Abstract
Patients with hepatocellular carcinoma (HCC) often experience hepatic morbidity. Hepatitis B virus (HBV) reactivation is well documented as a serious hepatic morbidity during anti-cancer therapy. Reported rates of HBV reactivation in chronic carriers with HCC undergoing chemotherapy range from 4%-67%. Apart from chemotherapy, HBV reactivation has been increasingly identified in settings of hepatectomy and local ablation therapies. The rates of HBV reactivation vary with different levels of immunosuppression and depend on treatment, viral factors, and patient characteristics. The principal concern relating to reactivation is that a substantial proportion of patients with reactivation suffer from liver dysfunction during therapy, which often leads to disruption of planned, potentially life-prolonging treatments, adversely affecting the patients’ final outcome. The first step in the management of HBV reactivation is identification of patients at risk of reactivation by testing for HBV serology prior to commencing anti-cancer therapy. Although it is a serious complication, HBV reactivation is preventable with prophylactic anti-HBV drugs. Multiple publications have shown the benefit of prophylactic or preemptive antiviral therapy in this setting and justified such an approach before the start of therapy. Given the tumors and underlying cirrhosis, long-term use of antivirals with high potency and low risk of resistance is recommended in patients with HCC. This topic review will summarize the epidemiology, pathogenesis, and clinical issues related to HBV reactivation in HCC patients, and will discuss proper management against HBV reactivation during anti-cancer therapy for HCC.
Keywords: Hepatitis B virus, Virus activation, Hepatic morbidity, Hepatocellular carcinoma, Immunosuppression
Core tip: Hepatitis B virus (HBV) reactivation is a serious hepatic morbidity during anti-cancer therapy. The principal concern relating to reactivation is that a substantial proportion of patients with reactivation suffer from liver dysfunction, which often leads to disruption of planned, potentially life-prolonging treatments, adversely affecting the patients’ final outcome. Given the tumors and underlying cirrhosis, awareness of the management of reactivation is crucial for patients with hepatocellular carcinoma (HCC). This topic provides a summary of the literature and discusses clinical issues of HBV reactivation in HCC patients that are distinct from those in other cancer patients.
INTRODUCTION
Cancer patients often get viral infections that may be fatal, either directly due to the impaired host immunity that is accompanied by the underlying malignancy or indirectly due to immunosuppressive anti-cancer therapy. Among the viruses, hepatitis B virus (HBV) reactivation is one of the most serious complications of chemotherapy and is associated with morbidity and mortality in cancer patients. A substantial proportion of patients suffering from HBV reactivation experience liver dysfunction during anti-cancer therapy; liver dysfunction may lead to disruptions in scheduled treatments, thus potentially affecting patient outcome. Although earlier reports of HBV reactivation focused on patients with hematologic malignancy, reactivation is now increasingly seen in patients with other malignancies. In cancer management using more complex treatment protocols, HBV reactivation occurs in varying clinical instances and appears to be more common.
Over the past decade, there has been a growing body of evidence on HBV reactivation in patients with hepatocellular carcinoma (HCC). Pooled data suggest that the reactivation of HBV is not infrequent in chronic HBV carriers with HCC who are undergoing anti-cancer therapy. For patients with HBV-related HCC, HBV reactivation and subsequent hepatic morbidity are among negative prognostic indicators for HCC survival. Awareness of prevention and management of HBV reactivation in patients with HBV-related HCC is crucial so that patients may continue to receive potentially life-saving treatments. In this review, the author introduces the epidemiology, pathogenesis, risk factors, and clinical manifestations of HBV reactivation in HCC patients that are distinct from those in other cancer patients and discuss the proper management of HBV reactivation during anti-cancer therapy.
HBV REACTIVATION AND DEGREE OF IMMUNOSUPPRESSION
Although reactivation of HBV can occur spontaneously, it commonly occurs following chemotherapy or immune-suppressive therapy. This implies that the dampening of immune mechanisms by anti-cancer therapies plays key roles in inducing viral reactivation in these patients. Not all patients with viral reactivation develop hepatitis; with the same treatment, some patients with reactivation develop severe hepatic injury while others do not. In this situation, the degree of immunosuppression induced by treatment is highly implicated in the frequency and severity of HBV reactivation[1,2]. This notion is supported by reports of severe reactivation following more aggressive treatments such as with the use of rituximab, organ transplantation, or concurrent chemo-radiation[3-7].
