Abstract
Background
Engaging in thought suppression as a coping mechanism has been associated with higher rates of anxiety and depressive disorders in younger adults. Homebound older adults are a population of elders experiencing poor health and high levels of depression and anxiety. It is unclear the extent to which psychological factors, such as thought suppression, are associated with distress, given that their health and disability status may be more salient. The aim of this study was to investigate thought suppression in relation to anxiety and depressive symptoms in homebound older adults.
Methods
Participants (N = 142) were clients of home-based case management services delivered by aging service agencies in Florida. Participants were administered a research interview that included the White Bear Suppression Inventory, Structured Clinical Interview for DSM-IV Diagnosis (SCID), Brief Symptom Inventory-18 (BSI-18), and Modified Mini-Mental Status Examination (3MS). Case managers provided standard assessments containing functional and health status of the participant.
Results
After controlling for physical health and cognitive functioning, thought suppression was significantly associated with higher likelihood of clinically significant somatic, depressive, and anxiety symptoms on the BSI-18. Thought suppression was also associated with meeting criteria for a SCID depressive or adjustment disorder. Engaging in thought suppression was associated with worse mental health in this sample of homebound older adults even after taking into account physical health, disability, and cognitive functioning.
Conclusions
These findings suggest the need to develop and test interventions that may address thought suppression as a coping mechanism.
Keywords: homebound elderly, thought suppression, anxiety, depression
Approximately 11% of Medicare recipients experience chronic illness and substantial disability, rendering them in need of formal or informal care to prevent institutionalization.[1] In 2009, Medicare spent approximately 72.2 billion dollars on home health care.[2] Additionally, policymakers have identified aging in the home as a high priority as evidenced by recent legislation that supports home health services in Medicare.[3] The importance of and costs associated with home health care will grow as the number of older adults continues to increase.
Homebound older adults commonly experience a number of stressors such as chronic illness, functional impairment, and cognitive impairment.[4] As a result, this population is at high risk for experiencing psychological distress. Studies suggest that approximately 40.5% experience a psychiatric disorder,[5] with estimates suggesting that 13.7% of older adults in homecare meet criteria for DSM-IV depressive disorders[6] and as many as 31.6% meet criteria for an anxiety disorder.[7] Both depression and anxiety in older adulthood are associated with adverse outcomes. Depression and anxiety have been associated with greater functional impairment,[8,9] higher rates of suicide,[10,11] cognitive impairment,[12,13] higher health care costs,[14,15] higher risk of nursing home place-ment,[16] and decreased quality of life.[17,18] Additionally, depression and anxiety commonly are comorbid in older adulthood.[19,20] Comorbid anxiety is associated with poorer outcomes such as longer time to respond to treatment for depression.[21] Given these high societal costs associated with depression and anxiety, interventions to decrease suffering and prevent the adverse outcomes associated with these disorders are important.
Thought suppression is a strategy to cope with unwanted internal experiences (cognitions or emotions) in which the individual actively attempts not to think about the unwanted thought or feeling that they are experiencing. This process, however, is paradoxical. Research suggests a “rebound effect,” in which the individual actually thinks about the suppressed thought with greater frequency and intensity.[22] In addition to the rebound effect, engaging in thought suppression may lead to distress in that it may also be representative of using avoidance coping to deal with stressors. Avoidance coping styles, which may include other avoidance coping strategies such as cognitive avoidance (rumination/worry) and behavioral avoidance of situations that evoke distressing thoughts and emotions (withdrawel, procrastination), have been demonstrated to be associated with higher rates of distress. Greater use of thought suppression has been implicated as a causal or maintenance factor for a number of psychological disorders including both anxiety and depression.[23] Studies suggest that the association between thought suppression and adverse outcomes persists into older adulthood. Thought suppression has been associated with decreased meaning in life in community dwelling older adults,[24] suicidal ideation in depressed older adults with personality disorders,[25] and poorer outcomes following depression treatment.[26] Additionally, avoidance of trauma-related thoughts may mediate the association between past trauma exposure and distress later in life.[27]
Research examining risk factors for distress in homebound populations have generally studied the association between medical factors such as disability and worse health and depression.[28,29] These studies, however, have not investigated potential psychological factors such as thought suppression in relation to current distress. Given the high rate of chronic illness and disability in this population, one may posit that these medical factors may be more important to the current well-being of homebound elders than psychological risk factors such as engaging in thought suppression. Alternatively, studies have shown that most individuals who are experiencing high levels of chronic illness, disability, and poor health do not develop mental health problems. This suggests that psychological vulnerability factors also may be important to current well-being. To our knowledge, no studies have investigated psychological vulnerability factors such as engaging in thought suppression in relation to anxiety or depressive symptoms in older homecare patients.
