Abstract
Entamoeba histolytica and Giardia lamblia are anaerobic protozoan parasites that cause amebiasis and giardiasis, two of the most common diarrheal diseases worldwide. Current therapy relies on metronidazole, but resistance has been reported and the drug has significant adverse effects. Therefore, it is critical to search for effective, better-tolerated antiamebic and antigiardial drugs. We synthesized several examples of a recently reported class of Hsp90 inhibitors and evaluated these compounds as potential leads for antiparasitic chemotherapy. Several of these inhibitors showed strong in vitro activity against both E. histolytica and G. lamblia trophozoites. The inhibitors were rescreened to discriminate between amebicidal and giardicidal activity and general cytotoxicity toward a mammalian cell line. No mammalian cytotoxicity was found at >100 μM for 48 h for any of the inhibitors. To understand the mechanism of action, a competitive binding assay was performed using the fluorescent ATP analogue bis-ANS (4,4′-dianilino-1,1′-binaphthyl-5,5′-disulfonic acid dipotassium salt) and recombinant E. histolytica Hsp90 preincubated in both the presence and absence of Hsp90 inhibitors. There was significant reduction in fluorescence compared to the level in the control, suggesting that E. histolytica Hsp90 is a selective target. The in vivo efficacy and safety of one Hsp90 inhibitor in a mouse model of amebic colitis and giardiasis was demonstrated by significant inhibition of parasite growth at a single oral dose of 5 mg/kg of body weight/day for 7 days and 10 mg/kg/day for 3 days. Considering the results for in vitro activity and in vivo efficacy, Hsp90 inhibitors represent a promising therapeutic option for amebiasis and giardiasis.
INTRODUCTION
The protozoan intestinal parasites Entamoeba histolytica and Giardia lamblia are the agents of human amebiasis and giardiasis, respectively. Infections by these parasites are major causes of morbidity and mortality in tropical countries and a significant public health problem in the United States. Amebiasis is responsible for 50 million cases of invasive disease (1) and about 70,000 deaths annually in the world (2). Giardiasis has an estimated worldwide prevalence of 280 million cases annually. In developed countries, G. lamblia infects about 2% of adults and 6 to 8% of children (3–5). The prevalence of G. lamblia infection is generally higher in developing countries, ranging from 3% to 90% (6–12). Furthermore, giardial infections contribute substantially to the 2.5 million annual deaths from diarrheal disease (13, 14). In Asia, Africa, and Latin America, about 500,000 new giardiasis cases are reported each year. Both E. histolytica and G. lamblia have been listed by the NIH as category B priority biodefense pathogens due to their low infectious doses and potential for dissemination through compromised food and water supplies in the United States. Because of its link with poverty, Giardia was included in the WHO Neglected Diseases Initiative in 2004 (15).
Despite the prevalence of amebiasis and giardiasis, there are no vaccines or prophylactic drugs. The first-line drugs for amebiasis and giardiasis chemotherapy are nitroimidazoles, with the prototype, metronidazole, being the drug of choice, particularly in developing countries (16). The standard treatment with metronidazole requires at least 10 days at a high dosage (750 mg 3 times a day [t.i.d.]) to eradicate intestinal amebae and 3 to 5 days of 250 mg t.i.d. for Giardia (3, 17–19). In addition, follow-up treatment with a second drug, such as paromomycin, is recommended for amebiasis to prevent prolonged retention and excretion of cysts (20). Newer metronidazole derivatives, such as tinidazole (21) and nitazoxanide, a nitrothiazoly-salicylamide derivative (22), have fewer side effects and shorter treatment courses. Other drugs, such as furazolidone, albendazole, and paromomycin, are used for giardiasis to a lesser extent, with similar or lower success rates. Metronidazole has been shown to be both mutagenic in a microbiological system and carcinogenic to rodents (23–25). In addition, this drug has several adverse effects, the most common being gastrointestinal disturbances, especially nausea, vomiting, and diarrhea or constipation (26). Potential resistance of E. histolytica to metronidazole is an increasing concern as, in vitro, E. histolytica trophozoites adapt to therapeutically relevant levels of metronidazole (27, 28). In spite of the efficacy of nitroimidazole drugs, treatment failures in giardiasis occur in up to 20% of cases (29). Clinical resistance of G. lamblia to metronidazole is proven, and cross-resistance occurs to the newer drugs, tinidazole and nitazoxanide, so drug resistance is a concern with all commonly used antigiardial drugs (14, 29, 30). Therefore, it is critical to search for effective and better-tolerated antiamebic and antigiardial drugs.
Hsp90 is a highly conserved molecular chaperone that assists protein folding and participates in the regulation of the cell cycle, as well as in signal transduction pathways in eukaryotes. Hsp90 is implicated in growth and development in many protozoan species, including Dictyostelium, Leishmania, Plasmodium, Trypanosoma, and Giardia species (31–35). Inhibition of parasite Hsp90 activity by geldanamycin resulted in lethality in Plasmodium falciparum (36), but this compound has not been pursued for clinical development due to unacceptable toxicity. The recent development of orally bioavailable and druglike Hsp90 inhibitors (37) inspired us to synthesize and evaluate several of these compounds as antiamebic and antigiardial agents. In this study, we demonstrate strong in vitro activity of several of these novel inhibitors against both E. histolytica and G. lamblia trophozoites. We used one such inhibitor, SNX-2112, and its orally bioavailable prodrug, SNX-5422, to investigate its efficacy in vivo against infection with E. histolytica and G. lamblia.
MATERIALS AND METHODS
Chemicals and reagents.
White, solid-bottom, tissue culture-treated 96-well microplates were purchased from E&K Scientific (Santa Clara, CA). The CellTiter-Glo luminescent cell viability assay was purchased from Promega (Madison, WI); dimethyl sulfoxide (DMSO), 4,4′-dianilino-1,1′-binaphthyl-5,5′-disulfonic acid dipotassium salt (bis-ANS), cyanogen bromide (CNBr)-activated Sepharose 4B, and metronidazole were purchased from Sigma-Aldrich (St. Louis, MO). SNX-5422 was purchased from Selleck Chemicals (Houston, TX).
Maintenance of E. histolytica, G. lamblia, and Jurkat T lymphocytes.
