Abstract
AIM
To investigate radiological and clinical characteristics of pathologically proven cases of intrathymic cysts.
MATERIALS AND METHODS
The study population consisted of 18 patients (five males, 13 females; median age 56 years) with pathologically confirmed intrathymic cysts who underwent thymectomy and had preoperative chest computed tomography (CT) available for review. The patient demographics, clinical presentation, and preoperative radiological diagnoses were reviewed. CT images were evaluated for shape, contour, location of the cysts and the presence of adjacent thymic tissue, mass effect, calcifications, and septa. The size and CT attenuations of the cysts were measured.
RESULTS
The most common CT features of intrathymic cysts included oval shape (9/18; 50%), smooth contour (12/18; 67%), midline location (11/18; 61%), the absence of visible adjacent thymic tissue (12/18; 67%), and the absence of calcification (16/18; 89%). The mean longest diameter and the longest perpendicular diameter were 25 mm (range 17–49 mm) and 19 mm (range 10–44 mm), respectively. The mean CT attenuation was 38 HU (range 6–62 HU) on contrast-enhanced CT, and was 45 HU (range 26–64 HU) on unenhanced CT (p=0.41). The CT attenuation was >20 HU in 15 of 18 patients (83%). Preoperative radiological diagnosis included thymoma in 11 patients.
CONCLUSION
In surgically removed, pathologically proven cases of intrathymic cyst, the CT attenuation was >20 HU in most cases, leading to the preoperative diagnosis of thymoma. Awareness of the spectrum of imaging findings of the entity is essential to improve the diagnostic accuracy and patient management.
INTRODUCTION
With the increasing use of computed tomography (CT) for thoracic imaging, detection of incidental mediastinal masses is becoming very common. Due to its unique embryonic derivation, the thymus gives rise to a variety of benign and malignant pathological conditions, which can be noted as incidental mediastinal masses 1. For example, in a study of the 9263 individuals who underwent CT screening for lung cancer as part of the Early Lung Cancer Action Project (ELCAP), 71 had a mediastinal mass at baseline screening, of which 41 (58%) were of thymic origin 2.
Given that the multiple published guidelines recommend CT screening for lung cancer for high-risk individuals within the appropriate age range3, incidental mediastinal masses may present more frequent challenges to radiologists in clinical practice. Although multiple studies have evaluated the radiological manifestations of thymic neoplasms, such as thymomas and thymic carcinoma4,5, there are few studies focused on the radiological manifestations of benign entities of the thymus, such as cysts or hyperplasia 6–8. In particular, the imaging characteristics of intrathymic cysts have rarely been studied, except for being mentioned in comparison to thymic neoplasm, under the non-specific category of “benign thymic pathology” 5.
Thymic cysts represent 1–3% of all mediastinal masses 9, 10, and can be either congenital or acquired. Congenital thymic cysts are typically unilocular and contain clear fluid within a thin wall. Most are asymptomatic and found incidentally during the first two decades of life 11. In contrast, acquired thymic cysts (also known as multilocular thymic cysts) are usually multilocular and contain turbid fluid or gelatinous material as a result of haemorrhage or infection 12. Acquired thymic cysts are reported to be associated with radiation therapy for Hodgkin’s disease 13, 14, thymic tumour 15, thymic hyperplasia 16, thoracostomy or chest trauma, 17 and human immunodeficiency virus (HIV) infection18. Although less common than thymic neoplasms, thymic cysts are one of the most common benign thymic lesions 5. One of the challenges to the systematic radiological investigation of the entity is the lack of surgical and pathological confirmation for asymptomatic patients with imaging features strongly suggestive of simple cysts without suspicion for solid neoplasm. On the other hand, it is well known that some cases of intrathymic cysts have higher attenuation than simple fluid due to protein-rich contents, and are surgically removed due to the suspicion of neoplasm or malignancy based on imaging. A systematic investigation of the imaging features of pathologically proven cases of intrathymic cysts will contribute to the description of the imaging spectrum of this entity.
The purpose of the present study was to investigate the imaging characteristics of pathologically proven intrathymic cysts at CT, combined positron-emission tomography (PET)/CT, and magnetic resonance imaging (MRI).
MATERIALS AND METHODS
Patients
The original cohort was obtained from the retrospective review of the pathology patient database between 2001 and 2012, which resulted in 29 patients with pathological diagnosis of intrathymic cysts. Of these 29 patients, 11 patients had no preoperative chest CT available for review and were excluded from this study. Therefore, the patient population for the present study comprised 18 patients (five men, 13 women; age range 37–79 years; median 56 years; mean 55 years) with histopathologically confirmed intrathymic cysts who had undergone preoperative chest CT, which was available for review. CT was performed using the standard clinical chest CT protocol at the time of each scan over the 11 year period of this retrospective study. In general, patients were scanned in the supine position from the cranial to caudal direction from the clavicles to the adrenal gland, using multidetector row CT scanners with 4–64 detectors, with 120 kVp and 116–160 mAs or by utilizing dose modulation. For contrast-enhanced studies, 75–100 ml non-ionic iodinated contrast agent was injected intravenously. Axial images of 5 mm thickness were reconstructed and transferred to the picture archiving communication system (PACS) workstation (Centricity, GE Healthcare, Barrington, IL, USA). Of these 18 patients, MRI images of the chest were also available in three patients, and 2-[18F]-fluoro-2-deoxy-D-glucose (FDG) PET/CT images were also available in three patients. Institutional review board approval was obtained for this retrospective study.
