Abstract
INTRODUCTION
Parenting behaviors and family conflict relate to type 1 diabetes outcomes in youth. The purpose of this study was to understand these relationships in parents and youth with type 2 diabetes (T2DM).
METHODS
The TODAY (Treatment Options for type 2 Diabetes in Adolescents and Youth) trial enrolled youth (10-17 years) with recent-onset T2DM and parent/guardian. For this ancillary study, we enrolled a sample of youth-parent pairs (N =137) in one TODAY study arm (metformin plus lifestyle intervention). Parents and youths completed questionnaires to assess parenting style related to normative (e.g., completing homework) and diabetes self-care (e.g., testing blood glucose) tasks, and parent-youth verbal conflict (baseline, 6 and 12 months).
RESULTS
Parenting style was consistent across normative and diabetes tasks, with gradual increases in autonomy perceived by youth. Conversations were generally calm, with greater conflict regarding normative tasks than diabetes tasks at baseline (youth: p<0.001, parent: p=0.01), 6 months (youth: p=0.02, parent: p >0.05) and 12 months (youth: p> 0.05., parent: p=0.05). A permissive parenting style towards normative tasks and a less authoritarian style towards diabetes tasks, at baseline, predicted better medication adherence (8-12 months) (normative: adjusted R2=0.48, p<0.001; diabetes: adjusted R2 = 0.47, p<0.001). Parent-youth conflict did not predict medication adherence.
DISCUSSION
Youth with T2DM who perceive more autonomy (less parental control) in day-to-day and diabetes tasks are more likely to adhere to medication regimens. It may be valuable to assess youth perceptions of parenting style at onset of medication treatment and help parents understand youths’ needs for autonomy.
Keywords: adolescence, parenting style, parent-adolescent relations, type 2 diabetes mellitus, medication adherence
The prevalence of type 2 diabetes mellitus (T2DM) among children and adolescents is a growing problem. A review of global data reports dramatic increases in T2DM in youth (Pinhas-Hamiel & Zeitler, 2005). More recently, analysis of US data from 1999-2010 found a prevalence of diagnosed and undiagnosed T2DM in adolescents of .36%, which the authors describe as a notable increase, although they note limitations in comparisons to earlier data ( Demmer, Zuk, Rosenbaum & Desvarieux, 2013). It is likely that this is related to the increasing prevalence of obesity, as past 30 year data shows an increase in prevalence of obesity from 6.5% to 19.6% in 6 to 11 year old children and from 5% to 18.1% in 12-19 year old youth (Ogden, Carroll, Curtin, Lamb & Flegal, 2008). Management of T2DM is complex, and involves daily medication use, careful attention to diet and increased physical activity. Previous research with adolescents with type 1 diabetes (T1DM) has documented that parenting behaviors and family conflict are related to adolescent adherence to treatment and to glycemic control, and that the transition from diagnosis to treatment is a stressful relational time for youth and their parents (Anderson, 2004; Anderson et al., 2002; Delamater et al., 2001; Miller-Johnson et al., 1994; Rubin, Young-Hyman, & Peyrot, 1989). However, little is known about how family functioning relates to adherence to treatment for youth with T2DM.
The Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study was a multi-center clinical trial designed to evaluate the efficacy of three treatment regimens (metformin alone, metformin plus rosiglitazone, metformin plus intensive lifestyle intervention) for youth with recent-onset T2DM (< 2 years since diagnosis). The primary outcome of TODAY was “time to treatment failure,” i.e., the time that elapses during which the youth is treated (with medications and/or lifestyle change) successfully, before the treatment “fails.” Failure was defined as the youth demonstrating a glycated hemoglobin level of at least 8% for 6 months or persistent metabolic decompensation (TODAY Study Group, 2007). (See TODAY Study Group, 2012 for results of this larger trial.)
The TODAY study provided a unique opportunity to explore the relationship of family dynamics to adherence to medication for youth with T2DM because all youth were enrolled with a parent or guardian closely involved in his/her daily activities. (TODAY Study Group, 2007; TODAY Study Group, 2010; TODAY Study Group, 2011) [Because 89% were parents, we use the term “parent” to include both parents and guardians in this paper.] We examined two salient aspects of family relationships in youth-parent dyads, parenting style (Baumrind, 1967; Baumrind, 1978) and parent-youth conflict (Anderson, 2004; Steinberg & Silverberg, 1987).
Our hypotheses were: (1) An authoritative parenting style (parent negotiates the task with the youth, but parent has final say) towards youth normative tasks (e.g., homework, chores) and diabetes-self-care tasks (e.g., diet, exercise) will be associated with better adherence to medication compared to an authoritarian or permissive parenting style; (2) Greater youth-parent conflict around completion of normative and diabetes-self care tasks will be associated with poorer medication adherence.