Trophozoites of E. histolytica strain HM1:IMSS and G. lamblia strain WB were axenically maintained in TYI-S-33 medium supplemented with penicillin (100 U/ml) and streptomycin (100 μg/ml) (38). Jurkat T lymphocytes (clone E6-1) were maintained in RPMI 1640 medium with HEPES, supplemented with penicillin (100 U/ml), streptomycin (100 μg/ml), and 10% heat-inactivated fetal bovine serum, and cultured according to ATCC specifications (ATCC, Manassas, VA) (39). E. histolytica and G. lamblia trophozoites and Jurkat cells were counted using a particle counter (Beckman Coulter, Fullerton, CA). The logarithmic phase of growth of the human cell line was determined by counting the cells using the particle counter, and the cells were maintained in this growth phase by routine passage every 2 days. All experiments were performed using trophozoites and human cells harvested during the logarithmic phase of growth.
Synthesis of Hsp90 inhibitors and evaluation of their activity against E. histolytica, G. lamblia, and Jurkat lymphocytes.
A novel class of Hsp90 inhibitors, indol-4-one and indazol-4-one-derived 2-aminobenzamides, was synthesized following the methods described by Huang et al. (37). The benzonitrile intermediates involved in the synthesis of the benzamides were also evaluated for activity. The compounds were screened for activity against E. histolytica and G. lamblia using an ATP-bioluminescence-based assay for cell growth and survival (40, 41). Briefly, 2.5 μl of 5 mM stock compounds were diluted with 17.5 μl sterile water to yield 625 μM working concentration of compounds. A 3-fold serial dilution was then performed, yielding a concentration range of 0.25 to 625 μM. From this dilution plate, 4-μl amounts were transferred into the 96-well screen plates, followed by the addition of 96 μl of trophozoites (5,000 parasites) to yield a final 8-point concentration range spanning 0.01 to 25 μM. Assay plates were incubated for 48 h at 37°C in the GasPak EZ gas-generating anaerobe pouch system (VWR, West Chester, PA) to maintain an anaerobic condition throughout the incubation period. The assays were performed in triplicate using the CellTiter-Glo luminescent cell viability assay (40).
For cytotoxicity assays, 4-μl amounts from the compound dilution plates were transferred into a 96-well screen plate, followed by the addition of 96 μl of Jurkat cells (10,000 cells) to yield different compound concentrations, with a final DMSO concentration of 0.5%. The negative control contained the final 0.5% DMSO, and the positive control contained a final concentration of 40 μM staurosporine (BioVision, Mountain View, CA). The assay was performed in triplicate using the CellTiter-Glo luminescent cell viability assay (42).
Morphological studies.
To evaluate the impact of Hsp90 inhibitor on trophozoite morphology, E. histolytica and G. lamblia trophozoites were incubated with different concentrations of SNX-2112 in 12-well tissue culture plates (Corning, NY) and incubated for 48 h at 37°C in the GasPak EZ gas-generating anaerobe pouch systems. After incubation, live trophozoites were imaged under an Axiovert 40 CFL phase-contrast microscope (Carl Zeiss, Germany).
Effect of Hsp90 inhibitors on recombinant E. histolytica Hsp90 ATP-binding domain.
The gene segment coding for the E. histolytica Hsp90 ATP-binding domain (amino acids 1 to 210) (Gene ID no. EHI_102270) was amplified from genomic DNA extracted from the E. histolytica HM1:IMSS strain using forward (5′-CCGGGATCCATGGGAAATAGAAAA-3′) and reverse (5′-GCGCGGTTCGAAATATTGAATAAATTC-3′) primers cloned into the pET28a vector and was transformed in BL21(DE3) CodonPlus cells. Protein expression was induced with 0.4 mM isopropyl-β-d-thiogalactopyranoside (IPTG) overnight at 24°C, the pellet was resuspended in lysis buffer (20 mM HEPES, pH 7.5, 10% glycerol, 20 mM imidazole, 500 mM NaCl, 0.5% NP-40) supplemented with bacterial protease inhibitor cocktail (Sigma-Aldrich), and the protein was purified by Ni-nitrilotriacetic acid (NTA) affinity chromatography (Qiagen, Germany) (43). The fluorescent probe 4,4′-dianilino-1,1′-binaphthyl-5,5′-disulfonic acid dipotassium salt (bis-ANS) was used for binding assays with the E. histolytica Hsp90 ATP-binding domain. Briefly, the recombinant purified E. histolytica Hsp90 (final concentration 1 μM) was preincubated for 45 min at 37°C with DMSO control or in the presence of Hsp90 inhibitors to a final concentration of 100 nM. bis-ANS was then added to a final concentration of 5 μM in binding buffer (20 mM Tris, pH 7.5, 10 mM MgCl2, 50 mM KCl) and incubated at 37°C for 30 min. Fluorescence emission data were collected on an EnVision fluorescent monochromator spectrophotometer (Perkin-Elmer, Waltham, MA). The excitation wavelength for bis-ANS was set at 372 nm, and emission was captured at 490 nm (43).
Hsp90 inhibitor-Sepharose 4B generation and in vitro Hsp90 inhibitor pulldown assay.
For pulldown assays, Hsp90 inhibitors were coupled to cyanogen bromide (CNBr)-activated Sepharose 4B (Sigma-Aldrich). Briefly, the CNBr-activated Sepharose was oversaturated with inhibitor to maximize coupling by nucleophilic attack. The conjugation was allowed to take place overnight at room temperature with agitation. The active groups were blocked with ethanolamine for 3 h. The conjugated bead slurry, as well as unbound control beads, were incubated with 100 μg of E. histolytica protein extract for 4 h at 4°C under agitation. After centrifugation, the unbound solution was discarded and the beads were washed four times with 1% SDS, 5 mM EDTA, pH 8. The beads were boiled in Laemmli sample buffer for 5 min, and the denatured proteins and the control were run on a SDS-PAGE gel and immunoblotted with a rabbit polyclonal anti-P. falciparum Hsp90 antibody (which cross-reacts with Hsp90 in E. histolytica) (44).
Efficacy of Hsp90 inhibitor in animal models of E. histolytica and G. lamblia infection.
One million cecal-passed E. histolytica HM1:IMSS trophozoites were injected into the cecum of 6-week-old C3H/HeJ male mice (The Jackson Laboratory, Bar Harbor, ME) (45). The mice were treated for 7 days by oral gavage with 5 mg/kg of body weight/day of SNX-5422 (Selleck Chemicals), a prodrug of the Hsp90 inhibitor SNX-2112. The severity of amebic infection was determined by histopathology and quantification of trophozoites in the cecum by real-time PCR (46). The number of trophozoites/g of cecum was determined by quantitative PCR (qPCR) and graphed as the percentage of the mean of the control, calculated as the number of trophozoites/g of cecum divided by the mean number of trophozoites in control mice times 100.