Clinical characteristics and radiologic and pathological diagnoses
Medical records were reviewed for the patient demographics, clinical presentation, indication for surgery, and radiological and pathological diagnoses. Medical conditions associated with thymic diseases, including myasthenia gravis, thyroid disease, autoimmune diseases, history of cancer, and history of thoracotomy or chest trauma were also reviewed. Preoperative radiological diagnosis was obtained by reviewing the radiology reports. Pathology reports were reviewed by a board-certified anatomic pathologist (L.S.) to determine the pathological subcategories of intrathymic cysts, such as thymic cysts and bronchogenic cysts 5, 19. Thymic cysts were also subcategorized into multilocular or unilocular according to the histopathology reports.
Assessments of imaging characteristics
Two board-certified radiologists with expertise in thoracic imaging (M.N. and T.A.) reviewed the CT images of the intrathymic cysts in consensus for qualitative imaging characteristics including (1) shape (round, oval, or irregular); (2) contour (smooth or lobulated); (3) location (right, left, or midline); (4) the presence or absence of thymic tissue adjacent to the cyst; (5) mass effect to the adjacent structure; (6) calcifications; and (7) septa. All images were reviewed on the PACS using a mediastinal window setting (level, 50 HU; width, 350 HU). Quantitative measurements of the size and CT attenuation of the intrathymic cysts were performed by a board-certified radiologist (T.A.) using a calliper-type measurement tool on the PACS. The longest diameter of the lesion and the longest perpendicular diameter were obtained. CT attenuation values were measured by placing an oval region of interest (ROI) covering the maximum area of thymic lesions. In three patients with chest MRI, the signal intensity on T1- and T2-weighted images of the intrathymic cyst was evaluated in reference to the skeletal muscle (hyperintense, isointense, or hypointense) in consensus. The presence or absence of septa within the cyst was evaluated in the same manner. In three patients with PET/CT images, the patterns and intensity of uptake in terms of maximum standard uptake value (SUVmax) of the thymic lesions were measured by an experienced nuclear medicine imaging scientist (V.H.G.).
Statistical analysis
Descriptive statistics were provided for the qualitative and quantitative imaging features of the intrathymic cysts. The imaging features were compared among the histopathological subtypes of the intrathymic cysts (thymic cysts versus bronchogenic cysts) as well as between multilocular cysts and unilocular cysts at histopathology, using Fisher’s exact test for categorical data, and the Mann–Whitney U-test (Wilcoxon’s rank sum test) for continuous data. SPSS version 21 (IBM, Armonk, NY, USA) was used for all statistical analyses. All tests conducted were two-sided at the 0.05 significance level.
RESULTS
Patient demographics and clinical characteristics
Of the total of 18 patients, 13 (72%) were female and three (28%) were male, with a median age of 56 (range 37–79 years). Six patients had autoimmune disorders including Wegener’s granulomatosis and rheumatoid arthritis (n=1), Grave’s disease (n=1), primary biliary cirrhosis (n=1), polymayalgia rheumatica (n=1), temporal arteritis (n=1), and rheumatoid arthritis (n=1). Four patients had history of cancer including prostate cancer and anal mucosa-associated lymphoid tissue lymphoma (n=1), breast cancer (n=1), thyroid cancer (n=1), and lung cancer (n=1). Two patients had hypothyroidism, including one with temporal arteritis. None of the patients had myasthenia gravis, and history of thymectomy or chest trauma.
The details of clinical presentation were available in 17 patients, while no detail was available in one patient. The intrathymic cyst was noted as a mediastinal lesion on chest CT in 12 of the 17 patients (70%), including eight patients who underwent chest CT for assessment of other diseases or conditions (including aortic aneurysm, lung cancer, pulmonary embolism, bronchiectasis, asthma, trauma, “possible cyst in the back”, and “screening for wellness”), and five patients who underwent chest CT for symptoms including shortness of breath (n=1), dyspnoea (n=1), cough (n=1) and shoulder pain (n=1). In four patients (24%), the mediastinal lesion was found on neck CT performed for neck symptoms including dysphagia (n=2), neck pressure (n=1), and pulsatile neck mass (n=1). In one patient (6%), a chest radiograph performed for asthma revealed an abnormality in the anterior mediastinum, which was further studied by chest CT.