The purpose of this study is to investigate the association between thought suppression and the mental health of homebound older adults. It is hypothesized that using greater amounts of thought suppression will be associated with worse mental health and greater distress, even after controlling for health, cognition, and disability.
Methods
Data Source and Sample
Data for these analyses were drawn from a larger project investigating the mental health needs of homebound older adults. A brief summary of the study design, sampling procedures, measures, and other procedures are presented below; a more detailed description appears in another article.[30] A sample of 142 older adults receiving in-home services through aging service agencies participated in this study. Individuals were eligible to receive these in-home services based on assessment by case managers and physicians. Individuals' eligibility for these services was determined by a physician based on their physical health in that they are at high risk for nursing home placement and unable to care for themselves at home without assistance. Case managers invited these older adults receiving aging services to participate in the study during routine home visits. Interested individuals were contacted by study staff. Standardized in-person assessments were conducted in the participant's home with study associates. Data were also taken from standardized assessments administered by case managers. Individuals were eligible to participate in this study if they were 60 years or older, spoke English, and did not have a known diagnosis of dementia per the case manager.
In total, 231 individuals agreed to be contacted by the research team, and 142 individuals completed the interview, resulting in a response rate of 61.5%. Of those who did not complete the interview, 70 refused primarily due to health problems, 11 were unable to participate due to cognitive impairment, 6 were unable to be contacted after numerous attempts, and 2 died before scheduling interviews, resulting in a sample of N = 142. Case managers were asked to invite every client that met the inclusion criteria to participate in the study. Unfortunately, due to high work demands of the case managers, we were unable to gather data on how many individuals refused to be contacted by the study team. To assess the representativeness of the current sample, the participants in this investigation were compared with the demographics of the entire population of clients in this region of Florida. When compared with the larger population, the current sample is younger, less ethnically diverse, and has fewer chronic medical conditions than the overall population older adults receiving in-home aging services. Please refer to Gum et al.[30] for further discussion of the sample.
All study procedures were approved by the University of South Florida Institutional Review Board, and all participants provided written informed consent.
Measures
Demographic variables
Participants self-reported their age, gender, race, ethnicity, marital status, and education.
Brief Symptom Inventory-18 [BSI-18; [31]]
The BSI-18 measures somatic, depressive, and anxiety symptoms during the past week on a five-point scale ranging from “0, not at all” to “4, extremely”. The total score ranges from 0 to 72 and the somatic, depression, and anxiety subscale scores range from 0 to 24, with higher scores representing more distress. The BSI-18 manual provides normative data on the BSI-18 and suggests adopting a T-score of 63 as a cut point to represent caseness on each subscale. The BSI-18 has been shown to be reliable and valid with homebound older adults.[32] Cronbach's αs were .69 for somatic, .87 for depression, .81 for anxiety, and .90 for the total score.