For Giardia infections, adult C57BL/6 mice (The Jackson Laboratory) were bred at the University of California, San Diego (UCSD). To infect suckling mice (5 to 7 days old), G. lamblia trophozoites were grown to mid-logarithmic phase and administered by oral gavage at 107/mouse in a 50-μl volume in Giardia growth medium (41). After 5 days of infection, mice were treated by oral gavage with 5 mg/kg/day or 10 mg/kg/day of SNX-5422 for 3 days. At the end of the treatment, the entire small intestine was removed, opened longitudinally, placed into 2 to 5 ml of phosphate-buffered saline (PBS), and cooled on ice for 10 min. Live trophozoites were counted in a hemocytometer. All animal studies were reviewed and approved by the UCSD Institutional Animal Care and Use Committee.
RESULTS
Effect of Hsp90 inhibitors against E. histolytica, G. lamblia, and Jurkat lymphocytes in vitro.
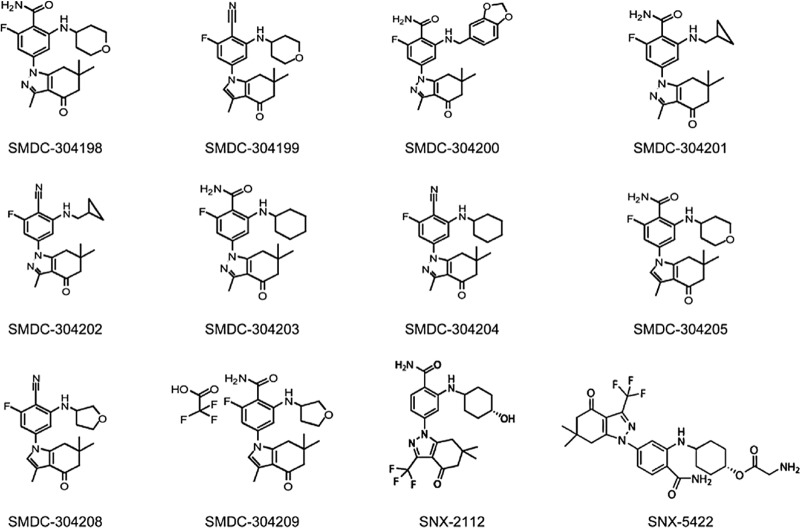
We synthesized and tested SNX-2112 and several analogues (SMDC-304198, SMDC-304200, SMDC-304201, SMDC-304203, SMDC-304205, and SMDC-304209) (Fig. 1) for efficacy against E. histolytica and G. lamblia. The benzonitrile intermediates involved in their preparation (SMDC-304199, SMDC-304202, SMDC-304204, and SMDC-304208) (Fig. 1) were also tested for their activity against E. histolytica and G. lamblia. In our system, the 50% effective concentrations (EC50s) for metronidazole, defined as the concentration of compound necessary to reduce cell growth and survival to 50% of that in DMSO-treated controls, were 5 μM for E. histolytica and 8.5 μM for G. lamblia. We found that SNX-2112, SMDC-304198, SMDC-304201, SMDC-304203, SMDC-304205, and SMDC-304209 were active against both E. histolytica and G. lamblia, with EC50s better than those of metronidazole (Table 1). SMDC-304200 failed to show potency, possibly due to the presence of a larger group in the C-2 position of the indazolone. The nitrile intermediates SMDC-304199, SMDC-304202, SMDC-304204, and SMDC-304208 were not active against E. histolytica and G. lamblia. Lack of activity for the nitrile compounds supports the hypothesis that the carboxamides are targeting parasite Hsp90.
FIG 1.
Chemical structures of Hsp90 inhibitors tested against E. histolytica and G. lamblia trophozoites.
TABLE 1.
Hits obtained after screening the Hsp90 inhibitors
| Hsp90 inhibitor | EC50 (μM) for: |
||
|---|---|---|---|
| E. histolytica | G. lamblia | Jurkat cells | |
| SMDC-304198 | 0.7 | 0.2 | >100 |
| SMDC-304201 | 2 | >1 | >100 |
| SMDC-304203 | 4.6 | 0.3 | >100 |
| SMDC-304205 | 3.5 | 0.1 | >100 |
| SMDC-304209 | 1.3 | 0.06 | >100 |
| SNX-2112 | 1.6 | 0.8 | >100 |
A mammalian cell line toxicity assay was performed with Jurkat T cells, an established model for in vitro compound toxicity (39). No cytotoxicity was seen at inhibitor concentrations of >100 μM for 48 h (Table 1).
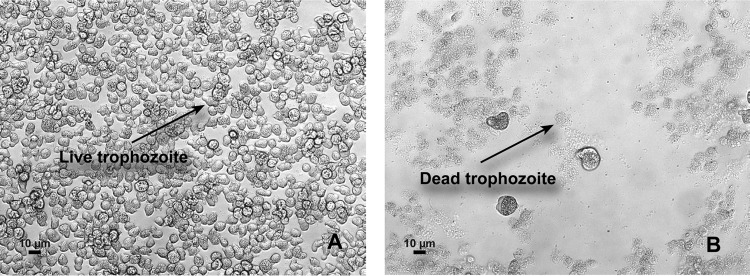
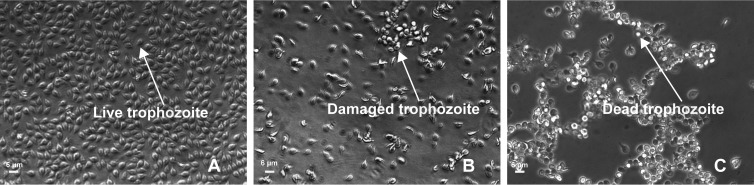
Effect of Hsp90 inhibitor on E. histolytica and G. lamblia morphology.
Morphological studies clearly showed the lethal effect of SNX-2112 at low concentrations. The examination of trophozoites incubated for 48 h in the presence of 3 μM SNX-2112 showed complete lysis of E. histolytica (Fig. 2B). The same concentration of SNX-2112 caused significant growth inhibition and morphological defects of G. lamblia (Fig. 3B), and at 6 μM SNX-2112, there was death of G. lamblia trophozoites (Fig. 3C).
FIG 2.
Effect of SNX-2112 on E. histolytica morphology. Trophozoites were treated with 3 μM SNX-2112 for 48 h. (A) E. histolytica trophozoites treated with 0.5% DMSO. Arrow indicates live trophozoite. Magnification, ×10. (B) E. histolytica trophozoites treated with 3 μM SNX-2112. Treatment caused complete lysis of trophozoites (arrow). Magnification, ×10. Trophozoites were imaged under phase-contrast microscope.
FIG 3.