METHODS
Participants
The TODAY study enrolled 699 participants across 15 clinical sites. Staff at all sites was invited to participate in the ancillary study. Eight of these sites, representing a broad geographic area, accepted the invitation to participate in this ancillary study (Baylor College of Medicine-Houston, Case Western Reserve School of Medicine-Cleveland, Children's Hospital of Los Angeles, University of Colorado – Denver, Oklahoma University Health Sciences Center-Oklahoma City, University of Texas Health Sciences Center- San Antonio, Saint Louis University, and SUNY Upstate Medical University-Syracuse, NY). Youth-parent dyads were recruited from the “metformin + intensive lifestyle change intervention” arm of TODAY. Only youth from this single arm were included because this ancillary study required that the TODAY study supervising psychologists coordinate the study, e.g., obtain consent. The psychologists were only actively involved in this arm (because of their behavioral expertise). All youth were obese, had T2DM of less than 2 years duration, and were 10-17 years old at the time of randomization to the main study. Participation in this ancillary study was voluntary and distinct from participation in the overall TODAY study.
Procedures
For this ancillary study, TODAY participants were approached at a TODAY study visit by a research staff member and invited to participate in the ancillary study we are reporting here. All participants provided informed consent (and assent) for the ancillary study. They then completed the study questionnaires (see Measures). These self-report questionnaires were completed independently by the parent and youth at the time of randomization into the main TODAY study (baseline), and after 6 and 12 months of TODAY participation at a regularly scheduled TODAY assessment visit. Questionnaires were completed in the participant's primary language (English or Spanish). This study was approved by the Institutional Review Boards for the Protection of Human Subjects for each site.
Measures
Parenting Style
Parenting style was assessed with a modified version of the Behavioral Autonomy Scale (Steinberg & Silverberg, 1987). The measure is based upon Baumrind's typology (Baumrind, 1991). The classification scheme has a long history of empirical work documenting that patterns of parental authority are related to adolescent behavior (Maccoby & Martin, 1983). The 17-item scale measures parenting style relative to normative adolescent responsibilities, i.e., curfew, completing homework, friends, leisure time and chores. Fourteen diabetes-related self-care tasks were added, adapted from Johnson (Johnson, Silverstein, Rosenbloom, Carter, & Cunningham, 1986). Youth and parents answered whether: the parent tells the youth to complete the task (authoritarian parenting style), the parent negotiates the task with the youth and parent has final say (authoritative parenting style), or the parent leaves the decision up to the youth (permissive parenting style), this continuum reflects increasing youth autonomy. Scores were calculated for each individual, for both the normative and diabetes domains, by summing the number of items in each of the three categories and converting the total to a proportion of the total number of items. The internal consistency (i.e., relationship of items to each other, a measure of reliability) of the original measure was 0.78. The internal consistency of the adapted questionnaire as calculated in this study is 0.81 for normative task items and 0.88 for diabetes self-care task items, considered to be a “good” level of reliability.
Parent-Youth Conflict
Parent-youth conflict around normative and diabetes tasks was assessed with the Discussions at Home Scale, adapted from the revised Issues Checklist (Prinz, Foster, Kent, & O'Leary, 1979; Robin & Foster, 1984). It has 37 items and measures the intensity and frequency of discussions associated with normative and diabetes-related tasks. The parent and youth independently recall discussions, and indicate whether the issue has been discussed in the previous two weeks. For each topic discussed, he/she rates the intensity of the discussions (5-point scale, 1 = very calm, 5 = very angry). The summary score is the mean anger-intensity level of each endorsed item. The internal consistency of the adapted questionnaire as calculated in this study is 0.84 regarding normative task items and 0.82 regarding diabetes self-care task items.
Medication Adherence
Adherence to medication was determined by nurses counting pills in blister packs that were dispensed at each medical visit and returned at the next medical visit. Counts for months 2, 4, and 6 were averaged and are reported as “percent of pills taken over the first 6 months” and the average of counts for months 8, 10, and 12 are reported as “percent of pills taken over the second 6 months.”
