Abstract
Objective
To demonstrate that sudden sensorineural hearing loss is possibly of viral origin rather than vascular.
Study Design
The histopathologic morphology in 7 temporal bones with known vascular impairment due to surgical interventions was compared with that of 11 bones with a history of idiopathic sudden sensorineural hearing loss (ISSNHL). Attention was paid to the spiral ligament, stria vascularis, organ of Corti hair cells, tectorial membrane, ganglion cell population, and degree of perilymph fibrosis and the auditory nerve.
Setting
A temporal bone laboratory that has been in operation for more than 50 years and includes a database consisting of clinical and histopathological information that facilitates quantitative and qualitative analysis.
Subjects
Eight hundred forty-nine individuals who pledged their temporal bones for scientific study, of which 18 were selected for this study by means of the database criteria of sudden sensorineural hearing loss and postmiddle fossa and retro sigmoid sinus tumor removal or vestibular nerve section.
Results
Sudden sensorineural hearing loss bones exhibited no perilymph fibrosis compared with 6 of 7 vascular cases with fibrosis (P ≤ .001), exhibited less loss of ganglion cells (P ≤ .026), exhibited greater survival of spiral ligament (P ≤ .029), and averaged twice the survival of hair cells and more widespread tectorial membrane abnormalities.
Conclusion
Analysis of human temporal bones from patients with a sudden sensorineural hearing loss does not support a vascular insufficiency but is more suggestive of a viral etiology.
Keywords: sudden sensorineural, viral, vascular
Unilateral idiopathic sudden sensorineural hearing loss (ISSNHL) was ascribed to a spontaneous vascular phenomenon in more than 20 articles in the year from November 2011 to October 2012, based on a PubMed search, despite numerous articles in the past half century suggesting a viral etiology. Most of these articles reported “population-based cohort” studies that linked risk of ISSNHL with other diseases having or thought to have a vascular basis. As such, they were correlational rather than cause/effect studies. The cochlear histopathology in ISSNHL of a specific virus, measles, was described by Lindsay and Hemenway in 1954.1 They found degeneration of the stria vascularis, organ of Corti, and the tectorial membrane. Six years later, Lindsay et al2 reported similar findings in a case of mumps. Although there was no direct evidence of a viral etiology, Van Dichhoeck and Bierman reported an association of respiratory infections with sudden ISSNHL in 40 of 100 patients.3 Magnetic resonance imaging enhancement of the inner ear in cases of ISSNHL has been demonstrated by Seltzer and Mark4 and Stokroos et al,5 suggesting an active inflammatory process. These findings all give credence to the idea that ISSNHL is of viral origin. To further explore this issue, we compared temporal bone findings in patients with known vascular interruptions due to surgical procedures that spare the auditory nerve to the morphology in cases of ISSNHL.
Materials and Methods
The temporal bone laboratory of our institution contains 840 pairs of temporal bones with accompanying complete clinical records. This study is in compliance with regulations of the institutional review board of St. Vincent Medical Center #06-030, October 4, 2012. Most bones are from patients in our own pledge program, but a few are from the National Temporal Bone Registry From the database containing information on these bones, a total of 7 bones from 6 patients were found that had undergone middle fossa, suboccipital, or retrolabyrinthine surgery for the removal of vestibular nerve schwannomas or vestibular nerve lysis for the relief of the vertigo of Ménière’s disease. These approaches were used to preserve the patient’s serviceable hearing. In all cases, the auditory nerve was left intact. The postoperative hearing loss could be attributed only to an inadvertent interruption of the blood supply. These cases were designated the postoperative vascular group. A total of 11 cases in the database were identified with ISSNHL. The bones had been fixed with buffered formalin, decalcified with ethylenediaminotetraacedic acid until shown by xray to be free of calcium, embedded in celloidin, and cut into 20-μm sections on a sliding microtome. Every 10th section was stained with hematoxylin and eosin and mounted on glass slides and cover slipped. The percentages of normal spiral ligament, stria vascularis, hair cells, and peripheral processes were calculated by analyzing the 5 cochlear segments apparent in the midmodiolar and 2 paramodiolar sections plus the section containing the hook area of the basal segment. The ganglion cells were counted according to the method reported by Schuknecht.6 These data are entered into our database and were retrieved for this study. The 2 groups were compared statistically using appropriate nonparametric tests due to the small sample sizes. Fisher exact test (for a 2X2 table) was used for comparing categorical variables. The Mann-Whitney U test was performed for comparison of continuous/interval-level variables, even though all but 1 such variable (spiral ligament percent normal) met the criterion for homogeneity of variance. For one analysis, univariate analysis of variance (ANOVA) with covariance was performed to control for a possibly confounding factor. The criterion for statistical significance was set at P ≤ .05, 2-tailed for all analyses. Table 1 shows the characteristics of the patients in the 2 groups. The ISSNHL group tended to have more females, more left ears, an older age at death, and a longer duration of hearing loss than the postoperative vascular group. However, only duration of hearing loss achieved statistical significance (P<.037). There was no significant difference between groups in pure-tone average hearing threshold at last audiological test.