Effect of SNX-2112 on G. lamblia morphology. Trophozoites were treated with 3 μM and 6 μM SNX-2112 for 48 h. (A) G. lamblia trophozoites treated with 0.3% DMSO. Arrow indicates live trophozoite. Magnification, ×20. (B) G. lamblia trophozoites treated with 3 μM SNX-2112. Treatment caused significant growth inhibition and morphological defects of trophozoites (arrow). Magnification, ×20. (C) G. lamblia trophozoites treated with 6 μM SNX-2112. Treatment caused death of trophozoites (arrow). Magnification, ×20. Trophozoites were imaged under a phase-contrast microscope.
Effect of Hsp90 inhibitors on recombinant E. histolytica Hsp90.
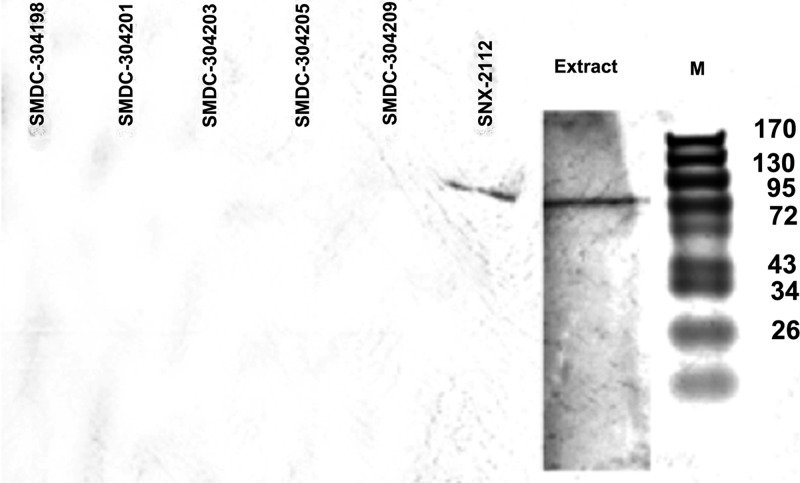
To understand the mechanism of action of Hsp90 inhibitors in E. histolytica, we used the established technique (47) of a bis-ANS binding assay with recombinant E. histolytica Hsp90 ATP-binding domain in the presence of Hsp90 inhibitors SNX-2112, SMDC-304198, SMDC-304201, SMDC-304203, and SMDC-304209. This assay relies on competitive inhibition of bis-ANS, which is known to compete with ATP for ATPase domain binding and emits fluorescence upon hydrophobic pocket binding (47). SNX-2112 caused a significant reduction in fluorescence at 100 nM compared to the fluorescence in the DMSO control (P = 0.0187), suggesting competitive inhibition of E. histolytica Hsp90 ATP binding (Fig. 4). To determine whether SNX-2112, SMDC-304198, SMDC-304201, SMDC-304203, SMDC-304205, and SMDC-304209 exhibit specificity for Hsp90 relative to any binding of other cellular proteins of E. histolytica, the denatured E. histolytica protein extract for the drug pulldown and the control were run on a SDS-PAGE gel and immunoblotted with polyclonal anti-P. falciparum Hsp90 antibody, which we had shown cross-reacts with E. histolytica Hsp90. For both the extract and the SNX-2112 pulldown, a band of the expected size (81 kDa) was seen with the anti-P. falciparum Hsp90 antibody but not with other inhibitors (Fig. 5).
FIG 4.
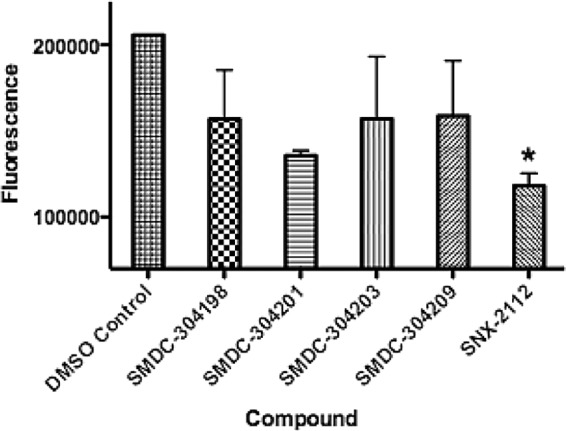
Results of competitive binding assay using the fluorescent ATP analogue bis-ANS. To identify E. histolytica Hsp90-specific inhibitors, bis-ANS was used for binding assay with the E. histolytica Hsp90 ATP-binding domain preincubated in the presence of DMSO or 100 nM Hsp90 inhibitors (SMDC-304198, 304201, 304203, 304209, and SNX-2112). Values represent means and standard errors of the means of duplicate readings. *, P = 0.0187, Student's t test.
FIG 5.
Interaction of Hsp90 inhibitor with E. histolytica protein extract in pulldown assay. Denatured proteins for Hsp90 inhibitor (SMDC-304198, 304201, 304203, 304205, 304209, and SNX-2112) pulldowns and E. histolytica extract were run on a SDS-PAGE gel and immunoblotted with polyclonal anti-Plasmodium falciparum Hsp90 antibody. M indicates protein marker; molecular weights (kDa) are shown to the right.
In vivo efficacy of SNX-5422, a prodrug of SNX-2112, in amebic colitis and giardiasis models.
Because SNX-2112 was found to be selective for binding to the E. histolytica Hsp90 ATP-binding domain and also showed specificity for the E. histolytica Hsp90 protein, we tested the in vivo efficacy of SNX-5422 (Fig. 1), the prodrug of SNX-2112, in mouse models of amebiasis and giardiasis. As the crystalline form of SNX-2112 was not orally bioavailable, we improved the kinetic solubility and bioavailability for oral dosing by using a glycine ester prodrug, SNX-5422, for animal studies (37, 48). The advantage of using SNX-5422 in the mouse models is that full toxicological and pharmacokinetic profiles are available for this compound. The parameters calculated for a single 50 mg/kg dose in female mice were as follows: half-life (t1/2) = 3.3 h, maximum concentration of drug in serum (Cmax) = 4,015 ng/ml, time to Cmax (Tmax) = 2 h, and area under the concentration-time curve to infinity (AUC∞) = 25,153 h · ng/ml (37). No adverse effects related to SNX-5422 were observed for the mice dosed at 50 mg/kg 3 times a week for 3 weeks (37). A single oral dose of 5 mg/kg/day of SNX-5422 for 7 days significantly decreased the burden of E. histolytica compared to the burden in control mice (P = 0.0058) (Fig. 6A). For Giardia infections, mice were treated at the peak of infection, that is, after 5 days of infection; a single oral dose of 10 mg/kg/day for 3 days significantly reduced the number of G. lamblia trophozoites compared to the number in control mice (P = 0.0112), but a single oral dose of 5 mg/kg/day did not have this effect (Fig. 6B).
