Abstract
Liposome-encapsulated ciprofloxacin for inhalation (CFI) was investigated as a putative postexposure therapeutic for two strains of Francisella tularensis. The efficacies of oral ciprofloxacin and intranasally instilled CFI could not be distinguished in a mouse model of infection with the F. tularensis live vaccine strain (LVS), where a single dose of either formulation offered full protection against a lethal challenge. However, mouse studies with the more virulent Schu S4 strain of F. tularensis demonstrated that a higher level of protection against a lethal aerosol infection is provided by CFI than by oral ciprofloxacin. In addition, using this infection model, it was possible to discriminate the efficacy of intranasally instilled CFI from that of aerosolized CFI, with aerosolized CFI providing full protection after just a single dose. The improved efficacy of CFI compared to oral ciprofloxacin is likely due to the high sustained concentrations of ciprofloxacin in the lung. In summary, CFI may be a promising therapy, perhaps enabling the prophylactic regimen to be shortened, for use in the event of a deliberate release of F. tularensis. The prophylactic efficacy of CFI against other biological warfare (BW) threat agents also warrants investigation.
INTRODUCTION
Francisella tularensis is an intracellular pathogen and the causative agent of tularemia, a debilitating and sometimes fatal disease in humans. Inhalation of F. tularensis can result in the most severe form of the disease, respiratory tularemia, which produces pneumonic plague-like symptoms in sufferers. Only low doses of F. tularensis are required for infection through this route, and without antibiotic treatment, a fatality rate of up to 30% has been observed (1). These properties led to the development of F. tularensis as a biological warfare (BW) agent by Russia, Japan, and the United States (1). The low infectious dose by the aerosol route, severe infection following inhalation, and historical interest in F. tularensis as an offensive BW agent have led to the classification of F. tularensis by the U.S. Centers for Disease Control and Prevention as a category A agent of concern (2).
Currently, no licensed vaccine is available for tularemia. However, historically the F. tularensis LVS strain has been used, and it is still recommended in some countries for laboratory personnel (1), demonstrating the potential of vaccination. Antibiotic treatment is generally effective, reducing mortality to approximately 2% (1). However, several orally administered antibiotics are unsuitable for treating tularemia, including β-lactams and macrolides (1). Aminoglycosides, specifically streptomycin, are traditionally the treatment of choice but need to be injected. Streptomycin treatment is now usually avoided due to limited availability, and gentamicin treatment is now recommended by Public Health England (http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1194947357555). Nevertheless, in the event of a deliberate release of F. tularensis, postexposure prophylaxis with aminoglycosides may not be practical, as, in addition to the need for parenteral dosing, monitoring of serum levels (to prevent toxicity) is required. Currently, the recommended F. tularensis prophylaxis is orally delivered ciprofloxacin or doxycycline for 14 days (1). However, in a murine model of pneumonic F. tularensis Schu S4 infection, 14 days of oral ciprofloxacin therapy resulted in all treated mice succumbing to the infection after the treatment regimen had finished (3). In addition, relapse has been reported in humans treated with ciprofloxacin or doxycycline (4). During an outbreak of tularemia in Spain, 6 of the 14 patients treated with doxycycline relapsed (5). An additional 22 individuals were treated with ciprofloxacin, and only 1 of these relapsed, suggesting that ciprofloxacin treatment results in a lower relapse rate (5). However, in a separate study, also carried out during this outbreak in Spain, 7 of 14 patients treated with ciprofloxacin relapsed (6).
The ability of F. tularensis to infect mononuclear phagocytes, escape the phagosome, and replicate in the cytosol is crucial for the pathogenicity of tularemia (2). Inside mononuclear phagocytes, F. tularensis is protected from the many humoral and cellular immune responses that target extracellular bacteria. In addition, this intracellular location also appears to protect the bacteria from antibiotic treatment (7). Thus, encapsulation of ciprofloxacin in liposomes has been suggested as a method to improve treatment outcomes for tularemia (8–11). As liposomes are phagocytosed by macrophages, encapsulation enables antibiotics to be delivered to the intracellular site of infection (12). In addition, encapsulation enables slow release of antibiotics into the blood and reduces excretion of the drugs, prolonging their half-lives (t1/2) (13).
A liposome-encapsulated ciprofloxacin formulation, “ciprofloxacin for inhalation” (CFI), has completed multiple phase 2 clinical trials for Pseudomonas aeruginosa infection in cystic fibrosis and non-cystic fibrosis bronchiectasis patients (14–16). Using this advanced development product, we have built upon previous data demonstrating the efficacy of liposomal ciprofloxacin against the highly virulent F. tularensis Schu S4 (8–11).
MATERIALS AND METHODS
Bacteria.