Statistical Analyses
Data analyses, using SPSS, included calculations of means and standard deviations for continuous variables, frequencies for categorical variables, and paired t-tests or repeated measures analysis of variance (ANOVA) to assess changes over time. Multivariable analysis of covariance (ANCOVA) was used to identify factors that might predict medication adherence over the second 6 months, controlling for adherence during the first 6 months of the ancillary study. The ANCOVA statistical models were constructed based on preliminary analyses that assessed the significance of variables that might affect adherence, including the percentages of each baseline parenting style of both normative and diabetes tasks, the mean tone of youth-parent interactions, demographic factors (age, gender, race/ethnicity), TODAY study outcome (i.e., treatment failure or not), and number of study visits. Using backward stepwise elimination, we then developed separate sets of multivariable regression models, one for each parenting style for both the normative and diabetes tasks; the purpose was to simultaneously assess the associations of variables of interest with second 6 month adherence. Similar statistical models were constructed for youth and parent reports of parenting style. Final analyses included all variables thought to be of potential clinical importance to the interpretation of the findings, regardless of statistical significance. The contributions of both youth and parent normative and diabetes task parenting styles to subsequent adherence were also assessed; covariables were identical to those described above. Final analyses report beta coefficients, 95% confidence intervals for beta, and p values.
RESULTS
Participants
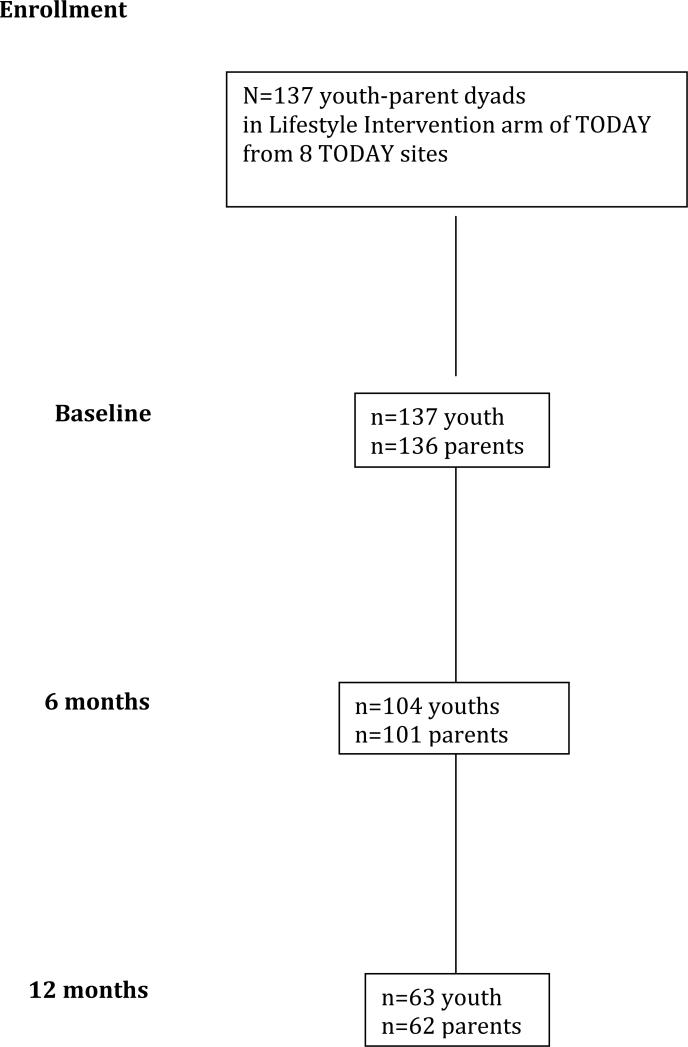
Data were collected from a convenience sample of 137 youth-parent dyads over a 2 year period (September 2004 – August 2006). See Figure 1 for a representation of the recruitment process.
Fig 1.
Recruitment and retention of TODAY ancillary study participants
See Table 1 for demographic data on the participants.
Table 1.
Demographic and Clinical Characteristics Of Participating Youth
| N=137 | |
| Age: years (mean ± SD) | 14.5 ± 2.1 |
| Gender: N(%) | |
| Female | 91 (66) |
| Male | 46 (34) |
| Race (Ethnicity: N(%) | |
| African American | 41 (30) |
| White | 30 (22) |
| Hispanic American | 46 (34) |
| Native American | 17 (12) |
| Asian American | 3 (2) |
| Parent's education: years, N(%) | |
| < High School | 31 (23) |
| High School/business school | 35 (25) |
| Associates degree/some college | 51 (37) |
| Bachelors degree or higher | 19 (14) |
| Diabetes duration: months, mean ± SD | 8.5 ± 6.2 |
| % pills taken, visits 2-6: mean ± SD | 82.3 ± 19.0 |
| % pills taken, visits 8-12: mean ± SD | 79.6 ± 23.8 |
This sample is similar (p>0.05) to the larger TODAY cohort in terms of demographic characteristics, with the exception of race/ethnicity (p=0.02), the TODAY study had fewer Native Americans and a larger percentage of Hispanics than this ancillary study. Participants who did not complete the follow-up surveys in the ancillary study at 6 or 12 months (n=78 dyads) did not differ (p>0.05) by gender, age, race/ethnicity or household income from participants who completed all three assessments (data not shown).