FIG 6.
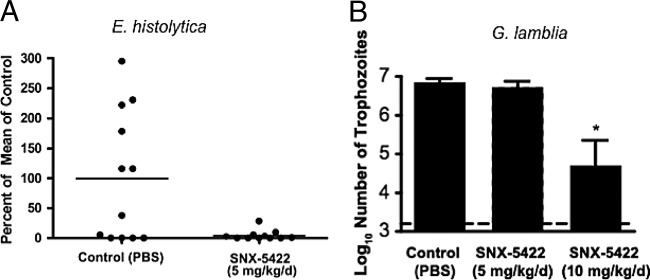
Effect of SNX-5422, the prodrug of Hsp90 inhibitor SNX-2112, in mouse model of amebic colitis and giardiasis. (A) At 24 h postinoculation, mice infected with E. histolytica were administered 5 mg/kg of SNX-5422 or PBS alone (Control) by gavage once a day for 7 days. On day 8, the number of trophozoites/g of tissue was determined by qPCR, and the results are graphed as the percentages of the mean of the control, calculated as the number of trophozoites/g of cecum divided by the mean number of trophozoites in control mice times 100. (B) At 5 days postinoculation, mice infected with G. lamblia were treated once daily with 5 mg/kg and 10 mg/kg of SNX-5422 for 3 days. Control mice received PBS. Error bars show standard errors of the means. The dashed horizontal line represents the detection limit of the assay.
DISCUSSION
In the past decade, pharmacologic inhibition of Hsp90 has received significant attention, and the development of Hsp90 inhibitors as therapeutic agents has progressed rapidly. Currently, at least 13 Hsp90 inhibitors are being evaluated in clinical trials as a treatment for different malignancies (49). Hsp90 inhibitors target the N-terminal domain of Hsp90. Following inhibition, Hsp90 client proteins cannot attain their active conformation, leading to their proteasomal degradation (50, 51). Degradation of these proteins disrupts critical cellular functions, such as cell growth and proliferation, and results in cell death.
Hsp90 is essential for the development of several parasites and is an emerging drug target in parasitic infections. P. falciparum Hsp90 is induced in response to environmental changes following the transit from insect vector to human host and plays a role in the adaptation and survival of the parasite in the human host. P. falciparum Hsp90 may also play a role in the development of drug resistance in the malaria parasite (52). In Leishmania donovani, Hsp90 plays a key role in the differentiation of the promastigote stage to the pathogenic mammalian amastigote stage (31). Hsp90 is also implicated in the development and survival of other intracellular parasites, such as Eimeria tenella (53), Toxoplasma gondii (54), and Trypanosoma cruzi (55). Hsp90 was found to be essential in the filarial nematode Brugia pahangi; exposure of B. pahangi to geldanamycin, a specific inhibitor of Hsp90, killed adult worms and microfilariae in vitro (56, 57). Geldanamycin also inhibited P. falciparum Hsp90 (36), T. gondii Hsp90 (54), and T. cruzi Hsp90 (55), leading to the arrest of parasite growth. But geldanamycin shows hepatotoxicity, is metabolically and chemically unstable, and has very low solubility in aqueous media (58). Therefore, geldanamycin was not pursued for clinical development but, rather, was studied to validate the concept of targeting Hsp90.
Despite Hsp90's importance, research on its role in protozoan parasitic diseases is still in its infancy. Hsp90 function in E. histolytica and G. lamblia was shown to be essential by the inhibition of the growth of E. histolytica and G. lamblia after treatment with the geldanamycin analogue 17-allylamino-17-demethoxygeldanamycin (17-AAG) (59). Recently, using molecular modeling and docking methods, geldanamycin was shown to have binding affinity for E. histolytica Hsp90 (60), indicating that Hsp90 is an attractive molecular target for drug development in E. histolytica and that Hsp90 inhibitors can be used as potential drug candidates. Most drug discovery efforts targeting Hsp90 come from anticancer drug development programs, which we used to obtain compounds to test as antiamebic and antigiardial drugs. Based on a previous study by Huang et al. (37), we hypothesized that primary benzamide and indol-4-one carbonyl groups may bind to the E. histolytica or G. lamblia Hsp90 ATP-binding domain. This scaffold was prioritized over others because of its reported druglike properties, including oral bioavailability and selectivity for binding to Hsp90 (37). We validated our hypothesis by demonstrating the potency of inhibitors containing this scaffold against both parasites (Table 1). Since the benzamide function is known to form important hydrogen bonding interactions in the ATP-binding site of Hsp90s, we also evaluated benzonitrile analogues that lack the crucial hydrogen bond donors. The nitrile derivatives entirely lacked activity against parasites, strongly suggesting that the activity of the benzamides is at least partially due to inhibition of parasite Hsp90.
SNX-5422 has completed a phase I clinical trial in adult patients with recurrent, refractory hematologic malignancies (61). Every-other-day oral dosing of SNX-5422 at 74 mg/m2 for 21 days of a 28-day cycle was found to be well tolerated, and phase II studies are under consideration for patients with multiple myeloma and lymphoma (61). In our study, SNX-5422 showed in vivo efficacy in a mouse model of amebic colitis and giardiasis at single oral daily doses of 5 mg/kg/day for 7 days (Fig. 6A) and 10 mg/kg/day for 3 days (Fig. 6B). This represents a human equivalent dose of 0.4 mg/kg or 0.8 mg/kg, which is 1/5 or less than 1/2 of the dose that was considered well tolerated in the phase I clinical trial (61). Considering the low effective dose and shorter treatment schedule for amebiasis and giardiasis, the Hsp90 inhibitor should be well tolerated by patients suffering from these diseases. Moreover, protozoan Hsp90 differs in biochemical characteristics from Hsp90 of the mammalian host. For example, Hsp90 from P. falciparum exhibits about six times higher ATPase activity than its human counterpart (34, 62). Furthermore, the ATP-binding pocket of E. histolytica Hsp90 may mediate unique ligand interactions, based on the presence of Cys49 and Arg109 relative to the corresponding Ser52 and Lys112 in the human Hsp90 ATP-binding domain. These features can be exploited for future lead optimization.
In conclusion, we have shown that Hsp90 is a viable target for E. histolytica and G. lamblia therapeutics. We also evaluated an Hsp90 inhibitor prodrug (SNX-5422) in animal models for proof of principle that an oral drug could be effective. This study represents a solid starting point for future medicinal chemistry optimizations using Hsp90 inhibitors as therapeutic options for amebiasis and, possibly, for giardiasis.