Diagnosis of depressive and anxiety disorders
Current depressive and anxiety disorders were assessed using the Structured Clinical Interview for DSM-IV [SCID; [33]]. The SCID was administered by bachelor's level research associates who were trained and supervised by a licensed clinical psychologist (A.G.). The following disorders were assessed: major depressive disorder, dysthymic disorder, depressive disorder not otherwise specified, depressive disorder due to a medical condition or substance, panic disorder, agoraphobia, specific phobia, social phobia, obsessive-compulsive disorder, posttraumatic stress disorder, generalized anxiety disorder, anxiety disorder not otherwise specified, and anxiety due to a general medical condition or substance. All interviews were audiotaped (unless refused by the participant) and a random 20% of the interviews were rated by A.G. to assess inter-rater reliability. Kappa's ranged from .61 to 1.00 across disorders, representing high inter-rater reliability.[34]
Thought suppression
Thought suppression was measured using the White Bear Suppression Inventory [WBSI; [35]]. The WBSI contains 15 items which participants rate on a 5-point scale (from A, “strongly disagree” to E, “strongly agree”). Research on the psychometric properties of the WBSI suggests that there are two subscales: a thought suppression subscale and a thought intrusion subscale.[36] The intrusive thought items measure intrusive or unwanted thoughts rather than attempts to suppress these thoughts. In a review of the WBSI items, the following items have comprised the thought suppression factor across all psychometric studies: 1 (“There are things I prefer not to think about”), 10 (“Sometimes I stay busy just to keep thoughts from intruding on my mind”), 11 (“There are things that I try not to think about”), 13 (“I often do things to distract myself from my thoughts”), and 14 (“I have thoughts that I try to avoid”).[36] To investigate thought suppression as distinct from a combination of suppressions and intrusions, we used both the suppression subscale as well as the full WBSI. Cronbach's α for the full WBSI was .86 and for the 5-item suppression subscale was .64.
Indicators of physical health
Health variables included the following: (a) number of prescription non-psychotropic medications; (b) number of chronic medical conditions (cancer, diabetes, emphysema, heart problems, liver problems, stroke, Parkinson's disease, allergies, asthma, bladder/kidney problems, high blood pressure, gall bladder problems, or thyroid problems); and (c) functional impairment as measured by a combined total of number of limitations in activities of daily living (ADL; bathing or showering, dressing, eating, getting in or out of bed or chairs, walking, and using the toilet) and instrumental activities of daily living (IADL; using the telephone, shopping, preparing food, housekeeping, laundry, transportation, taking medications, and handling finances). Number of prescribed medications was measured during the assessment with the research associate by asking the participant to provide a list of all medications that were being taken (sample ranged from 0 to 20). Number of chronic medical conditions (sample ranged from 1 to 15) and ADL and IADL limitations (sample ranged from 2 to 14) were derived from the case manager's assessment nearest in time to the research interview.
Modified Mini Mental Status Exam [3MS]. [37]
The 3MS is a modification of the Mini-Mental Status Examination[38] and is a measure of cognitive functioning. The 3MS includes items assessing delayed free and cued recall, recognition memory, and executive function. The 3MS has strong validity and reliability,[37] and scores range from 0 to 100. Cronbach's alpha in this sample was .72.
Data Analysis
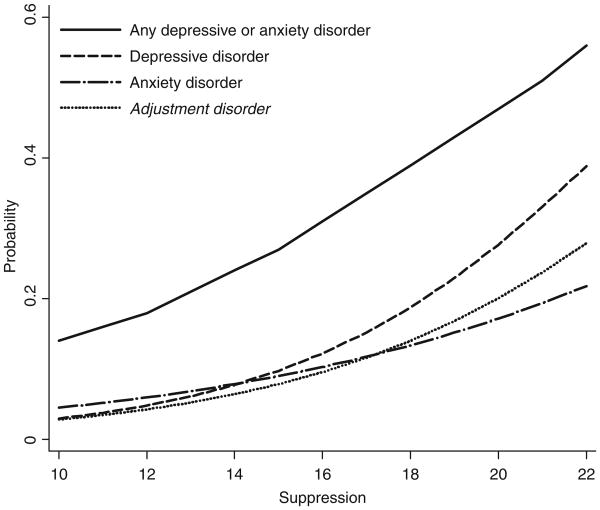
Descriptive statistics for all variables were computed. The BSI-18 data were significantly skewed; thus, the data were dichotomized using the caseness rule of a T-score of 63 to represent clinically significant distress.[31] To assess the study hypotheses, logistic regression analysis was used to examine the associations between thought suppression, BSI-18 caseness (no/yes), and the presence of a SCID disorder (no/yes). Each model was run with the entire WBSI as well as the 5-item suppression subscale. Results were the same for all but two outcomes (anxiety disorder and adjustment disorder). Thus, to be conservative, only the models with the thought suppression subscale are presented. For each outcome, the final regression model included the following covariates: age (60–93), gender (0 = male, 1 = female), number of chronic medical conditions (1–15), combined number of ADL and IADL limitations (2–14), number of non-psychotropic medications (0–20), 3MS scores (64–100), and WBSI thought suppression subscale (0–25). All continuous covariates were centered on the mean. Odds ratios were reported for all significant covariates. For the thought suppression scale, predicted probabilities were calculated for being identified as a case on the BSI-18 and meeting criteria for SCID diagnoses after controlling for other covariates. These predicted probabilities were graphed in relation to thought suppression subscale score.
