Abstract
Background
It is generally accepted that hospital volume is associated with mortality in high-risk procedures. However, as surgical safety has improved over the last decade, recent evidence has suggested that the inverse relationship has diminished or been eliminated.
Objective
To determine whether the relationship between hospital volume and mortality has changed over time.
Methods
Using national Medicare claims data from 2000 through 2009, we examined mortality among 3,282,127 patients who underwent one of eight gastrointestinal, cardiac, or vascular procedures. Hospitals were stratified into quintiles of operative volume. Using multivariable logistic regression models to adjust for patient characteristics, we examined the relationship between hospital volume and mortality, and assessed for changes over time. We performed sensitivity analyses using hierarchical logistic regression modeling with hospital-level random effects to confirm our results.
Results
Throughout the ten-year period, a significant inverse relationship was observed in all procedures. In five of the eight procedures studied, the strength of the volume-outcome relationship increased over time. In esophagectomy, for example, the adjusted odds ratio of mortality in very low volume hospitals compared to very high volume hospitals increased from 2.25 [95%CI: 1.57-3.23] in 2000-2001 to 3.68 [95%CI: 2.66-5.11] in 2008-2009. Only pancreatectomy showed a notable decrease in strength of the relationship over time, from 5.83 [95%CI: 3.64-9.36] in 2000-2001, to 3.08 [95%CI: 2.07 - 4.57] in 2008-2009.
Conclusion
For all procedures examined, higher volume hospitals had significantly lower mortality rates compared to lower volume hospitals. Despite recent improvements in surgical safety, the strong inverse relationship between hospital volume and mortality persists in the modern era.
INTRODUCTION
Evidence that hospital volume influences outcomes has been verified in nearly every major type of surgery.1-3 This body of work highlighted important and previously unrecognized variations in hospital performance and ignited efforts to improve surgical quality among poorly performing hospitals. In an effort to reduce these variations among hospitals, new health policy and quality improvement initiatives such as public reporting, pay-for-performance, and surgical checklists, have been implemented to promote best practice and improve standards of care.4-7 Over the last decade, surgical mortality rates have significantly decreased throughout the country, possibly due to these measures.8-10
As a result, it is unclear whether the volume-outcome relationship has persisted in the modern era. Recent improvements in surgical outcomes could change the relationship between volume and outcome in two possible ways. First, advances in surgical care could weaken or eliminate the influence of hospital volume on patient outcomes. Alternatively, despite absolute decreases in mortality, relative differences may persist between hospitals and the relationship endures over time. Recently published evidence supports the former hypothesis, asserting that the volume-outcome relationship is severely attenuated in recent years.11 However, this single study represents only a subset of U.S. hospitals in one year and may not be generalizable to all hospitals or longer periods. Given the incorporation of volume standards into several health policy initiatives (e.g. Centers of Excellence,12 Leapfrog Initiative13, 14), as well as accreditation processes and local credentialing decisions, it is important for policymakers and surgical leaders to understand whether the volume-outcome relationship has changed over time.
Given this uncertainty, we sought to evaluate whether the relationship between hospital volume and operative mortality has changed during a recent ten-year period, using a national dataset of high-risk patients. To do this, we examined the risk-adjusted operative mortality of Medicare patients undergoing one of eight complex gastrointestinal, cardiac, or vascular procedures at hospitals in the lowest and highest quintiles of operative volume during the years 2000 to 2009.
METHODS
Data Source and Study Population
To complete this study, we utilized analytic files for the years 2000 to 2009 from the Center for Medicare and Medicaid Services. The Medicare Provider Analysis and Review (MEDPAR) file, which contains hospital discharge records for fee-for-service acute care hospitalizations of all Medicare beneficiaries not enrolled in managed care plans, was used to create the main datasets for analysis, and the Medicare Denominator file was used to determine vital status of patients 30 days after surgery. The Institutional Review Board of the University of Michigan and the CMS approved this protocol and waived the requirement for informed consent.
We identified patients between the ages of 65 and 99 years old who underwent one of three gastrointestinal (colectomy, esophagectomy, and pancreatectomy), three cardiac (aortic valve replacement, mitral valve replacement, and coronary artery bypass grafting), or two vascular procedures (abdominal aortic aneurysm repair and carotid endarterectomy) during the study period, using appropriate procedure codes from the International Classification of Diseases, Ninth Revision, Clinicial Modification (ICD-9-CM). Patients undergoing open, laparoscopic, minimally-invasive and endovascular approaches were included in this analysis. These procedures were selected prospectively as they represent commonly performed complex elective procedures with non-trivial risks of mortality, for which previous literature has reported an association between volume and operative mortality of varying strengths.1, 2, 15
To minimize confounding and increase the homogeneity of our sample, we utilized multiple restrictions. Patients who underwent a repair of an abdominal aortic aneurysm were excluded if they had accompanying diagnosis or procedure codes suggesting a rupture of the aneurysm, presence of a thoracoabdominal aneurysm, or dissection. We also excluded patients who underwent simultaneous coronary artery bypass grafting and valve surgery. For the three gastrointestinal procedures identified, we included operations for both benign and malignant disease in the final analysis.
Hospital Volume
In this analysis, hospital volume for each procedure was defined as total volume of operations performed in Medicare beneficiaries during each two-year period. Two-year periods were chosen to improve the reliability and power of model estimates and minimize statistical noise, which would be increased in one-year periods. In order to more accurately estimate the volume at each center, the restrictions mentioned above were not applied when determining overall hospital volume, and only thoracoabdominal aneurysms associated with elective abdominal aortic aneurysm repair were excluded. To better understand the relationship between volume and mortality, volume was first evaluated as a continuous variable. To simplify the presentation of results, and to allow for understanding in the context of current literature, we also created a categorical variable detailing five categories of hospital volume: very low, low, medium, high, and very high. For each procedure, hospitals were ranked in order of increasing total two-year hospital volume, and categories were created by defining prospective whole number cut-offs that would separate all patients into five quintiles of equal size.