Reactivation of HBV is common in HBsAg-positive individuals who are undergoing chemotherapy, but it can also occur in patients with resolved hepatitis B in whom serological tests are negative for hepatitis B surface antigen (HBsAg), but positive for antibody to hepatitis B core antigen (anti-HBc) with or without antibody to HBsAg. Such de novo HBV-related hepatitis is reportedly most common in patients undergoing rituximab-containing regimens or hematopoietic stem cell transplantation, in which host immunity is extremely down-regulated and immune-suppression is much prolonged[3,4]. Thus, it should be stressed that HBV reactivation is not limited to chronic HBsAg carriers, but can take place in HBsAg-negative individuals with prior exposure to HBV who are under any intensive treatment.
The risk and severity of HBV reactivation among patients with various cancers appears to be proportionate to the degree of immunosuppression and the intensity of cancer chemotherapy (Figure 1). When the type of malignancy is categorized according to the risk of reactivation, HBsAg-positive chronic carriers with hematologic diseases or organ transplantation are at the highest risk of developing HBV reactivation during therapy. The reported incidence of HBV reactivation in this high risk group ranges from 40% to 50% or more[3,4]. Patients with HCC, lung cancer, and nasopharyngeal cancer undergoing chemotherapy fall within the intermediate risk category, in which HBV reactivation during therapy ranges from 10% to 30%[3,8]. The low-risk group includes patients with gastrointestinal malignancies receiving 5-fluorouracil-based therapy. This group is at low risk (< 10%) of viral reactivation, mainly due to the use of anti-cancer therapy with lower immuno-suppressing property[3,9]. For patients with HCC, the feature of HBV reactivation varies with treatments; the risk of developing reactivation is high on intensive chemo-radiotherapy, but low on local ablation therapy (LAT).
Figure 1.
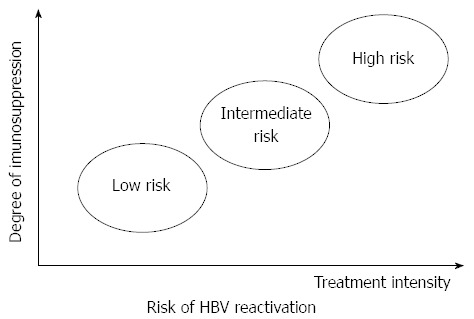
Role of treatment intensity and the degree of immunosuppression in hepatitis B virus reactivation during cancer therapy. The risk of hepatitis B virus (HBV) reactivation is proportionate to treatment intensity and the degree of immunosuppression.
CLINICAL MANIFESTATION AND PATHOGENESIS OF HBV REACTIVATION
The clinical spectrum of reactivated hepatitis B varies from a slight elevation of alanine aminotransferase (ALT) to fatal fulminant hepatitis, sometimes leading to death. The incidence of HBV reactivation in HBsAg-positive patients with HCC ranges from 4% to 67%, with mortality rates reaching up to 18%[3,8,10]. Despite the rare incidence of reactivation in HBsAg-negative patients, the prevalence of severe hepatitis leading to fulminant hepatitis is reportedly higher in HBsAg-negative than HBsAg-positive patients[4]. Different manifestations of reactivation are related to the type of cancer, treatment protocols, baseline viral replicating activity, and underlying liver diseases.
Reactivation typically starts with the increase in viral replication that occurs after initiating immune suppression or chemotherapy. During the immunosuppression, HBV replication is enhanced leading to widespread hepatocyte infection by the virus. When the chemotherapeutic drugs are withdrawn, restoration of host immune function results in the rapid destruction of infected hepatocytes, and hepatocellular injury arises[1,11]. Although immune-mediated lysis of infected cells by cytotoxic T lymphocytes is generally implicated in the mechanism of hepatitis due to reactivation, a direct cytopathic effect of increased HBV replication during immunosuppression cannot be fully excluded[12,13]. Thus, the development of reactivation hepatitis is best understood in the context of a complex interplay between the virus and host immunity.
In a typical case of hepatitis due to HBV reactivation, serum HBV DNA levels increase several weeks prior to increases in ALT levels. Because ALT flares lag behind the increase in HBV DNA levels, serum HBV DNA levels may be declining or undetectable when patients with flares are evaluated for reactivation. Thus, it should be noted that the diagnosis of HBV reactivation may be neglected or underestimated when testing for serum HBV DNA is performed in the recovery phase of reactivation, making estimates of the actual incidence of HBV reactivation in patients on chemotherapy a challenge. Indeed, in a prospective study, “serial HBV DNA monitoring” done intensively at less than monthly intervals improved the accuracy of diagnosing HBV reactivation when compared with “conventional monitoring”, which only measured HBV DNA at the time of clinical hepatitis[14]. This highlights the importance of close monitoring of HBV DNA levels in determining the accurate estimation of HBV reactivation during chemotherapy.