Results
Sample Characteristic and Severity of Symptoms and Scid Diagnoses
Table 1 provides descriptive information about the sample. Current depression, anxiety, and somatic symptom severity as well as frequency of DSM-IV diagnoses are provided in Table 1. On the BSI-18, 64 (45.1%) were identified as experiencing clinically significant somatic symptoms, 28 (19.7%) were experiencing clinically significant depressive symptoms, and 20 (14.1%) were experiencing clinically significant anxiety symptoms. Of the participants, 17 (12.0%) met criteria for a SCID depressive disorder and 17 (12.0%) met criteria for an anxiety disorder. Of those with an anxiety disorder, 6 (2.4%) had specific phobia, 4 (2.8%) panic disorder, 3 (2.1%) posttraumatic stress disorder, 3 (2.1%) social phobia, 2 (1.4%) agoraphobia, and one (.7%) anxiety due to a general medical condition. Five (3.5%) participants met criteria for both a depressive and anxiety disorder.
TABLE 1. Sample characteristics.
| N (%) or M (SD) | |
|---|---|
| Age | 74.73 (8.32) |
| Female | 113 (79.6) |
| Race | |
| Caucasian | 105 (73.9) |
| African American | 28 (19.7) |
| 3MS | 88.13 (8.55) |
| Health | |
| Number of non-psychotropic medications | 7.54 (4.49) |
| Number of chronic health conditions | 5.05 (2.62) |
| ADL impairments | 2.43 (1.91) |
| IADL impairments | 5.25 (1.48) |
| Mental health | |
| BSI-18 somatic case | 64 (45.1) |
| BSI-18 depression case | 28 (19.7) |
| BSI-18 anxiety case | 20 (14.1) |
| Any SCID disorder | 31 (21.8) |
| Depressive disorder | 17 (12.0) |
| Anxiety disorder | 17 (12.0) |
| Adjustment disorder | 17 (12.0) |
| WBSI total | 46.96 (11.04) |
| WBSI suppression subscale | 16.36 (3.91) |
ADL, activities of daily living; IADL, instrumental activities of daily living.
Logistic Regression of Somatic, Depressive, and Anxiety Symptoms
Table 2 displays results from the logistic regression investigating current distress as measured by the BSI-18 in relation to thought suppression, after controlling for covariates. For BSI-18 somatic caseness, the final multivariate logistic model was statistically significant, (χ2 (7) = 30.22, P<.001), and the model was found to accurately classify 71.8% of participants. In the multivariate model, thought suppression (OR = 1.139, 95% CI = 1.024–1.267, P = .017), number of nonpsychotropic medications (OR = 1.118, 95% CI = 1.020–1.226, P = .018), and number of chronic medical conditions (OR = 1.257, 95% CI = 1.059–1.492, P = .009) were associated with increased likelihood of experiencing clinically significant somatic symptoms.
