Abstract
Multiple pathogens, such as bacteria, fungi, and viruses, have been frequently found in asthmatic airways and are associated with the pathogenesis and exacerbation of asthma. Among these pathogens, Alternaria alternata (Alt), a universally present fungus, and human rhinovirus have been extensively studied. However, their interactions have not been investigated. In the present study, we tested the effect of Alt exposure on virus-induced airway epithelial immunity using live virus and a synthetic viral mimicker, double-stranded RNA (dsRNA). Alt treatment was found to significantly enhance the production of proinflammatory cytokines (e.g., IL-6 and IL-8) induced by virus infection or dsRNA treatment. In contrast to this synergistic effect, Alt significantly repressed type I and type III IFN production, and this impairment led to elevated viral replication. Mechanistic studies suggested the positive role of NF-κB and mitogen-activated protein kinase pathways in the synergism and the attenuation of the TBK1-IRF3 pathway in the inhibition of IFN production. These opposite effects are caused by separate fungal components. Protease-dependent and -independent mechanisms appear to be involved. Thus, Alt exposure alters the airway epithelial immunity to viral infection by shifting toward more inflammatory but less antiviral responses.
Keywords: Toll-like receptor 3, antiviral, epithelium, Alternaria, rhinovirus
Clinical Relevance
This is the first report about the interaction between two important asthma-associated pathogens. Alteration of the airway epithelial antiviral immunity by fungal exposure may play an important role in the pathogenesis of asthma and its exacerbation. Elucidation of this mechanism will advance our understanding of these complex airway diseases.
The prevalence of asthma has significantly increased in the United States and in other industrialized countries (1). The development of asthma depends on the complicated interactions between genetics and environmental exposures (2). The pathological features of asthma include chronic airway inflammation (mainly type 2 T-helper cells [Th2] type), mucus cell metaplasia (the cause of mucus overproduction), airway remodeling (collage deposition, thickening of the basement membrane, etc.), and bronchial hyperresponsiveness. The prelude of asthma development is usually a repeated environmental allergen exposure and sensitization (3, 4). However, not all allergens can cause asthma (5, 6), and there is no structural similarity among these allergens (7).
Alternaria alternata (Alt) was first found to be the major asthmagenic allergen (or asthmagen) in children raised in arid and semiarid regions (8). A European community respiratory health survey has found that sensitization to fungi (Alt or Cladosporium) was a powerful risk factor for severe asthma in adults (2). A recent National Institute of Environmental Health Sciences study has indicated that Alt exposure in homes throughout the United States was associated with active asthma symptoms (9). Thus, Alt exposure appears to be associated with asthma in children and adults across different demographic regions. Because of the heterogeneous nature of Alt, human exposure to Alt is complicated and may involve many fungal factors, such as proteases, chitin, glucan, and toxins (10–12). Airway epithelium appears to be first to be affected by Alt exposure. Several studies, primarily using cell line models, have found various Alt-induced epithelial responses, such as cytokine transcription (13, 14), secretion (15), ATP release (16), and calcium flux (15–17).
Rhinovirus (RV) is another asthma-related pathogen. It is a small, positive-stranded RNA virus (18). In healthy individuals, RV infection is the major cause of the common cold, which has no effective treatment and imposes great economic burden (18). RV infection also plays a significant role in the development of asthma and in triggering asthma exacerbation. The wheezing illness associated with RV infection during pregnancy is a strong predictor for asthma development (19). In the Childhood Origins of Asthma birth cohort study (20), data have shown that episodes of wheezing associated with RV infections early in life was the most robust predictor of the risk of asthma. The odds ratio for the development of asthma was not further enhanced when wheezing episodes linked to RV and RSV were compared with those due to RV infection alone (20). These data suggest that early-life RV infection significantly increases the risk of asthma development independent of RSV. Asthma exacerbation represents a precipitation of the symptoms in otherwise stable patients with asthma and has been an important credential for the diagnosis of severe asthma. Eighty-five percent of acute asthma exacerbations in children and approximately 60% in adults are associated with the presence of viral infection (21, 22). Among all the viruses, RV is the dominant viral pathogen detected in approximately 60% of viral exacerbations in children and adults (21, 23, 24). Consistently, RV was also the major viral pathogen detected in children and adults hospitalized for asthma exacerbations (25, 26). Thus, besides its critical role in the development of asthma, respiratory RV infection is also the predominant risk factor associated with exacerbations of asthma.
Airway epithelium is the primary infection site of RV (27). Although direct viral particle binding to the cell surface can induce some effects (28), the majority of studies have focused on the replicating virus and its intermediate double-stranded RNA (dsRNA) (29–32). We (29, 32) and others (30, 31) have demonstrated a diverse pathway network (i.e., TLR3, PKR, MDA5/RIG1) that leads to proinflammatory cytokine productions and the IFN-mediated antiviral defense in airway epithelium. Among these pathways, TLR3 is the initial sensor of RV infection, and its activation regulates the activity of RIG1/MDA5 pathways (33). When engaging their cognate ligands, TLR3 dimerize, trigger the recruitment of intracellular proteins, and initiate the signaling via an adaptor protein-TICAM1 (or TRIF) (34). The downstream signaling pathways mediated by TICAM1 include the activation of nuclear factor-κB (NF-κB), extracellular signal–regulated kinase (ERK), p38, and c-Jun N-terminal kinase (JNK), which lead to proinflammatory cytokine production (34). In addition, TLR3-TICAM1 activates the IFN pathway (34). IFN-β and IFN-λ have been linked to the epithelial anti-RV defense reported by us (32) and others (35). The repressed IFN response in asthma, which led to uncontrollable RV replication, has been associated with RV-induced asthma exacerbation (35, 36).
Despite the facts that multiple pathogens are found in asthmatic airways and that host–pathogen interactions (37–39) are important for the development and exacerbation of asthma, almost all recent studies are centered on the single pathogen, which may not reflect the nature of this complex disease. Thus, in the present study, we have made the first attempt to explore the potential interaction between Alt and RV, the two most important pathogens in asthma.
Materials and Methods
Reagents and Expression Constructs
Lyophilized cake of Alternaria filtrates was purchased from GREER (Lenoir, NC) and dissolved in cell culture media to make a 100× stock solution. RV16 stock was amplified and purified, and the titer was determined based on the previous published protocol (40). Synthetic dsRNA was from InvivoGen (San Diego, CA). Protease inhibitor mix was from Sigma (St. Louis, MO). Monoclonal antibody targeting RV16 coat protein was generated as described elsewhere (32). Antibodies targeting phosphorylated (p)-ERK, p-IκBα, and p-IRF3 were purchased from Cell Signaling Technology (Danvers, MA). p-P38 and p-JNK antibodies were from BD Transduction Laboratories (San Jose, CA). Anti-actin antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA). IL-6 and IL-8 ELISA kits were purchased from R&D systems (Minneapolis, MN). The IFN-β ELISA kit was from Invitrogen (Carlsbad, CA). The medium concentration of IL-6 or IL-8 was reported in pg/ml, and IFN was reported in international units/ml (32). TBK1, kinase inactive mutant TBK1 (K38A), and IFN reporter were generous gifts from K. Fitzgerald (University of Massachusetts).