IMPORTANCE OF HBV REACTIVATION IN THE TREATMENT OF HCC
In a study of patients with HBV-related HCC, hepatitis following treatment of HCC was reported in 60% of patients. Most of the hepatic events were attributed to HBV reactivation, which has a 30% mortality rate[15]. Such high morbidity and mortality rates from HBV reactivation call for physicians’ awareness and appropriate management to prevent reactivation in patients undergoing treatment of HCC, especially considering that HCC patients with reactivation are more prone to have severe hepatic damage due to underlying liver cirrhosis.
HBV reactivation in HCC patients is linked directly with poor HCC survival. Given that hepatic functional deterioration is a leading cause of death in patients with HCC, the development of HBV reactivation is anticipated to negatively affect survival of HCC patients. Indeed, a recent study involving 1609 patients who underwent hepatectomy demonstrated that HBV reactivation was independently associated with shorter overall and recurrence-free survival[16]. Furthermore, when reactivation occurs, scheduled treatment for HCC should be delayed until the deteriorated liver function recovers. Two prospective studies showed that reactivation resulted in delay or premature termination of treatment schedules for HCC[15,17]. Patients with reactivation experience significantly more frequent disruptions in treatment schedules than those without[14]. The overall findings suggest that HBV reactivation is an independent factor that adversely affects the final outcome of patients as it causes not only direct hepatic damage, but also disruptions in treatments of HCC, ultimately precluding therapeutic benefit from scheduled treatment.
DIAGNOSIS OF HBV REACTIVATION
When HBV reactivation is suspected in chronic carriers, HBV DNA testing is the mainstay in the diagnosis of HBV reactivation, because many cases of reactivation occur without changes in serologic markers such as HBsAg or HBeAg. The critical issue is to demonstrate whether a patient with viral reactivation actually has “hepatitis”. Histological examination by liver biopsy may be the best diagnostic tool for hepatitis, but sampling liver tissues may be difficult, because patients suffering from HBV reactivation frequently have severe hepatic injury including coagulopathy. Thus, despite the lack of consensus on diagnostic criteria, it is generally accepted that hepatitis due to HBV reactivation is diagnosed when there is an abrupt increase in serum ALT to > 3 times the baseline level in case of HBV reactivation, which is defined as an increase in HBV DNA levels to > 10 times the baseline level. It has been reported that histological proof of reactivation hepatitis using liver biopsy is not needed using these criteria[18]. Nevertheless, because the presentation of ALT levels varies with underlying liver diseases, the optimal cut-off value for the diagnosis of hepatitis due to reactivation remains to be confirmed.
HBsAg-negative patients undergoing rituximab-containing chemotherapy or transplantation are also at risk of developing HBV reactivation. In these patients, occult HBV infection is implied as the origin of reactivation[19]. Reversion of HBsAg or a decrease in the titers of anti-HBs often precedes an increase in the HBV DNA level. Thus, the definition of HBV reactivation for HBsAg-negative patients is made when there is a reappearance of HBsAg or HBV DNA in the serum[18,20].
RISK FACTORS OF HBV REACTIVATOIN IN HCC
Several risk factors identified for HBV reactivation in patients undergoing cancer chemotherapy have been broadly categorized into host, viral, and treatment factors (Figure 2). These risk factors are not different for patients with HCC and with other malignancies.
Figure 2.
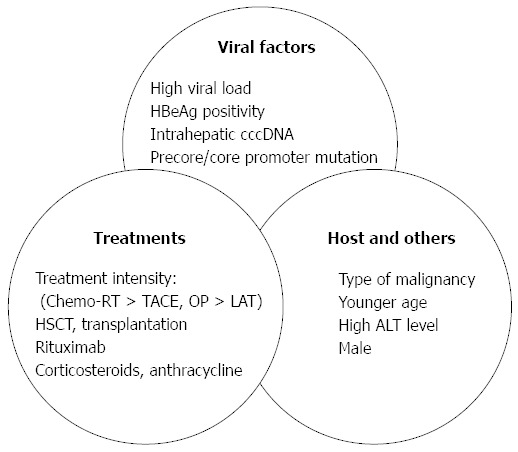
Risk factors of hepatitis B virus reactivation in chronic hepatitis B virus carriers with or without hepatocellular carcinoma. Modified from Jang et al[8]. ALT: Alanine aminotransferase; RT: Radiotherapy; TACE: Transarterial chemoembolization; OP: Operation; LAT: Local ablation therapy; HSCT: Hematopoietic stem cell transplantation.