Imaging characteristics
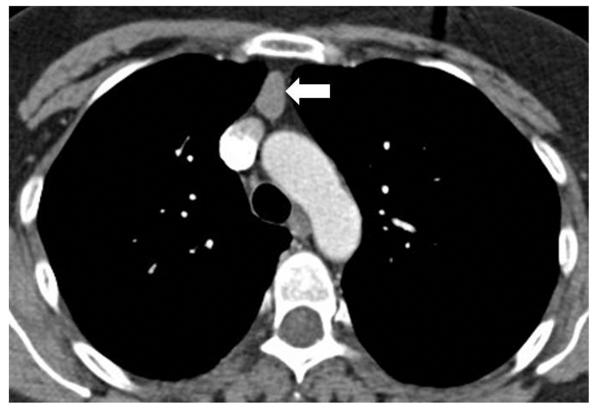
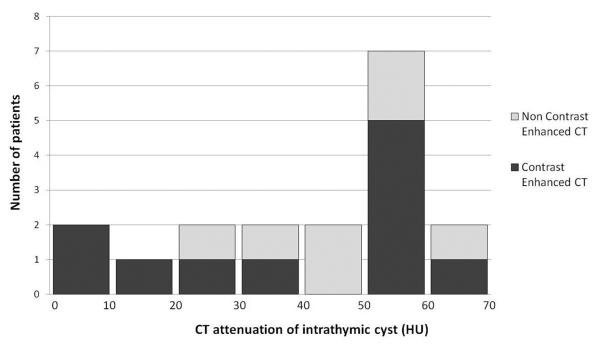
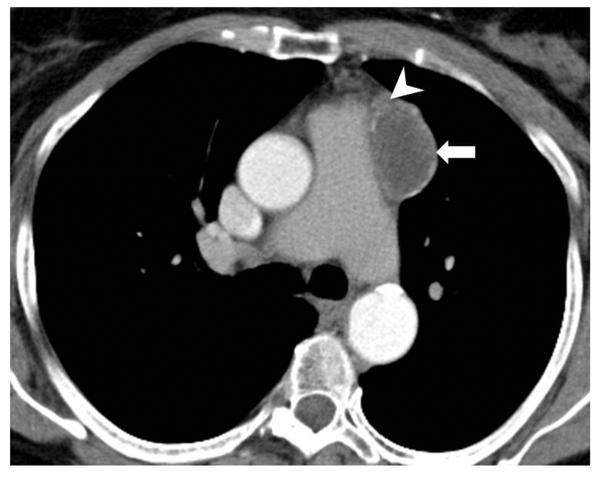
Qualitative CT characteristics of intrathymic cysts are summarized in Table 1. Intrathymic cysts were most commonly oval in shape (9/18; 50%), had smooth contours (12/18; 67%), were located at the midline (11/18; 61%), lacked visible adjacent thymic tissue (12/18; 67%), and had no calcification (16/18; 89%; Fig. 1). None of the 18 cases demonstrated mass effect or septa at CT. Quantitative measurements of intrathymic cysts on CT are summarized in Table 2. The mean longest diameter was 25 mm (range 17–49 mm), and the mean longest perpendicular diameter was 19 mm (10–44 mm). The mean CT attenuation of the cysts was 38 HU (range 6–62 HU) among the 11 patients with contrast-enhanced chest CT, and was 45 HU (range 26–64 HU) among the seven patients with unenhanced CT (p=0.41). In 15 out of 18 patients (83%), the CT attenuation was >20 HU, the threshold usually used to differentiate fluid from soft tissue (Figs. 2–4).
Table 1.
Qualitative features of intrathymic cyst at computed tomography
| Qualitative features | Total (n=18) |
|---|---|
| Shape | |
| Oval | 9 (50%) |
| Round | 5 (28%) |
| Triangular | 4 (22%) |
| Contour | |
| Smooth | 12 (67%) |
| Lobulated | 6 (33%) |
| Location | |
| Midline | 11 (61%) |
| Left | 5 (28%) |
| Right | 2 (11%) |
| Adjacent thymic tissue | |
| Absent | 12 (67%) |
| Present | 6 (33%) |
| Calcification | |
| Absent | 16 (89%) |
| Present | 2 (11%) |
Fig. 1.
A 47-year-old woman with Wegener’s granulomatosis underwent contrast-enhanced chest CT for evaluation of suspected pulmonary embolism. Axial CT image of the chest at the level of aortic arch demonstrated a well-circumscribed oval-shaped mass (arrow), located in the midline, measuring 55 HU. No visible septa or calcification was noted. Thymic neoplasm was suspected and thymectomy was performed. Histopathological diagnosis was intrathymic cyst.
Table 2.
Size and computed tomography (CT) attenuation of intrathymic cyst at CT in 18 patients
| Measurements | ||
|---|---|---|
| The longest diameter (mm) | Median [Q1, Q3] | 23 [20, 28] |
| Mean [SD] | 25 [8] | |
| The longest perpendicular diameter (mm) | Median [Q1, Q3] | 17 [15, 21] |
| Mean [SD] | 19 [8] | |
| CT attenuation (HU) | ||
| Contrast-enhanced CT (n=11) |
Median [Q1, Q3] | 51 [12, 55] |
| Mean [SD] | 38 [22] | |
| Unenhanced CT (n=7) | Median [Q1, Q3] | 40 [31, 58] |
| Mean [SD] | 45 [14] | |
Q1, Q3: the first and third quartiles, SD: standard deviation
Fig. 2.
