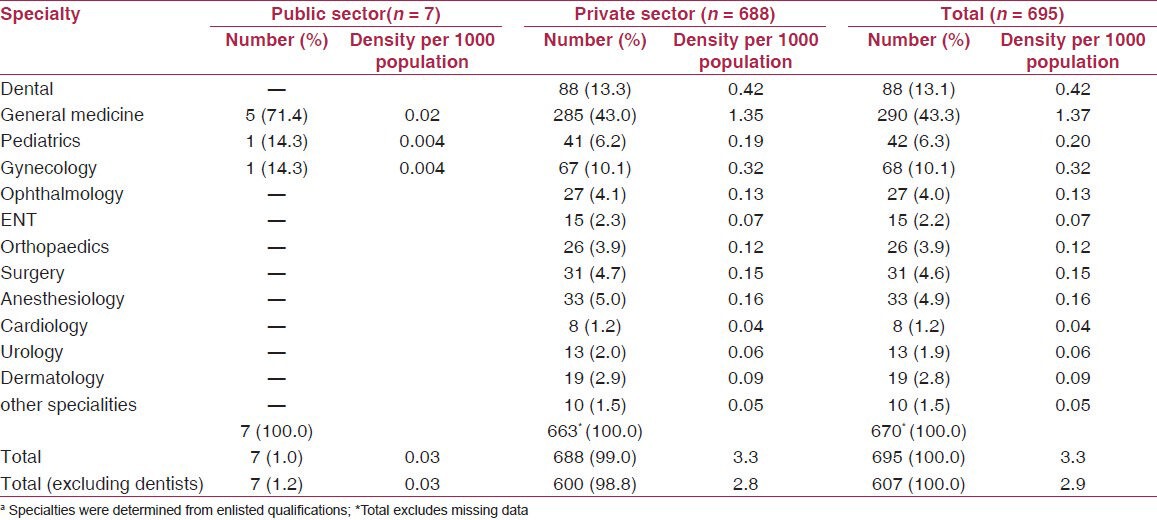
Types of human resources
There were 695 doctors practising in the entire study area giving a doctor to population ratio of 3.3 doctors per 1000 population. Of these, 7 (1%) doctors worked within government owned health facilities (0.03 doctors per 1000 persons) and the remaining 688 (99%) worked within the private health facilities (3.3 doctors per 1000 persons). The majority of the private sector doctors (43%) were general practitioners [Table 3]. Modern medicine was practised by a major proportion of the private doctors (320, 56.6%), while 28.0% (158) were trained in ayurveda and 15.4% (87) in homeopathy. In terms of specialty, dentists formed the largest group (88, 13.3%), followed by gynaecologists (67, 10.1%) and pediatricians (41, 6.2%). Excluding dentists the total physician to population ratio was 2.9 physicians per 1000 population. Paramedical staff included 169 trained nurses within the private sector (ratio of 0.8 nurses per 1000 persons) and 5 trained nurses within the public sector (ratio of 0.02 nurses per 1000 persons). The public sector, however, also had 130 community health workers. The nurse to doctor ratio in the private sector was 0.24, while that in the public sector was 0.71.
Table 3.
Characteristics of medical practitioners by specialtya
Bed to population ratio
A total of 399 (97.6%) beds were available within the private sector of which 290 were general medical beds, 77 beds were for maternity and gynaecological cases, and 26 beds were designated as paediatric beds. The public sector services had only 10 beds for maternity services (0.05 beds per 1000 persons). The private sector had 1.9 beds per 1000 persons.