TABLE 2. Thought suppression as a predictor of mental health problems after controlling for demographics, health, and cognitive performance.
| Odds ratio | Standard error | 95% Confidence interval | P | |||
|---|---|---|---|---|---|---|
| BSI-18 Caseness Outcome | ||||||
| Somatic | 1.139 | .054 | 1.024 | 1.267 | .017 | * |
| Depression | 1.243 | .073 | 1.077 | 1.435 | .003 | ** |
| Anxiety | 1.362 | .091 | 1.139 | 1.628 | .001 | ** |
| Psychiatric Disorder Outcome | ||||||
| Any | 1.189 | .067 | 1.043 | 1.356 | .010 | ** |
| Depression | 1.287 | .095 | 1.069 | 1.550 | .008 | ** |
| Anxiety | 1.160 | .082 | .987 | 1.363 | .072 | |
| Adjustment | 1.242 | .085 | 1.052 | 1.466 | .011 | * |
P<0.01;
P<0.05.
For BSI-18 depression caseness, the final multi-variate model was statistically significant, (χ2 (7) = 19.31, P = .007), and the model accurately classified 71.8% of participants. Higher thought suppression (OR = 1.243, 95% CI = 1.077–1.435, P = .003) was associated with increased likelihood of experiencing clinically significant depressive symptoms.
For BSI-18 anxiety caseness, the final multivariate model was statistically significant, (χ2 (7) = 26.133, P<.001), and the model accurately classified 85.9% of participants. Thought suppression (OR = 1.362, 95% CI = 1.139–1.628, P = .001) and poor cognitive performance (OR = .936, 95% CI = .877–.999, P = .049) were associated with increased likelihood of experiencing clinically significant anxiety symptoms.
Logistic Regression of Depressive, Anxiety, and Adjustment Disorders
Table 2 displays results from the logistic regression regressions investigating the relationship between thought suppression and psychiatric disorder, after controlling for covariates. The multivariate model with the outcome of meeting criteria for any Axis I disorder was statistically significant (χ2 (7) = 19.722, P = .006), and the model accurately classified 78.3% of participants. Participants were more likely to meet criteria for an Axis I disorder if they had greater thought suppression (OR = 1.189, 95% CI = 1.043–1.356, P = .017). Participants with more chronic medical conditions were also more likely to meet criteria for an Axis I disorder (OR = 1.303, 95% CI 1.081–1.570, P = 0.006.
The multivariate model with the outcome of meeting criteria for a depressive disorder was statistically significant, (χ2 (7) = 20.776, P = 0.004), and the model accurately classified 90.1% of participants. Participants were more likely to meet criteria for a depressive disorder if they used higher levels of thought suppression (OR = 1.287, 95% CI = 1.069–1.550, P = .008) and had a higher number of chronic medical conditions (OR = 1.337, 95% CI = 1.055–1.693, P = .016).
The multivariate model with the outcome of meeting criteria for an anxiety disorder was also statistically significant, (χ2 (7) = 16.456, P<.021), and the model accurately classified 87.7% of participants. Thought suppression was not associated with increased likelihood of meeting criteria for an anxiety disorder (OR = 1.160, 95% CI = 0.987–1.363, P = .072).
The multivariate model with the outcome of meeting criteria for an adjustment disorder was not statistically significant, (χ2 (7) = 12.411, P = .088), although the model accurately classified 87.3% of participants. Thought suppression (OR = 1.24, 95% CI = 1.052– 1.466, P = .011) was associated with increased probability of meeting criteria for an adjustment disorder. Figure 1 displays the predicted probabilities of meeting criteria for a psychiatric disorder by thought suppression after controlling for all covariates.
Figure 1.
Predicted probability of meeting criteria for a psychiatric disorder in relation to thought suppression after controlling for demographics, health, disability, and cognitive performance.
Discussion
This cross-sectional study investigated engaging in thought suppression in relation to current distress in homebound older adults. After controlling for physical health and cognitive functioning, greater use of thought suppression was associated with higher probability of experiencing clinically significant somatic, depressive, and anxiety symptoms as measured by the BSI-18. Furthermore, engaging in thought suppression was also associated with being more likely to meet criteria for any psychiatric disorder, any depressive disorder, and current adjustment disorder. These findings are consistent with the study hypotheses.