Francisella tularensis LVS (NDBR lot 4) was cultured on blood cysteine glucose (BCG) agar or in modified cysteine partial hydrolysate (MCPH) broth (17). For the mouse challenges, F. tularensis LVS was prepared by harvesting from agar plates into phosphate-buffered saline (PBS) to obtain an optical density at 600 nm (OD600) of 0.17, equating to approximately 1 × 109 CFU/ml. F. tularensis Schu S4 was prepared for the animal challenge by growing in MCPH broth with shaking at 37°C for 48 h. The OD600 of the culture was adjusted to 0.1, which equates to approximately 1 × 109 CFU/ml. Bacterial numbers were determined by enumeration of serially diluted bacteria on agar plates. All experiments with F. tularensis Schu S4 were carried out in a class III microbiological safety cabinet complying with British standard 5726.
Animals.
Female BALB/c mice (6 to 8 weeks old) were obtained from Charles River Laboratories (United Kingdom). For the experiments using F. tularensis LVS, mice were caged in groups of 5 in a flexible-film isolator and allowed to acclimatize for 6 days before challenge. For experiments using F. tularensis Schu S4, mice were caged in groups of 4 in an ACDP (United Kingdom) level 3 rigid-wall isolator, complying with British standard 5726, and allowed to acclimatize for 5 days before challenge. All experiments with mice were carried out in accordance with the United Kingdom Animal (Scientific Procedures) Act (1986).
Antibiotics.
Ciprofloxacin (Fluka, Buchs, Switzerland) and liposomal ciprofloxacin (CFI) (Aradigm, Hayward, CA, USA) were used in these experiments. CFI (ARD-3100, Lipoquin) is an aqueous colloidal dispersion containing ciprofloxacin encapsulated in unilamellar liposomes. It is manufactured at a 50-mg/ml concentration (expressed in terms of mg/ml ciprofloxacin hydrochloride, with the corresponding ciprofloxacin base concentration being 45 mg/ml). The average particle size of the ciprofloxacin-loaded liposomes is 75 to 120 nm. More than 99% of the drug is typically encapsulated inside the liposome formulation.
Antibiotic efficacy in BALB/c mice.
Groups of 5 mice were challenged via the intranasal route by pipette, under halothane anesthesia, with approximately 6 × 104 CFU of F. tularensis LVS in 40 μl. Treatment was initiated at 72 or 96 h postchallenge. A single dose of 50 mg/kg ciprofloxacin was administered orally via a pipette. This dose was selected to enable comparisons with previous studies (8–11). Similarly, a single dose of 50 mg/kg CFI was administered via the intranasal route with a pipette to mice under halothane anesthesia. Mice were observed for 3 weeks postchallenge; animals were weighed daily, and clinical signs were scored twice daily. Clinical scores were determined by the extent of piloerection, hunching, eye problems, and locomotion, with scores of 0, 1, and 2 specified for each category.
The F. tularensis Schu S4 aerosol was generated using a Collison nebulizer, containing 20 ml of F. tularensis Schu S4 at a concentration of approximately 4.2 × 106 CFU/ml, and conditioned using a modified Henderson apparatus (18). Mice were exposed to the aerosol for 10 min via a head-only exposure chamber, with aerosol sampling of the aerosol chamber performed using an all-glass impinger (AGI-30; Ace Glass, NJ) containing PBS. The enumeration of F. tularensis concentration in the aerosol together with a calculation (19) using Guyton's formula (20) determined that each mouse was exposed to approximately 10 CFU. Therapy with oral ciprofloxacin (50 mg/kg either once or twice daily), intranasal CFI (50 mg/kg once daily), or aerosolized CFI (1 mg/kg lung dose delivered once daily) was initiated in groups of 12 mice at 24 h postchallenge; groups received either a single dose of antibiotic or 3 days or 5 days of therapy. The aerosolized CFI lung dose was determined from the concentration of ciprofloxacin in the lung at 1 min postadministration. The CFI aerosol was generated by using a Pari LC Star Sprint nebulizer powered by a Pari Boy SX compressor (Pari Medical Ltd., West Byfleet, United Kingdom), and mice were exposed to the aerosol via the attached head-only exposure chamber. Aerosolized CFI was drawn from the exposure chamber and then through a midget impinger (Ace Glass Inc., NJ) using a Universal standard pump pulling at 4 liters/min (SKC Limited, Blandford Forum, United Kingdom). Four milliliters of 50-mg/ml CFI was placed into the Pari LC Sprint Star nebulizer, and mice were exposed to the aerosol for 20 min. Mice were observed for 28 days postchallenge, with clinical signs recorded twice daily using the scoring system described for the F. tularensis LVS mouse study.
Relative bioavailability of ciprofloxacin in BALB/c mice.
