Abstract
Background
People with chronic non-communicable diseases (NCD) are particularly vulnerable to socioeconomic inequality due to their long-term expensive health needs. This study aimed to assess socioeconomic-related inequality in health service utilization among NCD patients in China and to analyze factors associated with this disparity.
Methods
Data were taken from the 2008 Chinese National Health Survey, in which a multiple stage stratified random sampling method was employed to survey 56,456 households. We analyzed the distribution of actual use, need-expected use, and need-standardized usage of outpatient services (over a two-week period) and inpatient services (over one-year) across different income groups in 27,233 adult respondents who reported as having a NCD. We used a concentration index to measure inequality in the distribution of health services, which was expressed as HI (Horizontal Inequity Index) for need-standardized use of services. A non-linear probit regression model was employed to detect inequality across socio-economic groups.
Results
Pro-rich inequity in health services among NCD patients was more substantial than the average population. A higher degree of pro-rich inequity (HI = 0.253) was found in inpatient services compared to outpatient services (HI = 0.089). Despite a greater need for health services amongst those of lower socio-economic status, their actual use is much less than their more affluent counterparts. Health service underuse by the poor and overuse by the affluent are evident. Household income disparity was the greatest inequality factor in NCD service use for both outpatients (71.3%) and inpatients (108%), more so than health insurance policies. Some medical insurance schemes, such as the MIUE, actually made a pro-rich contribution to health service inequality (16.1% for outpatient and 12.1% for inpatient).
Conclusions
Inequality in health services amongst NCD patients in China remains largely determined by patient financial capability. The current insurance schemes are insufficient to address this inequity. A comprehensive social policy that encompasses a more progressive taxation package and redistribution of social capital as well as pro-poor welfare is needed.
Background
In recent decades, China has achieved unprecedented success in economic development largely due to market reforms. Unfortunately, the rapid growth of available wealth has not been distributed evenly across the population, resulting in a widening wealth gap between rich and poor and increased disparity in health service utilization. Although people had started to recognize health equality disparities [1], many were astonished when the 2000 Health System Performance Report published by the World Health Organization (WHO) ranked China as one of the lowest three among 191 countries in terms of fairness of health financing. Indeed, in 2001 Chinese people paid 60% of total health expenditure (THE) out of pocket (OOP) [2]. This exacerbated the pre-existing financial obstacles regarding access to health care services, forcing more people, especially those living in poverty [3], to forego much needed medical services. The 2008 National Health Services Survey (NHSS) revealed that among constituents of non-treatment: 10.6% of people did not seek medical attention they needed over a two–week period, 25.1% of people refused inpatient services recommended or prescribed by doctors. Of these two groups, 29.2% and 70.3% refused or avoided treatment due to financial difficulties [4]. Equity of access to healthcare in the Chinese healthcare system has since become a serious concern [5]–[7].
People with chronic non-communicable diseases (NCD) are particularly vulnerable to health inequities due to long-term and often expensive health care needs, compounded by an inability to earn more money. A 2003 study estimated that in China NCD associated costs amounted to $123,548 Billion (USD), which accounted for 71.45% of the financial burden of all diseases and 7.31% of GDP [8]. The burden of NCD was expected to continue to rise [9]. By 2010, the number of patients with diagnosed hypertension in China exceeded 200 million [10], while those with diabetes mellitus numbered 92 million [11]. It was estimated that cardiovascular diseases alone accounts for 41% of all deaths in China [12]. In total, NCD contributed to 80% of deaths and 70% of disability-adjusted life-years (DALYs) lost in China [9]. Previous studies showed that people living with NCD were more susceptible to medical impoverishment [13]. International evidence suggests that people of lower economic status often demonstrate lower rates of access to medical services when compared with those more affluent [14]–[16], especially among those with NCD [17]–[19]. People with NCD often lack access to or eligibility for affordable medical insurance [20], [21]. Consequently, those who do seek medical services have to pay large co-payments, which they can often ill afford, and so compound their socioeconomic status - keeping them in poverty [19], [22], [23].
Previous studies in China have failed to determine the full extent of nation-wide inequality of access to health services [18], [24]. With limited aggregated data, most studies have focused on either regional disparity in relation to a specific service [7], [25]–[29] or income differences in service utilization within a given general population (urban [6], [30]–[33] or rural [18], [34], [35]). We believe that it is likely that inequality of access may have been underestimated by failing to take into account study subjects with and without NCD. People with NCD often require more frequent visits to health facilities in the long term, and are more likely to eschew health services if financial difficulties arise. Unfortunately, there is a paucity of literature documenting inequality in access to health services among NCD patients in China. This study aims to meet this need by determining the degrees of inequality in health services access amongst people with NCD in China, and identifying factors that may be associated with this inequality.
Methods
Data source
The data collected from the 2008 National Health Services Survey (NHSS) were used for this study. The NHSS is one of the most representative health surveys in China organized by the Ministry of Health. It is conducted every five years (in 1993, 1998, 2003 and 2008). The surveys used a questionnaire collecting data in relation to demographic characteristics, income, health status, medical service utilization and medical expenses of those surveyed.
A total of 177,501 questionnaires were completed in the 2008 NHSS, involving 56,456 households across 31 provinces in China. For this study, respondents of 15 years old and over (143,214) were eligible: of these, 27,233, or 19.01% reported having had NCD.
Sampling method
A four-stage stratified random sampling strategy was employed to maximize the representation of the social and economic characteristics of the entire population of China. In the first stage, 94 counties/cities were proportionally and randomly selected, representing five social economic zones. In the second stage, five rural townships in each county and five urban districts in each city were chosen at random. In the third stage, two villages in each rural township and two neighborhoods in each urban district were randomly selected. In the fourth stage, 60 households were randomly selected in each village or neighborhood.
A questionnaire survey was administered via face-to-face interviews with household members. Written informed consent was obtained prior to the survey. For those unable to give informed consent, for example those under 15 years or those with intellectual disability, consent were sought from their next of kin, carers, or parents. The database used in this study contained de-identified data to protect the privacy of participants.
Ethics statement
Ethics clearance was obtained from the Medical Ethics Committee of Harbin Medical University (Da Qing). The authors declare no conflict of interest.
Measurements
Dependent variables
NCD-associated use of services was measured by two binary variables: (1) use (yes or no) of outpatient care over a two week period and (2) use (yes or no) of inpatient care over a 12 month period. Respondents were asked: “Have you received any medical treatment during the last two weeks?” and “Have you been admitted to hospital during the past year?” Those who answered “yes” to the above questions were asked to explain reasons for the treatment or/and hospitalization (including duration of conditions and diagnosis in relation to those conditions). The reported reasons were coded and classified into NCD-associated and non-NCD-associated conditions.
NCD was defined as a chronic medical condition diagnosed by a doctor at least six months before the survey, for which either the symptom(s) persisted or relevant medical treatment continued. In this study, the chronic conditions identified included hypertension, cardiovascular disease, cancer, chronic obstructive pulmonary disease, diabetes mellitus and cerebrovascular disease, which accounted for 88% of all reported NCDs.
Independent and control variables
Health service usage is associated not only with response to disease, age, sex, self-assessed health and limitation of daily activities (need variables), but also with other factors such as socioeconomic status (non-need variables). In this study, we considered household income, education, marital status, occupation, health insurance policies, distance to health facilities, and location of residence as non-need variables.