Assessment of Outcomes
Our primary outcome measure was operative mortality, defined as the rate of death before hospital discharge, or within 30-days of the index procedure for patients discharged prior to that date. As with previous literature in this area, late in-hospital mortality was included to allow for a more accurate understanding of operative mortality, as many patients that die following surgery first experience one or multiple complications and a prolonged hospitalization greater than 30 days. The relationship between hospital volume and operative mortality was evaluated separately for each two-year period, and longitudinal trends were observed.
Statistical Analysis
We used multivariable logistic regression to examine the relationship between hospital volume and operative mortality during the ten-year study period, after adjusting for patient characteristics, year of the procedure, and surgical approach (when that data was available). The patient was used as the unit of analysis, with volume characterized at the hospital level. For each procedure, we fitted a separate model against the hospital volume variable for each two-year period. To account for the lack of independence of deaths within hospitals, or clustering, we calculated robust standard errors.
To account for differences in patient characteristics within individual hospitals, we adjusted for age, sex, race (black or non-black) and their interactions, urgency or emergency of the admission, the presence of coexisting conditions, and socioeconomic status. For this last variable, we constructed a summary measure of socioeconomic status for each US ZIP code using data on income, education, and occupation from the 2000 US Census and linked this information to the patient’s ZIP code of residence in the Medicare files. The individual variables chosen and methods for calculating the summary measure were based on previously developed methods.16 Coexisting conditions were identified by their appropriate ICD-9-CM codes, and were defined with the Elixhauser method, which uses ICD-9-CM codes to classify secondary diagnoses recorded on the MEDPAR record into 30 different comorbid conditions.17 Final risk-adjustment models had C statistics ranging from 0.716 (for mitral valve replacement) to 0.821 (for colectomy).
To confirm the accuracy of our final risk-adjustment models, we performed sensitivity analyses using hierarchical logistic regression modeling with hospital-level random effects. Because these models are complex and prone to failure (non-convergence), we simplified the regression by first creating a predictive score for operative mortality using all available patient covariates. This summary risk score was used to model the relationship between hospital volume and operative mortality after adjustment for patient characteristics and year of procedure. This was performed for all procedures except esophagectomy and carotid endarterectomy, which were too unstable given the small numbers of patients or events. Results of hierarchical modeling, using both continuous and categorical measures of hospital volume, were then compared to the results of multivariable logistic regression modeling with robust standard errors.
For all statistical tests, p values are two-tailed, and alpha is set at 0.05. All analyses were performed using STATA version 12.1 (StataCorp, College Station, TX).
RESULTS
Between the years 2000 and 2009, 3,282,127 patients underwent 1 of the 8 specified procedures. Table 1 shows the number of patients in each model, as well as patient demographic information, within quintiles of very low and very high volume for each procedure and period. The criteria used to create quintiles varied between procedures due to the different frequencies at which each operation was performed. During the study period, coronary artery bypass grafting, colectomy and carotid endarterectomy were the most commonly performed procedures, while pancreatectomy and esophagectomy were performed the least. The total Medicare volume decreased for coronary artery bypass grafting, carotid endarterectomy and mitral valve replacement during the ten-year period, while it remained stable for esophagectomy, and increased for abdominal aortic aneurysm repair, aortic valve replacement, and pancreatectomy. In general, sex showed minimal variation between very low and very high volume hospitals. Although cardiac procedures showed similar rates of non-elective admissions in both groups, other operations revealed higher rates in very low volume hospitals, with the largest discrepancies observed in esophagectomy and pancreatectomy. Very low volume hospitals cared for more African American patients, patients with 3 or more comorbidities, and patients older than 75 years.
Table 1.
Patient characteristics among very low and very high volume quintiles for the eight procedures during the study period.