The time-concentration profile of ciprofloxacin following a single dose of oral ciprofloxacin, intranasal CFI, or aerosolized CFI was determined using liquid chromatography-mass spectrometry (LC-MS). At 1 min, 15 min, 0.5 h, 1 h, 2 h, 4 h, 6 h, 10 h, 18 h, and 24 h postdosing, 3 BALB/c mice were culled and lungs were removed. Lung standards and samples were weighed and homogenized with 3 volumes of 0.1% formic acid in a Precellys bead homogenizer (Bertin Technologies, Villeurbanne, France). The homogenized lung was mixed with an equal volume of the internal standard, d-8 ciprofloxacin (Sigma-Aldrich Ltd., Dorset, United Kingdom), dissolved in 0.1% aqueous formic acid, and 2 volumes of dichloromethane were added. The mixture was centrifuged, and an aliquot of the upper, aqueous layer was removed and mixed with 3 volumes of acetonitrile. Following centrifugation, the supernatant was removed, reduced in volume to remove the acetonitrile using a centrifugal evaporator (Genevac Ltd., Ipswich, United Kingdom), and injected onto the LC-MS system. This system consisted of an Agilent 1100 binary pump (Agilent Technologies UK Ltd., Wokingham, United Kingdom), CTC PAL injector (Presearch Ltd., Basingstoke, United Kingdom), and Sciex API3000 LC-MS (AB Sciex, Warrington, United Kingdom,) using an ACE-3–C18HL 20- by 2.1-mm column (Hichrom, Theale, United Kingdom) with a gradient of 0.1% aqueous formic acid–0.1% formic acid in acetonitrile. Standard ciprofloxacin curves were generated in mouse lung homogenate. The lower and upper limits of detection were 10 ng/ml and 2,000 ng/ml, respectively. Lung homogenates were diluted with 0.1% aqueous formic acid to fall within the calibration range where appropriate.
Noncompartmental pharmacokinetic analysis of the mean concentration-time profiles of ciprofloxacin in the mouse lung was performed using WinNonlin Phoenix v.6.1 (Pharsight Corp., St. Louis, MO). The relative bioavailability of oral ciprofloxacin quantified in lung homogenate was calculated using an equation adapted from reference 21.
Statistical analysis.
Mouse weight differences were analyzed using 2-way analysis of variance (ANOVA) with Bonferroni posttests. Mouse survival was analyzed using Fisher's exact test, and a tied nonparametric technique was used to analyze survival times (22). The test uses ranks given by a data point's position in magnitude within the data and is designed to take into account tied data, which are common in the discrete data sets used. P values of <0.05 were considered statistically significant.
RESULTS
The efficacies of intranasally instilled CFI and oral ciprofloxacin against F. tularensis LVS cannot be distinguished in a mouse model of infection.
A single dose of intranasally instilled liposome-encapsulated ciprofloxacin has been shown to offer full protection against an intranasal challenge with F. tularensis LVS in a mouse model and provided significantly better protection than intranasally instilled ciprofloxacin (9, 11). These results have been confirmed in our laboratory (data not shown).