Thought suppression was associated with more depressive symptoms and greater likelihood of meeting criteria for a depressive disorder. This association was independent of current physical health, disability, and cognitive functioning. These findings are consistent with theories and previous research implicating thought suppression in depression in younger adults and in less disabled older adults. Thought suppression was also associated with greater symptoms of anxiety as measured by the BSI-18. The association between thought suppression and meeting criteria for an anxiety disorder, however did not reach statistical significance. This finding is consistent with studies with younger adults that have demonstrated that engaging in thought suppression is also associated with anxiety.[23,39]
One interpretation of these findings is that efforts to avoid distressing cognitions or emotions are associated with increased levels of distress, independent of physical, cognitive, and functional health status. These results are consistent with studies that demonstrate that attempting to suppress thoughts results in a “rebound effect” in which the person experiences the suppressed thought with more frequency and greater intensity. Additionally, engaging in though suppression may be a proxy for broader general usage of avoidance, both cognitive and behavioral to cope with stressors. These avoidance behaviors may be reinforced because they typically immediately are associated with decreased distress; however the overall problem which is causing distress remains. These avoidance behaviors may potentially increase the impact of stressors in the environment. For example, stressful life events that may ameliorate by active problem solving may persist due to avoidance coping. Additionally, behavioral avoidance of emotionally arousing activities may result in low social support, and less engagement in meaningful activities.
It is possible that engaging in thought suppression is an important factor in the etiology or maintenance factor of emotional disorders such as depression and anxiety in homebound elders. Interestingly, this association was independent of physical health, functional impairment, and cognitive abilities. These findings suggest that psychological coping factors such as thought suppression may contribute as much to the development to anxiety and depression in this population as do physical health and functional impairment.
These results also have potentially important clinical implications for the treatment of depression and anxiety in homebound older adults. They suggest that psychosocial interventions that target psychological coping factors could be beneficial for treating depression and anxiety, even in older adults who are experiencing significant chronic illness and disability. Research needs to be done to empirically test exposure or mindfulness based interventions in the home to examine if these interventions are effective with this population. Furthermore, it may be possible that these treatments are possible and effective in academic settings, however, not feasible to be implemented in standard clinical settings. Thus, in addition to testing the effectiveness of these treatments, research needs to be done to examine ways to successfully implement these treatments into home health and other current home services that provide care to this important population.
This study has several limitations. First, the cross-sectional design does not permit conclusions of causality. We are unable to determine if increased thought suppression occurred before the development of distress or if increased symptoms resulted in more thought suppression. It is possible that distress may cause thought suppression, or the two factors may have a bi-directional relationship; additional longitudinal research is needed to investigate this alternative explanation. Second, the use of self-report measures of thought suppression is not optimal, and more objective measures of thought suppression would be preferable. Despite the lack of objective measures, thought suppression as measured conservatively by the thought suppression subscale of the WBSI was consistently associated with increased distress, suggesting robustness of these findings. Finally, the sample was one of convenience; case managers invited clients to participate, limiting generalizability.
The primary strength of this study is that it is the first to examine thought suppression in a homebound population of older adults. Additionally, this is the first study with any sample of older adults to investigate thought suppression using the more psychometrically valid subscale of the WBSI. Another strength is the focus on multiple domains of distress, including depression, anxiety, and somatic symptoms. Further longitudinal or experimental research should investigate whether thought suppression plays a causal or maintenance role in distress in homebound older people.
If additional research confirms that thought suppression is an underlying mechanism that maintains anxiety and depression, transdiagnostic psychosocial interventions that address this underlying mechanism may be appropriate models for treatment. Such transdiagnostic interventions for depression and anxiety in homebound older adults would potentially be more efficient than disorder-specific treatments[40] and is consistent with recent developments in psychotherapy research in younger adults with depression or anxiety.[41,42] They would also be consistent with the fact that anxiety and depression commonly co-occur, and a transdiagnostic approach to treatment would potentially be easier to implement into existing home health services, making treatment more accessible to this underserved population.