Age was categorized into five year groups until 65 years. Self-assessed health was measured using a single question on a five-point Likert scale. Limitation of daily activities was measured as “yes” or “no” in relation to the experience of survey participants over the past 12 month prior to the survey. Household income was measured using per capita consumption expenditure and was equally divided into five groups, ranging from the poorest to the richest. Education attainment was measured as the maximum education level attained by the survey participants. Occupation was categorized using the Chinese government standards (student, farmer, worker, self-employed, manager/professional/clerk, unemployed and others). Five major health insurance policies were identified: Free Medical Care (FMC) for governmental officials and senior veterans, Medical Insurance for Urban Employees (MIUE), Medical Insurance for Urban Residents (MIUR), New Cooperative Medical Insurance Scheme (NCMS), and others. The NCMS is an insurance scheme designed specifically for rural residents. By 2008, more than 90% of rural residents had been covered by the NCMS[36]. Participant residence was classified as either eastern (wealthier), middle, or western (poorer) regions. All independent and control variables were coded as dummy variables for further analysis.
Statistical analysis
The World Health Organization defines health equity as “the absence of avoidable or remediable differences among groups of people” [37]. Equality is an aspirational ideal, an equal distribution of access to health services across groups of people. When differential need has been adjusted, an inequality can be interpreted as inequity [38]. A common interpretation of equity in health utilization is that health care ought to be allocated according to health need rather than characteristics of non-need variables, such as income or residence [39]. The conceptual literature on equity in health utilization distinguishes between horizontal and vertical equity. This study is focused on horizontal equity, that is, persons with equivalent need for healthcare ought to have access to treatment irrespective of their socioeconomic status [39].
We calculated distributions of actual use of services, need-expected use of services and need-standardized use of services across income groups. The actual use of services is a factual depiction of the extent of equality (or inequality) in the distribution of services; whereas, the need-expected use of services is a predicted use of services by the "need variables". The gap between “actual use of services” (a) and “need-expected use of services” (b) reflects underuse (if a<b) or overuse (if a>b) of services. However, the combination of the above two measurements does not quantify the extent of inequity. Inequity can be reflected from need-standardized use of services. The aim of the standardization is to determine how the actual distribution of use of services would appear in the absence of differences in the distribution of health need [40]. An unequal distribution in need-standardized use of services can be explained as horizontal inequity because it implies that persons with the same needs are not treated the same.
This study used an indirect standardization method to calculate the distribution of need-standardized use of services. It required estimates of the distribution of the standardizing variables (x) and the variable of interest (y), and the correlation between these variables [40]. A non-linear probit regression model was employed to estimate the need-standardized use of service.
The non-linear regression proceeded by an equation for estimating the actual use of services (yi):
| (1) |
then a linear approximation of this function was given by:
| (2) |
where i denotes the individual; χj are need variables for which we want to standardize; and the  are non-need variables for which we do not want to standardize but to control in the estimation of the
are non-need variables for which we do not want to standardize but to control in the estimation of the  ,
,  are the marginal effects of a set of j need. The
are the marginal effects of a set of j need. The  is an intercept;
is an intercept;  is the implied error term which includes approximation errors [38]; and
is the implied error term which includes approximation errors [38]; and  are the marginal effects of a set of k non-need variables.
are the marginal effects of a set of k non-need variables.
Estimates of the coefficients in (1) were then combined with actual values of the x variables and sample means of the z variables [38] to obtain the distribution of need-expected use of services ( ).
).
| (3) |
Estimates of indirectly need-standardized use of services ( ) were obtained as the difference between actual and x-expected use, plus the mean of predictions (
) were obtained as the difference between actual and x-expected use, plus the mean of predictions ( ).
).
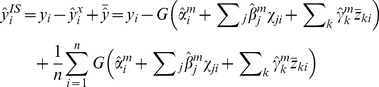 |
(4) |
Where  is the sample size, and we have chosen to set
is the sample size, and we have chosen to set  variables (
variables ( ) to their means, in obtaining the predictions.
) to their means, in obtaining the predictions.
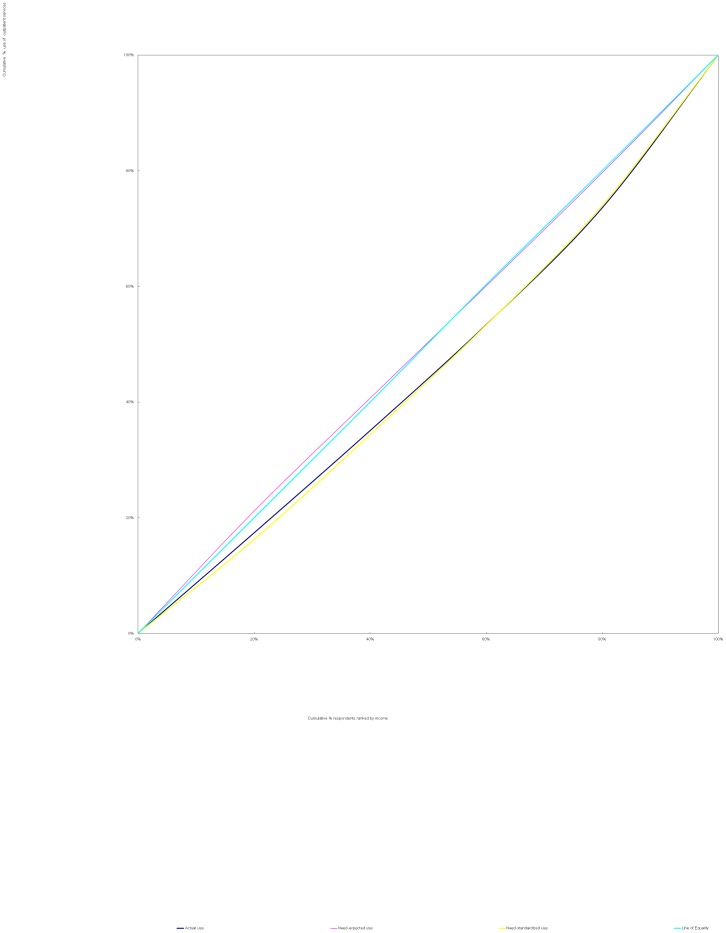
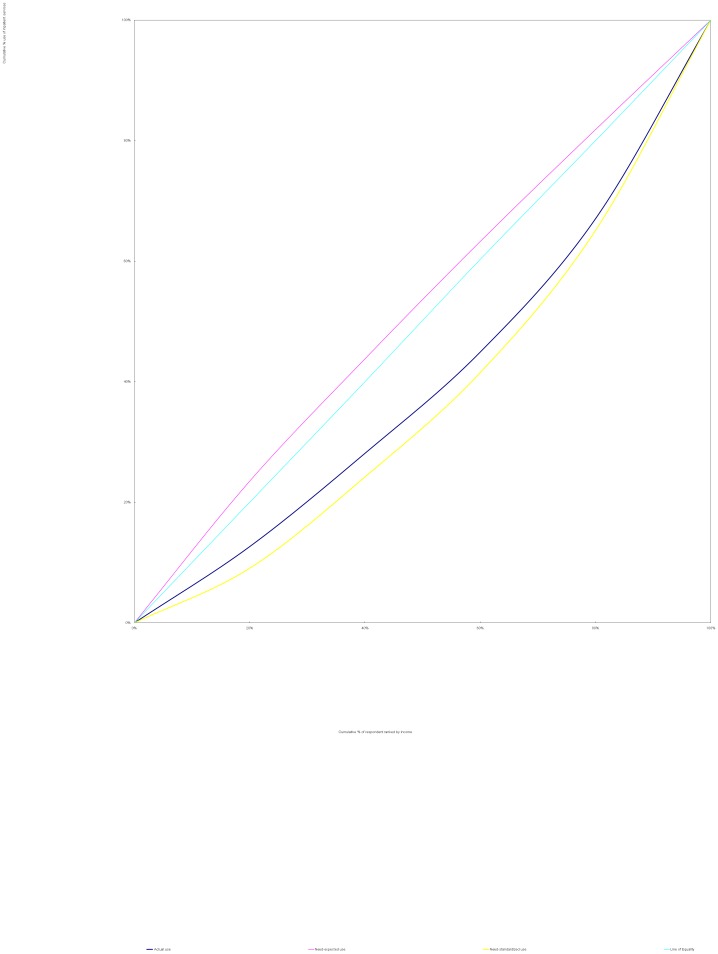
The methods used in this study were identical to those proposed by Wagstaff et al [41]. We used a concentration curve to depict inequality. A concentration curve plots the cumulative percentage of use of services (y-axis) against the cumulative percentage of respondents, ranked by household income, beginning with the least affluent and ending with the most affluent (x-axis). If every person, irrespective of his or her income, has exactly the same use of services, the concentration curve will be a 45 degree line, running from the bottom left-hand corner to the top right-hand corner. This is known as the line of equality. The farther the concentration curve lies from the line of equality, the greater the degree of inequality [42], [43].