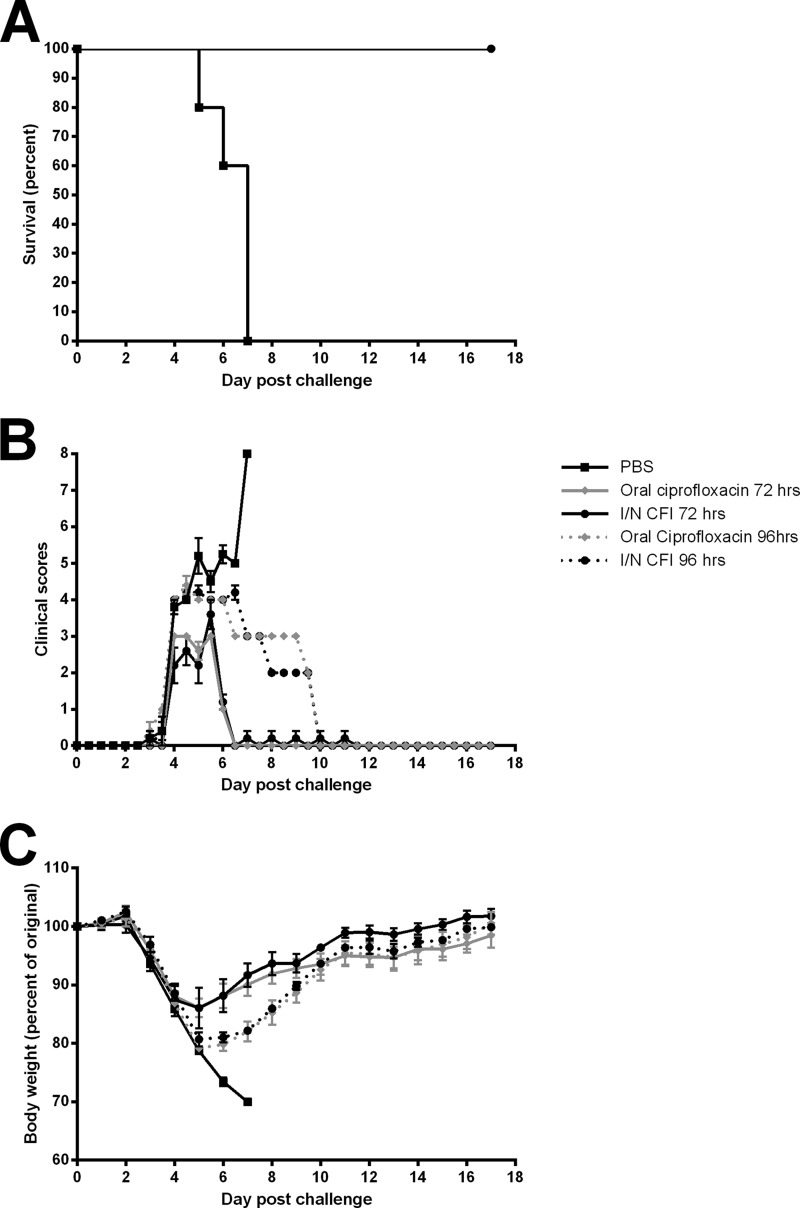
To further assess the efficacy of CFI as a potential treatment for tularemia, we compared intranasally instilled CFI to oral ciprofloxacin, the usual delivery route for this antibiotic. A single 50-mg/kg dose of intranasally delivered CFI offered full protection against a lethal intranasal F. tularensis LVS challenge, even when therapy was initiated at 72 or 96 h postchallenge (Fig. 1A). Similarly, a single dose of oral ciprofloxacin also provided full protection (Fig. 1A). The severity of clinical signs and weight loss were similar following all three treatment regimens (Fig. 1B and C). The only significant differences in weight were seen in animals undergoing treatment that was the same but initiated at a different time, i.e., at 96 h compared to 72 h, with later initiation of therapy causing greater weight loss on days 6, 7, and 8 (P < 0.05).
FIG 1.
Therapeutic efficacies of oral ciprofloxacin and intranasal CFI against an inhalational F. tularensis LVS infection in mice. Groups of 5 BALB/c mice were challenged with F. tularensis LVS via the intranasal (I/N) route and treated at 72 h (solid lines) or 96 h (dotted lines) postchallenge with a single 50-mg/kg dose of oral ciprofloxacin (diamonds), intranasal CFI (circles), or PBS (squares) delivered by the intranasal route. (A) Survival of mice. Only mice treated with PBS succumbed to the infection. (B) Clinical scores of mice. Mice were scored on the extent of piloerection, hunching, eye problems, and locomotion, with scores of 0, 1, and 2 specified for each category. (C) Weight change of mice over the course of the experiment. There were no significant differences in weight between mice dosed with oral ciprofloxacin or intranasally instilled CFI.
Intranasally instilled CFI provides significantly better protection than oral ciprofloxacin against highly virulent F. tularensis Schu S4.
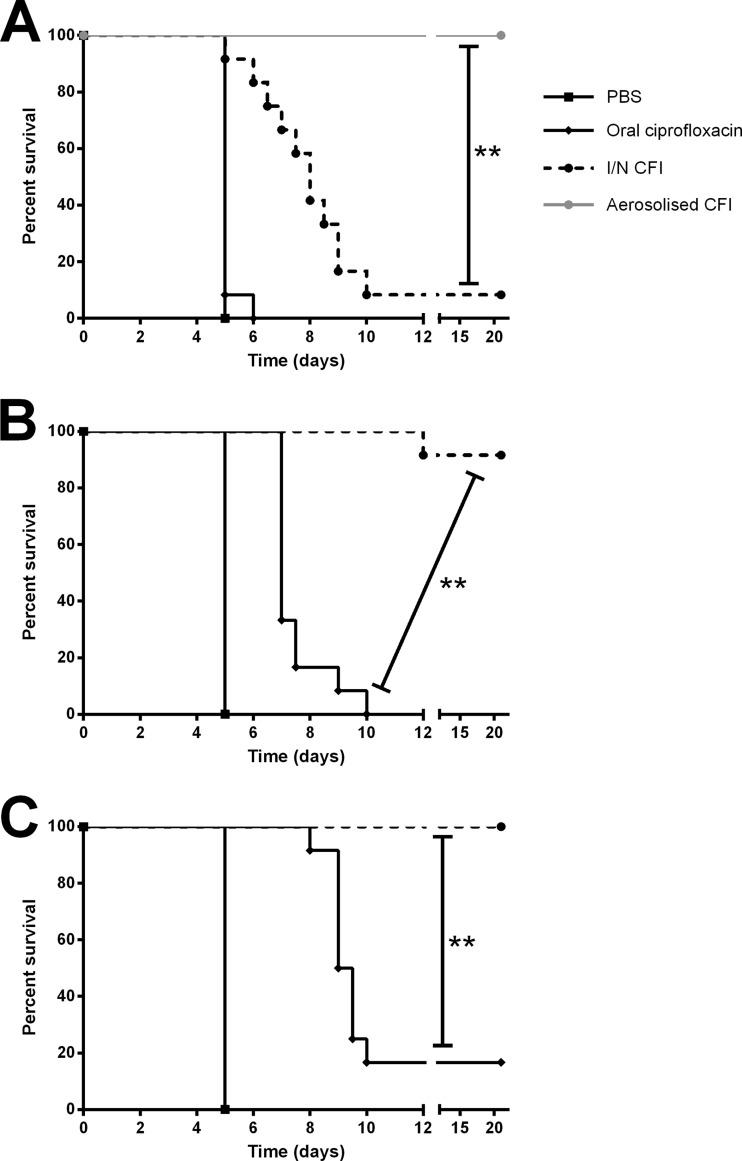
In an attempt to distinguish the efficacies of oral ciprofloxacin and intranasally instilled CFI, these antibiotics were evaluated against a highly virulent type A strain, F. tularensis Schu S4. A single dose of oral ciprofloxacin offered no protection to infected mice and did not increase time to death compared to the untreated controls (Fig. 2A). Furthermore, 3- and 5-day dosing regimens of twice-daily oral ciprofloxacin therapy did not prevent mortality but did significantly increase time to death compared to the untreated control animals (Fig. 2B and C) (P < 0.005). In contrast, treatment with intranasally delivered CFI once daily for 3 days resulted in over 90% survival, with 5 days of therapy providing full protection (Fig. 2). CFI intranasally instilled for 3 or 5 days significantly increased survival of infected mice compared to that of control animals (P < 0.005) and compared to all other oral ciprofloxacin treatment regimens in this study, including 5 days of twice-daily orally delivered ciprofloxacin (P < 0.005) (Fig. 2).
FIG 2.