Parenting Style
The first research question was whether parenting style was associated with medication adherence. As shown in Table 2, both parents and youth reported a predominantly authoritative parenting style regarding both normative and diabetes self-care tasks over the 12 month period studied.
Table 2.
Parenting Style* as Reported by Youth and Parents
| Baseline | 6 month | 12 month | p values + | ||
|---|---|---|---|---|---|
| mean (95% CI) | mean (95% CI) | mean (95% CI) | Baseline to 6 months | Baseline to 12 months | |
| YOUTH | |||||
| Normative Tasks | |||||
| Authoritarian | 0.33 (0.29-0.36) | 0.29(0.24-0.33) | 0.24 (0.18-0.29) | 0.008 | <0.00 |
| Authoritative | 0.24 (0.21-0.27) | 0.26(0.22-0.29) | 0.28 (0.23-0.33) | 0.33 | 0.018 |
| Permissive | 0.43 (0.39-0.46) | 0.45(0.40-0.49) | 0.48 (0.42-0.54) | 0.037 | 0.012 |
| Diabetes Tasks | |||||
| Authoritarian | 0.25 (0.21-0.29) | 0.23(0.17-0.24) | 0.15 (0.09-0.20) | 0.13 | 0.003 |
| Authoritative | 0.27 (0.23-0.31) | 0.23(0.18-0.28) | 0.29 (0.23-0.35) | 0.075 | 0.61 |
| Permissive | 0.47 (0.42-0.52) | 0.53(0.47-0.59) | 0.56 (0.47-0.64) | 0.004 | 0.099 |
| PARENTS | |||||
| Normative Tasks | |||||
| Authoritarian | 0.39 (0.35-0.43) | 0.35(0.30-0.40) | 0.30 (0.24-0.36) | 0.16 | 0.007 |
| Authoritative | 0.30 (0.26-0.34) | 0.33(0.29-0.38) | 0.36 (0.30-0.41) | 0.027 | 0.026 |
| Permissive | 0.29 (0.25-0.33) | 0.25(0.21-0.30) | 0.28 (0.22-0.35) | 0.58 | 0.44 |
| Diabetes Tasks | |||||
| Authoritarian | 0.20 (0.15-0.25) | 0.19(0.14-0.24) | 0.16 (0.09-0.22) | 1.0 | 0.72 |
| Authoritative | 0.35 (0.29-0.40) | 0.33(0.27-0.39) | 0.33 (0.25-0.41) | 0.77 | 0.37 |
| Permissive | 0.44 (0.37-0.50) | 0.41(0.35-0.48) | 0.45 (0.36-0.55) | 0.64 | 0.24 |
Percentage of responses falling within each parenting style for each of the domains (normative and diabetes tasks)
p values from paired t-test comparisons, baseline to 6 months, baseline to 12 months for subjects with both assessments.
Youth perceptions
As seen in Table 2, youth perceived both a decrease in authoritarian parenting and an increase in permissive parenting for normative tasks at both 6 and 12 months (p= 0.008 and p<0.001 for changes in authoritarian style at 6 and 12 months; p=0.037 and p=0.012 for changes in permissive style at 6 and 12 months). For diabetes tasks, youth reported a significant decrease in the authoritarian parenting style across 12 months (p=0.003), while the increase in permissiveness occurred primarily between baseline and 6 months (p=0.004). As would be expected, older adolescents (14-17 years) reported a more permissive parenting style in both task domains than younger youth (10-13 years) at baseline and 12 months (p<0.001) (data not shown).
Parent perceptions
As seen in Table 2, for normative tasks, parents perceived an increase in authoritative parenting at both 6 months (p=0.027) and 12 months (p=0.026), and a decrease in authoritarian parenting at 12 months (p=0.046). For diabetes tasks, parents did not perceive any significant changes in parenting style over time.
Relationship of parenting style to medication adherence
Adherence, as measured by percent of pills taken, was generally high throughout the study period: in the first 6 months, Mean=83.1% (+/−18.3%); in the second 6 months, Mean=80.2% (+/−20.2%) (data not shown).