Discussion
Mixed health systems, made up of public and private sector services, are a predominant characteristic of developing countries.(9) The paucity of health resources in the public sector in these countries is filled in by the private sector practitioners, who provide a range of speciality services that are not available within the public sector services. Several high-income countries have overcome mixed health system challenges through effective stewardship mechanisms.(2) However, lower-middle income countries like India are still far behind in utilizing the resources of the private sector for achieving public health goals. Lack of primary data to construct models for achieving an appropriate partnership for addressing public health issues has been noted to be an important constraint toward achieving this objective.(2,11,12)
Our study presents primary data on the availability of health services in an urban mixed health system. We have not attempted to address the level of utilization of the available health resources or the determinants of their spatial distribution in this study. Like many other developing countries, India lacks information on the number of doctors and health facilities in the private sector. There is no uniform regulation on compulsory registration of these practitioners although some states have initiated this activity.(5) The consequence of lack of enforced regulation for registration of medical services was reflected in this study, where official data were only 39% complete for private sector health facilities. The data revealed the strengths and weaknesses of public and private sector medical services and thereby the potential for collaborative provision of preventive and curative health services. For example, while public services were located close to slums and had a higher number of community-based workers and nurses, they lacked specialist services, were low in bed strength and in the number of doctors serving in the population. These weaknesses were compensated by the characteristics of the private sector which had a range of specialist services and a higher bed strength.
Our study also indicated the caveats in extrapolating urban health data. The density of services varied by geographical location within the 15.46 sq km study area. Although national estimates report 0.6 physicians per 1000 population,(14) the uneven distribution of private practitioners make comparisons difficult. For example, as compared with our data of 2.9 physicians per 1000 persons in Pune, a similar study done within the urban area of Ujjain district in Madhya Pradesh reported 1.19 physicians per 1000 population.(15) Thus, the projection of physician to population density from sample areas would be imprecise in India, suggesting the need for compulsory registration of private healthcare services as mandated under the Clinical Establishments (Registration and Regulation) Act.(5)
Our study is one of the few that report the metrics and the characteristics of mixed health systems in a selected urban area in India.(6,15,16) The baseline characterization reflects the complexity of urban health systems, which would be true for health systems of many other developing countries as well. India proposes to initiate a National Urban Health Mission for which baseline data will be necessary.(17) The primary data presented here are being used to test out models by which public stewardship of private sector services can be implemented. Several associated issues will be highlighted in the subsequent work. For example, nearly 50% of practitioners in our study area belonged to traditional systems of medicine. Methods to incorporate this vast resource to achieve the objectives of public health activities would have to be devised. The study reveals that doctor to population ratio of 2.9 obtained in our study was equal to or higher than developed countries such as Japan (2.06) and Great Britain (2.74).(14) Despite this, existing health indicators reinforce the fact that the mere presence of health manpower does not translate into a healthy population, reiterating the need for planned utilization of the health workforce in the country.
Conclusion
The unregulated proliferation of private sector health services limits its utilization by the public health system to achieve population health goals. Compulsory registration of private sector health facilities and workforce needs to be implemented in order that the information on these health resources is available with health administrators while implementing urban health plans.
Acknowledgment
We thank officers and staff of the health department of Pune Municipal Corporation for their cooperation and advice during this study. Funding support from the Department of Science and Technology, Government of India for an INSPIRE fellowship to KMF is gratefully acknowledged.
Footnotes
Source of Support: Kheya Melo Furtado has been funded through an INSPIRE fellowship from the Department of Science and Technology, Government of India
Conflict of Interest: None declared.
References
- 1.Lagomarsino G, de Ferranti D, Pablos-Mendez A, Nachuk S, Nishtar S, Wibulpolprasert S. Public stewardship of mixed health systems. Lancet. 2009;374:1577–8. doi: 10.1016/S0140-6736(09)61241-1. [DOI] [PubMed] [Google Scholar]
- 2.Lagomarsino G, Nachuk S, Kundra SS. Washington, DC: Results for Development Institute; 2009. [Last accessed on 2012 Mar 30]. Public stewardship of private providers in mixed health systems. Available from: http://www.rockefellerfoundation.org/uploads/files/f5563d85-c06b-4224-bbcd-b43d46854f83-public.pdf . [Google Scholar]
- 3.Hanson K, Gilson L, Goodman C, Mills A, Smith R, Feachem R, et al. Is private health care the answer to health problems of the world's poor? PLoS Med. 2008;5:e233. doi: 10.1371/journal.pmed.0050233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krickeberg K, Kar A, Chakraborty AK. Epidemiology in developing countries. In: Ahrens A, Pigeot I, editors. Handbook of Epidemiology. Berlin, Heidelberg, New York: Springer; 2005. pp. 1572–3. [Google Scholar]
- 5.The Clinical Establishments (Registration and Regulation) Act. 2010. [Last accessed on 2012 Jul 22]. Available from: http://www.mohfw.nic.in/WriteReadData/l892s/6867094504Clinical%20Establishment%20Act%202010%20(final).pdf .