Therapeutic efficacies of oral ciprofloxacin, intranasal CFI, and aerosolized CFI against inhalational F. tularensis Schu S4 infection in mice. Groups of 12 BALB/c mice were challenged with F. tularensis Schu S4 via the aerosol route and treated at 24 h postchallenge with 50 mg/kg of oral ciprofloxacin (diamonds line), 50 mg/kg of intranasal CFI (circles, solid lines), a 1-mg/kg lung dose of aerosolized CFI (circles, dashed lines), or PBS (squares) delivered by the intranasal route. Graphs show the survival of mice treated with a single dose of antibiotic (A), 3 days of therapy (B), or 5 days of therapy (C). Asterisks indicate significant differences in survival (**, P < 0.005).
Aerosolized CFI is more efficacious than intranasally instilled CFI.
A single intranasal dose of CFI administered at 24 h postchallenge provided very little protection against a lethal F. tularensis Schu S4 challenge, with only 1 mouse of 12 surviving (Fig. 2A). However, the treatment regimen did significantly increase the time to death of infected mice compared to untreated control animals or those given a single dose of oral ciprofloxacin (P < 0.005). In comparison, a single dose of aerosolized CFI given at 24 h postchallenge provided full protection and significantly increased survival compared to that of untreated controls (P < 0.005), all groups treated with oral ciprofloxacin (P < 0.005), or those given a single intranasal dose of CFI (P < 0.005) (Fig. 2A). This result was surprising, as intranasally instilled CFI resulted in a greater peak concentration in the lung than aerosolized CFI and a 60-fold greater area under the concentration-time curve (AUC) in the lung (Table 1), which represents the total overall ciprofloxacin exposure.
TABLE 1.
Pharmacokinetic parameters of ciprofloxacin in lung homogenate following a single dose of oral ciprofloxacin, intranasal CFI, or aerosolized CFI
| Therapy | Dose (mg/kg) | Cmax (μg/g) | t1/2 (h) | Clearance (kg/h/kg) | AUC0–24 (h · μg/g) |
|---|---|---|---|---|---|
| Oral ciprofloxacin | 50 | 55.8 | 4.2 | 5,014.7 | 9.2 |
| Intranasal CFI | 50 | 3,326.7 | 6.6 | 0.8 | 52,373.8 |
| Aerosolized CFI | 1a | 116.1 | 7.4 | 1.2 | 772.7 |
Actual received lung dose (determined during pharmacokinetics study from 1-min time point).
A high lung concentration of ciprofloxacin is sustained following administration of aerosolized CFI.
A single dose of oral ciprofloxacin results in a high initial concentration of ciprofloxacin in the lung, which is similar to the concentration achieved after delivery of aerosolized CFI (Table 1, maximum concentration [Cmax] values). However, the unencapsulated ciprofloxacin is rapidly eliminated from the lungs (Table 1), resulting in an 80-times-longer terminal half-life in the lung for aerosolized CFI than for oral ciprofloxacin. This difference in elimination produced a 100-fold-greater AUC in the lung for aerosolized CFI than for oral ciprofloxacin (Table 1), with the relative bioavailability of oral ciprofloxacin in the lung with reference to the aerosolized CFI being 0.02%.