Given that highly replicating HBV is a key factor for the development of HCC[21], it is speculated that HBV itself in patients with HCC is more prone to reactivate under the circumstances of immunosuppression. Although other viral factors including HBeAg seropositivity and molecular variants in the HBV genome, such as basal core promoter or precore mutations, are sporadically reported to predispose reactivation, a high viral load has been most strongly associated with reactivation in multiple publications[17,18,22].
The type of treatment can contribute to the differential risk of HBV reactivation. The reported incidences of HBV reactivation in patients undergoing systemic chemotherapy, transarterial therapy, LAT, and surgical resection were approximately 40%, 15%-35%, 5%-10%, and 15%-30%, respectively (Table 1, Table 2 and Table 3). Radiation therapy leads to viral reactivation by actively suppressing the immune system, as evidenced by the decrease in the number of immune cells as well as by a bystander mechanism involving interleukin (IL)-6 released during radiotherapy[6,7,23]. A previous study comparing HBV reactivation between various loco-regional therapies indicated that there is a high risk of HBV reactivation with concurrent chemo-radiation therapy, an intermediate risk with conventional transarterial chemoembolization (TACE), and a relatively low risk with LAT[7].
Table 1.
Results of hepatitis B virus reactivation in patients with hepatocellular carcinoma receiving chemotherapy n (%)
| Ref. | No of patients | Chemotherapy | No of sessions | HBV reactivation (hepatitis)1 | Morbidity/mortality |
| Nagamatsu et al[29] | 33 | TAI | Weekly infusion | 24% | 3 died |
| Jang et al[27] | 146 | TACL | 5 (2-14) | 33.7% (21.7%) | 25 resolved, 3 died |
| Nagamatsu et al[10] | 17 | TAI | bi-weekly infusion | 67% | 3 died of HBV reactivation |
| Yeo et al[15] | 102 | Systemic chemotherapy | 3-weekly intervals | (36%) | Twelve died of HBV reactivation |
| Park et al[31] | 89 | TACE | 1 | 4.3% | 3 resolved, 1 had tumor-related hepatic failure |
| Jang et al[17] | 73 | TACL | 1-monthly intervals | 40.5% (29.7%) | One died of HBV reactivation |
| Kim et al[6] | 91 | TACE + RT | NA | 21.8% (a rebound of HBV DNA to > 100 × baseline) | 4 (12.5) developed CHB exacerbation |
| Lao et al[32] | 172 | TACE | 1.3/person | 14.5% | 12.1% in the reactivation group had CHB exacerbation |
| Jang et al[7] | 205 | LAT, TACL, TACL + RT | 1-2 monthly intervals | 30.2% | 10 developed decompensation, 1 died |
| Lao et al[30] | 320 | TACE | 4-10 weekly intervals | 17.5% | 26 (8.1) had liver functional deterioration |
The rates of hepatitis B virus (HBV) reactivation were the frequencies in antiviral-untreated patients. Modified from Jang et al[8]. HCC: Hepatocellular carcinoma; TAI: Transarterial infusion chemotherapy; TACL: Transarterial chemo-lipiodolization; TACE: Transarterial chemo-embolization; RT: Radiotherapy; LAT: Local ablation therapy.
Table 2.
Results of hepatitis B virus reactivation in patients with hepatocellular carcinoma receiving hepatectomy n (%)
| Ref. | No of patients | HBV reactivation1 | Morbidity/mortality |
| Kubo et al[36] | 25 | 28.0% | 24% had postoperative hepatitis |
| Huang et al[35] | 164 | 21.1% | No patient developed liver failure postoperation |
| Huang et al[37] | 84 | 31.8% | 8.3% had postoperative liver insufficiency |
| Dan et al[38] | 93 | 14.0% | 25% developed hepatitis, None of them developed hepatic failure |
| Lao et al[30] | 121 | 15.7% | 26 (8.1) had liver functional deterioration |
The rates of hepatitis B virus (HBV) reactivation were the frequencies in antiviral-untreated patients.
Table 3.