ACKNOWLEDGMENTS
We thank Potter Wickware for editorial assistance.
This work was supported by NIAID grants 5U01AI077822 and 5U01AI075527, NIH grant DK035108, and the UCSD Digestive Diseases Research Development Center (grant DK080506). A.D. receives support from the Bill and Melinda Gates Foundation.
Footnotes
Published ahead of print 12 May 2014
REFERENCES
- 1.Walsh JA. 1986. Problems in recognition and diagnosis of amebiasis: estimation of the global magnitude of morbidity and mortality. Rev. Infect. Dis. 8:228–238. 10.1093/clinids/8.2.228 [DOI] [PubMed] [Google Scholar]
- 2.Stanley SL., Jr 2003. Amoebiasis. Lancet 361:1025–1034. 10.1016/S0140-6736(03)12830-9 [DOI] [PubMed] [Google Scholar]
- 3.Gardner TB, Hill DR. 2001. Treatment of giardiasis. Clin. Microbiol. Rev. 14:114–128. 10.1128/CMR.14.1.114-128.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laupland KB, Church DL. 2005. Population-based laboratory surveillance for Giardia sp. and Cryptosporidium sp. infections in a large Canadian health region. BMC Infect. Dis. 5:72. 10.1186/1471-2334-5-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoder JS, Beach MJ. 2007. Giardiasis surveillance—United States, 2003-2005. MMWR Surveill. Summ. 56:11–18 [PubMed] [Google Scholar]
- 6.Cifuentes E, Suarez L, Espinosa M, Juarez-Figueroa L, Martinez-Palomo A. 2004. Risk of Giardia intestinalis infection in children from an artificially recharged groundwater area in Mexico City. Am. J. Trop. Med. Hyg. 71:65–70 [PubMed] [Google Scholar]
- 7.Park SK, Kim DH, Deung YK, Kim HJ, Yang EJ, Lim SJ, Ryang YS, Jin D, Lee KJ. 2004. Status of intestinal parasite infections among children in Bat Dambang, Cambodia. Korean J. Parasitol. 42:201–203. 10.3347/kjp.2004.42.4.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Celiksoz A, Acioz M, Degerli S, Cinar Z, Elaldi N, Erandac M. 2005. Effects of giardiasis on school success, weight and height indices of primary school children in Turkey. Pediatr. Int. 47:567–571. 10.1111/j.1442-200x.2005.02110.x [DOI] [PubMed] [Google Scholar]
- 9.Al-Saeed AT, Issa SH. 2006. Frequency of Giardia lamblia among children in Dohuk, northern Iraq. East. Mediterr. Health J. 12:555–561 [PubMed] [Google Scholar]
- 10.Barnawi AB, Tonkal AM, Fouad MA, Al-Braiken FA. 2007. Detection of Entamoeba histolytica/dispar in stool specimens by using enzyme-linked immunosorbent assay in the population of Jeddah City, Saudi Arabia. J. Egypt. Soc. Parasitol. 37:143–150 [PubMed] [Google Scholar]
- 11.de Souza EA, da Silva-Nunes M, dos Santos Malafronte R, Muniz PT, Cardoso MA, Ferreira MU. 2007. Prevalence and spatial distribution of intestinal parasitic infections in a rural Amazonian settlement, Acre State, Brazil. Cad. Saude Publica 23:427–434. 10.1590/S0102-311X2007000200019 [DOI] [PubMed] [Google Scholar]
- 12.Granados CE, Reveiz L, Uribe LG, Criollo CP. 2012. Drugs for treating giardiasis. Cochrane Database Syst. Rev. 12:CD007787. 10.1002/14651858.CD007787.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adam RD. 2001. Biology of Giardia lamblia. Clin. Microbiol. Rev. 14:447–475. 10.1128/CMR.14.3.447-475.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright JM, Dunn LA, Upcroft P, Upcroft JA. 2003. Efficacy of antigiardial drugs. Expert Opin. Drug Saf. 2:529–541. 10.1517/14740338.2.6.529 [DOI] [PubMed] [Google Scholar]
- 15.Savioli L, Smith H, Thompson A. 2006. Giardia and Cryptosporidium join the ‘Neglected Diseases Initiative'. Trends Parasitol. 22:203–208. 10.1016/j.pt.2006.02.015 [DOI] [PubMed] [Google Scholar]
- 16.Freeman CD, Klutman NE, Lamp KC. 1997. Metronidazole. A therapeutic review and update. Drugs 54:679–708 [DOI] [PubMed] [Google Scholar]
- 17.Kanani SR, Knight R. 1972. Experiences with the use of metronidazole in the treatment of non dysenteric intestinal amoebiasis. Trans. R. Soc. Trop. Med. Hyg. 66:244–249. 10.1016/0035-9203(72)90154-X [DOI] [PubMed] [Google Scholar]
- 18.Thacker SB, Simpson S, Gordon TJ, Wolfe M, Kimball AM. 1979. Parasitic disease control in a residential facility for the mentally retarded. Am. J. Public Health 69:1279–1281. 10.2105/AJPH.69.12.1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pehrson PO, Bengtsson E. 1984. A long-term follow up study of amoebiasis treated with metronidazole. Scand. J. Infect. Dis. 16:195–198. 10.3109/00365548409087141 [DOI] [PubMed] [Google Scholar]
- 20.Haque R, Huston CD, Hughes M, Houpt E, Petri WA., Jr 2003. Amebiasis. N. Engl. J. Med. 348:1565–1573. 10.1056/NEJMra022710 [DOI] [PubMed] [Google Scholar]
- 21.Fung HB, Doan TL. 2005. Tinidazole: a nitroimidazole antiprotozoal agent. Clin. Ther. 27:1859–1884. 10.1016/j.clinthera.2005.12.012 [DOI] [PubMed] [Google Scholar]
- 22.Rossignol JF, Ayoub A, Ayers MS. 2001. Treatment of diarrhea caused by Giardia intestinalis and Entamoeba histolytica or E. dispar: a randomized, double-blind, placebo-controlled study of nitazoxanide. J. Infect. Dis. 184:381–384. 10.1086/322038 [DOI] [PubMed] [Google Scholar]
- 23.Cedillo-Rivera R, Tapia-Contreras A, Torres J, Munoz O. 1997. In vitro susceptibility of Entamoeba histolytica to fluoroquinolones, nitrofurans and other antiamebic agents. Arch. Med. Res. 28(Spec No):295–297 [PubMed] [Google Scholar]
- 24.Kapoor K, Chandra M, Nag D, Paliwal JK, Gupta RC, Saxena RC. 1999. Evaluation of metronidazole toxicity: a prospective study. Int. J. Clin. Pharmacol. Res. 19:83–88 [PubMed] [Google Scholar]