Table 1.
Characteristics of the patients from whom the temporal bones in each group were obtained.
| Postoperative Vascular (n = 7) | ISSNHL (n = 11) | Statistical Significance | |
|---|---|---|---|
| Sex, %, female/male | 71.4/28.6 | 81.8/18.2 | Fisher, NS |
| Ear, %, right/left | 71.4/28.6 | 36.4/63.6 | Fisher, NS |
| Age at death, y, mean (SD) | 63.4 (23.5) | 79.6(12.2) | M-W, NS (P = .070) |
| Duration of hearing loss, y, mean (SD) | 6.6 (10.7) | 19.9(17.2) | M-W, P = .037 |
| Pure-tone average of last test, dB: mean (SD) | 118.0 (37.7) | 95.8 (36.9) | M-W, NS |
Abbreviations: ISSNHL, idiopathic sudden sensorineural hearing loss: Fisher, Fisher exact test: M-W, Mann-Whitney U test.
Results
Table 2 summarizes the histopathological findings. Despite the small number of subjects, some of the differences between groups achieved statistical significance. The most outstanding differentiating finding between bones with a known vascular insufficiency and the ISSNHL bones was the presence of fibrosis in the hook area of the basal segment in 6 of 7 cases in contrast to no fibrosis in any of the bones with ISSNHL (P ≤ .001; Figure 1). Although few bones showed ossification in the cochlea, those that did were all in the postoperative vascular group. The tectorial membrane was more frequently affected in ISSNHL (Figure 2). Although this difference did not achieve statistical significance, the distribution of number of segments with abnormal tectorial membrane was interesting, with 4 of the 5 abnormal ISSNHL bones being abnormal in all 5 cochlear segments and 1 abnormal in 3 of the segments, while the 2 postoperative vascular bones with abnormal tectorial membrane had abnormalities in 1 and 2 segments each. Both the mean percentage remaining normal spiral ligament and the percentage of the bones with 100% normal spiral ligament differed significantly between the groups, with the ISSNHL group highly likely to have normal spiral ligament, compared with less than 50% normal in the postoperative vascular group (P ≤ .029 and P <.047, respectively). The stria vascularis and organ of Corti hair cell findings did not differ significantly between the groups, although the ISSNHL group tended to have twice the percentage remaining hair cells. Finally, there was a greater loss of ganglion cells in the postoperative vascular group, with only an average of 25.5% of normal ganglion cells present as compared with age-based norms, while the ISSNHL group had a mean percentage normal of 49.3% (P ≤ .035; Figures 3 and 4). An ANOVA with covariate was used to confirm that duration of hearing loss did not affect this difference between groups. When controlling for differences in the duration of hearing loss, the difference between groups in percentage remaining ganglion cells was still highly statistically significant (P ≤ .009).
Table 2.
Histopathology findings.
| Postoperative Vascular (n = 7) | ISSNHL (n = 11) | Statistical Significance | |
|---|---|---|---|
| Fibrosis, % of cases | 85.7 | 0.0 | Fisher, P ≤.001 |
| Ossification:, % of cases | 28.6 | 0.0 | Fisher, NS (P = .14) |
| Tectorial membrane normal, % of cases | 71.4 | 54.5 | M-W, NS |
| Spiral ligament, % normal, mean (SD) | 45.7(51.0) | 91.4 (28.6) | M-W, P≤.029 |
| Spiral ligament normal, % of cases | 42.9 | 90.9 | M-W, P≤.047 |
| Stria vascularis, % normal, mean (SD) | 35.7 (37.3) | 34.1 (25.7) | M-W, NS |
| Organ of Corti, % normal, mean (SD) | 23.6 (32.8) | 47.7 (34.7) | M-W, NS |
| Spiral ganglion cells, % normal, mean (SD)a | 25.5 (22.5) | 49.3 (20.7) | M-W, P≤.026 |
Abbreviations: ISSNHL, idiopathic sudden sensorineural hearing loss; Fisher, Fisher exact test M-W, Mann-Whitney U test.
Using age-normative correction.
Figure 1.