We calculated concentration index (CI) to measure socioeconomic inequality in use of services according to Equation (5) [44].
| (5) |
where yi is the measure of actual use of services and Ri is the relative fractional rank (based on weights) of the ith individual which indicates the weighted cumulative proportion of the population up to the midpoint of each individual weight. The µ is the (weighted) mean of use of services and covw denotes the weighted covariance.
The CI was defined as twice the area between the concentration curve and the line of equality, which quantitatively reflects the degree of equality. It lies in the range of -1 to +1, with a negative (positive) value representing inequality in favor of groups with lower (higher) income. Zero indicates that there is no inequality. The greater the absolute value of concentration index, the worse off for the disadvantaged groups of people.
The method proposed by Wagstaff et al. [43] was employed to decompose socioeconomic inequality in use of services into individual determinants. A decomposition analysis estimates how determinants proportionally contribute to inequality in the use of services [44].
Because “use of services” was measured as a binary variable in this study, we applied a nonlinear probit regression model. By using a nonlinear model; however, decomposition can only be made via some linear approximation (a linear approximation to equation (1) is expressed as equation (2). The overall inequalities in use of services (C) is expressed as [43].
where  is the mean of
is the mean of  ;
;  and
and  are the concentration index of
are the concentration index of  and
and  ; and
; and  is the generalized concentration index of the error tem
is the generalized concentration index of the error tem  [43].
[43].
The overall inequality in an outcome contains two components: an explained component and an unexplained component. In the explained component, the impact of each determinant on an outcome is measured by its elasticity ( or
or  ) and the extent of unequal distribution of each determinant across income groups is measured by (CI) [21]. The absolute contribution of each determinant is calculated by multiplying the η and CI with respect to that determinant. An unexplained component is residual which reflects the inequality in health that can't be explained by systematic variation.
) and the extent of unequal distribution of each determinant across income groups is measured by (CI) [21]. The absolute contribution of each determinant is calculated by multiplying the η and CI with respect to that determinant. An unexplained component is residual which reflects the inequality in health that can't be explained by systematic variation.
All analyses were performed with the STATA software version 10.
Results
1. Social demographic characteristics of respondents
Our study subjects (respondents with NCD) had differing social demographic profiles compared with the total adult respondents. On average they were more likely to be older, in poorer health, have a lower level of education, unemployed, divorced or widowed compared to the total adult respondent population (Table 1). However, respondents reporting NCD were slightly more likely to be covered by health insurance than the average of the adult respondents (90.8% vs 88.4%).
Table 1. Social demographic characteristics and healthcare accessibility of respondents.
| Variables | All adult respondents (n = 143,214) | Subjects of study (n = 27,233) | ||
| Number | (%) | Number | (%) | |
| Gender and Age (years) | ||||
| Men * | ||||
| 15–24 | 11,026 | 7.7 | 236 | 0.9 |
| 25–34 | 9,744 | 6.8 | 401 | 1.5 |
| 35–44 | 15,223 | 10.6 | 1,404 | 5.2 |
| 45–54 | 14,010 | 9.8 | 2,618 | 9.6 |
| 55–64 | 10,795 | 7.6 | 3,276 | 12.00 |
| 65- | 9,693 | 6.8 | 4,316 | 15.9 |
| Women * | ||||
| 15–24 | 10,764 | 7.5 | 194 | 0.7 |
| 25–34 | 10,449 | 7.3 | 550 | 2.0 |
| 35–44 | 16,182 | 11.3 | 1,930 | 7.1 |
| 45–54 | 14,324 | 10.0 | 3,460 | 12.7 |
| 55–64 | 10,679 | 7.5 | 3,804 | 14.0 |
| 65- | 10,325 | 7.1 | 5,044 | 18.4 |
| Health Status | ||||
| Limitation of daily Activities * | ||||
| Yes | 7,808 | 5.4 | 5,095 | 18.7 |
| No | 135,406 | 94.6 | 22,138 | 81.3 |
| Self-rated health * | ||||
| Very poor | 478 | 0.3 | 364 | 1.3 |
| Poor | 2,730 | 1.9 | 1,847 | 6.8 |
| Fair | 16,150 | 11.3 | 8,024 | 29.5 |
| Good | 59,950 | 41.9 | 13,533 | 49.7 |
| Excellent | 63,906 | 44.6 | 3,465 | 12.7 |
| Socioeconomic Status | ||||
| Education * | ||||
| Illiterate | 22,107 | 15.4 | 7,222 | 26.5 |
| Primary school | 88,800 | 62.0 | 15,556 | 57.1 |
| Secondary school | 22,927 | 16.0 | 3,195 | 11.8 |
| University | 9,380 | 6.6 | 1,260 | 4.6 |
| Occupation * | ||||
| Student | 9,854 | 6.9 | 120 | 0.4 |
| Unemployed | 21,773 | 15.2 | 6,486 | 23.8 |
| Peasant | 76,224 | 53.2 | 12,246 | 45.0 |
| Worker | 6,079 | 4.2 | 1,904 | 7.0 |
| Self-employed | 8,529 | 6.0 | 1,224 | 4.5 |
| Manager/Professional/Clerk | 18,139 | 12.7 | 4,780 | 17.6 |
| Other | 2,616 | 1.8 | 473 | 1.7 |
| Marital status * | ||||
| Unmarried | 23,243 | 16.2 | 983 | 3.6 |
| Married | 107,462 | 75.0 | 21,487 | 78.9 |
| Divorced/widowed | 12,159 | 8.5 | 4,713 | 17.3 |
| Other | 350 | 0.3 | 50 | 0.2 |
| Household income | ||||
| Quintile I (poorest) | 28,649 | 20.0 | 5,453 | 20.0 |
| Quintile II | 28,957 | 20.2 | 5,451 | 20.0 |
| Quintile III | 28,325 | 19.8 | 5,473 | 20.1 |
| Quintile IV | 28,643 | 20.0 | 5,417 | 19.9 |
| Quintile V (richest) | 28,640 | 20.0 | 5,439 | 20.0 |
| Location of residence * | ||||
| East | 49,466 | 34.5 | 10,269 | 37.7 |
| Middle | 40,424 | 28.2 | 7,718 | 28.3 |
| Western | 53,324 | 37.3 | 9,246 | 34.0 |
| Healthcare Accessibility | ||||
| Insurance scheme * | ||||
| MIUE | 22,106 | 15.4 | 6,268 | 23.0 |
| FMC | 1,674 | 1.2 | 607 | 2.2 |
| MIUR | 5,021 | 3.5 | 846 | 3.1 |
| NCMS | 96,634 | 67.5 | 16,822 | 61.8 |
| Other insurance | 1,137 | 0.8 | 178 | 0.7 |
| No insurance | 16,642 | 11.6 | 2,512 | 9.2 |
| Distance to the nearest health facilities * | ||||
| ≤5 km | 136,146 | 95.1 | 26,056 | 95.7 |
| >5 km | 7,068 | 4.9 | 1,177 | 4.3 |
| Time to the nearest health facilities * | ||||
| ≤30 min | 137,071 | 95.7 | 26,161 | 96.1 |
| >30 min | 6,143 | 4.3 | 1,072 | 3.9 |
| HI of outpatient service (HIo) | 0.017 | 0.089 | ||
| HI of inpatient service (HIi) | 0.207 | 0.253 | ||
| Average Medical Expense Per Outpatient(US$) | 24.3 | 70.4 | ||
| Average Medical Expense Per Inpatient(US$) | 728.3 | 1056.7 |
*p<0.05, compared between the study population (people with NCD) and the average of adult respondents.