- 6.Rao KD, Bhatnagar A, Berman P, Saran I, Raha S. India's Health Workforce: Size, Composition and Distribution. Human Resources for Health in India New Delhi. 2008. [Last accessed 2012 Mar 30]. Available from: http://www.hrhindia.org/assets/images/Paper-I.pdf .
- 7.Census of India 2001, Office of the Registrar General and Census Commissioner, Government of India. [Last accessed on 2012 Apr 10]. Available from: http://www.censusindia.gov.in/2011-common/censusdataonline.html .
- 8.New Delhi: 61st Survey Round on Employment and Unemployment in India. National Sample Survey Organization; National Sample Survey Organization 2004-05. [Google Scholar]
- 9.Nishtar S. The mixed health systems syndrome. Bull World Health Organ. 2010;88:74–5. doi: 10.2471/BLT.09.067868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Report of the National Commission of Macroeconomics and Health, Ministry of Health and Family Welfare, Government of India. 2005. [Last accessed on 2011 Nov 15]. Available from: http://www.who.int/macrohealth/action/Report%20of%20the%20National%20Commission.pdf .
- 11.Folsom A, Rao A, Lagomarsino G, Hecht R, de Ferranti D. Washington, DC: Results for Development Institute, Engelbert Centre for Health Care Reform, Brookings Institution; 2010. [Last accessed on 2012 Jul 27]. Improving Stewardship of Complex Mixed Health Systems: Learning from Health Care in the United States. Available from: http://www.resultsfordevelopment.org/sites/resultsfordevelopment.org/files/resources/Stewardship%20Issue%20Brief.pdf . [Google Scholar]
- 12.Tangcharoensathien V, Limwattananon S, Patcharanarumol W, Vasavid C, Prakongsai P, Pongutta S. Thailand: International Health Policy Program; 2008. [Last accessed on 2012 Jul 30]. Regulation of health service delivery in private sector: Challenges and opportunity. Available from: http://www.resultsfordevelopment.org/sites/resultsfordevelopment.org/files/resources/Regulation%20of%20Health%20Service%20Delivery%20in%20the%20Private%20Sector.pdf . [Google Scholar]
- 13.Census of India 2011, provisional figures Office of the Registrar General and Census Commissioner, Government of India. [Last accessed on 2012 Jan 15]. Available from: http://www.censusindia.gov.in .
- 14.World Health Organization Global Health Atlas. [Last accessed on 2011 Dec 5]. Available at: http://www.apps.who.int/globalatlas/dataQuery/default.asp .
- 15.De Costa A, Diwan V. ‘Where is the public health sector.’ Public and private sector healthcare provision in Madhya Pradesh, India? Health Policy. 2007;84:269–76. doi: 10.1016/j.healthpol.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Deshpande K, RaviShankar, Diwan V, Lönnroth K, Mahadik VK, Chandorkar RK. Spatial pattern of private health care provision in Ujjain, India: A provider survey processed and analysed with a Geographical Information System. Health Policy. 2004;68:211–22. doi: 10.1016/j.healthpol.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 17.Ministry of Health and Family Welfare, Government of India, June; 2010. [Last accessed on 2012 Apr 12]. National Urban Health Mission- Framework for Implementation draft. Available from: http://www.mohfw.nic.in/NRHM/Documents/Urban_Health/UH_Framework_Final.pdf . [Google Scholar]