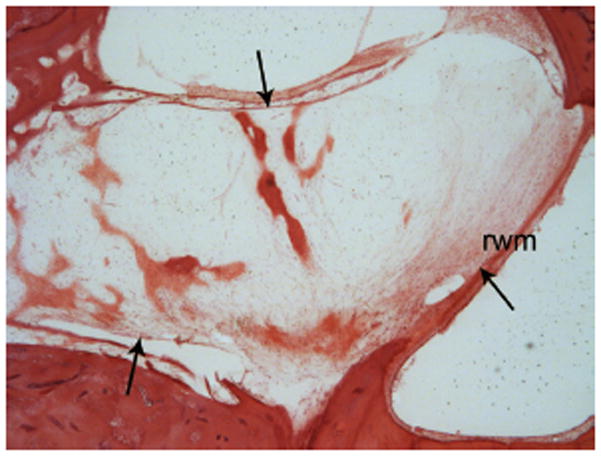
Fibrosis (arrows) with some neo-ossification spicules in the cochlear basal segment in a case of vascular insufficiency following a middle fossa vestibular nerve schwannoma removal. rwm indicates round window membrane. Hematoxylin and eosin 40X.
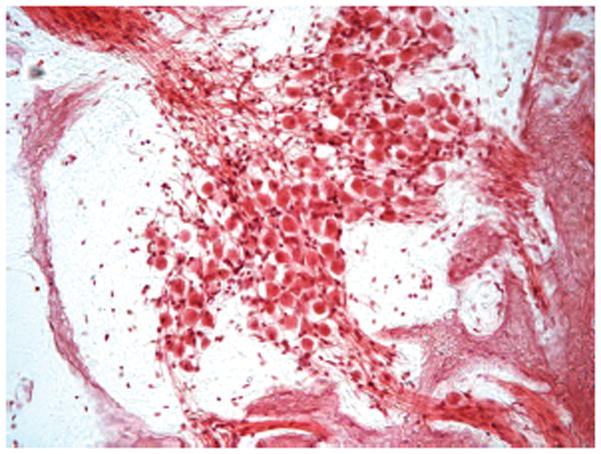
Figure 2.

Abnormal tectorial membrane (arrow) characteristic of idiopathic sudden sensorineural hearing loss. Hematoxylin and eosin 200X.
Figure 3.
Spiral ganglion in Rosenthal’s canal with a low normal number of neurons of 23,971 (normal for age 79 years, 26,200 ± 4491)7 in the case of idiopathic sudden sensorineural hearing loss. Hematoxylin and eosin 200X.
Figure 4.
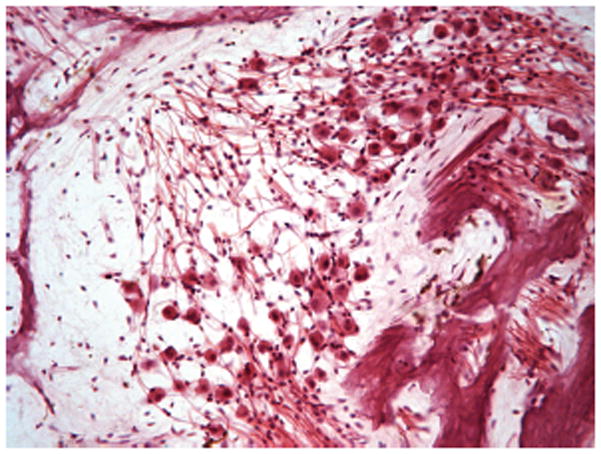
Rosenthal’s canal with a subnormal population of neurons of 12,789 (normal for age 72 years, 26,200 ± 4491)7 in a case of vascular insufficiency. Hematoxylin and eosin 200X.