A histogram represents the distribution of CT attenuation of intrathymic cysts in the cohort of 18 patients.
Fig. 4.
A 55 year-old woman with an incidentally noted mediastinal mass on neck CT performed for neck pressure. Contrast-enhanced CT image of the chest at the level of aortic arch demonstrated a round-shaped, well-circumscribed mass measuring 55 HU (arrow). Thymoma was suspected radiologically and surgical resection was performed. Histopathological diagnosis was intrathymic cyst.
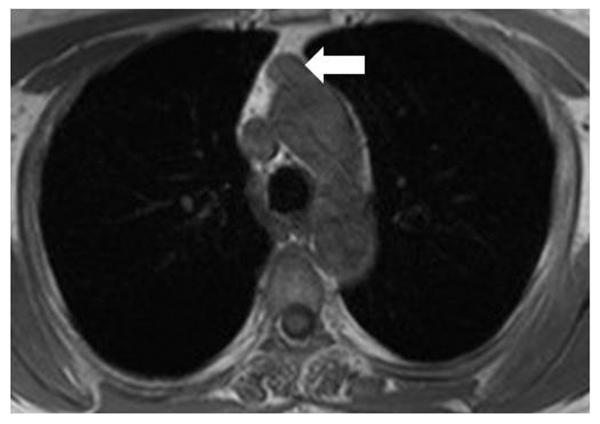
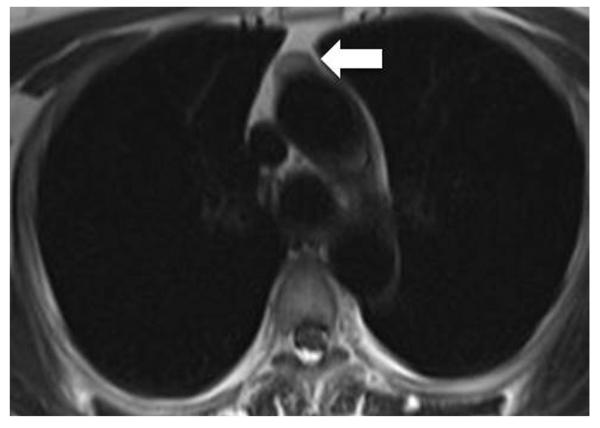
At MRI, intrathymic cysts were hyperintense to skeletal muscle on T2-weighted images in all three cases. The signal intensity on T1-weighted images was isointense to skeletal muscle in two cases, which were diagnosed as thymoma at MRI, and hypointense in one case, which was diagnosed as thymic cyst or foregut duplication cyst at MRI (Fig. 5). Septa were noted in none of the three cases, either on T1-weighted or T2-weighted images. Of the three cases with PET/CT, intrathymic cysts were not FDG avid in two cases (SUVmax of 1.01 and 0.84), whereas one case demonstrated FDG avidity in the area of cyst (SUVmax of 2.75) and was consistent with thymic hyperplasia on histopathology.
Fig. 5.
A 58-year-old woman with a history of hypothyroidism underwent MRI for a mediastinal lesion noted incidentally on a neck CT examination performed for dysphagia and throat pain. (a) An oval-shaped lesion abutting the aorta was noted (arrows), which was isointense on T1-weighted image [140 ms repetition time (TR)/2.46 ms echo time], and (b) slightly hyperintense to skeletal muscle on HASTE image (1000 ms TR/101 ms TE). Surgical resection was performed for definitive diagnosis and it was histopathologically confirmed to be intrathymic cyst.
Radiological and pathological diagnosis
Official radiology reports for the chest CT were available in 16 patients, whereas two patients underwent CT at other institutions and their reports were not available. Preoperative radiological diagnosis was thymoma in 10 patients, thymic/bronchogenic cyst in three, thymoma or thymic cyst in one patient, thymic mass or lymphoma or teratoma in one, and thymic hyperplasia in one. In the patient with a radiological diagnosis of thymic hyperplasia, the presence of hyperplasia was confirmed by histopathology along with the cyst.
After review of the histopathology reports, seven cases were subcategorized as thymic cysts, 11 cases were categorized as bronchogenic cysts. The distinction between thymic versus bronchogenic cysts was based on the presence of cilia; if the cyst was ciliated, it was considered to be bronchogenic cyst of foregut derivation, whereas if it had squamous or cuboidal epithelium lined without cilia, it was classified as a thymic cyst. Four cases were multilocular and 14 cases were unilocular based on the histopathology reports. There were no significant differences in qualitative or quantitative CT features between the histopathological subtypes of intrathymic cysts (thymic cysts versus bronchogenic cysts; p>0.14), or between multilocular and unilocular cysts (p>0.08).