As seen in Table 3A, the youth report, but not the parent report, of a permissive parenting style (i.e., one that provides more autonomy and less parental control) regarding normative tasks, proved to be a significant predictor of subsequent medication adherence (the second 6 months), even after controlling for age, gender, ethnicity, overall TODAY outcome, number of study visits, and medication adherence during the first 6 months of this ancillary study (Adjusted R2=0.48, p<0.001). Similarly, as seen in Table 3B, the youth report (but not the parent report) of a less authoritarian parenting style regarding diabetes self-care tasks was also a significant predictor of subsequent medication adherence ( Adjusted R2=0.47, p<0.001) ). Ethnicity, gender and treatment failure were not significant predictors of adherence during the second 6 months but were still included in the final analyses as potentially meaningful covariates. When we looked at both youth and parent reports of the same parenting style (e.g. authoritarian style) for normative tasks in the same statistical analyses, the youth report remained a significant predictor of adherence, whereas the parent report was non-significant, as it was when we looked at the parent-only report data (data not shown). A similar observation was made for the statistical analyses with both youth and parent reports of parenting style for the diabetes tasks, the youth reports were significant predictors of adherence while the parent reports were not (data not shown).
Table 3.
Youth reports of Parenting Style for Normative & Diabetes Tasks as Predictors of Medication Adherence*
| A. Normative Task Models - YOUTH reports | |||||
|---|---|---|---|---|---|
| Variables | Beta | 95% CI of Beta | p value | Model Adjusted R2 | Model p value |
| Model 1: Authoritarian Style | 0.46 | <0.001 | |||
| Age (years) | −1.60 | (−3.34, 0.14) | 0.072 | ||
| Parenting style-youth report | −17.88 | (−37.61, 1.85) | 0.075 | ||
| Adherence first 6 months | 0.74 | (0.56, 0.92) | <0.001 | ||
| # of visits | 12.51 | (5.65, 19.36) | <0.001 | ||
| Model 2: Authoritative Style | 0.45 | <0.001 | |||
| Age (years) | −0.77 | (−2.59, 0.69) | 0.32 | ||
| Parenting style-youth report | −7.82 | (−8.27, 10.80) | 0.43 | ||
| Adherence first 6 months | 0.74 | (0.52, 0.89) | <0.001 | ||
| # of visits | 11.65 | (4.15, 18.39) | 0.001 | ||
| Model 3: Permissive Style | 0.48 | <0.001 | |||
| Age (years) | −1.98 | (−3.69, −0.27) | 0.024 | ||
| Parenting style-youth report | 25.40 | (6.74, 44.07) | 0.008 | ||
| Adherence first 6 months | 0.77 | (0.59, 0.95) | <0.001 | ||
| # of visits | 12.79 | (6.06, 19.52) | <0.001 | ||
|
B. Diabetes Task Models - YOUTH reports
| |||||
|---|---|---|---|---|---|
| Variables | Beta | 95% CI of Beta | p value | Model Adjusted R2 | Model p value |
| Model 1: Authoritarian | 0.47 | <0.001 | |||
| Age (years) | −1.62 | (−3.30, 0.06) | 0.059 | ||
| Parenting style-youth report | −15.27 | (−29.64, −0.90) | 0.037 | ||
| Adherence first 6 months | 0.77 | (0.59, 0.95) | <0.001 | ||
| # of Visits | 11.24 | (4.47, 18.01) | 0.001 | ||
| Model 2: Authoritative | 0.45 | <0.001 | |||
| Age (years) | −0.79 | (−2.30, 0.73) | 0.31 | ||
| Parenting style-youth report | −0.14 | (−14.36, 14.08) | 0.98 | ||
| Adherence first 6 months | 0.72 | (0.55, 0.91) | <0.001 | ||
| # of Visits | 11.69 | (4.79, 18.58) | 0.001 | ||
| Model 3: Permissive | 0.46 | <0.001 | |||
| Age (years) | −1.33 | (−2.95, 0.29) | 0.11 | ||
| Parenting style-youth report | 10.65 | (−1.48, 22.77) | 0.085 | ||
| Adherence first 6 months | 0.76 | (0.58, 0.94) | <0.001 | ||
| # of Visits | 11.63 | (4.83, 18.43) | 0.001 | ||
Multivariable regression models. Each model also includes: gender, race/ethnicity and overall TODAY study outcome.
Adherence = % of pills taken over months 8, 10, and 12.
In summary, the data indicate: (1) Youth perceived their parents as becoming more permissive (normative tasks) and less authoritarian (diabetes tasks) over time, while parents perceived their own parenting as becoming less authoritarian for normative tasks, but saw no change for diabetes tasks over time; (2) Youth who perceived their parents as being less authoritarian towards diabetes tasks and more permissive towards normative tasks, and thus supporting their autonomy across both contexts, demonstrated better adherence to medication over time than those who perceived their parents as using a more controlling parenting style.