| Procedure | Time Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000-2001 | 2002-2003 | 2004 - 2005 | 2006-2007 | 2008-2009 | ||||||
| Hospital Volume | ||||||||||
| Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | |
| Pancreatectomy | ||||||||||
| Medicare Patients (N) | 5,002 | 5,651 | 5,564 | 5,944 | 8,571 | |||||
| Age >75 years (%) | 37.3 | 38.5 | 38.8 | 37.2 | 39.8 | 42.8 | 42.3 | 42.3 | 39.0 | 40.3 |
| Female (%) | 51.0 | 47.2 | 53.5 | 52.2 | 52.8 | 51.1 | 50.9 | 50.2 | 53.0 | 48.2 |
| African American Race (%) | 8.3 | 3.8 | 10.6 | 3.7 | 10.3 | 4.1 | 9.0 | 4.4 | 9.0 | 5.5 |
| Nonelective admission (%) | 37.9 | 10.7 | 41.8 | 11.1 | 37.2 | 9.8 | 32.4 | 10.1 | 32.3 | 11.6 |
| ≥3 Comorbid Conditions (%) | 33.8 | 21.8 | 39.2 | 24.2 | 41.0 | 31.2 | 41.2 | 33.1 | 36.3 | 31.8 |
| Colectomy | ||||||||||
| Medicare Patients (N) | 186,300 | 191,656 | 170,009 | 162,525 | 221,423 | |||||
| Age >75 years (%) | 56.6 | 54.6 | 56.0 | 53.6 | 56.8 | 54.7 | 56.8 | 55.6 | 53.3 | 51.2 |
| Female (%) | 59.9 | 59.2 | 59.4 | 59.0 | 59.8 | 59.7 | 59.0 | 59.0 | 58.9 | 58.8 |
| African American Race (%) | 9.1 | 7.3 | 9.1 | 8.5 | 9.0 | 8.9 | 9.1 | 8.1 | 8.9 | 8.6 |
| Nonelective admission (%) | 55.2 | 44.6 | 53.4 | 42.9 | 52.4 | 41.9 | 51.9 | 40.6 | 51.2 | 39.4 |
| ≥3 Comorbid Conditions (%) | 31.5 | 30.1 | 34.2 | 32.5 | 36.9 | 34.2 | 38.3 | 36.2 | 33.9 | 31.3 |
| Esophagectomy | ||||||||||
| Medicare Patients (N) | 6,315 | 6,046 | 5,464 | 5,204 | 6,601 | |||||
| Age >75 years (%) | 43.4 | 30.6 | 42.6 | 32.0 | 43.5 | 32.8 | 43.2 | 33.7 | 39.7 | 33.8 |
| Female (%) | 31.2 | 25.7 | 32.2 | 23.8 | 31.9 | 26.1 | 34.6 | 25.5 | 29.6 | 24.1 |
| African American Race (%) | 8.4 | 4.1 | 9.4 | 3.2 | 9.2 | 3.1 | 8.0 | 2.8 | 8.2 | 3.8 |
| Nonelective admission (%) | 34.4 | 11.4 | 34.0 | 8.2 | 33.9 | 6.3 | 31.2 | 6.5 | 29.2 | 6.8 |
| ≥3 Comorbid Conditions (%) | 34.2 | 19.8 | 37.2 | 20.8 | 40.3 | 23.7 | 39.8 | 28.4 | 31.7 | 24.1 |
| Coronary Artery Bypass Grafting | ||||||||||
| Medicare Patients (N) | 263,232 | 242,362 | 189,273 | 155,625 | 178,849 | |||||
| Age >75 years (%) | 38.1 | 38.5 | 37.8 | 38.2 | 39.6 | 40.3 | 40.2 | 41.0 | 36.4 | 27.8 |
| Female (%) | 34.2 | 34.0 | 33.6 | 33.3 | 32.9 | 32.6 | 32.0 | 32.0 | 31.7 | 30.8 |
| African American Race (%) | 4.6 | 5.3 | 6.3 | 5.6 | 6.6 | 5.9 | 6.4 | 6.4 | 6.4 | 6.0 |
| Nonelective admission (%) | 54.8 | 54.3 | 52.6 | 53.5 | 51.8 | 54.9 | 51.3 | 52.5 | 50.5 | 51.7 |
| ≥3 Comorbid Conditions (%) | 21.6 | 21.1 | 25.0 | 25.4 | 29.1 | 28.6 | 39.4 | 39.7 | 41.4 | 38.5 |
| Aortic Valve Replacement | ||||||||||
| Medicare Patients (N) | 52,847 | 56,636 | 52,594 | 54,175 | 76,649 | |||||
| Age >75 years (%) | 52.5 | 56.0 | 52.1 | 56.5 | 52.9 | 58.2 | 56.2 | 60.8 | 53.5 | 59.7 |
| Female (%) | 42.5 | 43.2 | 42.5 | 41.6 | 42.7 | 42.1 | 42.0 | 42.5 | 41.4 | 40.9 |
| African American Race (%) | 4.9 | 2.1 | 4.8 | 2.8 | 4.5 | 3.2 | 4.6 | 2.8 | 4.9 | 2.9 |
| Nonelective admission (%) | 37.8 | 35.4 | 36.0 | 37.9 | 35.7 | 36.6 | 35.5 | 35.9 | 33.8 | 35.1 |
| ≥3 Comorbid Conditions (%) | 18.7 | 17.2 | 22.0 | 19.7 | 26.0 | 22.7 | 41.0 | 40.3 | 46.0 | 43.9 |
| Mitral Valve Replacement | ||||||||||
| Medicare Patients (N) | 17,462 | 16,736 | 13,593 | 11,539 | 14,146 | |||||
| Age >75 years (%) | 41.4 | 45.1 | 43.5 | 47.2 | 45.8 | 51.0 | 46.7 | 52.3 | 43.8 | 48.6 |
| Female (%) | 58.6 | 58.0 | 60.2 | 57.8 | 57.7 | 58.2 | 57.9 | 58.5 | 58.3 | 56.7 |
| African American Race (%) | 5.6 | 3.1 | 5.6 | 4.0 | 6.1 | 4.4 | 6.1 | 4.5 | 7.4 | 5.7 |
| Nonelective admission (%) | 42.9 | 43.5 | 42.4 | 42.4 | 42.7 | 41.7 | 42.8 | 41.8 | 40.1 | 41.1 |
| ≥3 Comorbid Conditions (%) | 14.4 | 12.6 | 17.2 | 14.3 | 20.5 | 15.8 | 41.5 | 38.0 | 43.8 | 43.7 |
| Abdominal Aortic Aneurysm Repair | ||||||||||
| Medicare Patients (N) | 51,043 | 51,962 | 46,105 | 47,289 | 62,327 | |||||
| Age >75 years (%) | 43.2 | 45.2 | 43.3 | 47.4 | 46.4 | 49.9 | 50.1 | 52.4 | 49.5 | 49.6 |
| Female (%) | 31.3 | 25.8 | 29.9 | 24.2 | 28.7 | 23.9 | 26.8 | 23.7 | 26.1 | 24.5 |
| African American Race (%) | 6.1 | 3.2 | 6.3 | 3.4 | 6.1 | 3.8 | 5.3 | 3.6 | 5.8 | 3.7 |
| Nonelective admission (%) | 27.8 | 19.2 | 24.3 | 16.6 | 22.6 | 15.5 | 21.6 | 16.3 | 21.4 | 14.7 |
| ≥3 Comorbid Conditions (%) | 29.6 | 27.8 | 32.5 | 29.7 | 35.0 | 29.2 | 41.6 | 37.7 | 40.2 | 40.2 |