Cell Culture, Alt Exposure, and RV Infection
Human tissues were obtained from the National Disease Research Interchange or from University Medical Center. The University of Arizona Institutional Review Board approved all procedures involved in tissue procurement. Primary airway tracheobronchial epithelial cell cultures were established as described elsewhere (41, 42). Because of the high resistance to viral infection of the well-differentiated airway epithelial cells, monolayered primary cells (mainly basal cells) were used in the study to achieve high viral infection. To account for the donor variation, every experiment involving primary cells was repeated on at least three independent donors. A549 cells were cultivated in RPMI media plus 10% FBS. Alt was first titrated in A549 and primary epithelial cells for the induction of IL-8. The dose of 21.5 μg/ml was found to be the optimal dose. Higher doses of Alt induced cytotoxicity, presumably due to its intrinsic protease activity. Heat-inactivated Alt was prepared by heating Alt stock solution to 70°C for 30 minutes. For protease inactivation, Alt stock was incubated with protease inhibitor mix for 30 minutes. For RV infection, a multiplicity of infection of 10 was used as described elsewhere (32). For the combined treatment, RV/dsRNA and Alt were coincubated with cells for the indicated time points. Immediately before the sample collection (RNA or protein), the cells were thoroughly washed to remove residual RV or Alt.
Real-Time PCR
Real-time PCR was performed as described previously (43). The relative mRNA amount in each sample was calculated based on the ΔΔCt method using housekeeping gene GAPDH. Results were usually calculated as fold induction over control as described previously (29), except for the RV positive-stranded RNA, which was presented in relative viral RNA abundance (32). All primer sequences are listed in Table 1.
Table 1:
Real-Time Primers
| Gene | Primers |
|---|---|
| IFN-β | Forward: ATTGCCTCAAGGACAGGATG; reverse: GCTGCAGCTGCTTAATCTCC |
| IFN-λ1 | Forward: GGACGCCTTGGAAGAGTCACT; reverse: AGAAGCCTCAGGTCCCAATTC |
| RV16 | Forward: GCTGTGCAGTTGGATGTGAT; reverse: AAAGCCATGATGCAATCTCC |
| IL-6 | Forward: GTAGTGAGGAACAAGCCAGAGC; reverse: TCAGGGGTGGTTATTGCATCTA |
| IL-8 | Forward: GCTCTGTGTGAAGGTGCAGTT; reverse: TGTGGTCCACTCTCAATCACTC |
| GAPDH | Forward: CAATGACCCCTTCATTGACC; reverse: GACAAGCTTCCCGTTCTCAG |
Definition of abbreviation: RV, rhinovirus.
Transient Transfection and Dual-Luciferase Reporter Assay
For the dual-luciferase reporter gene assay, cells were transfected with IFN luciferase reporter plus TBK1 or plus TBK1 (K38A) together with the Renilla luciferase expression plasmid pGL4.74 (Rluc/TK) (Promega, Madison, WI). At 24 hours after transfection, the cells were treated with or without Alt for 3 hours and lysed with passive lysis buffer (Promega). Firefly and Renilla luciferase activities were measured with the dual-luciferase reporter assay system (Promega). Firefly luciferase activity was normalized to Renilla luciferase activity. The experiment was performed in triplicate and expressed as mean ± SD.
Western Blot
Total cellular protein was collected based on the methods described previously (29). Equal protein load for total cellular proteins was confirmed using the staining of antiactin antibody.
Statistical Analysis
Experimental groups were compared using a two-sided Student's t test, with significance level set as P < 0.05. When data were not distributed normally, significance was assessed with the Wilcoxon matched-pairs signed-ranks test, and P < 0.05 was considered to be significant.
Results
Alt Enhanced RV-Induced Proinflammatory Cytokines but Repressed RV-Induced IFN Production
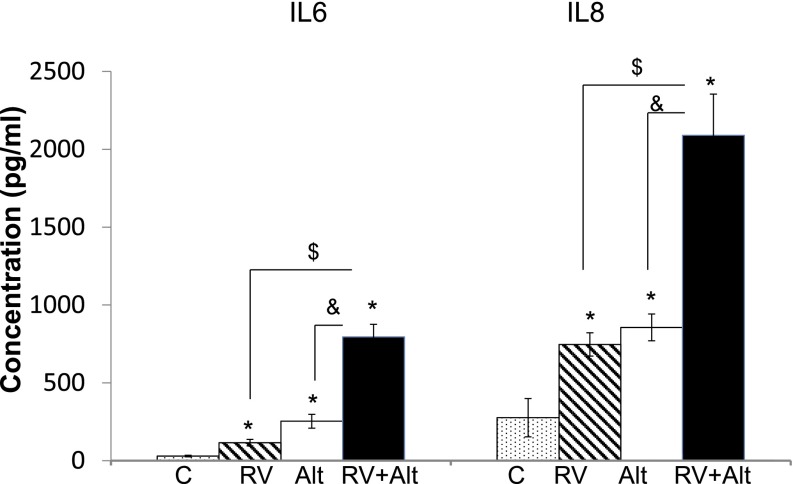
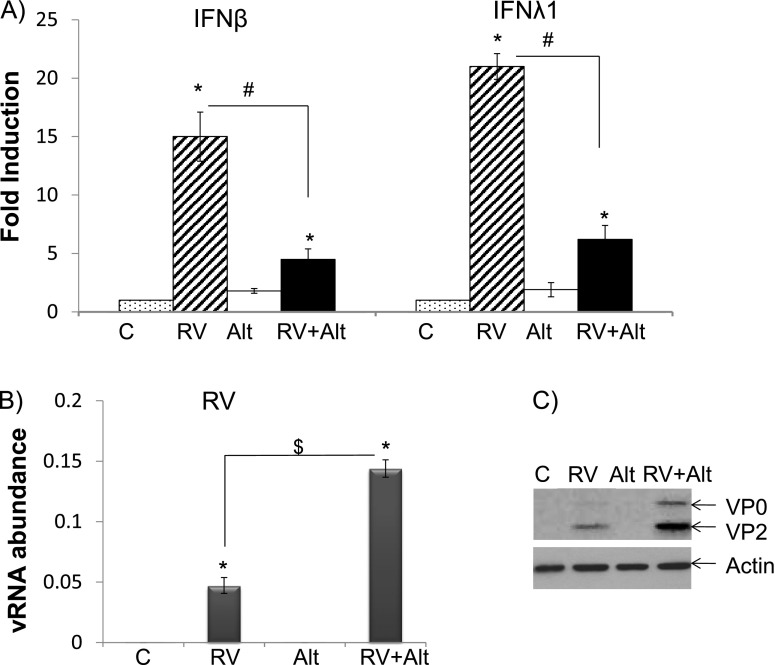
Because airway epithelium is the primary site of Alt exposure and viral infection, we tested if Alt had any effect on RV-induced epithelial signaling. Alt significantly enhanced productions of IL-6 and IL-8 induced by RV infection (Figure 1). IL-6 concentration was 115, 253, 795 pg/ml in the samples of RV infection alone (RV), Alt exposure alone (Alt), and the combined treatment (RV+Alt), respectively, and IL-8 was 746, 856, and 2,089 pg/ml, respectively. Thus, this enhancement was not a merely additive effect; rather, it was a synergistic effect. Alt also strongly repressed gene expression of type I IFN (IFN-β) and type III IFN (IFN-λ1) (Figure 2A). Consistently, this repression led to significant increases of viral RNA (Figure 2B) and coat protein (Figure 2C), suggesting the increase of RV replication and production. Thus, Alt-induced impairment of IFN production appeared to increase the susceptibility of these cells to RV infection.