Acknowledgments
This study was supported by a University of South Florida New Researcher Grant awarded to Amber M. Gum, Ph.D.
The authors disclose the following financial relationships within the past 3 years: Contract grant sponsor: University of South Florida New Researcher Grant.
References
- 1.Administration on Aging. A Profile of Older Americans. Washington, D.C.: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- 2.Centers for Medicare and Medicaid Services. National Expenditure Projections 2009–2019. Washington D.C.: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- 3.111th Cong. 2nd session. 2010. Independence at home medical practice demonstration program. [Google Scholar]
- 4.Qiu WQ, Dean M, Liu T, et al. Physical and mental health of homebound older adults: an overlooked population. J Am Geriatr Soc. 2010;58:2423–2428. doi: 10.1111/j.1532-5415.2010.03161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li LW, Conwell Y. Mental health status of home care elders in Michigan. Gerontologist. 2007;47:528–534. doi: 10.1093/geront/47.4.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 7.Preville M, Cote G, Boyer R, Hebert R. Detection of depression and anxiety disorders by home care nurses. Aging Ment Health. 2004;8:400–409. doi: 10.1080/13607860410001725009. [DOI] [PubMed] [Google Scholar]
- 8.Brenes GA, Guralnik JM, Williamson JD, et al. The influence of anxiety on the progression of disability. J Am Geriatr Soc. 2005;53:34–39. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- 10.Diefenbach GJ, Woolley SB, Goethe JW. The association between self-reported anxiety symptoms and suicidality. J Nerv Ment Dis. 2009;197:92–97. doi: 10.1097/NMD.0b013e318196127c. [DOI] [PubMed] [Google Scholar]
- 11.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- 12.Dotson VM, Resnick SM, Zonderman AB. Differential association of concurrent, baseline, and average depressive symptoms with cognitive decline in older adults. Am J Geriatr Psychiatry. 2008;16:318–330. doi: 10.1097/JGP.0b013e3181662a9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sinoff G, Werner P. Anxiety disorder and accompanying subjective memory loss in the elderly as a predictor of future cognitive decline. Int J Geriatr Psychiatry. 2003;18:951–959. doi: 10.1002/gps.1004. [DOI] [PubMed] [Google Scholar]
- 14.Porensky EK, Dew MA, Karp JF, et al. The burden of late-life generalized anxiety disorder: effects on disability, health-related quality of life, and healthcare utilization. Am J Geriatr Psychiatry. 2009;17:473–482. doi: 10.1097/jgp.0b013e31819b87b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Unutzer J, Patrick DL, Simon G, et al. Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. J Am Med Assoc. 1997;277:1618–1623. doi: 10.1001/jama.1997.03540440052032. [DOI] [PubMed] [Google Scholar]
- 16.Gibbons L, Teri L, Logsdon R, et al. Anxiety symptoms as predictors of nursing home placement in patients with Alzheimer's disease. J Clin Geropsychol. 2002;8:335–342. [Google Scholar]
- 17.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 18.Wetherell JL, Thorp SR, Patterson TL, et al. Quality of life in geriatric generalized anxiety disorder: a preliminary investigation. J Psychiatr Res. 2004;38:305–312. doi: 10.1016/j.jpsychires.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Gum AM, Cheavens JS. Psychiatric comorbidity and depression in older adults. Curr Psychiatry Rep. 2008;10:23–29. doi: 10.1007/s11920-008-0006-5. [DOI] [PubMed] [Google Scholar]
- 20.Lenze EJ, Mulsant BH, Shear MK, et al. Comorbidity of depression and anxiety disorders in later life. Depress Anxiety. 2001;14:86–93. doi: 10.1002/da.1050. [DOI] [PubMed] [Google Scholar]
- 21.Hybels CF, Steffens DC, McQuoid DR, Rama Krishnan KR. Residual symptoms in older patients treated for major depression. Int J Geriatr Psychiatry. 2005;20:1196–1202. doi: 10.1002/gps.1418. [DOI] [PubMed] [Google Scholar]