| Carotid Endarterectomy | ||||||||||
| Medicare Patients (N) | 148,468 | 144,130 | 112,339 | 103,038 | 127,433 | |||||
| Age >75 years (%) | 50.9 | 47.3 | 51.1 | 48.8 | 52.2 | 49.3 | 53.2 | 51.0 | 51.2 | 49.6 |
| Female (%) | 46.1 | 43.5 | 45.7 | 43.5 | 46.2 | 44.0 | 45.8 | 42.8 | 44.6 | 42.7 |
| African American Race (%) | 4.3 | 2.8 | 4.6 | 2.8 | 5.2 | 3.2 | 4.8 | 3.0 | 5.5 | 3.3 |
| Nonelective admission (%) | 29.1 | 23.6 | 26.0 | 18.6 | 26.9 | 16.8 | 23.6 | 16.0 | 23.6 | 14.2 |
| ≥3 Comorbid Conditions (%) | 20.7 | 19.4 | 23.5 | 22.5 | 27.2 | 26.2 | 32.4 | 32.5 | 34.4 | 33.6 |
Table 2 lists the total number of hospitals performing each procedure, as well as the number of hospitals and the volume thresholds contained within quintiles of very low and very high volume for each procedure and period. For all three gastrointestinal procedures and abdominal aortic aneurysm repair, the number of hospitals performing the operation decreased, while the volume threshold of the very high volume quintile increased. All three cardiac procedures showed increases in the total number of hospitals performing the operation, but the effects on volume thresholds varied.
Table 2.
Distribution of hospitals and hospital volume among very low and very high volume quintiles for the eight procedures during the study period.
| Procedure | Time Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000-2001 | 2002-2003 | 2004 - 2005 | 2006-2007 | 2008-2009 | ||||||
| Hospital Volume | ||||||||||
| Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | |
| Pancreatectomy | ||||||||||
| Hospitals (N) | 1,237 | 1,119 | 964 | 883 | 926 | |||||
| Hospitals per quintile (N) | 866 | 15 | 740 | 14 | 674 | 11 | 639 | 14 | 692 | 14 |
| Annual procedure volume | <2 | >17 | <2 | >22 | <3 | >28 | <3 | >30 | <5 | >41 |
| Colectomy | ||||||||||
| Hospitals (N) | 4,259 | 4,160 | 4,181 | 3,920 | 3,894 | |||||
| Hospitals per quintile (N) | 2,621 | 177 | 2,578 | 174 | 2,638 | 170 | 2,443 | 164 | 2,483 | 155 |
| Annual procedure volume | <22 | >82 | <23 | >88 | <22 | >84 | <22 | >80 | <29 | >109 |
| Esophagectomy | ||||||||||
| Hospitals (N) | 1,559 | 1,477 | 1,310 | 1,216 | 1,229 | |||||
| Hospitals per quintile (N) | 1,023 | 27 | 996 | 26 | 880 | 19 | 816 | 20 | 870 | 19 |
| Annual procedure volume | <2 | >12 | <2 | >12 | <2 | >17 | <2 | >17 | <3 | >18 |
| Coronary Artery Bypass Grafting | ||||||||||
| Hospitals (N) | 1,069 | 1,107 | 1,150 | 1,187 | 1,189 | |||||
| Hospitals per quintile (N) | 569 | 53 | 565 | 57 | 594 | 59 | 606 | 62 | 594 | 69 |
| Annual procedure volume | <127 | >480 | <113 | >422 | <93 | >325 | <72 | >257 | <79 | >272 |
| Aortic Valve Replacement | ||||||||||
| Hospitals (N) | 1,024 | 1,078 | 1,112 | 1,150 | 1,159 | |||||
| Hospitals per quintile (N) | 587 | 39 | 621 | 38 | 636 | 41 | 666 | 40 | 674 | 39 |
| Annual procedure volume | <23 | >107 | <23 | >112 | <23 | >99 | <22 | >99 | <28 | >135 |
| Mitral Valve Replacement | ||||||||||
| Hospitals (N) | 975 | 1,027 | 1,049 | 1,069 | 1,077 | |||||
| Hospitals per quintile (N) | 562 | 34 | 599 | 38 | 607 | 36 | 631 | 39 | 610 | 41 |
| Annual procedure volume | <10 | >42 | <9 | >38 | <8 | >35 | <7 | >28 | <7 | >31 |
| Abdominal Aortic Aneurysm Repair | ||||||||||
| Hospitals (N) | 2,301 | 2,167 | 2,050 | 1,913 | 1,888 | |||||
| Hospitals per quintile (N) | 1,511 | 64 | 1,451 | 59 | 1,367 | 60 | 1,235 | 61 | 1,177 | 69 |
| Annual procedure volume | <14 | >73 | <16 | >78 | <16 | >72 | <16 | >70 | <18 | >77 |
| Carotid Endarterectomy | ||||||||||
| Hospitals (N) | 2,569 | 2,487 | 2,444 | 2,325 | 2,275 | |||||
| Hospitals per quintile (N) | 1,602 | 96 | 1,532 | 101 | 1,502 | 102 | 1,408 | 100 | 1,364 | 103 |
| Annual procedure volume | <32 | >141 | <32 | >134 | <28 | >112 | <26 | >100 | <29 | >108 |
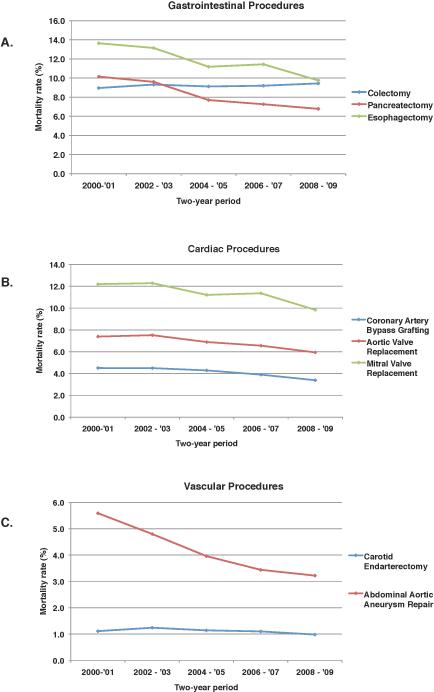
Adjusted mortality for most operations decreased during the ten-year study period, as shown in Figure 1. The largest decreases in mortality were seen following esophagectomy, which decreased from 13.6% in 2000, to 9.8% in 2009 (difference of 3.8%), and pancreatectomy, which decreased from 10.2% to 6.8% (difference of 3.4%). Mortality following carotid endarterectomy remained relatively stable, and varied from 1.0% to 1.2% over the ten-year period. Colectomy showed a slight increase, from 9.0% to 9.4%.