DISCUSSION
The present study provided clinical, radiological, and histopathological characteristics of intrathymic cysts that were surgically removed and histopathologically confirmed. The majority (72%) of the patients was female, and one third had autoimmune diseases. The lesion was found incidentally during imaging studies for other purposes in all the patients with detailed history, and the preoperative radiological diagnosis was thymoma in more than half of the patients. The most common CT findings of intrathymic cyst included oval shape, smooth contour, and midline location, with mean diameters of 25×19 mm and mean CT attenuation of 38 HU on contrast-enhanced CT.
In terms of the demographics of patients with histopathologically proven intrathymic cysts, the median age was 56 years with a range of 37–79 years, which is similar to the previously reported age range of patients with thymic tumours including thymic epithelial tumours, thymic carcinoid, and lymphoma 4, 5, 20-22. In a recent study by McErlean et al.,5 it was suggested that indeterminate thymic lesions in patients <43 years tend more often to be benign. The present cohort included only four patients <43 years; thus, benign thymic cysts are not uncommon among an older adult population. The present cohort was female predominant, with 13 female and five male patients, including three females and one male with multilocular thymic cysts. There is no clear gender difference reported in the incidence of thymic cysts 23; however, multilocular thymic cysts have been reported to occur more often in male patients 12, 17, 24.
One-third of the patients in the present study population had autoimmune diseases. Although an association with medical conditions including autoimmune diseases are more commonly known in thymomas and thymic hyperplasia, there are several sporadic reports of thymic cysts associated with autoimmune diseases, including Grave’s disease, rheumatoid arthritis, Sjögren’s syndrome, and myasthenia gravis 25–30. Although myasthenia gravis is the most common condition associated with thymic disease, there was no patient with myasthenia gravis in the present cohort. The details and significance of medical conditions associated with intrathymic cysts remain to be investigated in larger cohorts.
In the majority of the patients in the present cohort, intrathymic cysts were noted on a chest or neck CT examination that was performed for other diseases or conditions, or for symptoms that were presumably unrelated to the cysts. The present results are consistent with the conventional knowledge that intrathymic cysts are found incidentally at chest radiography or CT 23. The results are also indicative of increased frequency of detection of these lesions with increasing use of chest CT, especially with wider implementation of CT screening for lung cancer. Although less frequent, cough, chest pain, and dyspnoea are reported as presenting symptoms, as noted in some of the present cases 12.
Oval shape, smooth contour, midline location without visible adjacent thymic tissue, calcification, mass effect, or septa were the most frequent qualitative imaging features of intrathymic cyst. In a recent report of 66 patients who underwent thymectomy for benign thymic lesions or early-stage malignant thymic neoplasms by McErlean et al.,5 28 benign thymic lesions were studied, including 10 benign thymic cysts. They concluded that intralesional fat, midline location, and triangular thymic shape are more frequently found in “benign thymic lesions”5. Although midline location was one of the most common findings of intrathymic cyst in the present cohort, accounting for 61% of the cases, triangular shape or intralesional fat was not seen in the present cohort, probably because these are the findings associated with other benign entities, such as thymic hyperplasia, thymolipoma, or benign thymus rather than cyst. Therefore, the distinction between intrathymic cyst versus thymic neoplasm, especially low-grade thymoma, can be difficult based on these CT features alone. Indeed, Choi et al.10 investigated CT features of idiopathic multilocular thymic cyst in eight patients and reported that multilocular thymic cysts typically appear as heterogeneous, unilocular, or multilocular cystic mass, often with a soft-tissue attenuation component, and well-defined wall sometimes with calcifications10. They concluded that CT was not helpful to distinguish neoplastic from non-neoplastic soft-tissue components 10.
The mean and median longest diameters of intrathymic cyst was 25 mm and 23 mm, respectively, and the mean and median longest perpendicular diameters were 19 mm and 17 mm; very similar to the measurement results of benign thymic lesions in a study by McErlean et al.,5 in which the longest perpendicular diameter (short axis) was significantly smaller in benign lesions than in malignant lesions. The longest diameter in the present study was much smaller compared to the mean diameter of 65 mm in eight patients with histologically proven multilocular thymic cysts reported by Choi et al.10, presumably because the present cohort included only four cases of multilocular cysts.
The CT attenuation of intrathymic cyst was >20 HU in 83% (15/18) of the patients in the present cohort, with a mean attenuation of 38 HU on contrast-enhanced CT and 45 HU on unenhanced CT. The CT attenuation is much higher than “water attenuation” or “fluid attenuation”, which are often used to describe characteristic features of thymic cyst,11 and is higher than the mean CT attenuation of 3 HU (ranging –20 to 17 HU) in three patients with multilocular thymic cysts in the study of Choi et al.10 Although the CT attenuation of thymic epithelial tumours and other thymic malignancy is not quantitatively evaluated in a systematic manner, the CT attenuation of intrathymic cysts in the present pathologically proven cohort is likely comparable to soft-tissue lesions. It is likely that the present cohort is biased towards patients who underwent thymectomy due to imaging findings suspicious for solid tumours than cysts. It should be stressed that this article describes the atypical features of intrathymic cysts because according to the present inclusion criteria, patients who underwent thymectomy had an initial diagnosis not typical for intrathymic cyst, rather suspicious for thymoma. However, it is important to be aware of this one end of the spectrum of imaging features of intrathymic cysts.