MIUE, Medical Insurance for Urban Employees;
FMC, Free Medical Care.
MIUR, Medical Insurance for Urban Residents.
NCMS, New Cooperative Medical Insurance Scheme for Rural Residents.
Respondents with NCD reported more expensive medical costs: their outpatient and inpatient expenses were respectively 2.9 and 1.5 times higher than average. The concentration index for need-standardized use of services (expressed as HI) proved our assumption that people with NCD had a higher degree of inequity in both outpatient services (0.089 vs 0.017) and inpatient services (0.253 vs 0.207) as compared with the average of adult respondents.
2. Distribution of health services
Significant income-related inequality as measured by CI was found in actual, need-expected and need-standardized use of outpatient and inpatient services (p<0.05). There was a pro-poor inequality in need-expected use of services(From Figure 1 and Figure 2, greater need of services from the poor was demonstrated by the lines of need-expected services, which lie above the equality lines), indicating that NCD patients with lower income had greater needs for both outpatient (CN = −0.006) and inpatient (CN = −0.052) services. However, pro-rich inequality in actual and need-standardized use of services (From Figure 1 and Figure 2, both lines of actual use and of need-standardized services lie below the equality lines) was found. Greater CI (inequality) was found for use of inpatient services (CM = 0.201 for actual use; HI = 0.253 for need-standardized use) as compared with outpatient services (CM = 0.083 for actual use; HI = 0.089 for need-standardized use) (Table 2). This indicates that the NCD patients with lower income used less services despite a greater need compared with their richer counterparts, and such inequality was more substantial in inpatient services than in outpatient services. As seen from Figure 1 and Figure 2, the lines of actual use and of need-standardized services for inpatient services lie farther away from the equality lines than those for outpatient services.
Figure 1. Concentration curves for use of outpatient services, China 2008.
The line of need-expected services lie nearer to equality line. Both lines of actual use and of need-standardized services lie below the equality line and almost coincide with each other.
Figure 2. Concentration curves for use of inpatient services, China 2008.
The line of need-expected services lie above the equality line. Both lines of actual use and of need-standardized services lie below the equality line. The line of need-standardized services lie farther away from the equality line than that of actual use.
Table 2. Distribution of actual, need-expected and need-standardized NCD use of outpatient and inpatient services across household income quintiles.
| Household income | Outpatient service use | Inpatient service use | ||||
Actual ( ) ) |
Need–Expected ( ) ) |
Need-Standardized ( ) ) |
Actual ( ) ) |
Need–Expected( ) ) |
Need-Standardized ( ) ) |
|
| Quintile I (Poorest) | 0.089 | 0.109 | 0.084 | 0.043 | 0.081 | 0.031 |
| Quintile II | 0.091 | 0.100 | 0.093 | 0.053 | 0.070 | 0.052 |
| Quintile III | 0.094 | 0.100 | 0.097 | 0.058 | 0.067 | 0.059 |
| Quintile IV | 0.104 | 0.101 | 0.106 | 0.076 | 0.064 | 0.081 |
| Quintile V (Richest) | 0.136 | 0.105 | 0.134 | 0.113 | 0.063 | 0.119 |
| CM/CN/HI | 0.083 | −0.006 | 0.089 | 0.201 | −0.052 | 0.253 |
| SrErr | 0.011 | 0.002 | 0.011 | 0.014 | 0.003 | 0.013 |
| T | 7.69 | −3.75 | 8.42 | 14.72 | −18.64 | 18.96 |
Bold values indicate statistically significance (p<0.05) of the parameters.
CI was expressed as CM for actual use of services; CN for need-expected services; HI (Horizontal Inequity) for need-standardized services.
A 1.5 times gap in actual use of outpatient services between rich and poor appeared, rising from 0.089 for the least affluent to 0.136 for the most affluent. The gap in actual use of inpatient services was even larger (2.6 times), rising from 0.043 for the least affluent to 0.113 for the most affluent. This formed a sharp contrast with the higher expected need of poorer patients. The actual use of inpatient services by the respondents in the lowest income quintile accounted for only 53% of their expected need. Whereas, the actual use of inpatient services by the respondents in the highest income quintile (0.113) was 1.8 times of their expected need (0.063). Obviously, underuse of services by the poor and overuse of services by the rich coexisted (Table 2).
Large income-related inequity was evident as indicated by the distribution of need-standardized use of services. The gap in use of services between the rich and the poor, after adjustment with health need actually increased. A 1.6 times gap (rising from 0.084 for the least affluent to 0.134 for the most affluent) for use of outpatient services and 3.8 times gap (rising from 0.031 for the least affluent and 0.119 for the most affluent) for use of inpatient services was demonstrated (Table 2).
A substantial proportion of respondents with NCD forsook their otherwise needful health services, both outpatient and inpatient. Respondents with lower income were more likely to be influenced by financial difficulties. Almost 22.7% of those in the lowest quintile did not seek medical attention when needed, much higher than the 9.9% of those in the highest quintile. Similarly, 47.8% of those in the lowest quintile refused hospital admissions, much higher than the 28.1% of those in the highest quintile. The denied services were most likely to be associated with financial difficulties, which respectively accounted for 87.4% of the lowest quintile and 59.8% of the highest quintile declined or avoided inpatient services. Meanwhile, 54.5% of the least affluent and 30.6% of the most affluent attributed financial difficulties to their declined outpatient services (Table 3).
Table 3. Reasons for denied inpatient and outpatient services for the NCD patients across income quintiles.
| Quintile of Household living standard | |||||
| I (Poorest) | II | III | IV | V (Richest) | |
| % of denied use of outpatient services (over two-week)* | 22.7% | 18.8% | 12.4% | 10.9% | 9.9% |
| Reasons for not using outpatient services over two weeks (%) | |||||
| Felt minor illness | 30.1 | 34.9 | 49.5 | 43.4 | 47.2 |
| Financial difficulties | 54.5 | 39.6 | 28.9 | 30.2 | 30.6 |
| Lack of time | 2.8 | 1.9 | 4.1 | 3.6 | 3.7 |
| Traffic inconvenience | 0 | 0 | 0 | 0 | 0 |
| Effective treatment not available | 9.1 | 17.9 | 13.4 | 10.8 | 8.3 |
| Other reasons | 3.5 | 5.7 | 4.1 | 12 | 10.2 |
| % of refused hospital admission* | 47.8% | 40.8% | 40.7% | 35.2% | 28.1% |
| Reasons for not using inpatient services over one year (%) | |||||
| Felt not necessary | 4.9 | 7.5 | 8.4 | 17.3 | 15.7 |
| Effective treatment not available | 3.8 | 5.3 | 3 | 4 | 6.1 |
| Financial difficulties | 87.4 | 74.3 | 72.9 | 68.6 | 59.8 |
| Poor hospital services | 0 | 0 | 0 | 0 | 0.3 |
| Lack of time | 2.7 | 2.2 | 10.8 | 4 | 4.1 |
| No beds available | 0 | 0.5 | 0 | 0.7 | 3.2 |
| Other reasons | 1.2 | 10.2 | 4.9 | 5.4 | 10.8 |
| Inpatient reimbursement rates for NCD patients enrolled in insurance schemes (%) | |||||
| Patients Enrolled in NCMS | 39.7 | 27.6 | 31.9 | 26.7 | 25.8 |
| Patients Enrolled in MIUE | 43.9 | 44.1 | 58.7 | 58.7 | 52.2 |
| Patients enrolled in MIUR | 46.7 | 30.5 | 30.9 | 35.4 | 33.9 |
| OOP medical expenditure as a percentage of non-food household expenses (%) | |||||
| Patients Enrolled in NCMS | 40.3 | 35.4 | 28.6 | 21.4 | 29.9 |
| Patients Enrolled in MIUE | 60.0 | 54.3 | 40.7 | 35.9 | 22.9 |
| Patients enrolled in MIUR | 42.6 | 58.6 | 30.9 | 37.4 | 31.8 |
*p<0.01, compared across the five income quintile groups.