Figure 1.
Alternaria alternata (Alt) enhanced rhinovirus (RV)-induced cytokine production in epithelial cells. Epithelial cells were infected with RV 16 (multiplicity of infection, 10) and treated with Alt (21.5 μg/ml) individually or in combination. Culture medium was collected 24 hours later and was analyzed by ELISA for IL-6 or IL-8. *P < 0.05 (n = 5) when the treated samples (Alt, RV, or ALT+RV) were compared with the nontreated control (C). $,&P < 0.05 (n = 5) when RV-infected or Alt-treated samples were compared with the samples with cotreatment (RV+Alt).
Figure 2.
Alt repressed RV-induced IFN expression and enhanced RV replication in epithelial cells. Cells were infected with RV 16 and treated with Alt individually or in combination. RNA was collected 24 hours later and was analyzed by real-time PCR. Fold induction of IFN-β and IFN-λ1 (A) or relative abundance of viral RNA (vRNA) (B) were determined. *P < 0.05 (n = 5) when the treated samples (Alt, RV, or Alt+RV) were compared with the control. #P < 0.05 (n = 5) when the samples with cotreatment (RV+Alt) were compared with RV-infected samples. $P < 0.05 (n = 5) when RV-infected samples were compared with the cotreatment (RV+Alt) samples. (C) Cellular protein was collected and analyzed by Western blot. VP0 and VP2 = RV coat protein. Actin was used as a loading control. The image is representative of at least three independent experiments.
Alt Enhanced dsRNA-Induced Proinflammatory Cytokines but Repressed IFN Production
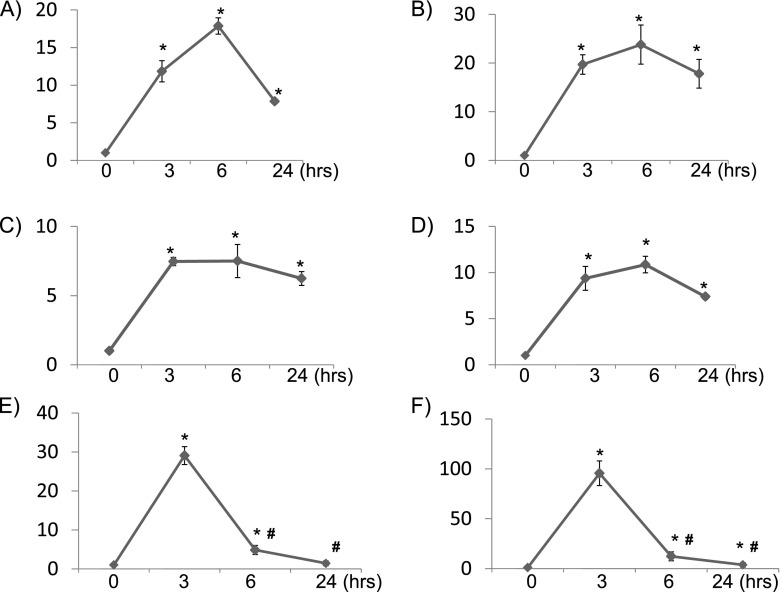
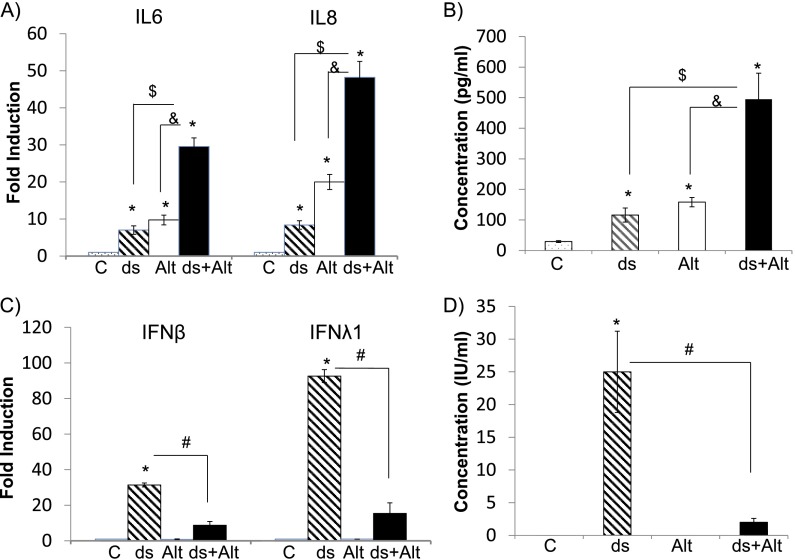
We (29, 32) and others (30, 31) have demonstrated a diverse pathway network (i.e., involving TLR3 and MDA5/RIG1) that mediates epithelial proinflammatory cytokine production and IFN-mediated antiviral defense. Because there is no established ligand for MDA5/RIG1, we tested if Alt affected TLR3 signaling using its specific ligand, dsRNA. First, we tried to define the kinetics of Alt- or dsRNA-induced gene expression. Alt significantly increased the expression of proinflammatory cytokines (e.g., IL-6 and IL-8) (Figures 3A and 3B) but not of any IFN genes (data not shown). The gene expression was significantly elevated at 3 hours, peaked at 6 hours, and then decreased at 24 hours. dsRNA treatment also induced the expression of IL-6 (Figure 3C) and IL-8 (Figure 3D). In contrast to Alt, dsRNA robustly induced the expression of type I (Figure 3E) and III IFN (Figure 3F). The kinetics of IFN elevation were more transient as compared with cytokine induction. Both IFN’s gene expressions peaked at 3 hours, rapidly decreased at 6 hours, and almost completely fell back to the control level at 24 hours. Therfore, we used the early time points (i.e., 3, 6 h) to examine the interaction between Alt and dsRNA at the level of gene expression and used the 6-hour time point for the combined secretory protein level in the media. We found that Alt significantly enhanced dsRNA-induced expression of IL-6 and IL-8 (Figure 4A) but robustly repressed expression of IFN-β and IFN-λ1 (Figure 4C) at 3 hours. The samples from the 6-hour treatment had identical results (data not shown). Consistently, at the protein level, Alt significantly increased dsRNA-induced IL-6 secretion (Figure 4B) while repressing dsRNA-induced IFN-β secretion (Figure 4D). Thus, the opposite effects of Alt on RV-induced epithelial gene expression (Figures 1 and 2) may be mediated by the interactions between the Alt and TLR3 signaling pathways.