Results of hepatitis B virus reactivation in patients with hepatocellular carcinoma receiving local ablation therapy
| Ref. | No of patients | Therapy | HBV reactivation (hepatitis)1 | Morbidity/mortality |
| Jang et al[7] | 43 | 7 with PEIT and 36 with RFA | 0% vs 9.1% in patients with low and high viremia, respectively | None of the patients developed hepatic decompensation |
| Yoshida et al[39] | 104 | RFA | (5.6%) | Not specified |
| Dan et al[38] | 125 | RFA | 5.6% | None of the patients developed hepatic failure |
The rates of hepatitis B virus (HBV) reactivation were the frequencies in antiviral-untreated patients. RFA: Radiofrequency ablation.
Taken together, the key element that determines the risk of HBV reactivation during cancer therapy is the degree of immunosuppression induced by individual treatment options. As all chemotherapeutic agents have at least some immune suppressive effect, the varying risk of HBV reactivation with different treatments reflects the distinct levels of immunosuppression on host immunity contributed by each treatment.
HBV REACTIVATION IN PATIENTS WITH HBV-RELATED HCC
HBV reactivation following chemotherapy or radiotherapy
In East Asian countries such as Korea, in which HBV infection is endemic, more than two thirds of patients diagnosed with HCC have evidence of chronic HBV infection. Because HBV-related liver morbidity can be intensified with the underlying cirrhosis of these patients, HBV reactivation remains a critical issue in the management of HBV-related HCC. Nevertheless, it is paradoxical that HBV reactivation in patients with HCC has been recognized only recently, approximately 30 years after the first description in 1975 of cases of reactivation in patients with hematologic malignancies[24]. Reactivation of HBV in patients with HCC was first reported in 2003 in case reports; in these instances flares of hepatitis associated with HBV reactivation developed after transarterial chemo-infusion and resolved after lamivudine administration[25,26].
Unlike systemic chemotherapy, TACE may not directly contribute to HBV reactivation because it has little systemic effect on host immunity. However, TACE does have a systemic effect through arterio-venous shunt or peritumoral microcirculation, by which host immune regulation is often compromised. This notion is supported by a body of evidence showing that TACE itself is directly associated with an increased rate of HBV reactivation[3,10,27]. The chemotherapeutic agent chosen for treatment of HCC may also stimulate HBV reactivation. As a putative mechanism of reactivation, anthracyclines have been experimentally shown to stimulate HBV DNA secretion from HCC cell lines in a dose-dependent manner[28]. That anthracyclines such as doxorubicin are commonly used as part of intra-arterial chemotherapy for HCC may explain the increased risk of HBV reactivation in patients undergoing doxorubicin-containing TACE. Table 1 summarizes the results from studies on HBV reactivation during intra-arterial or systemic chemotherapy for HCC, which will be mentioned below.
In one of the earliest reports, Nagamatsu et al[29] showed that 24% of patients receiving weekly infusions of intra-arterial chemotherapy had HBV reactivation, and the presence of hepatitis B e antigen (HBeAg) was associated with hepatic damage during the therapy. The same group of investigators subsequently recruited 17 HBeAg-positive patients and investigated the efficacy of prophylactic lamivudine. In that study, three patients expired, and exacerbation of liver damage was detected in six of the nine patients who did not receive lamivudine therapy, providing a presumed rate of HBV reactivation of 67%. None of the 8 patients receiving lamivudine had liver damage. Although the number of patients was small and only HBeAg-positive patients were included in analysis, this study was the first to suggest any beneficial effect from antivirals in patients with HBV-related HCC[10].
A study by Jang et al[27] involving 146 Korean patients also showed a higher incidence of hepatitis due to HBV reactivation with TACE than with other local therapies [21.7% (18/83) vs 1.6% (1/63), respectively]; the authors found varying incidences of HBV reactivation according to individual treatments for HCC. In a study by Yeo et al[15], which prospectively followed 102 patients receiving systemic chemotherapy, 59 (58%) patients developed hepatitis; 37 (36%) of these cases were attributable to HBV reactivation, with 12 deceased cases. More recently, a large Chinese study by Lao et al[30] revealed that 17.5% of patients treated with TACE developed HBV reactivation, with a liver deterioration rate of 8.1%. In contrast, they demonstrated that only 1.5% of antiviral-treated patients developed HBV reactivation following TACE.