Discussion
Vascular insufficiency may produce a SSNHL, but when it occurs, it is usually in conjunction with some known systemic pathological process such as leukemia or intracranial lesions such as vestibular nerve schwannomas or meningiomas or surgical interventions. Kimura and Perlman8 produced hearing loss in animals by obstructing the labyrinthine artery and producing fibrosis and finally ossification of the cochlear compartments, a condition we did not see in ISSNHL. Yoon et al9 reported on 11 cases of SSNHL and found that the two that were attributed to a vascular insult had evidence of fibrosis. One was associated with cerebral thrombosis and the other with an abnormally high platelet count. The presence of perilymph fibrosis and significant loss of neurons in the 7 cases of surgical intervention and their absence in the 11 cases of ISSNHL is convincing evidence that ISSNHL is not typically due to a vascular insult. Large health-related databases have become available in some countries, leading to a number of population-based studies in which the risk of ISSNHL has been linked to the risk of other comorbidities such as chronic renal disease, diabetes, myocardial infarction, hypertension, and erectile dysfunction. Based on these related risk findings, the assumption is made that the relationship is based on an underlying common pathophysiological mechanism of vascular damage or insufficiency. However, findings are not consistent from study to study within the various disease entities, and the study designs yield correlational (not cause/effect) interpretations. Rarely does this literature discuss the possibility that an unobserved third factor that is related to both ISSNHL and the other disease may be the basis for the correlational finding. One can certainly imagine at least one such factor that could be a link in some of the findings. A sudden hearing loss is likely to produce a strong stress reaction in an individual, both physiological and/or psychological. This could be a factor in the relationship of ISSNHL to erectile dysfunction and perhaps even myocardial infarction in someone with cardiovascular disease. Chronic renal disease can be caused by hypertension, and increased stress might play a role in increasing hypertension, thereby leading to correlations between ISSNHL (the producer of the stress) and both chronic renal disease and hypertension. It is not the purpose of this article to examine the exact pathophysiological mechanisms of all of these diseases but simply to point out that in correlational studies, there may be confounding factors that could also account for the statistical relationships found. The current histopathological findings contradict the theory that vascular disease or a vascular event is the etiological basis for sudden hearing loss and are much more suggestive of a viral etiology, as described by Lindsay et al1,2 in cases of known viral etiology (i.e., measles and mumps). Clinically, a widely accepted first-line treatment for ISSNHL is the use of steroids, orally or by intratympanic injection. This treatment presumes an underlying inflammatory process is playing a role in the reduction in hearing, somewhat in contradiction to the idea of a vascular etiology. Thus, it is important for clinical practice to try to determine the most common etiological basis for ISSNHL, keeping in mind that there may be multiple causes requiring different treatment approaches.
Acknowledgments
Funding source: National Institutes of Health grant U24
DC011962 and House Research Institute.
Footnotes
Disclosures
Competing interests: None.
Sponsorships: None.
Author Contributions: Fred H. Linthicum Jr, analyzed temporal bones, made images, and wrote rough draft; Joni Doherty, reviewed and edited draft, will present a paper at AAO/HNS; Karen I. Berliner, performed statistical analysis and edited article.
This article was presented at the 2013 AAO-HNSF Annual Meeting & OTO EXPO; September 29–October 3, 2013; Vancouver, BC, Canada.
References
- 1.Lindsay JR, Hemenway WG. Inner ear pathology due to measles. Ann Otol Rhinol Laryngol. 1954;63:754–771. doi: 10.1177/000348945406300310. [DOI] [PubMed] [Google Scholar]
- 2.Lindsay JR, Davey PR, Ward PH. Inner ear pathology in deafness due to mumps. Ann Otol Rhinol Laryngol. 1960;69:918–935. doi: 10.1177/000348946006900318. [DOI] [PubMed] [Google Scholar]
- 3.Van Dishoeck HAE, Bierman TA. Sudden perceptive deafness and viral infection: report of the first one hundred patients. Ann Otol Rhinol Laryngol. 1957;66:963–980. doi: 10.1177/000348945706600406. [DOI] [PubMed] [Google Scholar]
- 4.Seltzer S, Mark AS. Contrast enhancement of the labyrinth on MR scans in patients with sudden hearing loss and vertigo: evidence of labyrinthine disease. AJNR Am J Neuroradiol. 1991;12:13–16. [PMC free article] [PubMed] [Google Scholar]
- 5.Stokroos RJ, Albers FW, Krikke AP, Casselman JW. Magnetic resonance imaging of the inner ear in patients with idiopathic sudden sensorineural hearing loss. Eur Arch Otorhinolaryngol. 1998;255:433–436. doi: 10.1007/s004050050093. [DOI] [PubMed] [Google Scholar]
- 6.Schuknecht HF. Pathology of the Ear. 2. Philidelphia, PA: Lea & Febiger; 1993. [Google Scholar]
- 7.Makary CA, Shin J, Kujawa SG, Liberman MC, Merchant SN. Age-related primary cochlear neuronal degeneration in human temporal bones. J Assoc Res Otolaryngol. 2011;12:711. doi: 10.1007/s10162-011-0283-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perlman HB, Kimura R, Fernandez C. Experiments on temporary obstruction of the internal auditory artery. Laryngoscope. 1959;69:591–613. doi: 10.1288/00005537-195906000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Yoon TH, Paparella MM, Schachern PA, Alleva M. Histopathology of sudden hearing loss. Laryngoscope. 1990;100:707–715. doi: 10.1288/00005537-199007000-00006. [DOI] [PubMed] [Google Scholar]