Parent-youth conflict
The second research question was whether parent-youth conflict related to medication adherence. The emotional tone of conversations as reported by youth and parents regarding self-care tasks at all three time points was relatively calm, though some differences did emerge (see Table 4).
Table 4.
Parent-youth conflict+ as reported by youth and parents
| Baseline mean (95% CI) | 6 month mean (95% CI) | 12 month mean (95% CI) | |
|---|---|---|---|
| Youth Reports | |||
| Normative Tasks | 1.89 (1.74-2.05) | 2.08 (1.90-2.26) | 1.92 (1.70-2.15) |
| Diabetes Tasks | 1.70 (1.55-1.86) | 1.90 (1.72-2.09) | 1.86 (1.63-2.10) |
| *P values | 0.003 | 0.015 | 0.43 |
| Parent Reports | |||
| Normative Tasks | 1.91 (1.78-2.05) | 1.99 (1.84-2.15) | 1.99 (1.81-2.17) |
| Diabetes Tasks | 1.76 (1.63-1.90) | 2.07 (1.89-2.25) | 1.89 (1.66-2.13) |
| P values | 0.014 | 0.15 | 0.046 |
5 point scale: 1=very calm to 5=very angry
p values from paired t-test comparisons across domains within each time period.
Youth comparisons separate from parent comparisons.
At baseline, both youth and parents reported that conversations about normative tasks were more heated than conversations about diabetes tasks (youth: p=0.003; parent: p= 0.014). At 6 months, youth again reported greater conflict in conversations about normative tasks (p= 0.015), but there were no differences reported by parents. At 12 months, youth did not report any significant differences in emotional tone of conversations between the two task domains, but parents reported angrier conversations regarding normative than diabetes tasks (p=0.046). No significant differences in conflict scores were found based on child's age, disease duration, gender, or race/ethnicity.
Relationship of parent-youth conflict to medication adherence
Neither youth nor parent reports of conflict in discussions regarding normative tasks or diabetes self-care tasks were predictors of subsequent medication adherence, i.e., during the second 6 months (data not shown).
DISCUSSION
This is the first study we are aware of that examines the relationship between parenting style and parent-youth conflict regarding self-care tasks and medication adherence in youth with recently-diagnosed T2DM. The dyads in this sample reported a predominantly “authoritative” parenting style, in which youth and parents negotiate self-care responsibilities, but the parent has the final say. This can be distinguished from an “authoritarian” style, in which the parent dictates the youth's behaviors (most controlling), and a “permissive” style, in which the parent exerts the least control. Of course, these styles are not pure and should be considered to be on a continuum of increasing youth autonomy. Developmental theorists suggest that an authoritative parenting style, which allows for youth autonomy with parental involvement, is a good balance (Baumrind, 1978), and this is supported by evidence that authoritative parenting style relates to better youth self-reliance, achievement, and social competence (Steinberg, Dornsbusch & Brown, 1992) and self-regulation (Baumrind, 1996).
Our key finding, that parenting style as reported by youth with T2DM was a significant predictor of medication adherence, is consistent with research with youth with T1DM (Shorer, et al., 2011). Self-Determination Theory (SDT) provides a theoretical framework to help us understand these findings. SDT posits that three factors influence one's motivation to change one's behavior (Deci & Ryan, 1985; Ryan & Deci, 2000). These are autonomy (the belief that one has will and choice about changing behaviors), competence (the belief in one's own ability to make the change) and relatedness (support from others to make the change). Studies of adults that have assessed the relevance of these constructs to diabetes outcomes have reported that competence and autonomous motivations are related to improvements in blood glucose control (Williams, Friedman & Deci, 1998; Williams, McGregor, Zeldman, Freedman & Deci, 2004), diabetes self-care (Senecal, Mouwen & White, 2000) and weight loss (Williams, Grow, Freedman, Ryan & Deci, 1996). Our findings suggest that the construct of autonomy may also be key for youth with T2DM. In this study, the youth's perception of parenting that allowed for greater autonomy over their self-care behaviors was strongly predictive of the youth's future adherence to medication-taking behaviors. Future research should explore these theoretically grounded constructs further in youth with T2DM.