Figure 1.
Trend over time of adjusted mortality for all Medicare patients in each two-year period undergoing: A) gastrointestinal procedures, B) cardiac procedures, and C) vascular procedures.
The influence of hospital volume on risk-adjusted mortality is shown in Table 3. A significant inverse relationship was observed in all procedures and nearly every two-year period studied. When examined as a continuous variable, identical results were obtained (data not shown). No relationship was significant as a categorical variable that was not significant as a continuous variable (p < 0.05). Throughout most of the period, hospital volume had the greatest influence on mortality following pancreatectomy. The adjusted odds ratio (AOR) of mortality was 5.83 [95% CI: 3.64 - 9.36] in 2000, and 3.08 [95% CI: 2.07 - 4.57] in 2009. Esophagectomy also exhibited a strong inverse relationship throughout the period, and exhibited the highest odds of mortality during the years 2008-2009 (AOR 3.68, 95% CI 2.66 - 5.11). Colectomy exhibited the weakest significant association, with an AOR of 1.08 [95% CI: 1.01 - 1.15] in 2000, and 1.20 [95% CI: 1.13 - 1.28] in 2009. Only carotid endarterectomy during the years 2006-2007 did not have a significant relationship.
Table 3.
Adjusted rate, absolute difference in rates, and adjusted odds ratios of operative mortality for very low volume hospitals compared to very high volume hospitals (CI: confidence interval).
| PROCEDURE | Time Period | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000-2001 | 2002-2003 | 2004 - 2005 | 2006-2007 | 2008-2009 | ||||||
| Hospital Volume | ||||||||||
| Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | Very Low | Very High | |
| Pancreatectomy | ||||||||||
| Mortality rate (%) | 14.11 | 3.17 | 13.65 | 4.05 | 11.76 | 3.70 | 11.05 | 4.13 | 11.13 | 4.22 |
| Absolute difference in rates (%) | 10.94 | 9.60 | 8.06 | 6.92 | 6.91 | |||||
| Adjusted Odds Ratio (95% CI) | 5.83 (3.64 -9.36) | 4.21 (2.60 - 6.82) | 3.87 (2.91 - 5.16) | 3.19 (2.16 - 4.72) | 3.08 (2.07 - 4.57) | |||||
| Colectomy | ||||||||||
| Mortality rate (%) | 9.22 | 8.68 | 9.73 | 8.84 | 9.75 | 8.44 | 9.97 | 8.28 | 10.29 | 8.92 |
| Absolute difference in rates (%) | 0.54 | 0.89 | 1.31 | 1.69 | 1.37 | |||||
| Adjusted Odds Ratio (95% CI) | 1.08 (1.01 - 1.15) | 1.13 (1.06 - 1.21) | 1.20 (1.12 - 1.29) | 1.27 (1.18 - 1.36) | 1.20 (1.13 - 1.28) | |||||
| Esophagectomy | ||||||||||
| Mortality rate (%) | 16.76 | 8.90 | 15.37 | 9.16 | 15.01 | 5.80 | 15.14 | 7.49 | 13.94 | 4.72 |
| Absolute difference in rates (%) | 7.86 | 6.21 | 9.21 | 7.65 | 9.22 | |||||
| Adjusted Odds Ratio (95% CI) | 2.25 (1.57 - 3.23) | 1.92 (1.36 - 2.70) | 3.18 (2.41 - 4.18) | 2.41 (1.66 - 3.52) | 3.68 (2.66 - 5.11) | |||||
| Coronary Artery Bypass Grafting | ||||||||||
| Mortality rate (%) | 4.88 | 4.13 | 4.87 | 4.12 | 4.78 | 3.87 | 4.65 | 3.52 | 3.95 | 2.83 |
| Absolute difference in rates (%) | 0.75 | 0.75 | 0.91 | 1.13 | 1.12 | |||||
| Adjusted Odds Ratio (95% CI) | 1.20 (1.08 - 1.34) | 1.21 (1.08 - 1.34) | 1.26 (1.12 - 1.42) | 1.36 (1.21 - 1.52) | 1.44 (1.28 - 1.61) | |||||
| Aortic Valve Replacement | ||||||||||
| Mortality rate (%) | 8.06 | 6.17 | 8.44 | 6.25 | 8.49 | 5.69 | 7.98 | 5.01 | 7.64 | 4.50 |
| Absolute difference in rates (%) | 1.89 | 2.19 | 2.80 | 2.97 | 3.14 | |||||
| Adjusted Odds Ratio (95% CI) | 1.36 (1.16 - 1.59) | 1.41 (1.22 - 1.65) | 1.58 (1.34 - 1.86) | 1.68 (1.44 - 1.98) | 1.80 (1.56 - 2.08) | |||||
| Mitral Valve Replacement | ||||||||||