Despite high enrolment in health insurance schemes, compensation for medical expenses from those schemes was generally low (Table 3). The reimbursement rate for enrollees of the rural New Cooperative Medical Scheme (NCMS) declined as household income increased, changing from 39.7% for the least affluent to 25.8% for the most affluent. The Medical Insurance for Urban Residents (MIUR) offered a higher reimbursement rate for the least affluent (46.7%) as compared to the most affluent (30.5%–35.4%). However, higher reimbursement rates (52.2%–58.7%) were found for the more affluent enrollees of the Medical Insurance for Urban Employees (MIUE) as compared with their less well off counterparts (43.9%–44.1%).
The NCD patients with low income paid a disproportionally higher amount of medical expenditure out of pocket (OOP) as a percentage of their income. The OOP medical expenditure as a percentage of non-food household expenses declined as household income increased, changing from 40.3% to 29.9% for NCMS enrollees, 60.0% to 22.9% for MIUE enrollees and 42.6% to 31.8% for MIUR enrollees, respectively (Table 3).
3. Factors contributing to income-related inequalities
Income-related inequalities as measured by CI in outpatient and inpatient services were decomposed into contributions of individual determinants, including both need and non-need variables (Table 4). The marginal effect (βk) of each variable was obtained by running regression based on Equation 2, which indicates an association between a particular variable and use of services. Those with a positive sign demonstrate a positive association with use of services, and vice versa. In addition, the larger the absolute value a βk is, the more substantial the association is.
Table 4. Decomposition of income-related inequalities in use of outpatient and inpatient services by need and non-need variables.
| Determinants | Outpatient Services | Inpatient Services | ||
| Marginal effects (βk) | Contribution% | Marginal effects (βk) | Contribution% | |
| Gender and Age | ||||
| Men | ||||
| 15–24 | −0.041 | 0.4% | −0.046 | 0.3% |
| 25–34 | 0.018 | −0.1% | −0.007 | 0.0% |
| 35–44 | 0.124 | 0.6% | −0.005 | 0.0% |
| 45–54 | 0.174 | 7.8% | 0.031 | 0.9% |
| 55–64 | 0.230 | −6.6% | 0.071 | −1.3% |
| 65- | 0.262 | 0.5% | 0.089 | 0.1% |
| Women | ||||
| 15–24 | Reference | |||
| 25–34 | 0.046 | −0.7% | −0.020 | 0.2% |
| 35–44 | 0.110 | 0.5% | −0.015 | 0.0% |
| 45–54 | 0.202 | 8.2% | 0.014 | 0.4% |
| 55–64 | 0.239 | −2.3% | 0.039 | −0.2% |
| 65- | 0.251 | −4.6% | 0.058 | −0.7% |
| Health Status | ||||
| Limitation of daily activities | ||||
| Yes | 0.015 | −2.4% | 0.043 | −4.4% |
| No | Reference | |||
| Self-perceived health | ||||
| Very poor | 0.105 | −0.6% | 0.082 | −0.3% |
| Poor | 0.096 | −1.9% | 0.050 | −0.6% |
| Fair | 0.053 | −5.4% | 0.024 | −1.5% |
| Good | 0.018 | 1.9% | −0.001 | 0.0% |
| Excellent | Reference | |||
| Socioeconomic Status | ||||
| Education | ||||
| Illiterate | Reference | |||
| Primary school | −0.002 | 0.2% | 0.003 | −0.2% |
| Secondary school | −0.011 | −4.7% | −0.002 | −0.5% |
| University | 0.003 | 0.9% | 0.000 | 0.0% |
| Occupation | ||||
| Student | 0.007 | 0.0% | −0.020 | 0.0% |
| Unemployed | Reference | |||
| Peasant | 0.001 | −0.8% | −0.003 | 1.7% |
| Worker | 0.015 | 3.9% | −0.006 | −0.9% |
| Self-employed | 0.019 | 3.1% | −0.015 | −1.5% |
| Manager/Technician/Clerk | 0.011 | 9.1% | −0.007 | −4.0% |
| Other | 0.034 | 0.7% | 0.000 | 0.0% |
| Marital status | ||||
| Unmarried | Reference | |||
| Married | 0.014 | 2.9% | 0.021 | 2.7% |
| Divorced/widow | 0.020 | −3.0% | 0.019 | −1.7% |
| Other | −0.004 | 0.0% | 0.025 | 0.0% |
| Household income | ||||
| Quintile I (Poorest) | Reference | |||
| Quintile II | 0.008 | −7.8% | 0.021 | −11.9% |
| Quintile III | 0.010 | 0.0% | 0.028 | 0.1% |
| Quintile IV | 0.015 | 14.0% | 0.050 | 29.2% |
| Quintile V (Richest) | 0.038 | 71.3% | 0.093 | 108.0% |
| Location of residence | ||||
| East | 0.029 | 19.5% | −0.017 | −7.0% |
| Middle | 0.003 | −0.4% | 0.013 | −1.1% |
| Western | Reference | |||
| Healthcare Accessibility | ||||
| Insurance | ||||
| MIUE | 0.015 | 16.1% | 0.018 | 12.1% |
| FMC | 0.005 | 0.7% | 0.044 | 3.4% |
| MIUR | 0.026 | 0.7% | 0.017 | 0.3% |
| NCMS | 0.021 | −24.3% | 0.015 | −10.7% |
| Other insurance | −0.013 | −0.2% | 0.050 | 0.6% |
| No insurance | Reference | |||
| Shortest distance to health facilities | ||||
| ≤5 km | Reference | |||
| >5 km | −0.027 | 3.0% | −0.001 | 0.1% |
| Time to the nearest health facilities* | ||||
| ≤30 min | Reference | |||
| >30 min | −0.001 | 0.2% | 0.001 | −0.1% |
Bold values indicate statistical significance (p<0.05) of the estimates of marginal effects.
MIUE: Medical Insurance for Urban Employees;
FMC: Free Medical Care;
MIUR: Medical Insurance for Urban Residents;
NCMS: New Cooperative Medical Insurance Scheme for Rural Residents.
Regardless of outpatient and inpatient services, the βk showed that older age and poorer health status were associated with an increased use of services (Table 4). However, those need variables were not able to explain the full extent of inequality. In fact, disparities in household income and access to health insurance schemes were the greatest contributors to the inequality in health services among the NCD patients. A positive value of “% contribution” as shown in Table 4 signifies a contribution in favor of the affluent, while a negative value of “% contribution” indicates a contribution in favor of the poor. Household income made alarmingly high contributions in favor of rich, including 71.3% of pro-rich CI for outpatient services and 108.0% pro-rich CI for inpatient services from the highest quintile of household income. Disparities in access to medical insurance schemes came second in contributing to inequality in health services. Although the NCMS made a pro-poor contribution for both outpatient (−24.3%) and inpatient (−10.7%) services, the other insurance schemes all made a pro-rich contribution (ranging from 0.6% to 12.1%). In addition, residing in eastern regions made a significant (19.5%) pro-rich contribution to use of outpatient service, but a pro-poor (−7.0%) effect on use of inpatient services.