In the three cases with MRI studies, intrathymic cysts were hyperintense on T2-weighted images in all three cases. Two cases that were isointense on T1-weighted images were diagnosed as thymoma at MRI, and one case with T1 hypointense signal was diagnosed as thymic cyst. The MRI appearance of the three cases were consistent with the prior reports, where uncomplicated thymic cysts typically show iso-intensity signals to skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images18. An inhomogeneous signal intensity on T2-weighted image, which was not observed in the present three cases, is suggestive for thymoma rather than thymic cysts 31. In a systematic study by Tomiyama et al.32 investigating the diagnostic accuracy of CT and MRI in 127 patients with pathologically diagnosed anterior mediastinal tumours, 12 cases of thymic cyst were included along with 48 cases of thymoma, 12 cases of thymic carcinoma, 20 cases of mature teratoma, 13 cases of malignant germ cell tumour, and 22 cases of malignant lymphoma. CT was equal or superior to MRI in the diagnosis of all anterior mediastinal tumours except for thymic cyst; for thymic cyst, the percentage of correct diagnosis was 46% on CT and 71% on MRI32. Further studies are needed to increase the diagnostic accuracy of thymic cysts. In the limited number of cases with FDG-PET in the present study, intrathymic cysts were non-FDG avid unless associated with additional thymic disease (i.e., thymic hyperplasia in one of the present cases).
Given the overlapping features with solid tumours, especially with CT attenuation higher than the fluid attenuation in most cases, the preoperative radiological diagnosis was most commonly thymoma (63%), and only three cases had preoperative diagnosis of thymic or bronchogenic cyst. The results are somewhat expected because the cohort specifically focus on patients who underwent thymectomy, and the patients with imaging characteristics strongly suggestive of thymic cysts are unlikely undergo surgery if asymptomatic, and are likely observed conservatively. It is also known that CT attenuation in the cyst increases if haemorrhage or infection occurs as a complication and may be misdiagnosed as solid, mass-like thymoma 1, 11, 18. Nonetheless, it is important to note that some of the cases diagnosed as thymoma at CT were intrathymic cysts at histopathology. Thus, indicating the necessity to improve the diagnostic performance of imaging in differentiating these two entities, in order to avoid unnecessary surgical intervention as much as possible while capturing cases that benefit from surgical resection.
Histologically, seven cases were subcategorized as thymic cysts, and 11 cases were categorized as bronchogenic cysts, based on the presence of cilia along the epithelial lining of the cyst. The imaging findings were not significantly different between the two histopathological subgroups, which was expected given that the difference at histopathology is very subtle between the two subtypes. No differences were observed in imaging findings of unilocular versus multilocular cysts, probably due to the limited number of multilocular cysts in this cohort (n=4).
The limitations of the present study include its retrospective study design and a limited number of patients from a single institution. As the study focused on the cohort of patients with histopathologically proven intrathymic cysts after thymectomy, the study population is certainly skewed and represents one end of the spectrum of intrathymic cysts where the imaging findings were suspicious for solid tumour rather than cysts. The small number of cases with MRI or PET/CT is another limitation, which is also likely due to the skewed population with high suspicion of neoplasm therefore undergoing surgical resection. The low diagnostic accuracy of CT in discriminating thymic cyst from thymic neoplasm as demonstrated in the prior report,32 may have also affected the characteristics of the patients consisting of the surgically resected cohort. However, the study was designed to focus on the pathologically proven cases, as there has been no systematic report focusing on the imaging findings of histopathologically proven intrathymic cysts. Although the characteristic cases with fluid-attenuating simple cysts are often described in textbooks and prior literature, none of the studies have focused on the detailed qualitative and quantitative description of cases that were suggestive of solid tumours to the degree that thymectomy was indicated. In addition, detailed diagnostic accuracy of CT and MRI for various thymic diseases, including thymic cysts, thymomas, and thymic carcinomas, has already been described by Tomiyama et al. in the prior study involving 127 pathologically proven cases32. Therefore, the present study was not designed to assess the accuracy of the imaging for diagnosis of intrathymic cysts, but it rather focused on the detailed description of the surgically resected cases. The results of the present study should be interpreted in the context of the study design.
In conclusion, the clinical and radiological characteristics of pathologically proven cases of intrathymic cysts were described. The most frequent features of intrathymic cysts on CT were oval shape, smooth contour, and midline location. CT attenuation of the cysts was >20 HU in most of the cases of surgically resected intrathymic cysts, leading to the preoperative radiological diagnosis of thymoma. This study describes one end of the spectrum of imaging findings of intrathymic cysts, and indicates the need for further studies to improve diagnostic accuracy of thymic diseases.