| Mortality rate (%) | 13.62 | 11.00 | 13.40 | 10.30 | 13.31 | 9.86 | 13.51 | 8.80 | 11.30 | 7.20 |
| Absolute difference in rates (%) | 2.62 | 3.10 | 3.45 | 4.71 | 4.10 | |||||
| Adjusted Odds Ratio (95% CI) | 1.30 (1.08 - 1.56) | 1.38 (1.13 - 1.68) | 1.44 (1.18 - 1.77) | 1.67 (1.32 - 2.10) | 1.69 (1.36 - 2.09) | |||||
| Abdominal Aortic Aneurysm Repair | ||||||||||
| Mortality rate (%) | 6.60 | 5.00 | 5.56 | 3.73 | 4.25 | 3.43 | 4.06 | 2.88 | 3.85 | 2.74 |
| Absolute difference in rates (%) | 1.60 | 1.83 | 0.82 | 1.18 | 1.11 | |||||
| Adjusted Odds Ratio (95% CI) | 1.39 (1.19 - 1.62) | 1.59 (1.35 - 1.88) | 1.28 (1.07 - 1.52) | 1.48 (1.21 - 1.81) | 1.48 (1.27 - 1.72) | |||||
| Carotid Endarterectomy | ||||||||||
| Mortality rate (%) | 1.26 | 0.96 | 1.43 | 1.11 | 1.35 | 0.99 | 1.29 | 1.11 | 1.12 | 0.88 |
| Absolute difference in rates (%) | 0.30 | 0.32 | 0.36 | 0.18 | 0.24 | |||||
| Adjusted Odds Ratio (95% CI) | 1.32 (1.12 - 1.56) | 1.31 (1.11 - 1.52) | 1.38 (1.14 - 1.69) | 1.17 (.965 - 1.43) | 1.28 (1.08 - 1.53) | |||||
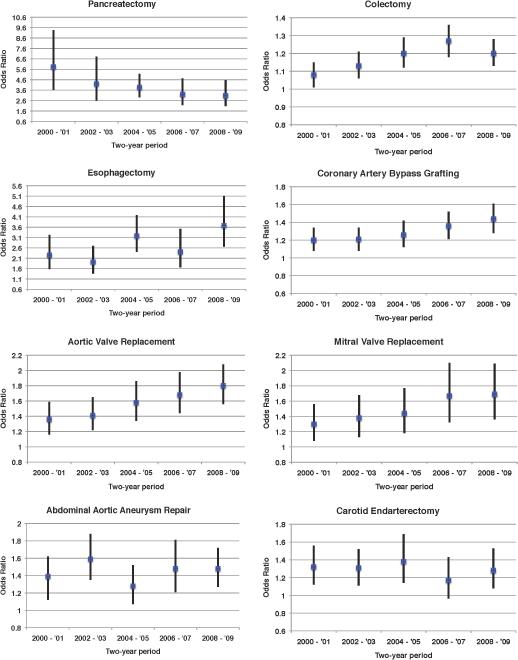
Figure 2 illustrates the trend in adjusted odds ratios between the years 2000 and 2009 for each procedure. Over the ten-year period, the risk-adjusted odds of mortality in very low volume hospitals increased for coronary artery bypass grafting, aortic valve replacement, mitral valve replacement, colectomy, and esophagectomy. Adjusted odds ratios remained stable for carotid endarterectomy and abdominal aortic aneurysm repair, and showed a substantial decrease for pancreatectomy.
Figure 2.
Trend over time of adjusted odds ratios and associated 95% confidence intervals of mortality in very low volume hospitals compared to very high volume hospitals, for each two-year period.
Sensitivity analyses using hierarchical logistic regression models with hospital-level random effects revealed similar results (in both estimates and significance) for nearly all procedures and years. This held true using both continuous and categorical measures of hospital volume. Only colectomy in the years 2000-2001 revealed a discrepancy, as the hierarchical model failed to reach statistical significance (AOR 1.06, 95% CI: 0.991 - 1.14, compared to 1.08, 95% CI: 1.01 - 1.15, for the logistic model with robust standard errors).
DISCUSSION
In a large, national dataset of Medicare patients, we found that both absolute and relative differences in adjusted mortality between hospitals with the lowest and highest volume persist in the modern era. This relationship endures despite significant improvements in adjusted mortality over the ten-year period. As shown in previous studies, the strength of the relationship varies between procedures. Given these findings, in the absence of more granular data regarding a hospital's performance, for certain high-risk procedures hospital volume remains a useful proxy of surgical quality.
Over the last ten years, a large body of literature supporting the presence of a hospital volume-outcome relationship, including numerous systematic reviews,18-25 has been developed. An early definitive systematic review on the subject was performed by Halm and colleagues and reported a significant association across a wide range of procedures and conditions.26 More recently, Pieper and colleagues performed a review and synthesis of systematic reviews on the topic.27 They evaluated systematic reviews of 14 different procedures across a wide range of specialties and found evidence to support a significant relationship in almost all procedures examined.