Discussion
Significant income-related inequity in use of health services by people with NCD exists in China. Despite a greater need of the less affluent for health services (Figure 1 and Figure 2), they have been disproportionately deprived of health services due to their socioeconomic situation. This study revealed a 1.6 times gap in outpatient service utilization and a 3.8 times gap in inpatient service utilization between the lowest income quintile and the highest income quintile of people after adjustment due to health need. Only 53% of necessary inpatient services for the poorest were delivered. By contrast, the richest used 1.8 times of need-expected inpatient services. The horizontal inequity indices also indicate a more substantial income-related inequity in inpatient services (HIi = 0.253) compared with outpatient services (HIo = 0.089) (Figure 1 and Figure 2).
This study also proved our hypothesis that health inequality could be underestimated by mixing study subjects with and without NCD. Indeed, the horizontal inequity indices of the people with NCD (HIo = 0.089, HIi = 0.253) are higher than the average of general public (HIo = 0.017, HIi = 0.207).
The levels of horizontal inequity in our study population are higher than those of Thai (HIo = −0.067, HIi = −0.061) [45] and Australia (HIo = 0.019, HIi = −0.083) [46]. More importantly, the Chinese health system still favours the affluent, whereas in Thailand and Australia they have become in favour of the less affluent due to the universal coverage of health care.
The decomposition analysis showed that financial factors have the most significant association with inequality in health services among the people with NCD in China. The pro-rich contributions made by household income were alarmingly high: 71.3% CI for outpatient services and 108.0% CI for inpatient services came from the highest quintile of household income. By 2008, about 90% of Chinese residents had been covered by health insurance [4], [19]. How can financial difficulties still be associated with such significant inequity in health services? First, despite rapid accumulation of social wealth, income gap between the rich and the poor is widening in China at an alarming speed. The income Gini coefficient reached 0.48 in 2008 [47], exceeding the internationally recognized warning level. The most affluent 10% of Chinese families collective wealth was equivalent to 65 times of those at the least affluent 10% in 2008 [48]. Second, despite decades of almost miraculous economic growth due to market-oriented reforms, unfortunately, the Chinese government has failed to ensure equal attention to wealth re-distribution and social insurance and safety net. Without those social protection measures, individuals and families have become a major bearer of financial risks resulted from catastrophic events such as serious diseases. This is not uncommon in a market dominated system. In the USA, for example, 47.6% of inequality in outpatient services is a result from income disparities [49]. Third, the Chinese system has actually resulted in an enlarged gap in ability to pay for health services between the rich and the poor. This study found that the richer people tended to overuse health services, especially the more expensive inpatient services. On the other hand, poorer people tended to underuse health services. Our data demonstrated that 22.7% of the people in the poorest income quintile did not seek medical attention when needed, 54% of which were caused by financial difficulties. Meanwhile, as high as 47.8% of those in the poorest income quintile denied hospital admissions, 87.4% of which were caused by financial difficulties. Finally, insufficient financial investment from both national and provincial governments and fee-for-service payment mechanisms for health providers (and perhaps also the high demand from the affluent) have altered the market equilibrium for medical cost [50], which may in turn compounds the financial difficulties of the poor. In the last three decades, governmental subsidies to public hospitals have been reduced to less than 8% of total revenue of public hospitals [51]. Public hospitals have to rely on user charges for cost recovery [52]. These fee-for-service arrangements encouraged health workers to provide more (but often unnecessary) services [13]. The supplier-induced demand has fuelled the rise of health expenditure and increased the financial burden of consumers. The NCD patients may become the first to feel the burden, because medical expenditure incurred on the NCD patients were 2.9 and 1.5 times of the average for outpatient and inpatient services, respectively.
It has been widely accepted that health insurance can help reduce inequality in use of health services [17], [19], [20]. Our study revealed that health insurance was the second largest determinant of inequality in health services; however, some medical insurance schemes such as the MIUE actually made a pro-rich contribution to the inequality in health services (16.1% for outpatient and 12.1% for inpatient). There are several possible reasons for this. The compensation rate for MIUE enrollees fell short of government expectation (75%) [53]. Our study showed that consumers had to pay about half of medical expenses out of pocket (OOP). The average inpatient medical expenditure for the people with NCD had reached 1672 US$ in 2008 and consumers shared 60% of the charge. The OOP medical payments amounted to 60% of non-food expenses of the household in the poorest quintile, much higher than that of the household in the richest quintile (22.9%). In addition, richer people enjoyed a higher reimbursement rate for inpatient services (52.2%–58.7%) than their poorer counterparts (43.9%–44.1%). These were associated with underuse of inpatient services by the poor and overuse of inpatient services by the rich. Our results showed that the richer people used more inpatient services than what they needed. The actual use of inpatient services by the richest quintile was 0.113, 1.8 times the need-expected (0.063). The overuse of inpatient service by the rich is perhaps also stimulated by the strong focus of the MIUE on hospital services, offering the highest reimbursement rate for inpatient services among all insurance schemes.
Unlike the MIUE, the NCMS made a contribution in favor of the poor (−24.3% for outpatient services and −10.7% for inpatient services). This finding is consistent with studies undertaken by others [54]. The NCMS covered a very large rural population (91.5% of rural residents), with 585 million having their medical bills reimbursed in 2008 [51]. The widespread financial benefits were achieved through a primary care-oriented approach. The NCMS offered higher levels of reimbursement for services in township facilities (40%–50%) than in county hospitals (15%–45%) [23], [55], which encouraged people to seek primary care services closer to their communities. Our data showed that 41.3% of NCMS enrollees chose township facilities for inpatient services for their NCD, resulting in much cheaper bills (The average cost for township facilities was 174.8 US$). The average expenditure for inpatient services was 654 US$ for NCMS enrollees, 1018 US$ less than the average for MIUE enrollees. In addition, the reimbursement policy of NCMS was also in favor of the poor (25.8% for the richest, 39.7% for the poorest). Nevertheless, the overall level of reimbursement of the NCMS was very low (30.8%, lowest in the insurance schemes), which had restricted its role in improving equality in health services.
Serious flaws exist in the design of China's health insurance schemes. Both MIUE and NCMS comprise two components: individual medical saving accounts (IMSA) and social pooling account (SPA). The SPA are intended to cover inpatient costs while the IMSA are to cover outpatient costs and to pay for deductibles in inpatient fee. These multi-tier insurance schemes are inequitable in themselves. In 2008, the per capita fund in the IMSA reached 160 US$ for MIUE enrollees, much higher than the 1.2 US$ for NCMS enrollees [13]. Since NCD patients need life-long medical treatment, the IMSA can only offer very limited assistance because funds in the IMSA are not intended to be shared amongst enrollees. Given this, many NCD patients, especially those from a household with higher income, turned to inpatient services so that they could at least get some compensation from the SPA. But they still faced greater financial hurdles imposed by the OOP payment requirement (deductibles, co-payment requirement and maximum amount of money that the insurance fund would pay for). As a result, the poor have to seek cheaper services and may eventually give up their needed services. Studies have found that rich people are more likely to visit expensive tertiary health facilities than the poor [24], [56], although many of the services are deemed unnecessary and necessary services could be provided in primary care facilities. Unfortunately, services offered in primary care facilities are often deemed to be inappropriate or of poor quality [57], which in turn encourages more people (especially those who can afford) to seek perhaps unnecessary services from tertiary facilities. OOP spending has been believed to be the biggest barrier for reducing urban-rural health service gap [17].