These youth-parent dyads exhibited relatively low conflict in conversations related to self-care. Both youth and parents reported greater conflict regarding normative tasks than diabetes self-care, but conflict was still low. In contrast, studies of youth with T1DM found an increase in family conflict regarding diabetes-specific issues (Anderson, et al., 2002; Anderson, 2001).We did not find a relationship between conflict and medication adherence, and it may be because the conflict level was low. Also, these youth were participating in a lifestyle change intervention that may have led parents to believe that diabetes self-care tasks were being ‘taken care of’ by the educators, thus allowing them to withdraw from potential conflict. Finally, the parents were participating in a program designed to help youth take care of themselves more effectively, and this participation may have ameliorated conflict. We note that none of the TODAY participants in this study were using insulin therapy at baseline, though a few were doing so at 12 months. Whether T2DM youth requiring insulin therapy would experience greater family conflict concerning diabetes issues than those treated with oral medications will require further investigation.
There are several limitations to this study. First, we relied on self-report measures to assess parenting style and youth-parent conflict. Second, the changes we found may have been related to participation of the dyads in the lifestyle change arm of TODAY, or to developmental maturation. Third, since this sample is a subset of the larger TODAY trial sample, one might question how generalizable are our findings. Fourth, at 12 months, less than half of the respondents completed the ancillary study questionnaires. Though this may have happened for a variety of reasons, e.g., no time at the clinic visit, lost interest, it may be that parents with a more authoritarian parenting style, or families in which there was more conflict, did not complete the 12 month assessment, thus affecting our interpretations. However, we note that our subset did not differ in measured ways from the larger cohort (other than a larger percentage of Native American youth), those who did not complete the 12 month assessment did not differ in measured ways from those who were retained, and, TODAY recruited the largest sample of youth with T2DM thus far studied. These factors enhance our confidence in the generalizability of our results. Still, there may be other unmeasured factors that differentiated this subset from the larger population of youth with T2DM.
In conclusion, in this study we found that youth with T2DM perceived parents as supporting greater autonomy towards self-care behaviors over time, and that greater parental permissiveness towards daily tasks, and less of an authoritarian style towards diabetes tasks, predicted better future medication adherence. Thus, youth who felt that they had more control over their behavior were more adherent. These findings may help clinicians enhance their focus on the impact of parenting style on youth behavior. They suggest that it may be valuable to assess parenting style regarding youth self-care, and especially the youth's perception of it, at the onset of medication treatment. Further research is needed in youth with T2DM to enhance confidence in these conclusions. If supported, interventions that target the youth-parent relationship and help parents understand the value of supporting increased youth autonomy while continuing their involvement may be warranted. Future research should also extend this line of study to examine whether parenting style predicts glycemic control and/or adaptation to the illness.
Acknowledgements
We thank TODAY participants and staff at the following clinical centers that participated in the ancillary study: Baylor College of Medicine, Case Western Reserve University, Children's Hospital Los Angeles, Saint Louis University, University of Colorado Denver, University of Oklahoma Health Sciences Center, University of Texas Health Science Center at San Antonio and SUNY Upstate Medical University in Syracuse NY. We thank the TODAY Study Group for allowing us access and data to conduct this ancillary study. This work was funded by the National Institutes of Health/NIDDK U01-DK061230. Clinical trials reg. no. NCT00081328, clinicaltrials.gov.
REFERENCES
- Anderson BJ. Family conflict and diabetes management in youth: Clinical lessons from child development and diabetes research. Diabetes Spectrum. 2004;17:22–6. [Google Scholar]
- Anderson BJ, Vangsness L, Connell A, Butler D, Goebel-Fabbri A, Laffel LMB. Family conflict, adherence, and glycemic control in youth with short duration type 1 diabetes. Diabetic Medicine. 2002;19:635–42. doi: 10.1046/j.1464-5491.2002.00752.x. [DOI] [PubMed] [Google Scholar]
- Anderson BJ. Children with diabetes mellitus and family functioning: Translating research into practice. Journal of Pediatric Endocrinology & Metabolism. 2001;14(Suppl. 1):645–52. doi: 10.1515/jpem.2001.14.s1.645. [DOI] [PubMed] [Google Scholar]
- Baumrind D. Child care practices anteceding three patterns of preschool behavior. Genetic Psychology Monographs. 1967;75:43–88. [PubMed] [Google Scholar]
- Baumrind D. Authoritarian vs. authoritative parental control. Adolescence. 1978;3:255–72. [Google Scholar]