- 25.Bendesky A, Menendez D, Ostrosky-Wegman P. 2002. Is metronidazole carcinogenic? Mutat. Res. 511:133–144. 10.1016/S1383-5742(02)00007-8 [DOI] [PubMed] [Google Scholar]
- 26.Sweetman SC. 2002. Martindale: the complete drug reference, 33rd ed. Pharmaceutical Press, London, United Kingdom [Google Scholar]
- 27.Samarawickrema NA, Brown DM, Upcroft JA, Thammapalerd N, Upcroft P. 1997. Involvement of superoxide dismutase and pyruvate:ferredoxin oxidoreductase in mechanisms of metronidazole resistance in Entamoeba histolytica. J. Antimicrob. Chemother. 40:833–840. 10.1093/jac/40.6.833 [DOI] [PubMed] [Google Scholar]
- 28.Wassmann C, Hellberg A, Tannich E, Bruchhaus I. 1999. Metronidazole resistance in the protozoan parasite Entamoeba histolytica is associated with increased expression of iron-containing superoxide dismutase and peroxiredoxin and decreased expression of ferredoxin 1 and flavin reductase. J. Biol. Chem. 274:26051–26056. 10.1074/jbc.274.37.26051 [DOI] [PubMed] [Google Scholar]
- 29.Upcroft P, Upcroft JA. 2001. Drug targets and mechanisms of resistance in the anaerobic protozoa. Clin. Microbiol. Rev. 14:150–164. 10.1128/CMR.14.1.150-164.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salas-Herrera IG, Pearson RM, Johnston A, Turner P. 1991. Concentration of metronidazole in cervical mucus and serum after single and repeated oral doses. J. Antimicrob. Chemother. 28:283–289. 10.1093/jac/28.2.283 [DOI] [PubMed] [Google Scholar]
- 31.Wiesgigl M, Clos J. 2001. Heat shock protein 90 homeostasis controls stage differentiation in Leishmania donovani. Mol. Biol. Cell 12:3307–3316. 10.1091/mbc.12.11.3307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neckers L, Tatu U. 2008. Molecular chaperones in pathogen virulence: emerging new targets for therapy. Cell Host Microbe 4:519–527. 10.1016/j.chom.2008.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sawarkar R, Roy N, Rao S, Raman S, Venketesh S, Suguna K, Tatu U. 2008. Heat shock protein 90 regulates development in Dictyostelium discoideum. J. Mol. Biol. 383:24–35. 10.1016/j.jmb.2008.08.006 [DOI] [PubMed] [Google Scholar]
- 34.Pallavi R, Roy N, Nageshan RK, Talukdar P, Pavithra SR, Reddy R, Venketesh S, Kumar R, Gupta AK, Singh RK, Yadav SC, Tatu U. 2010. Heat shock protein 90 as a drug target against protozoan infections: biochemical characterization of HSP90 from Plasmodium falciparum and Trypanosoma evansi and evaluation of its inhibitor as a candidate drug. J. Biol. Chem. 285:37964–37975. 10.1074/jbc.M110.155317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nageshan RK, Roy N, Hehl AB, Tatu U. 2011. Post-transcriptional repair of a split heat shock protein 90 gene by mRNA trans-splicing. J. Biol. Chem. 286:7116–7122. 10.1074/jbc.C110.208389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Banumathy G, Singh V, Pavithra SR, Tatu U. 2003. Heat shock protein 90 function is essential for Plasmodium falciparum growth in human erythrocytes. J. Biol. Chem. 278:18336–18345. 10.1074/jbc.M211309200 [DOI] [PubMed] [Google Scholar]
- 37.Huang KH, Veal JM, Fadden RP, Rice JW, Eaves J, Strachan JP, Barabasz AF, Foley BE, Barta TE, Ma W, Silinski MA, Hu M, Partridge JM, Scott A, DuBois LG, Freed T, Steed PM, Ommen AJ, Smith ED, Hughes PF, Woodward AR, Hanson GJ, McCall WS, Markworth CJ, Hinkley L, Jenks M, Geng L, Lewis M, Otto J, Pronk B, Verleysen K, Hall SE. 2009. Discovery of novel 2-aminobenzamide inhibitors of heat shock protein 90 as potent, selective and orally active antitumor agents. J. Med. Chem. 52:4288–4305. 10.1021/jm900230j [DOI] [PubMed] [Google Scholar]
- 38.Diamond LS, Harlow DR, Cunnick CC. 1978. A new medium for the axenic cultivation of Entamoeba histolytica and other Entamoeba. Trans. R. Soc. Trop. Med. Hyg. 72:431–432. 10.1016/0035-9203(78)90144-X [DOI] [PubMed] [Google Scholar]
- 39.Buenz EJ. 2007. A high-throughput cell-based toxicity analysis of drug metabolites using flow cytometry. Cell Biol. Toxicol. 23:361–365. 10.1007/s10565-007-0226-1 [DOI] [PubMed] [Google Scholar]
- 40.Debnath A, Parsonage D, Andrade RM, He C, Cobo ER, Hirata K, Chen S, Garcia-Rivera G, Orozco E, Martinez MB, Gunatilleke SS, Barrios AM, Arkin MR, Poole LB, McKerrow JH, Reed SL. 2012. A high-throughput drug screen for Entamoeba histolytica identifies a new lead and target. Nat. Med. 18:956–960. 10.1038/nm.2758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tejman-Yarden N, Miyamoto Y, Leitsch D, Santini J, Debnath A, Gut J, McKerrow JH, Reed SL, Eckmann L. 2013. A reprofiled drug, auranofin, is effective against metronidazole-resistant Giardia lamblia. Antimicrob. Agents Chemother. 57:2029–2035. 10.1128/AAC.01675-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ang KK, Ratnam J, Gut J, Legac J, Hansell E, Mackey ZB, Skrzypczynska KM, Debnath A, Engel JC, Rosenthal PJ, McKerrow JH, Arkin MR, Renslo AR. 2011. Mining a cathepsin inhibitor library for new antiparasitic drug leads. PLoS Negl. Trop. Dis. 5:e1023. 10.1371/journal.pntd.0001023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shahinas D, Liang M, Datti A, Pillai DR. 2010. A repurposing strategy identifies novel synergistic inhibitors of Plasmodium falciparum heat shock protein 90. J. Med. Chem. 53:3552–3557. 10.1021/jm901796s [DOI] [PubMed] [Google Scholar]