Limitations
There are a few limitations in this study. First, the NHHS is carried out every five years in China. This study has not been able to analyze the most updated progress in recently years of health reform in China. Second, two binary indicators were used for measuring use of outpatient and inpatient services. This can only capture the extensive margin of health service utilization. Further studies are needed to investigate the intensive margin of health service utilization, using indicators in relation to financial burden and quality of services. Third, the NHHS is a cross-sectional survey, which prevents us from making any causal conclusions in the analyses. Some independent variables may be endogenously determined: for example, sicker people who utilize more healthcare services are more likely to be covered by health insurance, and therefore it would be hard to distinguish which factor affects the other. However, Chinese people have very limited choice of health insurance policies. Over 90% of rural residents have been covered by the NCMS. Urban insurance schemes also have strict eligibility criteria and very high coverage in their respective populations. Although empirical evidence shows that household income and insurance policies - the two main factors concerned in this study are likely to affect service use rather than the other way around, we can not exclude the possibility of endogeneity. A potential correlation in both directions of those variables will bias the coefficient estimations and lend weak support to the model for service use inequality measures and decomposition. Finally, the two week short recall period for outpatient service use may result in large measurement errors.
Conclusion
There is strong pro-rich inequality in health services for the Chinese people with NCD. Disproportionately high use of health services by the most affluent coexists with underuse of health services by the least affluent. The income-related horizontal inequity in inpatient services is much higher than that of outpatient services. Disparities in financial capacity and medical insurance entitlement are the two main factors contributing to the pro-rich inequity.
The unusual large share of contribution from financial factors to inequality in health services reflects the widening wealth gap in China and its powerful association with health services. Health policy alone is far from enough to address the inequality issue. A comprehensive social policy that encompasses a more progressive taxation package and redistribution of social wealth as well as pro-poor welfare is needed. This should include a more equitable health insurance program, which extends the pooling of resources to cover all forms of healthcare.
The current financing levels of health insurance schemes are inadequate. The general low insurance benefit level in combination with multi-tier insurance arrangements may actually exacerbate pro-rich inequity in use of health services. The design of the insurance schemes is unable to cater to the real needs of NCD patients, and may encourage NCD patients to use more expensive inpatient services instead of cheaper and more cost effective preventative and primary care.
It is important to develop a mechanism that ensures services are delivered according to the need of consumers, not their ability to pay. There is a need for the government to redirect resources to subsidize the less affluent in the insurance schemes, to increase the percentage of insurance compensation, to encourage primary care through social pooling mechanism for outpatient services, and to eliminate perverse financial incentives for health providers by changing funding instruments. There is a long way to go to achieve the government defined goal of increasing insurance compensation from 52.5% to 75% for MIUE and from 30.8% to 60% for NCMS [53].
Supporting Information
Description of independent and control variables.
(DOCX)
Acknowledgments
We are grateful to all of the people who participated in the 2008 NHHS and Mr. Adamm Ferrier for language editing.
Funding Statement
This work was supported by the Key National Natural Science Fund (71333003) and the China Medical Board (09–979). Website of Key National Natural Science Fund (71333003): http://isisn.nsfc.gov.cn/egrantindex/funcindex/prjsearch-list. Website of China Medical Board (09–979): http://chinamedicalboard.org/grants/evaluation_and_capacity_building_chinas_hospital_reform_pilots-09_979. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Liu Y, Hsiao WC, Eggleston K (1999) Equity in health and health care: the Chinese experience. Social Science & Medicine 49(10): 1349–56. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health (2005) Chinese Health Statistical Digest 2004. Beijing: Ministry of Health.
- 3. Meng Q, Xu L, Zhang Y, Qian J, Cai M, et al. (2012) Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. The Lancet 379(9818): 805–814. [DOI] [PubMed] [Google Scholar]
- 4.Center for Health Statistics and Information of MOH (2009) An Analysis Report of 2008 National Health Services Survey in China. Beijing: Union Medical University Press.
- 5. Gao J, Tang S, Tolhurst R, Rao K (2001) Changing access to health services in urban China: implications for equity. Health Policy & Planning 16(3): 302–12. [DOI] [PubMed] [Google Scholar]
- 6. Luo J, Zhang X, Jin C, Wang D (2009) Inequality of access to health care among the urban elderly in northwestern China. Health Policy 93(2–3): 111–7. [DOI] [PubMed] [Google Scholar]
- 7. Fang P, Dong S, Xiao J, Liu C, Feng X, et al. (2010) Regional inequality in health and its determinants: evidence from China. Health Policy 94(1): 14–25. [DOI] [PubMed] [Google Scholar]
- 8. Hu J, Rao K, Qian J (2007) The study of economic burden of chronic non-communicable diseases in China. Chinese Journal of Prevention and Control of Chronic Diseases(3): 189–193. [Google Scholar]
- 9. Wang L, Kong L, Wu F, Bai Y, Burton R (2005) Preventing chronic diseases in China. The Lancet 366: 1821–1824. [DOI] [PubMed] [Google Scholar]
- 10. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension (2011) 2010 Chinese guidelines for the management of hypertension. Chinese Journal of Hypertension 19(8): 701–743. [Google Scholar]
- 11. Chinese Diabetes Society (2012) China Guideline for Type 2 Diabetes (2010 Edition). Chinese Journal of Diabetes 20(1): 1–37. [Google Scholar]
- 12.Chinese National Center for Cardiovascular Diseases (2011) Report on Cardiovascular Diseases in China (2010). Beijing: Encyclopedia of China Publishing House.