DISCUSSION
Following a deliberate release of F. tularensis, authorities would aim to offer prophylaxis to those who may have been exposed. Ideally, this prophylaxis would be highly effective and could be taken by patients without medical supervision. The currently recommended prophylactic options, oral ciprofloxacin and oral doxycycline, although easy to administer, have been associated with relapse in murine prophylaxis studies (3, 23) and in some cases of human therapy (4, 6). Therefore, there is the need for a new antibiotic, or a new presentation of an existing antibiotic, such as an alternative formulation and administration method, that can offer a higher level of protection against F. tularensis without the need for delivery by injection. Previous studies have suggested that liposomal ciprofloxacin may be useful as a postexposure therapeutic for tularemia via the inhalational route (8–11). In this study, we aimed to further evaluate the efficacy of CFI, currently in clinical trials as an inhalational therapy for infections associated with bronchiectasis (14–16), for use against F. tularensis.
F. tularensis LVS was developed by the U.S. Department of Defense from a Russian live vaccine strain in the 1950s (24). Although LVS offers protection against low inhalational challenges, its use as a vaccine has been restricted due to limited efficacy at higher challenge doses, inconsistencies with the preparation, and an unknown basis of attenuation (2). It is not licensed in the United States and Europe. Nonetheless, this relatively avirulent strain is useful as a model for the more virulent strains of F. tularensis, as it does not require the high levels of biocontainment normally associated with handling F. tularensis and yet causes a lethal infection in mice (24).
In this study, an evaluation of CFI in the murine model of lethal F. tularensis LVS infection demonstrated that just a single dose of intranasally instilled CFI offered full protection. However, perhaps somewhat surprisingly, a single dose of oral ciprofloxacin also gave full protection against F. tularensis LVS, preventing differentiation between the efficacies of the antibiotics given by either route of administration. Oral ciprofloxacin treatment for 14 days does not fully protect against F. tularensis Schu S4 infection in mice (3), suggesting that the efficacy of the short treatment regimen used in this study against LVS does not reflect the efficacy against more virulent F. tularensis strains. The shortcomings of F. tularensis LVS as a model for understanding the gene function of more virulent strains has been highlighted previously (25). The results presented in this study highlight that antibiotic testing using LVS as a model of the more virulent F. tularensis strains also has its limitations.
The use of the more virulent F. tularensis Schu S4 strain, which was originally isolated from a human ulcer (26), enabled the efficacies of oral ciprofloxacin and CFI to be distinguished in vivo. Aerosolized CFI provided full protection after just a single dose, whereas even with 5 days of twice-daily dosing, oral ciprofloxacin did not prevent mortality, although it did extend the time to death. This study also demonstrated that in this mouse model, CFI delivered as an aerosol is superior to intranasally instilled CFI, as a single dose of intranasally instilled CFI provided only minimal protection. This result may appear surprising considering the much lower quantities of ciprofloxacin delivered to the mouse lung by the inhalational route than by intranasal instillation. In addition, delivery of CFI by intranasal instillation results in a much greater AUC in the lung than aerosol delivery. However, previous studies comparing intratracheal instillation and inhalational delivery have shown that intratracheal instillation results in a more centralized deposition, while aerosol delivery results in a more even and widely distributed drug delivery (27). This finding may explain the observed difference in efficacy of CFI delivered by intranasal instillation versus aerosol, as the inhalational F. tularensis Schu S4 challenge is able to penetrate deep into lung tissue where the intranasally instilled delivered formulation may not reach. Therefore, some bacteria may not come into contact with the intranasally instilled CFI, enabling the disease to progress and resulting in the animals succumbing to the infection if just a single dose of antibiotic is administered. In contrast, CFI delivered as an aerosol may be better able to reach the bacteria localized in the lung periphery, preventing disease progression and death.
This study has demonstrated the longevity of ciprofloxacin in the lungs after intranasal or aerosolized CFI administration compared to oral ciprofloxacin administration. The data suggest that the elimination of ciprofloxacin is rate limited by its slow release from the liposome following administration of CFI. In addition, increased uptake of encapsulated ciprofloxacin by macrophages (28) may further slow elimination and increase the proximity of the antibiotic to this intracellular pathogen harbored by the macrophages.
These factors may also explain the superior efficacy of CFI compared to oral ciprofloxacin in the mouse studies with F. tularensis Schu S4. The results suggest that the length of the prophylaxis regimen could be shortened if CFI was used instead of oral ciprofloxacin. Additional studies in nonhuman primates using appropriately scaled antibiotic doses could be used to confirm any potential reduction in the prophylaxis regimen. A reduced prophylaxis regimen and localized therapy to the lung will reduce systemic exposure and therefore the associated systemic side effects associated with ciprofloxacin. A survey of U.S. postal workers during the anthrax attacks in the United States in 2001 showed that of those prescribed oral ciprofloxacin, 3% stopped the medication due to side effects, with an additional 1% ceasing medication due to fear of side effects (29). Thus, the use of a shortened CFI prophylaxis regimen instead of the standard oral ciprofloxacin treatment may reduce the associated side effects, improving uptake and continued compliance with prophylaxis.