- 44.Shahinas D, Folefoc A, Taldone T, Chiosis G, Crandall I, Pillai DR. 2013. A purine analog synergizes with chloroquine (CQ) by targeting Plasmodium falciparum Hsp90 (PfHsp90). PLoS One 8:e75446. 10.1371/journal.pone.0075446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Houpt ER, Glembocki DJ, Obrig TG, Moskaluk CA, Lockhart LA, Wright RL, Seaner RM, Keepers TR, Wilkins TD, Petri WA., Jr 2002. The mouse model of amebic colitis reveals mouse strain susceptibility to infection and exacerbation of disease by CD4+ T cells. J. Immunol. 169:4496–4503. 10.4049/jimmunol.169.8.4496 [DOI] [PubMed] [Google Scholar]
- 46.Melendez-Lopez SG, Herdman S, Hirata K, Choi MH, Choe Y, Craik C, Caffrey CR, Hansell E, Chavez-Munguia B, Chen YT, Roush WR, McKerrow J, Eckmann L, Guo J, Stanley SL, Jr, Reed SL. 2007. Use of recombinant Entamoeba histolytica cysteine proteinase 1 to identify a potent inhibitor of amebic invasion in a human colonic model. Eukaryot. Cell 6:1130–1136. 10.1128/EC.00094-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wassenberg JJ, Reed RC, Nicchitta CV. 2000. Ligand interactions in the adenosine nucleotide-binding domain of the Hsp90 chaperone, GRP94. II. Ligand-mediated activation of GRP94 molecular chaperone and peptide binding activity. J. Biol. Chem. 275:22806–22814. 10.1074/jbc.M001476200 [DOI] [PubMed] [Google Scholar]
- 48.Fadden P, Huang KH, Veal JM, Steed PM, Barabasz AF, Foley B, Hu M, Partridge JM, Rice J, Scott A, Dubois LG, Freed TA, Silinski MA, Barta TE, Hughes PF, Ommen A, Ma W, Smith ED, Spangenberg AW, Eaves J, Hanson GJ, Hinkley L, Jenks M, Lewis M, Otto J, Pronk GJ, Verleysen K, Haystead TA, Hall SE. 2010. Application of chemoproteomics to drug discovery: identification of a clinical candidate targeting hsp90. Chem. Biol. 17:686–694. 10.1016/j.chembiol.2010.04.015 [DOI] [PubMed] [Google Scholar]
- 49.Zagouri F, Sergentanis TN, Chrysikos D, Papadimitriou CA, Dimopoulos MA, Psaltopoulou T. 2013. Hsp90 inhibitors in breast cancer: a systematic review. Breast 22:569–578. 10.1016/j.breast.2013.06.003 [DOI] [PubMed] [Google Scholar]
- 50.Prodromou C, Pearl LH. 2003. Structure and functional relationships of Hsp90. Curr. Cancer Drug Targets 3:301–323. 10.2174/1568009033481877 [DOI] [PubMed] [Google Scholar]
- 51.Chiosis G, Vilenchik M, Kim J, Solit D. 2004. Hsp90: the vulnerable chaperone. Drug Discov. Today 9:881–888. 10.1016/S1359-6446(04)03245-3 [DOI] [PubMed] [Google Scholar]
- 52.Pavithra SR, Kumar R, Tatu U. 2007. Systems analysis of chaperone networks in the malarial parasite Plasmodium falciparum. PLoS Comput. Biol. 3:1701–1715. 10.1371/journal.pcbi.0030168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peroval M, Pery P, Labbe M. 2006. The heat shock protein 90 of Eimeria tenella is essential for invasion of host cell and schizont growth. Int. J. Parasitol. 36:1205–1215. 10.1016/j.ijpara.2006.04.006 [DOI] [PubMed] [Google Scholar]
- 54.Echeverria PC, Matrajt M, Harb OS, Zappia MP, Costas MA, Roos DS, Dubremetz JF, Angel SO. 2005. Toxoplasma gondii Hsp90 is a potential drug target whose expression and subcellular localization are developmentally regulated. J. Mol. Biol. 350:723–734. 10.1016/j.jmb.2005.05.031 [DOI] [PubMed] [Google Scholar]
- 55.Graefe SE, Wiesgigl M, Gaworski I, Macdonald A, Clos J. 2002. Inhibition of HSP90 in Trypanosoma cruzi induces a stress response but no stage differentiation. Eukaryot. Cell 1:936–943. 10.1128/EC.1.6.936-943.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Devaney E, O'Neill K, Harnett W, Whitesell L, Kinnaird JH. 2005. Hsp90 is essential in the filarial nematode Brugia pahangi. Int. J. Parasitol. 35:627–636. 10.1016/j.ijpara.2005.01.007 [DOI] [PubMed] [Google Scholar]
- 57.Taldone T, Gillan V, Sun W, Rodina A, Patel P, Maitland K, O'Neill K, Chiosis G, Devaney E. 2010. Assay strategies for the discovery and validation of therapeutics targeting Brugia pahangi Hsp90. PLoS Negl. Trop. Dis. 4:e714. 10.1371/journal.pntd.0000714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Taldone T, Sun W, Chiosis G. 2009. Discovery and development of heat shock protein 90 inhibitors. Bioorg. Med. Chem. 17:2225–2235. 10.1016/j.bmc.2008.10.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Singh M, Shah V, Tatu U. 2014. A novel C-terminal homologue of Aha1 co-chaperone binds to heat shock protein 90 and stimulates its ATPase activity in Entamoeba histolytica. J. Mol. Biol. 426:1786–1798. 10.1016/j.jmb.2014.01.008 [DOI] [PubMed] [Google Scholar]
- 60.Singh C, Atri N. 2013. Chemo-informatic design of antibiotic geldenamycin analogs to target stress proteins HSP90 of pathogenic protozoan parasites. Bioinformation. 9:329–333. 10.6026/97320630009329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reddy N, Voorhees PM, Houk BE, Brega N, Hinson JM, Jr, Jillela A. 2013. Phase I trial of the HSP90 inhibitor PF-04929113 (SNX5422) in adult patients with recurrent, refractory hematologic malignancies. Clin. Lymphoma Myeloma Leuk. 13:385–391. 10.1016/j.clml.2013.03.010 [DOI] [PubMed] [Google Scholar]
- 62.Roy N, Nageshan RK, Ranade S, Tatu U. 2012. Heat shock protein 90 from neglected protozoan parasites. Biochim. Biophys. Acta 1823:707–711. 10.1016/j.bbamcr.2011.12.003 [DOI] [PubMed] [Google Scholar]