- 13. Yip W, Hsiao W (2009) Non-evidence-based policy: how effective is China's new cooperative medical scheme in reducing medical impoverishment? Social Science & Medicine 68(2): 201–209. [DOI] [PubMed] [Google Scholar]
- 14. Abu-Zaineh M, Mataria A, Moatti JP, Ventelou B (2011) Measuring and decomposing socioeconomic inequality in healthcare delivery: A microsimulation approach with application to the Palestinian conflict-affected fragile setting. Social Science & Medicine 72(2): 133–41. [DOI] [PubMed] [Google Scholar]
- 15. Bago d'Uva T, Jones AM, van Doorslaer E (2009) Measurement of horizontal inequity in health care utilisation using European panel data. Journal of Health Economics 28(2): 280–9. [DOI] [PubMed] [Google Scholar]
- 16. Lu JF, Leung GM, Kwon S, Tin KY, Van Doorslaer E, et al. (2007) Horizontal equity in health care utilization evidence from three high-income Asian economies. Social Science & Medicine 64(1): 199–212. [DOI] [PubMed] [Google Scholar]
- 17. Jian W, Chan KY, Reidpath DD, Xu L (2009) China's rural-urban care gap shrank for chronic disease patients, but inequities persist. Health Affairs 29(12): 2189–96. [DOI] [PubMed] [Google Scholar]
- 18. Jing SS, Yin AT, Meng QY (2010) Study on the Equity of the Health Service Utilization of Rural Chronic Patients. Chinese Health Economics 29(2): 35–37. [Google Scholar]
- 19. Shi W, Chongsuvivatwong V, Geater A, Zhang J, Zhang H, et al. (2010) The influence of the rural health security schemes on health utilization and household impoverishment in rural China: data from a household survey of western and central China. International Journal for Equity in Health 9: 7 10.1186/1475-9276-9-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McGrail KM, van Doorslaer E, Ross NA, Sanmartin C (2009) Income-related health inequalities in Canada and the United States: a decomposition analysis. American Journal of Public Health 99(10): 1856–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shin H, Kim J (2010) Differences in income-related inequality and horizontal inequity in ambulatory care use between rural and non-rural areas: using the 1998–2001 U.S. National Health Interview Survey data. International Journal for Equity in Health 9: 17 10.1186/1475-9276-9-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ma X, Zhang J, Meessen B, Decoster K, Tang X, et al. (2011) Social health assistance schemes: the case of Medical Financial Assistance for the rural poor in four counties of China. International Journal for Equity in Health 10: 44 10.1186/1475-9276-10-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang L, Cheng X, Tolhurst R, Tang S, Liu X (2010) How effectively can the New Cooperative Medical Scheme reduce catastrophic health expenditure for the poor and non-poor in rural China? Tropical Medicine & International Health 15(4): 468–75. [DOI] [PubMed] [Google Scholar]
- 24. Liu S, Griffiths SM (2011) From economic development to public health improvement: China faces equity challenges. Public Health 125(10): 669–74. [DOI] [PubMed] [Google Scholar]
- 25. Chou WL, Wang Z (2009) Regional inequality in China's health care expenditures. Health Economics 2: S137–46 10.1002/hec.1511 [DOI] [PubMed] [Google Scholar]
- 26. Wu Z, Lei P, Hemminki E, Xu L, Tang S, et al. (2012) Changes and equity in use of maternal health care in china: from 1991 to 2003. Maternal & Child Health Journal 16(2): 501–9. [DOI] [PubMed] [Google Scholar]
- 27. Feng XL, Xu L, Guo Y, Ronsmans C (2012) Factors influencing rising caesarean section rates in China between 1988 and 2008. Bulletin of the World Health Organization 90(1): 30–39A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Feng XL, Xu L, Guo Y, Ronsmans C (2011) Socioeconomic inequalities in hospital births in China between 1988 and 2008. Bulletin of the World Health Organization 89(6): 432–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Feng XL, Guo S, Yang Q, Xu L, Zhu J, et al. (2011) Regional disparities in child mortality within China 1996–2004: epidemiological profile and health care coverage. Environmental Health & Preventive Medicine 16(4): 209–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sun P, Unger JB, Palmer P, Ma H, Xie B, et al. (2011) Relative income inequality and selected health outcomes in urban Chinese youth. Social Science & Medicine 74(1): 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xu J, Wu N, Jin S, Wang F, Wang Y, et al. (2010) Analysis of inpatient bed allocation equity and utilization in the city community health service center of China. Journal of Huazhong University of Science and Technology Medical Sciences 30(2): 141–4. [DOI] [PubMed] [Google Scholar]
- 32. Sun X, Rehnberg C, Meng Q (2009) How are individual-level social capital and poverty associated with health equity? A study from two Chinese cities. International Journal for Equity in Health 8: 2 10.1186/1475-9276-8-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liu GG, Zhao Z, Cai R, Yamada T, Yamada T (2002) Equity in health care access to: assessing the urban health insurance reform in China. Social Science & Medicine 55(10): 1779–94. [DOI] [PubMed] [Google Scholar]
- 34. Sun Q, Liu X, Meng Q, Tang S, Yu B, et al. (2009) Evaluating the financial protection of patients with chronic disease by health insurance in rural China. International Journal for Equity in Health 8: 42 10.1186/1475-9276-8-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Anson O, Sun S, Anson O, Sun S (2004) Health inequalities in rural China: evidence from HeBei Province. Health & Place10(1): 75–84. [DOI] [PubMed] [Google Scholar]
- 36. Li Y, Wu Q, Liu C, Kang Z, Xie X, et al. (2014) Catastrophic Health Expenditure and Rural Household Impoverishment in China: What Role Does the New Cooperative Health Insurance Scheme Play? Plos one 9: e93253 10.1371/journal.pone.0093253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization:Health System. Available: http://www.who.int/healthsystems/topics/equity/en/.
- 38. Van Doorslaer E, Koolman X, Jones AM (2004) Explaining income-related inequalities in doctor utilisation in Europe. Health Economics13: 629–647. [DOI] [PubMed] [Google Scholar]
- 39. Wagstaff A, van Doorslaer E, Paci P (1991) On the measurement of horizontal inequity in the delivery of health care. Journal of Health Economics10(2): 169–205. [DOI] [PubMed] [Google Scholar]
- 40.World Bank (2006) Measuring inequity in health service delivery. Quantitative Techniques for Health Equity Analysis PovertyNet, World Bank.
- 41. Wagstaff A, Paci P, van Doorslaer E (1991) On the measurement of inequalities in health. Soc Sci Med 33: 545–557. [DOI] [PubMed] [Google Scholar]
- 42. van Doorslaer E, Jones AM (2003) Inequalities in self-reported health: validation of a new approach to measurement. Journal of Health Economics 22(1): 61–87. [DOI] [PubMed] [Google Scholar]
- 43. Wagstaff A, van Doorslaer E, Watanabe N (2003) On Decomposing the Causes of Health Sector Inequalities with an Application to Malnutrition Inequalities in Vietnam. Journal of Econometrics 112(1): 219–227. [Google Scholar]
- 44. Hosseinpoor AR, Van Doorslaer E, Speybroeck N, Naghavi M, Mohammad K, et al. (2006) Decomposing socioeconomic inequality in infant mortality in Iran. International Journal of Epidemiology 35(5): 1211–9. [DOI] [PubMed] [Google Scholar]
- 45. Somkotra T (2011) Measurement and explanation of horizontal (in)equity in health care utilization among Thais after universal coverage policy implementation. Asia-Pacific Journal of Public Health 23(6): 980–95. [DOI] [PubMed] [Google Scholar]
- 46. Hajizadeh M, Connelly LB, Butler JRG (2012) Health policy and horizontal inequities of health-care utilization in Australia: 1983–2005. Applied Economics Letters 19: 1765–1775. [Google Scholar]
- 47. Hu ZJ, Liu ZM, Gong ZM (2011) Estimation of the Gini Coefficient in China: 1985 –2008. China Economic Quarterly 10(4): 1423–1436. [Google Scholar]
- 48. Wang X (2010) Blocking the “gray hand” of the expansion of the distribution of income gap. Human Resources 8: 51–52. [Google Scholar]
- 49.Van Doorslaer E, Masseria C, OECD Health Equity Research Group (2004) Income-related inequality in the use of medical care in 21 OECD countries. Towards high-performing health systems: policy studies. Paris: OECD, 109–66.
- 50. Hu S, Tang S, Liu Y, Zhao Y, Escobar M, et al. (2008) Reform of how health care is paid for in China: challenges and opportunities. Lancet 370: 1846–1853. [DOI] [PubMed] [Google Scholar]
- 51.Ministry of Health (2010) China health statistics yearbook 2009. Beijing: China Union Medical University Press.
- 52. Ramesh M (2008) Reasserting the role of the state in the healthcare sector: lessons from Asia. Policy and Society 27: 129–136. [Google Scholar]
- 53.State Council (2012) Plans on deepening reform of healthcare system for the "12th Five-Year". Beijing: State Planning and Development Commission.
- 54. Zhou Z, Gao J, Fox A, Rao K, Xu K, et al. (2011) Measuring the equity of inpatient utilization in Chinese rural areas. BMC Health Services Research 11: 201 10.1186/1472-6963-11-201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yu B, Meng Q, Collins C, Tolhurst R, Tang S, et al. (2010) How does the New Cooperative Medical Scheme influence health service utilization? A study in two provinces in rural China. BMC Health Services Research 10(1): 116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu C (2003) Closing the gap between policy and reality: a study of community health services in Chengdu and Panzhihua. Melbourne: La Trobe University.
- 57. Song L, Yan HB, Hu DY, Yang JG, Sun YH (2010) Pre-hospital care-seeking in patients with acute myocardial infarction and subsequent quality of care in Beijing. Chinese Medical Journal 123(6): 664–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of independent and control variables.
(DOCX)