Reactivation of HBV during radiotherapy with or without TACE has also been examined in several studies. Kim et al[6] conducted a retrospective analysis of 48 Korean patients who underwent radiotherapy and compared them to a control group of 43 chronic carriers with HCC or CHB who did not undergo any specific therapy. Among the antiviral-untreated patients, viral reactivation occurred in 21.8% (7/32) after radiotherapy, which is significantly higher than that of those receiving lamivudine (0%, 0/16) or of controls (2.3%, 1/43). However, this study adopted far stricter criteria for HBV reactivation, defined as > 100-fold increase in HBV DNA levels. Thus, the incidence of HBV reactivation would be higher when using the generally proposed criteria for reactivation, defined as > 10-fold increase in HBV DNA levels.
Another Korean study looked at HBV reactivation in 205 prospectively recruited HBsAg-positive patients receiving various loco-regional therapies[7]. In the study, the hazard ratios for HBV reactivation were shown to be 1.0 for LAT, 2.45 for TACE using a single agent, 4.19 for TACE using combined agents, and 10.17 for combined TACE with radiotherapy. This study further confirmed that the level of immunosuppression affected by cancer therapy is the main factor for HBV reactivation in patients with HCC.
Some other studies have provided conflicting results as to the risk of HBV reactivation after chemotherapy among patients with HCC. In a Korean study that prospectively followed 89 patients (69 with TACE vs 20 controls), Park et al[31] showed that the risk of HBV reactivation was low after one session of TACE, with a 4.3% (3/89) rate of reactivation. Another study by Lao et al[32] involving 172 patients indicated varying patterns in serum HBV DNA levels before and after TACE. In their analysis of 228 total sessions of TACE, HBV reactivated in 33 (14.5%), remained stable in 152 (66.7%), and decreased in 43 (18.8%) sessions. Finally, a study by Ahmad et al[33] from the United States showed no cases of reactivation after TACE. However, that particular study lacked the detailed definition and data of HBV reactivation and included both HBV and HCV-infected patients. The results from this study therefore will not be discussed. Although the above results showed relatively low rates of HBV reactivation, it should be noted that these studies provided short-term data. With regard to the time to reactivation, hepatitis due to reactivation has been reported to occur after a median of 3.5 cycles following initiation of TACE[17], suggesting that HBV reactivation generally occurs not after the first cycle, but after repeated cycles of chemotherapy enough for leading to host immune suppression. In addition, the treatments in these studies were performed at longer TACE intervals, with lower doses of drugs, and so the interpretation is complicated.
HBV reactivation following surgical resection
Surgical resection of HCC elicits profound changes in the metabolic and immune systems; these changes collectively constitute the “stress response”. Acute release of stress hormones and cytokines including cortisol, C-reactive protein, and IL-6 in response to surgical stress predispose patients to develop HBV reactivation during transient immunosuppression[34]. Additionally, partial hepatectomy potentiates reactivation of viral replication due to immunosuppression by blood transfusion and ischemic injury[35]. Thus, deficient immune responses and a skewed balance between pro-inflammatory and anti-inflammatory cytokines may cause increased replication of HBV in patients who undergo HCC resection. The following studies show the data on HBV reactivation after hepatectomy (Table 2).
Kubo et al[36] reported HBV reactivation in 7 (28.0%) of 25 surgical patients; since then, emerging data have consistently shown that reactivation of HBV after resection is common, calling for appropriate management of HBsAg carriers undergoing resection. Huang et al[35] also examined reactivation among all 164 study cohorts who underwent hepatectomy. With ten patients (6.1%) developing HBV reactivation within 1 mo after hepatectomy, reactivation occurred in 21.1% (8/38) of antiviral-untreated patients, which was significantly higher than that of antiviral-treated patients (1.6%, 2/126). The same investigators subsequently conducted a prospective study to evaluate the efficacy of preemptive antiviral therapy in patients undergoing resection[37]. In that study, HBV reactivation developed in 14 (31.8%) of the 44 control patients without antiviral therapy.
A retrospective study by Dan et al[38] involving 93 surgical patients with or without antiviral therapy showed an overall reactivation rate of 14.0% (13/93) post-resection. With subgroup analysis, the incidence of viral reactivation appeared to be higher in the antiviral untreated group vs the treated group (20.7% vs 2.9%). Another study by Lao et al[30] from China showed that of the 121 patients without antiviral therapy, 19 (15.7%) developed HBV reactivation following resection of HCC.