Figure 3.
Time course of Alt- or double-stranded RNA (dsRNA)-induced gene expression in epithelial cells. Epithelial cells were treated with Alt (A, B) or dsRNA (C–F) individually. RNA was collected at the indicated time point and was analyzed by real-time PCR. IL-6 (A, C), IL-8 (B, D), IFN-β (E), and IFN-λ1(F) expression was determined. *P < 0.05 (n = 5) when the treated samples (Alt or dsRNA) were compared with the control. #P < 0.05 (n = 5) when dsRNA-treated samples at later time points (i.e., 6 or 24 h) were compared with the samples treated with dsRNA for 3 hours.
Figure 4.
Alt enhanced dsRNA (ds)-induced cytokine production but repressed IFN production in epithelial cells. The cells were treated with ds (25 μg/ml) and/or Alt (21.5 μg/ml) individually or in combination. Real-time PCR was used to determine the expression of proinflammatory cytokines (i.e., IL-6, IL-8) (A) and IFN-β and IFN-λ1 (C). Culture medium was collected and analyzed by ELISA for the secretions of IL-6 (B) or IFN-β (D). *P < 0.05 (n = 5) when the treated samples (Alt, ds, or ds+Alt) were compared with the control. $,&P < 0.05 (n = 5) when ds- or Alt-treated samples were compared with cotreatment (ds+Alt) samples. #P < 0.05 (n = 5) when the samples with cotreatment (ds+Alt) were compared with ds-treated samples.
NF-κB and Mitogen-Activated Protein Kinase Were Involved in the Synergistic Effect of Alt on TLR3 Signaling
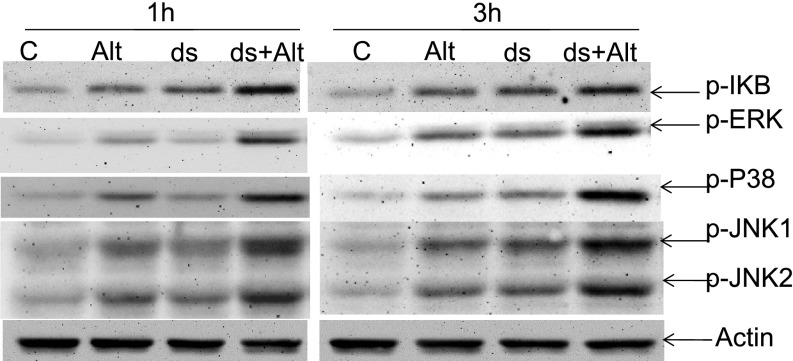
TLR3-mediated proinflammatory cytokine expression has been reported to be regulated by the mitogen-activated protein kinase (MAPK) and NF-κB pathways (44). Either dsRNA or Alt individually activated NF-κB (increased P–I-kappa B) and MAPKs (increased p-ERK, P38, and JNK) (Figure 5). As expected, the combined treatment of dsRNA and Alt further enhanced the activation of these pathways. Thus, the synergism of Alt and dsRNA on the proinflammatory cytokine expression may be mediated by the greater activation of the NF-κB and MAPK pathways by the combined treatment as compared with the individual treatment.
Figure 5.
Alt enhanced ds-activated cellular signaling in epithelial cells. The cells were treated with ds (25 μg/ml) and/or Alt (21.5 μg/ml) individually or in combination (ds+Alt) for the indicated time points, and cellular protein was collected for Western blot analysis. p, phosphorylated. Actin was used as a loading control. The image is representative of at least three independent experiments.
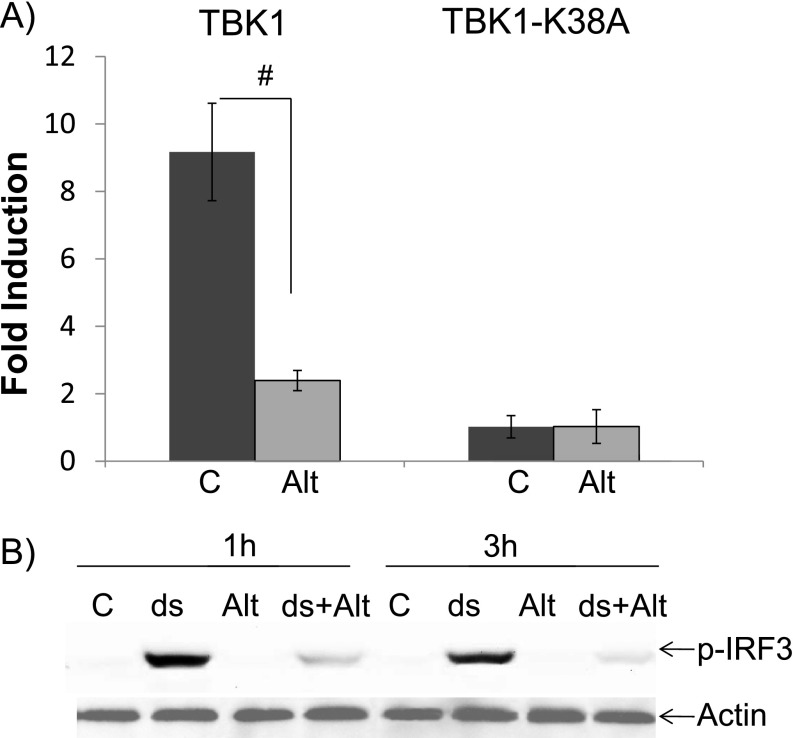
Alt Repressed TBK1-IRF3
IRF3 has been reported to be the key transcriptional factor that drives IFN expression downstream of TLR3 (44). Therefore, we tested TBK1, an upstream kinase of IRF3. In this assay, TBK1 overexpression in airway epithelial cells significantly increased IFN reporter activity, and this activation was repressed when the cells were treated with Alt (Figure 6A). As a negative control, a TBK1 mutant (K38A) was used. This construct contains a point mutation in the catalytic site of TBK1 (Lysine → Alanine) that renders the kinase inactive. As expected, TBK1-K38A failed to activate IFN reporter and did not respond to Alt. Consistently, Alt significantly repressed IRF3 activation, causing a decreased level of p-IRF3 (Figure 6B). Thus, the antagonistic effect of Alt on dsRNA-induced IFN expression appeared to be mediated by its repression of the TBK1-IRF3 pathway.
Figure 6.