- Baumrind D. Parenting styles and adolescent development. In: Brooks-Gunn J, Lerner R, Peterson AC, editors. The Encyclopedia of Adolescence. Garland, NY: 1991. [Google Scholar]
- Baumrind D. The discipline controversy revisited. Family Relations. 1996;45:405–14. [Google Scholar]
- Deci EL, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behavior. Plenum; New York: 1985. [Google Scholar]
- Delamater AM, Jacobson AM, Anderson B, et al. Psychosocial therapies in diabetes. Diabetes Care. 2001;24:1286–91. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- Demmer RT, Zuk AM, Rosenbaum M, Desvarieux M. Prevalence of diagnosed and undiagnosed type 2 diabetes mellitus among US adolescents: Results from the Continuous NHANES, 1999-2010. American Journal of Epidemiology. 2013:1–8. doi: 10.1093/aje/kwt088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinstein G, Muzumdar R, Aponte L, Vuguin P, Saenger P, DiMartino-Nardi J. Presentation and 5-year follow-up of Type 2 diabetes mellitus in African American and Caribbean-Hispanic adolescents. Hormone Research. 2003;60:121–26. doi: 10.1159/000072523. [DOI] [PubMed] [Google Scholar]
- Johnson SB, Silverstein J, Rosenbloom A, Carter R, Cunningham W. Assessing daily management in childhood diabetes. Health Psychology. 1986;5:545–64. doi: 10.1037/0278-6133.5.6.545. [DOI] [PubMed] [Google Scholar]
- Maccoby E, Martin J. Socialization in the context of the family: Parent-child interaction. In: Heatherington EM, editor. Handbook of Child Psychology (4th Edition), Vol. IV:Socialization, Personality and Social Development. Wiley; New York: 1983. pp. 103–196. [Google Scholar]
- Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Novinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. Journal of Consulting and Clinical Psychology. 1994;62:603–10. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. Journal of the American Medical Association. 2008;303(3):242–49. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Pinhas-Hamiel O, Zeitler P. The global spread of type 2 diabetes mellitus in children and adolescents. Journal of Pediatrics. 2005 May;:693–98. doi: 10.1016/j.jpeds.2004.12.042. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O'Leary KD. Multivariate assessment of conflict in distressed and non-distressed mother-adolescent dyads. Journal of Applied Behavioral Analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Foster SL. Problem-Solving Communication Training: A Behavioral Family Systems Approach to Parent-Child Conflict. In: Karoly P, Steffen J, editors. Adolescent Behavior Disorders: Foundations and Contemporary Concerns. DC Heath; Lexington, MA: 1984. [Google Scholar]
- Rubin RR, Young-Hyman D, Peyrot M. Parent-child responsibility and conflict in diabetes care (Abstract). Diabetes. 1989;38(Supplement 2):28A. [Google Scholar]
- Ryan RM, Deci EL. Self-Determination Theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- Senecal C, Nouwen A, White D. Motivation and dietary self-care in adults with diabetes: Are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychology. 2000;19:452–57. doi: 10.1037//0278-6133.19.5.452. [DOI] [PubMed] [Google Scholar]
- Shorer M, David R, Schoenberg-Taz M, Lefavi-Lavi I, Phillip M, Meyerovitch J. Role of parenting style in achieving metabolic control in adolescents with type 1 diabetes. Diabetes Care. 2011;34:1735–37. doi: 10.2337/dc10-1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg SB, Steinberg L. Adolescent autonomy, parent-adolescent conflict, and parental well-being. Journal of Youth and Adolescence. 1987;16:293–312. doi: 10.1007/BF02139096. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Silverberg S. The vicissitudes of autonomy in early adolescence. Child Development. 1987;57:841–51. doi: 10.1111/j.1467-8624.1986.tb00250.x. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Dornsbusch S, Brown B. Ethnic differences in adolescent achievement: An ecological perspective. American Psychologist. 1992;47:723–729. doi: 10.1037//0003-066x.47.6.723. [DOI] [PubMed] [Google Scholar]
- TODAY Study Group Treatment Options for Type 2 Diabetes in Adolescents and Youth: A study of the comparative efficacy of metformin alone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatric Diabetes. 2007;8:74–87. doi: 10.1111/j.1399-5448.2007.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TODAY Study Group Design of a family-based lifestyle intervention for youth with type 2 diabetes: the TODAY study. International Journal of Obesity. 2010;34:217–26. doi: 10.1038/ijo.2009.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TODAY Study Group Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. Journal of Clinical Endocrinology and Metabolism. 2011;96:159–67. doi: 10.1210/jc.2010-1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TODAY Study Group A clinical trial to maintain glycemic control in youth with type 2 diabetes. New England Journal of Medicine. 2012;366:2247–56. doi: 10.1056/NEJMoa1109333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–51. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. Journal of Personality & Social Psychology. 1996;70:115–26. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a Self-Determination Theory process model for promoting glycemic control through diabetes self-management. Health Psychology. 2004;23:58–66. doi: 10.1037/0278-6133.23.1.58. [DOI] [PubMed] [Google Scholar]