The final and the largest study by Huang et al[16] examined HBV reactivation in 1609 patients undergoing hepatectomy. HBV reactivation happened in 308 (19.1%) patients within 1 year after partial hepatectomy for HCC. Reactivation of HBV was common even in patients with preoperative low HBV-DNA levels (< 200 IU/mL), with a 16.7% (218/1303) incidence rate of reactivation, although it was lower as compared to 29.4% (90/306) in those with high HBV DNA levels (> 200 IU/mL). One of the most important findings emerging from this study was that HBV reactivation is significantly associated with post-hepatectomy liver failure, disease-free survival, and overall survival (all were statistically significant). The authors concluded that antiviral treatment should be routinely given before hepatectomy.
HBV reactivation following local ablation therapy
There is only limited information on HBV reactivation in patients treated with LAT (Table 3). The incidence of HBV reactivation following LAT was partly documented in an earlier Korean study, in which none of the 9 patients with percutaneous ethanol injection therapy (PEIT) experienced reactivation[27]. The same investigators subsequently examined 43 patients [7 with PEIT and 36 with radiofrequency ablation (RFA)] among whom HBV reactivation was a rare incident (3.9% at 6 mo). However, its incidence varied depending on viral replication status; reactivation rates were 0% and 9.1% in patients with low and high viremia, respectively, indicating a higher risk of reactivation in the high viremia group[7].
Another study from Japan involving 71 patients undergoing RFA showed that 4 (5.6%) patients developed reactivated hepatitis, which was defined as redetection of HBV DNA and an ALT elevation higher than twice the upper limit of normal[39]. Additionally, a study by Dan et al[38] following Chinese patients who underwent RFA or hepatectomy for small HCC revealed that 7 (5.6%) of the 125 patients treated with RFA developed HBV reactivation, indicating a lower rate of reactivation with RFA compared to hepatectomy (5.6% vs 14.0%).
Collectively, analyses show that the incidence of HBV reactivation after LAT is relatively low when compared with other treatment options such as systemic or intra-arterial chemotherapy or hepatectomy. Reactivation following PEIT appeared to be less frequent than that following RFA. Although the reason for the lower risk of reactivation after RFA is not fully understood, it has been suggested that RFA can cause immune activation[40] and thus may have a potential effect on immune control of HBV infection[38]. This hypothesis, however, should be confirmed in future studies.
HBV reactivation following targeted therapy and immunotherapy
Apart from aforementioned therapies, sorafenib can be opted for the treatment of HCC. This multikinase inhibitor has been the first approved systemic agent for HCC and is indicated as an option for advanced HCC[41]. It has been suggested that sorafenib can augment the host immunity through the action of immune modulation of effector T cells and regulatory T cells as well as induction of type 1 helper T cell dominance[42,43]. Immunotherapy has recently been tested as an alternative option for advanced HCC. In one case report, IL-2 therapy in a patient with HCC resulted in a decrease in HBV DNA levels that subsequently continued to remain undetectable until 3 mo following the last IL-2 cycle[44]. IL-2 has been shown to stimulate immune cells and increase the levels of proinflammatory cytokines[44,45]. Based on their role in immune activation, it is assumed that sorafenib or immunotherapy appear to be associated with a low risk of HBV reactivation. However, there are no detailed data focusing on viral reactivation during these therapies. Thus, until such time as convincing information becomes available, the effect of these new options on HBV reactivation remains unknown and awaits evaluation in future studies.
MANAGEMENT OF HBV REACTIVATION IN PATIENTS WITH HCC
All patients with HCC who are to receive anti-cancer therapy should be screened for HBV markers and monitored against a flare of HBV-related hepatitis. Early recognition and prompt administration of antiviral therapy is of paramount importance to reduce HBV reactivation-associated liver diseases. One potential means for minimizing the events is a deferred approach, which means a close monitoring for HBV markers and the use of antiviral drugs only when there is evidence of HBV reactivation. The deferred approach seems to be reasonable without unnecessary treatment. However, clinical data do not favor this approach because the effects of antiviral therapy take time and may not prevent liver injury when a flare has already developed. Recently, multiple reports have suggested a beneficial effect to patients from an early preemptive approach using antiviral drugs (Table 4). The most experience has been with lamivudine.
Table 4.