Alt repressed TBK1-IRF3. (A) Alt repressed TBK1 activity in airway epithelial cells. Cells were cotransfected with IFN reporter and with TBK1 or its inactive mutant (K38A) as well as Rluc/TK for the normalization of transfection efficiency. At 24 hours after transfection, cells were treated with Alt for 3 hours and lysed for luciferase assay. For luciferase, #P < 0.05 (n = 6). (B) Alt repressed ds-activated IRF3 in epithelial cells. p-IRF3, phosphorylated (activated) IRF3. Actin was used as a loading control.
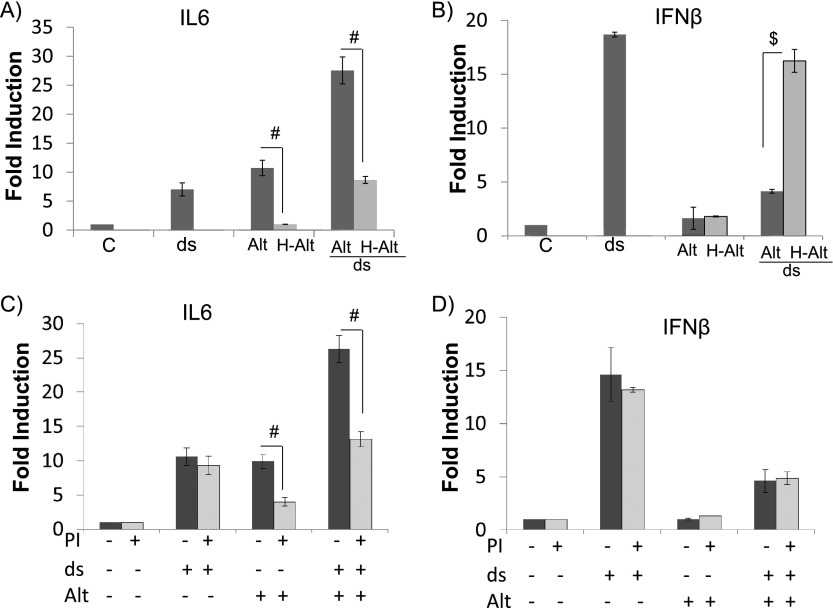
Separate Fungal Components Are Responsible for the Opposite Effects of Alt on the Two Branches of Virus-induced Epithelial Immunity
It has been reported that heat-sensitive fungal proteases are responsible for Alt-induced cytokine expression (13–17). Therefore, we tested if the combined effects of Alt and dsRNA were also heat sensitive and protease dependent. Consistent with the previous reports, heat-inactivated Alt failed to induce IL-6 expression, and its synergism with dsRNA treatment was lost (Figure 7A). In addition, preincubation of protease inhibitor mix with Alt partially abolished Alt-induced IL-6 expression and its synergism with dsRNA (Figure 7C). We had the same observation on IL-8 expression (data not shown). Thus, heat-sensitive, protease-dependent fungal components appeared to be responsible for the Alt-induced proinflammatory cytokine production and its synergism with dsRNA. However, IFN expression had a very different profile (for clarity, only IFN-β data are shown; IFN-λ1 had the same profile). Although heat-inactivated Alt lost the repressing effect on IFN expression (Figure 7B), protease inhibitor treatment had no effect on dsRNA-induced IFN expression (Figure 7D), suggesting that this effect was not caused by the established fungal proteases. Altogether, our data indicate that separate fungal components were responsible for the opposite effects of Alt on the two branches of virus-induced airway epithelial immunity.
Figure 7.
Separate fungal components are involved in the effects of Alt on virus-induced epithelial immunity. The cells were treated with ds (25 μg/ml) or Alt (21.5 μg/ml) individually or in combination for 3 hours, and RNA samples were analyzed by real-time PCR analysis. (A, B) Alt effects were heat sensitive. H-Alt = heat-inactivated Alt. #,$P < 0.05 (n = 5) when Alt-treated samples were compared with H-Alt–treated samples. (C) Alt’s effect on IL-6 expression was protease dependent. Alt was preincubated with protease inhibitor mix (PI) for 30 minutes before the treatments. The same percentage of DMSO (solvent for PI) was added to non-PI samples as the negative control. #P < 0.05 (n = 5). (D) Alt’s effect on IFN-β was protease independent.
Discussion
The precise mechanism underlying the interaction between Alt and virus/dsRNA is unclear. Ligand engagement of TLR3 activates two general branches of signaling pathways: one leads to the production of proinflammatory cytokines, and the other activates IFN transcription (34). A single adaptor protein, TICAM1 (or TRIF), is responsible for these two responses via separate protein domains (44). TRAF6 and RIP1 have been reported to activate TAK1, which further activates the NF-κB pathway. TAK1 also activates MAPK, which in turn leads to the activation of the AP-1 family of transcription factors. NF-κB and AP-1 are key factors driving the transcription of proinflammatory cytokines. An additional adaptor, NAP1, is required to activate TBK1-IKKε, which activates IRF3 (44). In our study, these two branches were affected in the opposite manners. However, the precise targets are unclear.
A large portion of the studies on Alt-induced cellular signaling have centered on protease-dependent pathways (13, 14, 16, 17). Our study confirms this notion by demonstrating that fungal proteases were indeed involved in the induction of proinflammatory cytokines. Furthermore, we have shown that these proteases were responsible for the enhancement of virus-induced cytokine productions by Alt. Because most of the common asthma-causing allergens (e.g., cockroach and house dust mite) have intrinsic protease activities (45, 46) that are associated with the sensitization and asthma development, the synergistic effects between these proteases and RV infection may exacerbate the symptom by markedly enhancing the inflammatory responses in the asthmatic airways. Proteases can induce multiple cellular responses, including the activation of proteinase-activating receptors (47) and receptor tyrosine kinases (48), the generation of reactive oxygen species (49), the disruption of epithelial barrier function (16, 50), and cell death (15, 49). Future study is required to delineate these pathways and to determine how they act individually or in combination with RV infection to promote airway inflammation.
We have also found that Alt represses virus-induced IFN production by a protease-independent mechanism. IFN-dominant Th1 responses are indispensable for the defense against fungal infection (51). Thus, Alt-induced repression of IFN production may represent an adapted response by fungus to survive the attacks from the host defense system. A recent report on the repression of IFN by Alt in dendritic cells (52) supports this notion. Viruses have been well established to evade host defense by compromising the IFN system through various mechanisms (53). However, this area has not been elaborated in the fungal infection/exposure. There are multiple reports on defective virus-induced IFN production in airway epithelial cells (35, 36, 54–56) and in other cell types from patients with asthma (57–61). This IFN defect may lead to uncontrollable viral production and plays a critical role in RV-induced asthma exacerbation (35, 36). Indeed, the defective IFN induction in patients with asthma was associated with greater airway hyperresponsiveness (55). Whether or not Alt is involved in some of these conditions and whether or not other allergens (e.g., cockroach or house dust mite) have IFN-repressing activity is unclear. However, considering the universal presence of Alt across the demographic regions, its IFN-suppressing property may have an important adjuvant effect in the development and exacerbation of asthma when present together with these other allergens.