Highlights.
The most frequent features of intrathymic cysts were oval shape, smooth contour located at midline
CT attenuation of the cysts was >20HU in most cases and were often diagnosed as thymoma on imaging
Awareness of the imaging spectrum of intrathymic cyst is essential for better diagnostic accuracy
Fig. 3.
A 79-year-old woman with a history of temporal arteritis and hypothyroidism underwent contrast-enhanced chest CT for evaluation of mediastinal mass incidentally noted on neck CT performed for pulsatile neck mass (which turned out to be a tortuous carotid artery). Axial CT image demonstrated a low-density anterior mediastinal mass (12 HU) abutting the pulmonary arterial trunk with partially calcified wall (arrow). Adjacent thymic tissue was visible on CT (arrowhead).
ACKNOWLEDGEMENTS
M.N. was supported by 1K23CA157631 (NCI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- guarantor of integrity of the entire study: Nishino, Hatabu
- study concepts and design: Nishino, Araki, Hatabu, Sholl, Gerbaudo
- literature research: Nishino, Araki
- clinical studies: Nishino, Araki, Hatabu, Sholl, Gerbaudo
- experimental studies / data analysis: Nishino, Araki, Hatabu
- statistical analysis: Nishino, Araki, Hatabu
- manuscript preparation: Nishino, Araki, Hatabu, Sholl, Gerbaudo
- manuscript editing: Nishino, Araki, Hatabu, Sholl, Gerbaudo
Items that do not apply should also be indicated with N/A. Where there is any uncertainty regarding authorship the editor of the study reserves the right to contact the guarantor of the study for further information.
REFERENCES
- 1.Nishino M, Ashiku SK, Kocher ON, Thurer RL, Boiselle PM, Hatabu H. The thymus: a comprehensive review. RadioGraphics. 2006;26:335–348. doi: 10.1148/rg.262045213. [DOI] [PubMed] [Google Scholar]
- 2.Henschke CI, Lee IJ, Wu N, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology. 2006;239:586–590. doi: 10.1148/radiol.2392050261. [DOI] [PubMed] [Google Scholar]
- 3.Wender R, Fontham ET, Barrera E, Jr., et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63:107–117. doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeong YJ, Lee KS, Kim J, Shim YM, Han J, Kwon OJ. Does CT of thymic epithelial tumors enable us to differentiate histologic subtypes and predict prognosis? AJR Am J Roentgenol. 2004;183:283–289. doi: 10.2214/ajr.183.2.1830283. [DOI] [PubMed] [Google Scholar]
- 5.McErlean A, Huang J, Zabor EC, Moskowitz CS, Ginsberg MS. Distinguishing benign thymic lesions from early-stage thymic malignancies on computed tomography. J Thorac Oncol. 2013;8:967–73. doi: 10.1097/JTO.0b013e3182904bc2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araki T, Sholl LM, Gerbaudo VH, Hatabu H, Nishino M. Imaging characteristics of pathologically proven thymic hyperplasia: identifying features that can differentiate true from lymphoid hyperplasia. AJR Am J Roentgenol. 2014;202:471–478. doi: 10.2214/AJR.13.11210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baron R, Lee J, Sagel S, Levitt R. Computed tomography of the abnormal thymus. Radiology. 1982;142:127–134. doi: 10.1148/radiology.142.1.7053522. [DOI] [PubMed] [Google Scholar]
- 8.Inaoka T, Takahashi K, Mineta M, et al. Thymic hyperplasia and thymus gland tumors: differentiation with chemical shift MR imaging. Radiology. 2007;243:869–876. doi: 10.1148/radiol.2433060797. [DOI] [PubMed] [Google Scholar]
- 9.Brown L, Muhm J, Sheedy P, 2nd, Unni KK, Bernatz PE, Hermann R., Jr The value of computed tomography in myasthenia gravis. AJR Am J Roentgenol. 1983;140:31–35. doi: 10.2214/ajr.140.1.31. [DOI] [PubMed] [Google Scholar]
- 10.Choi YW, McAdams HP, Jeon SC, et al. Idiopathic multilocular thymic cyst: CT features with clinical and histopathologic correlation. AJR Am J Roentgenol. 2001;177:881–885. doi: 10.2214/ajr.177.4.1770881. [DOI] [PubMed] [Google Scholar]
- 11.Jeung M-Y, Gasser B, Gangi A, et al. imaging of cystic masses of the mediastinum. RadioGraphics. 2002;22(Suppl. 1):S79–S93. doi: 10.1148/radiographics.22.suppl_1.g02oc09s79. [DOI] [PubMed] [Google Scholar]
- 12.Suster S, Rosai J. Multilocular thymic cyst: an acquired reactive process: study of 18 cases. Am J Surg Pathol. 1991;15:388–398. [PubMed] [Google Scholar]