One particular study of recent data, however, has gained attention for failing to reveal a significant volume effect in four-high risk procedures traditionally thought to exhibit the relationship.11 In that work, LaPar and colleagues cite concerns regarding the characterization of volume and type of models used in previous publications, and conclude that hospital volume should not be used as a measure of hospital quality. While interesting, this study has been criticized for methodological concerns due to small sample size and potentially unstable statistical models.28 Nonetheless, in the current study, using a much larger dataset over a longer period of time, we demonstrate that despite significant improvements in surgical safety, the inverse relationship between hospital volume and operative mortality persists in the modern era. In our analysis, this relationship is significant regardless of how volume is characterized or the relationship is modeled.
This study has several limitations. First, given this analysis only includes Medicare patients, it may not be generalizable to patients younger than 65 years old. Nevertheless, this cohort includes a substantial number of all patients undergoing the procedures in question, and represents a subset of patients with increased risks of morbidity and mortality for whom these results may be most applicable. A second limitation is the potential misclassification of hospital volume when only Medicare procedures are considered. While some hospitals with high volumes of non-Medicare patients may be misclassified, this misclassification would bias our results toward the null hypothesis (no relationship between volume and mortality). Third, this study utilizes a large administrative database, which can be limited by miscoding and imprecision,29-31 and lacks the granular clinical details of patient disease process, illness severity, or type of surgical approach (for some operations). Although this lack of detail may limit determination of which surgical approach was used for an individual patient in certain operations, inclusion of patients undergoing both traditional and minimally invasive approaches and adjustment for operative approach when possible (endovascular AAA repair and laparoscopic colectomy) ensures that selection bias due to choice of surgical approach is minimized. Furthermore, while miscoding errors are likely to be random and therefore do not introduce bias into the results, certain inequalities were found within some study cohorts. For instance, more African Americans, patients with multiple comorbidities, and patients older than 75 years were treated at very low volume centers. Despite this, we were able to adjust for many important patient characteristics and conditions, and the results of these models coincide with numerous previously published reports.
Although the inverse relationship between hospital volume and operative mortality persists in the modern era, this does not mean that volume should be an exclusive measure of surgical quality. Instead, a balanced approach to quality measurement should be used. There are two main policy approaches to improving surgical quality; the particular measure chosen should be tailored to the clinical context. First, for high-risk procedures that are less frequently performed — such as esophagectomy and pancreatectomy — direct measures of surgical outcomes (mortality and morbidity rates) will not be statistically reliable metrics for policy decisions. In these settings, hospital volume remains a useful proxy measure of surgical quality and allows for selective referral of patients to the best performing hospitals. Indeed, recent work has shown that market concentration of certain procedures has improved surgical outcomes in high-risk patients.9
Alternatively, for frequently performed procedures such as cardiac surgery and colectomy, direct measurement of surgical outcomes (such as major and minor complications, and functional outcomes) offers reliable evidence of a hospital's surgical quality. For patients undergoing these types of procedures, continuous risk-adjusted outcomes measurement should be used to assess the quality of care. Moreover, when systematic data measurement is coupled with regular performance feedback in the form of a regional collaborative improvement program, significant improvements in the quality of care can be achieved. Numerous studies have reported decreased morbidity and mortality rates, and decreased costs, associated with regional quality collaboratives.32-36
There is no doubt surgical outcomes have improved over the last decade. Advances in operative technique, surgical checklists, performance-related payment, selective referral, and outcomes feedback have each contributed to these improvements in some way.10 As healthcare reform continues to exert pressure on providers to improve outcomes, leaders in surgical policy must consider quality measures within the context that they are used and appropriately match them to the best approach: selective referral or continuous quality improvement. The question is not whether a volume-outcome relationship exists, but how do we use that information to benefit patients. In any policy discussion, the potential benefits of selective referral highlighted in this paper must be balanced against the possible unintended consequences, including limits to access that could be most pronounced in disadvantaged populations. However, given the results of this study, it is essential that stakeholders maintain a multifaceted approach to quality improvement. One such component, at least for Medicare patients undergoing certain high-risk operations, is the use of hospital volume as a proxy measure for surgical quality.
Acknowledgments
Source of Funding: Dr. Reames is supported by a grant from the National Cancer Institute (5T32CA009672-23). Dr. Dimick is supported by grant from the National Institute on Aging (5R01AG039434-03). These funding sources had no involvement in the manuscript herein.
Footnotes
Conflict of Interest: BNR and AAG have no conflicts of interest or disclosures related to the content of this manuscript. Both JDB and JBD have an equity interest in ArborMetrix, Inc, which provides software and analytics for measuring hospital quality and efficiency. The company had no role in this study.