The present data have to be interpreted with caution for several reasons. First, we used Alternaria filtrates, instead of live fungi, in all the experiments. Despite their wide usage in various previous studies (13–17), the filtrates contain a complex mixture of secretory products from an established fungal culture, and some of these products may reflect specific responses to the artificial in vitro growth environment. Thus, how representative these filtrates are as compared with the real-life Alt exposure is unclear. Nonetheless, the filtrates have been successfully used in a mouse model to generate many bona fide asthma-like pathologies (62), which strongly supports their applicability in asthma research. Second, although Alt is one of major indoor environmental allergens and although RV infection (symptomatic and asymptomatic) is widespread, the degree to which they coexist in the human airway is unclear. It is also likely that persistent exposure to Alt may permanently alter the epithelial antiviral immunity. Further studies in the areas of epidemiology and/or molecular biology are warranted to test these hypotheses. Third, the fungal life cycle has different phases. Filtrates represent the secretory products from a mature fungal growth that may be different from those from the spore germination. Fungal spores have been recently found to activate the TLR3 pathway by gene expression profiling in an epithelial cell line (63). Along this line, Daines and colleagues (64) have reported that fungal spores induced a very different immune response in mice as compared with the filtrates. In these experiments, the mice exposed to the spores had a strong neutrophilic inflammation but a weak IgE production, whereas the mice exposed to the filtrates had classical asthma-like Th2 responses. Thus, further studies are needed to completely understand the agonistic or antagonistic effect of Alt exposure on the epithelial antiviral immunity at different stages of the fungal life cycle.
This is the first attempt to understand the interaction between the two pathogens that are critical to the asthma pathogenesis. Alt exposure affected virus-induced immunity in an imbalanced manner, in which proinflammatory cytokine production was significantly enhanced and IFN production was severely repressed. Complete elucidation of this interaction at molecular level will advance our understanding of the complex nature of asthma and its exacerbation.
Footnotes
The study was supported by National Institutes of Health grant RO1AI061695, a pilot grant from Arizona Biomedical Research Commission, and Clinical a Innovator Award from Flight Attendant Medical Research Institute.
Originally Published in Press as DOI: 10.1165/rcmb.2013-0357OC on January 15, 2014
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Sunyer J, Antó JM, Tobias A, Burney P European Community Respiratory Health Study (ECRHS) Generational increase of self-reported first attack of asthma in fifteen industrialized countries. Eur Respir J. 1999;14:885–891. doi: 10.1034/j.1399-3003.1999.14d26.x. [DOI] [PubMed] [Google Scholar]
- 2.Zureik M, Neukirch C, Leynaert B, Liard R, Bousquet J, Neukirch F European Community Respiratory Health Survey. Sensitisation to airborne moulds and severity of asthma: cross sectional study from European Community respiratory health survey. BMJ. 2002;325:411–414. doi: 10.1136/bmj.325.7361.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Busse WW, Mitchell H. Addressing issues of asthma in inner-city children. J Allergy Clin Immunol. 2007;119:43–49. doi: 10.1016/j.jaci.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 4.Nelson HS, Szefler SJ, Jacobs J, Huss K, Shapiro G, Sternberg AL. The relationships among environmental allergen sensitization, allergen exposure, pulmonary function, and bronchial hyperresponsiveness in the Childhood Asthma Management Program. J Allergy Clin Immunol. 1999;104:775–785. doi: 10.1016/s0091-6749(99)70287-3. [DOI] [PubMed] [Google Scholar]
- 5.Abraham CM, Ownby DR, Peterson EL, Wegienka G, Zoratti EM, Williams LK, Joseph CL, Johnson CC. The relationship between seroatopy and symptoms of either allergic rhinitis or asthma. J Allergy Clin Immunol. 2007;119:1099–1104. doi: 10.1016/j.jaci.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 6.Anthracopoulos MB, Mantzouranis E, Paliatsos AG, Tzavelas G, Lagona E, Nicolaidou P, Priftis KN. Different effects of sensitization to mites and pollens on asthma symptoms and spirometric indices in children: a population-based cohort study. Ann Allergy Asthma Immunol. 2007;99:122–129. doi: 10.1016/S1081-1206(10)60635-7. [DOI] [PubMed] [Google Scholar]
- 7.Chapman MD, Pomés A, Breiteneder H, Ferreira F. Nomenclature and structural biology of allergens. J Allergy Clin Immunol. 2007;119:414–420. doi: 10.1016/j.jaci.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Halonen M, Stern DA, Wright AL, Taussig LM, Martinez FD. Alternaria as a major allergen for asthma in children raised in a desert environment. Am J Respir Crit Care Med. 1997;155:1356–1361. doi: 10.1164/ajrccm.155.4.9105079. [DOI] [PubMed] [Google Scholar]
- 9.Salo PM, Arbes SJ, Jr, Sever M, Jaramillo R, Cohn RD, London SJ, Zeldin DC. Exposure to Alternaria alternata in US homes is associated with asthma symptoms. J Allergy Clin Immunol. 2006;118:892–898. doi: 10.1016/j.jaci.2006.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burge HAHM, Solomon WR, Simmons EG, Gallup J. Quality-control factors for alternaria allergens. Mycotaxon. 1989;34:55–63. [Google Scholar]
- 11.Logrieco ABA, Solfrizzo M, Mule G. Incidence of Alternaria species in grains from Mediterranean countries and their ability to produce mycotoxins. Mycologia. 1990;82:501–505. [Google Scholar]
- 12.Logrieco ABA, Mule G, Moretti A, Perrone G. Epidemiology of toxigenic fungi and their associated mycotoxins for some Mediterranean crops. Eur J Plant Pathol. 2003;109:645–667. [Google Scholar]