Ciprofloxacin is the recommended prophylaxis for several other candidate BW agents, including the causative agents of anthrax and plague (30, 31). Our data suggest that the efficacy of CFI against these agents should also be studied as an alternative prophylaxis. Furthermore, the efficacy of CFI against the wide range of pathogens that enter the host through the inhalational path should be investigated. A reduction in length of the prophylaxis regimen resulting from the use of CFI, if shown to be efficacious, could have very significant advantages in terms of cost, logistics, and compliance. Consequently, inhaled CFI is a promising novel therapy which should be investigated further for use in the event of a deliberate release of BW agents.
ACKNOWLEDGMENTS
We thank T. Laws and G. Tetley for technical assistance.
This work was funded by the United Kingdom Ministry of Defense.
Published with the permission of the Defence Science and Technology Laboratory on behalf of the Controller of HMSO.
Footnotes
Published ahead of print 17 March 2014
REFERENCES
- 1.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Tonat K, for the Working Group on Civilian Biodefense 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763–2773. 10.1001/jama.285.21.2763 [DOI] [PubMed] [Google Scholar]
- 2.Oyston PCF, Sjöstedt A, Titball RW. 2004. Tularaemia: bioterrorism defence renews interest in Francisella tularensis. Nat. Rev. Microbiol. 2:967–978. 10.1038/nrmicro1045 [DOI] [PubMed] [Google Scholar]
- 3.Steward J, Piercy T, Lever MS, Simpson AJH, Brooks TJG. 2006. Treatment of murine pneumonic Francisella tularensis infection with gatifloxacin, moxifloxacin or ciprofloxacin. Int. J. Antimicrob. Agents 27:439–443. 10.1016/j.ijantimicag.2006.02.006 [DOI] [PubMed] [Google Scholar]
- 4.Hepburn MJ, Simpson AJH. 2008. Tularemia: current diagnosis and treatment options. Expert Rev. Anti Infect. Ther. 6:231–240. 10.1586/14787210.6.2.231 [DOI] [PubMed] [Google Scholar]
- 5.Perez-Castrillon JL, Bachiller-Luque P, Martin-Luquero M, Mena-Martin FJ, Herreros V. 2001. Tularemia epidemic in northwestern Spain: clinical description and therapeutic response. Clin. Infect. Dis. 33:573–576. 10.1086/322601 [DOI] [PubMed] [Google Scholar]
- 6.Chocarro A, Gonzalez A, Garcia I. 2000. Treatment of tularemia with ciprofloxacin. Clin. Infect. Dis. 31:623. 10.1086/313946 [DOI] [PubMed] [Google Scholar]
- 7.Carryn S, Chanteux H, Seral C, Mingeot-Leclercq MP, Van Bambeke F, Tulkens PM. 2003. Intracellular pharmacodynamics of antibiotics. Infect. Dis. Clin. North. Am. 17:615–634. 10.1016/S0891-5520(03)00066-7 [DOI] [PubMed] [Google Scholar]
- 8.Conley J, Yang HM, Wilson T, Blasetti K, Di Ninno V, Schnell G, Wong JP. 1997. Aerosol delivery of liposome-encapsulated ciprofloxacin: aerosol characterization and efficacy against Francisella tularensis infection in mice. Antimicrob. Agents Chemother. 41:1288–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Di Ninno VL, Cherwonogrodzky JW, Wong JP. 1993. Liposome-encapsulated ciprofloxacin is effective in the protection and treatment of Balb/c mice against Francisella tularensis. J. Infect. Dis. 168:793–794. 10.1093/infdis/168.3.793 [DOI] [PubMed] [Google Scholar]
- 10.Wong JP, Yang HM, Blasetti KL, Schnell G, Conley J, Schofield LN. 2003. Liposome delivery of ciprofloxacin against intracellular Francisella tularensis infection. J. Control Release 92:265–273. 10.1016/S0168-3659(03)00358-4 [DOI] [PubMed] [Google Scholar]
- 11.Wong JP, Cherwonogrodzky JW, Di Ninno V, Dela Cruz R, Saravolac EG. 1995. Liposome-encapsulated ciprofloxacin for the prevention and treatment of infectious diseases by intracellular pathogens, p 105–120 In Shek PN. (ed), Liposomes in biomedical applications. Harwood Academic Press, Amsterdam, The Netherlands [Google Scholar]
- 12.Ahsan F, Rivas IP, Khan MA, Torres Suárez AI. 2002. Targeting to macrophages: role of physicochemical properties of particulate carriers—liposomes and microspheres—on the phagocytosis by macrophages. J. Control Release 79:29–40. 10.1016/S0168-3659(01)00549-1 [DOI] [PubMed] [Google Scholar]
- 13.Schiffelers R, Storm G, Bakker-Woudenberg I. 2001. Liposome-encapsulated aminoglycosides in pre-clinical and clinical studies. J. Antimicrob. Chemother. 48:333–344. 10.1093/jac/48.3.333 [DOI] [PubMed] [Google Scholar]