REFERENCES
- 1.Begg CB, Cramer LD, Hoskins WJ, et al. Impact of hospital volume on operative mortality for major cancer surgery. JAMA. 1998;280:1747–51. doi: 10.1001/jama.280.20.1747. [DOI] [PubMed] [Google Scholar]
- 2.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 3.Katz JN, Barrett J, Mahomed NN, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86-A:1909–16. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Hannan EL, Kilburn H, Jr., O'Donnell JF, et al. Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA. 1990;264:2768–74. [PubMed] [Google Scholar]
- 5.Lindenauer PK, Remus D, Roman S, et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356:486–96. doi: 10.1056/NEJMsa064964. [DOI] [PubMed] [Google Scholar]
- 6.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 7.Hannan EL, Cozzens K, King SB, 3rd, et al. The New York State cardiac registries: history, contributions, limitations, and lessons for future efforts to assess and publicly report healthcare outcomes. J Am Coll Cardiol. 2012;59:2309–16. doi: 10.1016/j.jacc.2011.12.051. [DOI] [PubMed] [Google Scholar]
- 8.Weiser TG, Semel ME, Simon AE, et al. In-hospital death following inpatient surgical procedures in the United States, 1996-2006. World J Surg. 2011;35:1950–6. doi: 10.1007/s00268-011-1169-5. [DOI] [PubMed] [Google Scholar]
- 9.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–37. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birkmeyer JD. Progress and challenges in improving surgical outcomes. Br J Surg. 2012;99:1467–9. doi: 10.1002/bjs.8933. [DOI] [PubMed] [Google Scholar]
- 11.Lapar DJ, Kron IL, Jones DR, et al. Hospital procedure volume should not be used as a measure of surgical quality. Ann Surg. 2012;256:606–15. doi: 10.1097/SLA.0b013e31826b4be6. [DOI] [PubMed] [Google Scholar]
- 12.Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program Home Page. 2013 Available at: http://www.mbsaqip.org/
- 13.Milstein A, Galvin RS, Delbanco SF, et al. Improving the safety of health care: the leapfrog initiative. Eff Clin Pract. 2000;3:313–6. [PubMed] [Google Scholar]
- 14.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130:415–22. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 15.Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and failure to rescue with high-risk surgery. Med Care. 2011;49:1076–81. doi: 10.1097/MLR.0b013e3182329b97. [DOI] [PubMed] [Google Scholar]
- 16.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 17.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Gandjour A, Bannenberg A, Lauterbach KW. Threshold volumes associated with higher survival in health care: a systematic review. Med Care. 2003;41:1129–41. doi: 10.1097/01.MLR.0000088301.06323.CA. [DOI] [PubMed] [Google Scholar]
- 19.Nuttall M, van der Meulen J, Phillips N, et al. A systematic review and critique of the literature relating hospital or surgeon volume to health outcomes for 3 urological cancer procedures. J Urol. 2004;172(6 Pt 1):2145–52. doi: 10.1097/01.ju.0000140257.05714.45. [DOI] [PubMed] [Google Scholar]
- 20.Burgers JS, Wittenberg J, Kallewaard M, et al. [Relationship between volume and quality of care for surgical interventions; results of a literature review]. Ned Tijdschr Geneeskd. 2007;151:2105–10. [PubMed] [Google Scholar]
- 21.Henebiens M, van den Broek TA, Vahl AC, et al. Relation between hospital volume and outcome of elective surgery for abdominal aortic aneurysm: a systematic review. Eur J Vasc Endovasc Surg. 2007;33:285–92. doi: 10.1016/j.ejvs.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 22.Lauder CI, Marlow NE, Maddern GJ, et al. Systematic review of the impact of volume of oesophagectomy on patient outcome. ANZ J Surg. 2010;80:317–23. doi: 10.1111/j.1445-2197.2010.05276.x. [DOI] [PubMed] [Google Scholar]
- 23.Wouters MW, Gooiker GA, van Sandick JW, et al. The volume-outcome relation in the surgical treatment of esophageal cancer: a systematic review and meta-analysis. Cancer. 2012;118:1754–63. doi: 10.1002/cncr.26383. [DOI] [PubMed] [Google Scholar]
- 24.Zevin B, Aggarwal R, Grantcharov TP. Volume-outcome association in bariatric surgery: a systematic review. Ann Surg. 2012;256:60–71. doi: 10.1097/SLA.0b013e3182554c62. [DOI] [PubMed] [Google Scholar]
- 25.Trinh QD, Bjartell A, Freedland SJ, et al. A Systematic Review of the Volume-Outcome Relationship for Radical Prostatectomy. Eur Urol. 2013 doi: 10.1016/j.eururo.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–20. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 27.Pieper D, Mathes T, Neugebauer E, et al. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: a systematic review of systematic reviews. J Am Coll Surg. 2013;216:1015–1025. e18. doi: 10.1016/j.jamcollsurg.2012.12.049. [DOI] [PubMed] [Google Scholar]
- 28.Birkmeyer JDRB, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Annals of Surgery Journal Club. 2013 Available at: http://journals.lww.com/annalsofsurgery/blog/annalsofsurgeryjournalclub/pages/default.aspx. Accessed July 12th, 2013.
- 29.Jencks SF, Williams DK, Kay TL. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. JAMA. 1988;260:2240–6. [PubMed] [Google Scholar]
- 30.Iezzoni LI, Foley SM, Daley J, et al. Comorbidities, complications, and coding bias. Does the number of diagnosis codes matter in predicting in-hospital mortality? JAMA. 1992;267:2197–203. doi: 10.1001/jama.267.16.2197. [DOI] [PubMed] [Google Scholar]
- 31.Fisher ES, Whaley FS, Krushat WM, et al. The accuracy of Medicare's hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82:243–8. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O'Connor GT, Plume SK, Olmstead EM, et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. JAMA. 1996;275:841–6. [PubMed] [Google Scholar]
- 33.Ingraham AM, Richards KE, Hall BL, et al. Quality improvement in surgery: the American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44:251–67. doi: 10.1016/j.yasu.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Share DA, Campbell DA, Birkmeyer N, et al. How a regional collaborative of hospitals and physicians in Michigan cut costs and improved the quality of care. Health Aff (Millwood) 2011;30:636–45. doi: 10.1377/hlthaff.2010.0526. [DOI] [PubMed] [Google Scholar]
- 35.Guillamondegui OD, Gunter OL, Hines L, et al. Using the National Surgical Quality Improvement Program and the Tennessee Surgical Quality Collaborative to improve surgical outcomes. J Am Coll Surg. 2012;214:709–14. doi: 10.1016/j.jamcollsurg.2011.12.012. discussion 714-6. [DOI] [PubMed] [Google Scholar]
- 36.Finks JF, Kole KL, Yenumula PR, et al. Predicting risk for serious complications with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg. 2011;254:633–40. doi: 10.1097/SLA.0b013e318230058c. [DOI] [PubMed] [Google Scholar]