- 13.Baron RL, Sagel SS, Baglan RJ. Thymic cysts following radiation therapy for Hodgkin disease. Radiology. 1981;141:593–7. doi: 10.1148/radiology.141.3.7302209. [DOI] [PubMed] [Google Scholar]
- 14.Lindfors K, Meyer J, Dedrick C, Hassell L, Harris N. Thymic cysts in mediastinal Hodgkin disease. Radiology. 1985;156:37–41. doi: 10.1148/radiology.156.1.4001419. [DOI] [PubMed] [Google Scholar]
- 15.Nakamura S, Tateyama H, Taniguchi T, et al. Multilocular thymic cyst associated with thymoma: a clinicopathologic study of 20 cases with an emphasis on the pathogenesis of cyst formation. Am J Surg Pathol. 2012;36:1857–1864. doi: 10.1097/PAS.0b013e31826320c4. [DOI] [PubMed] [Google Scholar]
- 16.Izumi H, Nobukawa B, Takahashi K, et al. Multilocular thymic cyst associated with follicular hyperplasia: clinicopathologic study of 4 resected cases. Hum Pathol. 2005;36:841–844. doi: 10.1016/j.humpath.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Jaramillo D, Perez-Atayde A, Griscom N. Apparent association between thymic cysts and prior thoracotomy. Radiology. 1989;172:207–209. doi: 10.1148/radiology.172.1.2740504. [DOI] [PubMed] [Google Scholar]
- 18.Avila NA, Mueller BU, Carrasquillo JA, Kontny HU, Jaffe ES, Pizzo PA. Multilocular thymic cysts: imaging features in children with human immunodeficiency virus infection. Radiology. 1996;201:130–134. doi: 10.1148/radiology.201.1.8816533. [DOI] [PubMed] [Google Scholar]
- 19.Bogot NR, Quint LE. Imaging of thymic disorders. Cancer Imaging. 2005;5:139. doi: 10.1102/1470-7330.2005.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Jong WK, Blaauwgeers JL, Schaapveld M, Timens W, Klinkenberg TJ, Groen HJ. Thymic epithelial tumours: a population-based study of the incidence, diagnostic procedures and therapy. Eur J Cancer. 2008;44:123–130. doi: 10.1016/j.ejca.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer. 2003;105:546–551. doi: 10.1002/ijc.11099. [DOI] [PubMed] [Google Scholar]
- 22.Sadohara J, Fujimoto K, Müller NL, et al. Thymic epithelial tumors: comparison of CT and MR imaging findings of low-risk thymomas, high-risk thymomas, and thymic carcinomas. Eur J Radiol. 2006;60:70–79. doi: 10.1016/j.ejrad.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Shimosato Y, Mukai K. Tumors of the mediastinum: atlas of tumor pathology. Vol. 21. Armed Forces Institute of Pathology; Washington, DC: 1997. pp. 158–168. (3rd series). [Google Scholar]
- 24.Strollo DC. Rosado-de-Christenson ML. Tumors of the thymus. J Thorac Imaging. 1999;14:152–171. doi: 10.1097/00005382-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Peacey SR, Belchetz PE. Graves’ disease: associated ocular myasthenia gravis and a thymic cyst. J Roy Soc Med. 1993;86:297–298. doi: 10.1177/014107689308600520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matsumoto S, Mori Y, Takiya H, Iwata H, Shirahashi K. Multilocular thymic cyst associated with rheumatoid arthritis [in Japanese] Kyobu Geka. 2012;65:205–8. [PubMed] [Google Scholar]
- 27.Kondo K, Miyoshi T, Sakiyama S, Shimosato Y, Monden Y. Multilocular thymic cyst associated with Sjogren’s syndrome. Ann Thorac Surg. 2001;72:1367–1369. doi: 10.1016/s0003-4975(00)02706-5. [DOI] [PubMed] [Google Scholar]
- 28.Yamamura H, Mase T, Shioi K, et al. A case of thymic cyst and thymoma with myasthenia gravis [in Japanese] Kyobu Geka. 1997;50:975–977. [PubMed] [Google Scholar]
- 29.Okumura S, Ohta T, Fujioka M, Nakabayashi H. A case of multilocular thymic cyst with myasthenia gravis [in Japanese] Nihon Kyobu Geka Gakkai. 1995;43:917–921. [PubMed] [Google Scholar]
- 30.Mishra AK, Agarwal SK, Pradhan S, Agarwal A. Association of unilocular thymic cyst and myasthenia gravis. Neurol India. 2012;60:103–105. doi: 10.4103/0028-3886.93599. [DOI] [PubMed] [Google Scholar]
- 31.Sakai F, Sone S, Kiyono K, et al. MR imaging of thymoma: radiologic–pathologic correlation. AJR Am J Roentgenol. 1992;158:751–756. doi: 10.2214/ajr.158.4.1546586. [DOI] [PubMed] [Google Scholar]
- 32.Tomiyama N, Honda O, Tsubamoto M, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol. 2009;69:280–288. doi: 10.1016/j.ejrad.2007.10.002. [DOI] [PubMed] [Google Scholar]