- 14.Bruinenberg P, Blanchard J, Cipolla D, Dayton F, Mudumba S, Gonda I. 2010. Inhaled liposomal ciprofloxacin: once a day management of respiratory infections. In Dalby RN, Byron PR, Peart J, Suman JD, Farr SJ, Young PM. (ed), Respiratory Drug Delivery 2010, vol 1, p 73–82 Virginia Commonwealth University, Richmond, VA [Google Scholar]
- 15.Serisier D. 2012. Inhaled antibiotics for lower respiratory tract infections: focus on ciprofloxacin. Drugs Today 48:339–351. 10.1358/dot.2012.48.5.1789474 [DOI] [PubMed] [Google Scholar]
- 16.Serisier DJ, Bilton D, De Soyza A, Thompson PJ, Kolbe J, Greville HW, Cipolla D, Bruinenberg P, Gonda I. 2013. Inhaled, dual release liposomal ciprofloxacin in non-cystic fibrosis bronchiectasis (ORBIT-2): a randomised, double-blind, placebo-controlled trial. Thorax 68:812–817. 10.1136/thoraxjnl-2013-203207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartley G, Taylor R, Prior J, Newstead S, Hitchen PG, Morris HR, Dell A, Titball RW. 2006. Grey variants of the live vaccine strain of Francisella tularensis lack lipopolysaccharide O-antigen, show reduced ability to survive in macrophages and do not induce protective immunity in mice. Vaccine 24:989–996. 10.1016/j.vaccine.2005.08.075 [DOI] [PubMed] [Google Scholar]
- 18.Druett HA. 1969. A mobile form of the Henderson apparatus. Epidemiol. Infect. 67:437–448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harper GJ, Morton JD. 1953. The respiratory retention of bacterial aerosols: experiments with radioactive spores. Epidemiol. Infect. 51:372–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guyton AC. 1947. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 150:70–77 [DOI] [PubMed] [Google Scholar]
- 21.Rowland M, Tozer TN. 2010. Clinical pharmacokinetics and pharmacodynamics: concepts and applications, 4th ed, p 159–215 Lippincott Williams and Wilkins, Philadelphia, PA [Google Scholar]
- 22.Oyeka ICA, Ebuh GU, Nwosu CR. 2012. Analysis of tied data: an alternative non-parametric approach. Int. J. Eng. Sci. Technol. 4:811–817 [Google Scholar]
- 23.Piercy T, Steward J, Lever MS, Brooks TJG. 2005. In vivo efficacy of fluoroquinolones against systemic tularaemia infection in mice. J. Antimicrob. Chemother. 56:1069–1073. 10.1093/jac/dki359 [DOI] [PubMed] [Google Scholar]
- 24.Eigelsbach HT, Downs CM. 1961. Prophylactic effectiveness of live and killed tularemia vaccines. J. Immunol. 87:415–425 [PubMed] [Google Scholar]
- 25.Kadzhaev K, Zingmark C, Golovliov I, Bolanowski M, Shen H, Conlan W, Sjöstedt A. 2009. Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS One 4:e5463. 10.1371/journal.pone.0005463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eigelsbach HT, Braun W, Herring RD. 1951. Studies on the variation of Bacterium tularense. J. Bacteriol. 61:557–569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brain JD, Knudson DE, Sorokin SP, Davis MA. 1976. Pulmonary distribution of particles given by intratracheal instillation or by aerosol inhalation. Environ. Res. 11:13–33. 10.1016/0013-9351(76)90107-9 [DOI] [PubMed] [Google Scholar]
- 28.Oh YK, Nix DE, Straubinger RM. 1995. Formulation and efficacy of liposome-encapsulated antibiotics for therapy of intracellular Mycobacterium avium infection. Antimicrob. Agents Chemother. 39:2104–2111. 10.1128/AAC.39.9.2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brechner R, DiFerdinando G, Bresntiz E, Factor SH, Matte TD, Siegel L, Adams S, Walks I, Davies-Coles J, Richardson M, Peterson E, Stroube R. 2001. Update: adverse events associated with anthrax prophylaxis among postal employees—New Jersey, New York City, and the District of Columbia Metropolitan Area, 2001. JAMA 286:2935–2936. 10.1001/jama.286.23.2935 [DOI] [PubMed] [Google Scholar]
- 30.Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Gerberding J, Hauer J, Hughes J, McDade J, Osterholm MT, Parker G, Perl TM, Russell PK, Tonat K, for the Working Group on Civilian Biodefense 2002. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA 287:2236–2252. 10.1001/jama.287.17.2236 [DOI] [PubMed] [Google Scholar]
- 31.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Koerner JF, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Schoch-Spana M, Tonat K, for the Working Group on Civilian Biodefense 2000. Plague as a biological weapon: medical and public health management. JAMA 283:2281–2290. 10.1001/jama.283.17.2281 [DOI] [PubMed] [Google Scholar]