- 22.Wenzlaff RM, Wegner DM. Thought suppression. Annu Rev Psychol. 2000;51:59–91. doi: 10.1146/annurev.psych.51.1.59. [DOI] [PubMed] [Google Scholar]
- 23.Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 24.Krause N. Thought suppression and meaning in life: a longitudinal investigation. Int J Aging Hum Dev. 2007;64:67–82. doi: 10.2190/2044-390U-7106-5610. [DOI] [PubMed] [Google Scholar]
- 25.Cukrowicz KC, Ekblad AG, Cheavens JS, et al. Coping and thought suppression as predictors of suicidal ideation in depressed older adults with personality disorders. Aging Ment Health. 2008;12:149–157. doi: 10.1080/13607860801936714. [DOI] [PubMed] [Google Scholar]
- 26.Rosenthal MZ, Cheavens JS, Compton JS, et al. Thought suppression and treatment outcome in late-life depression. Aging Ment Health. 2005;9:35–39. doi: 10.1080/13607860512331334040. [DOI] [PubMed] [Google Scholar]
- 27.Dulin PL, Passmore T. Avoidance of potentially traumatic stimuli mediates the relationship between accumulated lifetime trauma and late-life depression and anxiety. J Trauma Stress. 2010;23:296–299. doi: 10.1002/jts.20512. [DOI] [PubMed] [Google Scholar]
- 28.Weinberger MI, Raue PJ, Meyers BS, Bruce ML. Predictors of new onset depression in medically ill, disabled older adults at 1 year follow-up. Am J Geriatr Psychiatry. 2009;17:802–809. doi: 10.1097/JGP.0b013e3181b0481a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen-Mansfield J, Shmotkin D, Hazan H. The effect of homebound status on older persons. J Am Geriatr Soc. 2010;58:2358–2362. doi: 10.1111/j.1532-5415.2010.03172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gum AM, Petkus A, McDougal SJ, et al. Behavioral health needs and problem recognition by older adults receiving home-based aging services. Int J Geriatr Psychiatry. 2009;24:400–408. doi: 10.1002/gps.2135. [DOI] [PubMed] [Google Scholar]
- 31.Derogatis L. Brief Symptom Inventory (BSI) 18: Administration, Scoring, And Procedures Manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- 32.Petkus AJ, Gum AM, Small B, et al. Evaluation of the factor structure and psychometric properties of the Brief Symptom Inventory-18 with homebound older adults. Int J Geriatr Psychiatry. 2010;25:578–587. doi: 10.1002/gps.2377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.First MB, Spitzer RL, Miriam G, Williams JB. Structured Clinical Interview for the DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with Psychotic Screen. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 34.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 35.Wegner DM, Zanakos S. Chronic thought suppression. J Pers. 1994;62:616–640. doi: 10.1111/j.1467-6494.1994.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 36.Schmidt RE, Gay P, Courvoisier D, et al. Anatomy of the White Bear Suppression Inventory (WBSI): a review of previous findings and a new approach. J Pers Assess. 2009;91:323–330. doi: 10.1080/00223890902935738. [DOI] [PubMed] [Google Scholar]
- 37.Teng EL, Chui HC. Manual for the Administration and Scoring of the Modified Mini-Mental State (3MS) Test. Los Angeles, CA: University of Southern California School of Medicine; 1991. [Google Scholar]
- 38.Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental State’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 39.Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: a transdiagnostic examination. Behav Res Ther. 2010;48:974–983. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Petkus A, Wetherell J. Acceptance and commitment therapy with older adults: Rationale and considerations. Cogn Behav Pract. 2011 doi: 10.1016/j.cbpra.2011.07.004. Early View Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 42.Wilamoska Z, Thompson-Hollands J, Fairholme C, et al. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety. 2010;27:882–890. doi: 10.1002/da.20735. [DOI] [PubMed] [Google Scholar]