- 13.Kouzaki H, O’Grady SM, Lawrence CB, Kita H. Proteases induce production of thymic stromal lymphopoietin by airway epithelial cells through protease-activated receptor-2. J Immunol. 2009;183:1427–1434. doi: 10.4049/jimmunol.0900904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsuwaki Y, Wada K, White T, Moriyama H, Kita H. Alternaria fungus induces the production of GM-CSF, interleukin-6 and interleukin-8 and calcium signaling in human airway epithelium through protease-activated receptor 2. Int Arch Allergy Immunol. 2012;158:19–29. doi: 10.1159/000337756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kouzaki H, Iijima K, Kobayashi T, O’Grady SM, Kita H. The danger signal, extracellular ATP, is a sensor for an airborne allergen and triggers IL-33 release and innate Th2-type responses. J Immunol. 2011;186:4375–4387. doi: 10.4049/jimmunol.1003020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Grady SM, Patil N, Melkamu T, Maniak PJ, Lancto C, Kita H. ATP release and Ca2+ signalling by human bronchial epithelial cells following Alternaria aeroallergen exposure. J Physiol. 2013;591:4595–4609. doi: 10.1113/jphysiol.2013.254649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boitano S, Flynn AN, Sherwood CL, Schulz SM, Hoffman J, Gruzinova I, Daines MO. Alternaria alternata serine proteases induce lung inflammation and airway epithelial cell activation via PAR2. Am J Physiol Lung Cell Mol Physiol. 2011;300:L605–L614. doi: 10.1152/ajplung.00359.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savolainen C, Blomqvist S, Hovi T. Human rhinoviruses. Paediatr Respir Rev. 2003;4:91–98. doi: 10.1016/s1526-0542(03)00030-7. [DOI] [PubMed] [Google Scholar]
- 19.Kotaniemi-Syrjänen A, Vainionpää R, Reijonen TM, Waris M, Korhonen K, Korppi M. Rhinovirus-induced wheezing in infancy: the first sign of childhood asthma? J Allergy Clin Immunol. 2003;111:66–71. doi: 10.1067/mai.2003.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson DJ, Gangnon RE, Evans MD, Roberg KA, Anderson EL, Pappas TE, Printz MC, Lee WM, Shult PA, Reisdorf E, et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson DJ, Johnston SL. The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol. 2010;125:1178–1187; quiz, 1188–1189. doi: 10.1016/j.jaci.2010.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Traves SL, Proud D. Viral-associated exacerbations of asthma and COPD. Curr Opin Pharmacol. 2007;7:252–258. doi: 10.1016/j.coph.2006.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, Anderson LJ, Teague WG. Prevalence of viral respiratory tract infections in children with asthma. J Allergy Clin Immunol. 2007;119:314–321. doi: 10.1016/j.jaci.2006.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kistler A, Avila PC, Rouskin S, Wang D, Ward T, Yagi S, Schnurr D, Ganem D, DeRisi JL, Boushey HA. Pan-viral screening of respiratory tract infections in adults with and without asthma reveals unexpected human coronavirus and human rhinovirus diversity. J Infect Dis. 2007;196:817–825. doi: 10.1086/520816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heymann PW, Carper HT, Murphy DD, Platts-Mills TA, Patrie J, McLaughlin AP, Erwin EA, Shaker MS, Hellems M, Peerzada J, et al. Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezing. J Allergy Clin Immunol. 2004;114:239–247. doi: 10.1016/j.jaci.2004.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Venarske DL, Busse WW, Griffin MR, Gebretsadik T, Shintani AK, Minton PA, Peebles RS, Hamilton R, Weisshaar E, Vrtis R, et al. The relationship of rhinovirus-associated asthma hospitalizations with inhaled corticosteroids and smoking. J Infect Dis. 2006;193:1536–1543. doi: 10.1086/503809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gern JE. The ABCs of rhinoviruses, wheezing, and asthma. J Virol. 2010;84:7418–7426. doi: 10.1128/JVI.02290-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lau C, Wang X, Song L, North M, Wiehler S, Proud D, Chow CW. Syk associates with clathrin and mediates phosphatidylinositol 3-kinase activation during human rhinovirus internalization. J Immunol. 2008;180:870–880. doi: 10.4049/jimmunol.180.2.870. [DOI] [PubMed] [Google Scholar]
- 29.Zhu L, Lee PK, Lee WM, Zhao Y, Yu D, Chen Y. Rhinovirus-induced major airway mucin production involves a novel TLR3-EGFR-dependent pathway. Am J Respir Cell Mol Biol. 2009;40:610–619. doi: 10.1165/rcmb.2008-0223OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Q, Nagarkar DR, Bowman ER, Schneider D, Gosangi B, Lei J, Zhao Y, McHenry CL, Burgens RV, Miller DJ, et al. Role of double-stranded RNA pattern recognition receptors in rhinovirus-induced airway epithelial cell responses. J Immunol. 2009;183:6989–6997. doi: 10.4049/jimmunol.0901386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hewson CA, Jardine A, Edwards MR, Laza-Stanca V, Johnston SL. Toll-like receptor 3 is induced by and mediates antiviral activity against rhinovirus infection of human bronchial epithelial cells. J Virol. 2005;79:12273–12279. doi: 10.1128/JVI.79.19.12273-12279.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen Y, Hamati E, Lee PK, Lee WM, Wachi S, Schnurr D, Yagi S, Dolganov G, Boushey H, Avila P, et al. Rhinovirus induces airway epithelial gene expression through double-stranded RNA and IFN-dependent pathways. Am J Respir Cell Mol Biol. 2006;34:192–203. doi: 10.1165/rcmb.2004-0417OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slater L, Bartlett NW, Haas JJ, Zhu J, Message SD, Walton RP, Sykes A, Dahdaleh S, Clarke DL, Belvisi MG, et al. Co-ordinated role of TLR3, RIG-I and MDA5 in the innate response to rhinovirus in bronchial epithelium. PLoS Pathog. 2010;6:e1001178. doi: 10.1371/journal.ppat.1001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brikos C, O’Neill LAJ.Signalling of toll-like receptors S. Bauer GH.editor. Toll-like receptors (TLRs) and innate immunity.Berlin, GermanySpringer; 200821–50. [Google Scholar]
- 35.Contoli M, Message SD, Laza-Stanca V, Edwards MR, Wark PA, Bartlett NW, Kebadze T, Mallia P, Stanciu LA, Parker HL, et al. Role of deficient type III interferon-lambda production in asthma exacerbations. Nat Med. 2006;12:1023–1026. doi: 10.1038/nm1462. [DOI] [PubMed] [Google Scholar]
- 36.Wark PA, Johnston SL, Bucchieri F, Powell R, Puddicombe S, Laza-Stanca V, Holgate ST, Davies DE. Asthmatic bronchial epithelial cells have a deficient innate immune response to infection with rhinovirus. J Exp Med. 2005;201:937–947. doi: 10.1084/jem.20041901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gavala ML, Bashir H, Gern JE. Virus/allergen interactions in asthma. Curr Allergy Asthma Rep. 2013;13:298–307. doi: 10.1007/s11882-013-0344-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gilstrap DL, Kraft M. Asthma and the host-microbe interaction. J Allergy Clin Immunol. 2013;131:1449–1450,e3. doi: 10.1016/j.jaci.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hansel TT, Johnston SL, Openshaw PJ. Microbes and mucosal immune responses in asthma. Lancet. 2013;381:861–873. doi: 10.1016/S0140-6736(12)62202-8. [DOI] [PubMed] [Google Scholar]
- 40.Wang W, Lee WM, Mosser AG, Rueckert RR. WIN 52035-dependent human rhinovirus 16: assembly deficiency caused by mutations near the canyon surface. J Virol. 1998;72:1210–1218. doi: 10.1128/jvi.72.2.1210-1218.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Y, Zhao YH, Di YP, Wu R. Characterization of human mucin 5B gene expression in airway epithelium and the genomic clone of the amino-terminal and 5′-flanking region. Am J Respir Cell Mol Biol. 2001;25:542–553. doi: 10.1165/ajrcmb.25.5.4298. [DOI] [PubMed] [Google Scholar]
- 42.Wu R, Zhao YH, Chang MM. Growth and differentiation of conducting airway epithelial cells in culture. Eur Respir J. 1997;10:2398–2403. doi: 10.1183/09031936.97.10102398. [DOI] [PubMed] [Google Scholar]
- 43.Kao CY, Chen Y, Thai P, Wachi S, Huang F, Kim C, Harper RW, Wu R. IL-17 markedly up-regulates beta-defensin-2 expression in human airway epithelium via JAK and NF-kappaB signaling pathways. J Immunol. 2004;173:3482–3491. doi: 10.4049/jimmunol.173.5.3482. [DOI] [PubMed] [Google Scholar]
- 44.Vercammen E, Staal J, Beyaert R. Sensing of viral infection and activation of innate immunity by toll-like receptor 3. Clin Microbiol Rev. 2008;21:13–25. doi: 10.1128/CMR.00022-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bessot JC, Pauli G. Mite allergens: an overview. Eur Ann Allergy Clin Immunol. 2011;43:141–156. [PubMed] [Google Scholar]
- 46.Page K. Role of cockroach proteases in allergic disease. Curr Allergy Asthma Rep. 2012;12:448–455. doi: 10.1007/s11882-012-0276-1. [DOI] [PubMed] [Google Scholar]
- 47.Lan RS, Stewart GA, Henry PJ. Role of protease-activated receptors in airway function: a target for therapeutic intervention? Pharmacol Ther. 2002;95:239–257. doi: 10.1016/s0163-7258(02)00237-1. [DOI] [PubMed] [Google Scholar]
- 48.Heijink IH, van Oosterhout A, Kapus A. Epidermal growth factor receptor signalling contributes to house dust mite-induced epithelial barrier dysfunction. Eur Respir J. 2010;36:1016–1026. doi: 10.1183/09031936.00125809. [DOI] [PubMed] [Google Scholar]
- 49.Aoshiba K, Yasuda K, Yasui S, Tamaoki J, Nagai A. Serine proteases increase oxidative stress in lung cells. Am J Physiol Lung Cell Mol Physiol. 2001;281:L556–L564. doi: 10.1152/ajplung.2001.281.3.L556. [DOI] [PubMed] [Google Scholar]
- 50.Vinhas R, Cortes L, Cardoso I, Mendes VM, Manadas B, Todo-Bom A, Pires E, Veríssimo P. Pollen proteases compromise the airway epithelial barrier through degradation of transmembrane adhesion proteins and lung bioactive peptides. Allergy. 2011;66:1088–1098. doi: 10.1111/j.1398-9995.2011.02598.x. [DOI] [PubMed] [Google Scholar]
- 51.Hamad M. Innate and adaptive antifungal immune responses: partners on an equal footing. Mycoses. 2012;55:205–217. doi: 10.1111/j.1439-0507.2011.02078.x. [DOI] [PubMed] [Google Scholar]
- 52.Wada K, Kobayashi T, Matsuwaki Y, Moriyama H, Kita H. Alternaria inhibits double-stranded RNA-induced cytokine production through Toll-like receptor 3. Int Arch Allergy Immunol. 2013;161:75–83. doi: 10.1159/000350365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor KE, Mossman KL. Recent advances in understanding viral evasion of type I interferon. Immunology. 2013;138:190–197. doi: 10.1111/imm.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wark PA, Grissell T, Davies B, See H, Gibson PG. Diversity in the bronchial epithelial cell response to infection with different rhinovirus strains. Respirology. 2009;14:180–186. doi: 10.1111/j.1440-1843.2009.01480.x. [DOI] [PubMed] [Google Scholar]
- 55.Sykes A, Edwards MR, Macintyre J, Del Rosario A, Bakhsoliani E, Trujillo-Torralbo MB, Kon OM, Mallia P, McHale M, Johnston SL. Rhinovirus 16-induced ifn-alpha and ifn-beta are deficient in bronchoalveolar lavage cells in asthmatic patients. J Allergy Clin Immunol. 2012;129:1506–1514,e6. doi: 10.1016/j.jaci.2012.03.044. [DOI] [PubMed] [Google Scholar]
- 56.Edwards MR, Regamey N, Vareille M, Kieninger E, Gupta A, Shoemark A, Saglani S, Sykes A, Macintyre J, Davies J, et al. Impaired innate interferon induction in severe therapy resistant atopic asthmatic children. Mucosal Immunol. 2013;6:797–806. doi: 10.1038/mi.2012.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iikura K, Katsunuma T, Saika S, Saito S, Ichinohe S, Ida H, Saito H, Matsumoto K. Peripheral blood mononuclear cells from patients with bronchial asthma show impaired innate immune responses to rhinovirus in vitro. Int Arch Allergy Immunol. 2011;155:27–33. doi: 10.1159/000327262. [DOI] [PubMed] [Google Scholar]
- 58.Gill MA, Bajwa G, George TA, Dong CC, Dougherty II, Jiang N, Gan VN, Gruchalla RS. Counterregulation between the FcepsilonRI pathway and antiviral responses in human plasmacytoid dendritic cells. J Immunol. 2010;184:5999–6006. doi: 10.4049/jimmunol.0901194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gehlhar K, Bilitewski C, Reinitz-Rademacher K, Rohde G, Bufe A. Impaired virus-induced interferon-alpha2 release in adult asthmatic patients. Clin Exp Allergy. 2006;36:331–337. doi: 10.1111/j.1365-2222.2006.02450.x. [DOI] [PubMed] [Google Scholar]
- 60.Durrani SR, Montville DJ, Pratt AS, Sahu S, DeVries MK, Rajamanickam V, Gangnon RE, Gill MA, Gern JE, Lemanske RF, Jr, et al. Innate immune responses to rhinovirus are reduced by the high-affinity IgE receptor in allergic asthmatic children. J Allergy Clin Immunol. 2012;130:489–495. doi: 10.1016/j.jaci.2012.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bufe A, Gehlhar K, Grage-Griebenow E, Ernst M. Atopic phenotype in children is associated with decreased virus-induced interferon-alpha release. Int Arch Allergy Immunol. 2002;127:82–88. doi: 10.1159/000048173. [DOI] [PubMed] [Google Scholar]
- 62.Doherty TA, Khorram N, Sugimoto K, Sheppard D, Rosenthal P, Cho JY, Pham A, Miller M, Croft M, Broide DH. Alternaria induces STAT6-dependent acute airway eosinophilia and epithelial FIZZ1 expression that promotes airway fibrosis and epithelial thickness. J Immunol. 2012;188:2622–2629. doi: 10.4049/jimmunol.1101632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Babiceanu MC, Howard BA, Rumore AC, Kita H, Lawrence CB. Analysis of global gene expression changes in human bronchial epithelial cells exposed to spores of the allergenic fungus, alternaria alternata. Front Microbiol. 2013;4:196. doi: 10.3389/fmicb.2013.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cunningham A, Pereira RS, Daines M. Differential immune responses to Alternaria alternata components [abstract] Am J Respir Crit Care Med. 2012;185:A5390. [Google Scholar]