Clinical trials of preemptive antiviral therapy for hepatitis B virus reactivation in patients with hepatitis B virus-related hepatocellular carcinoma
| Ref. | Study type | Cancer therapy | No of patients (Tx vs control) | Antiviral therapy | HBV reactivation (Tx vs control) | P value |
| Nagamatsu et al[10] | Retrospective | TAI | 17 (8 vs 9) | LAM | 0% vs 67% | 0.009 |
| Jang et al[17] | RCT | TACL | 73 (36 vs 37) | LAM | 2.8% vs 29.7% | 0.002 |
| Kim et al[6] | Retrospective | TACE + RT | 48 (16 vs 32) | LAM | 0% vs 21.8% | 0.048 |
| Huang et al[35] | Prospective | Hepatectomy | 164 (126 vs 38) | LAM, ETV, ADV, TBVD | 1.6% vs 21.1% | < 0.001 |
| Dan et al[38] | Retrospective | Hepatectomy, RFA | 218 (68 vs 150) | LAM, ETV, LAM + ADV | 2.9% vs 20.7%1 | 0.027 |
| 0% vs 7.6%2 | NS | |||||
| Huang et al[37] | RCT | Hepatectomy | 84 (40 vs 44) | TBVD | 2.5% vs 31.8% | 0.001 |
| Huang et al[16] | Retrospective | Hepatectomy | 1609 (150 vs 1459) | LAM, ETV, ADV | 4.7% vs 20.1% | < 0.001 |
Data following hepatectomy;
Data following RFA. HBV: Hepatitis B virus; HCC: Hepatocellular carcinoma; Tx: Treatment; RCT: Randomized controlled trial; TAI: Transarterial infusion chemotherapy; TACL: Transarterial chemo-lipiodolization; TACE: Transarterial chemo-embolization; RT: Radiotherapy; LAM: Lamivudine; ETV: Entecavir; ADV: Adefovir; TBVD: Telbivudine; NS: Not significant.
The first study of 17 HBeAg-positive Japanese patients assessing the prophylactic role of lamivudine revealed that while none [0% (0/8)] with lamivudine had reactivation, as much as 67% (6/9) without lamivudine had exacerbation of liver damage, and 3 of them died of progressive liver failure due to HBV reactivation[10]. In another study of 48 patients undergoing combined TACE with radiotherapy, HBV reactivation was observed in none (0%) of the 16 lamivudine-treated patients vs 7 (21.8%) of the 32 untreated patients[6]. The prophylactic effect of lamivudine in this study did not reach statistical significance, due to the small number of patients analyzed.
Recently, a series of studies indicating preemptive therapy to be of benefit in decreasing the risk of reactivation have emerged from patients who underwent hepatectomy. A study by Huang et al[35] involving 164 patients with resection of HCC showed that HBV reactivation was significantly lessened with antiviral therapy, with an incidence rate of 1.6% (2/126) vs 21.1% (8/38) in the antiviral and non-antiviral groups, respectively. Another Chinese study also provided similar results, in which antiviral therapy cut the risk by 86% compared to observation, with reactivation rates of 2.9% vs 20.7%, respectively[38]. Additionally, the investigators evaluated the preventive role of antiviral therapy against reactivation following RFA. Although the antivirals obviously protected against reactivation, their results did not reach statistical significance probably due to the overall low risk of HBV reactivation in the RFA group (0% in the antiviral vs 7.6% in the non-antiviral groups). Of note in this study is that the lack of antiviral therapy was an independent predictor of HBV reactivation. Recently, a large cohort study of 1609 Chinese patients demonstrated a clear benefit from preemptive antivirals post-resection[16]. In this study, HBV reactivation was a negative factor for all post-operative liver function, disease-free survival, and overall survival, while prophylactic use of antivirals significantly reduced post-operative viral reactivation, thereby carrying a protective effect for post-operative outcomes. Viral reactivation was common even in patients with low viremia. Thus, the authors emphasized that routine prophylactic antiviral treatment should be given for all patients before hepatectomy.
Two randomized controlled trials of preemptive antiviral therapy have been performed in patients with HCC. The first trial by Jang et al[17] included 73 patients undergoing TACE who were randomly assigned to lamivudine or observation groups. A flare of hepatitis due to HBV reactivation was observed significantly more often in the observation group [29.7% (11/37) vs 2.8% (1/36)]. The frequency and severity of overall hepatitis were also significantly greater in the observation group. A serum level of HBV DNA more than 10000 copies/mL was independently predictive of a flare.
In the second trial, Huang et al[37] recruited 84 patients with low viral load undergoing hepatectomy, who were randomly assigned to telbivudine or observation. They determined that telbivudine significantly lessened the occurrence of viral reactivation following hepatectomy compared to the observation group [2.5% (1/40) vs 31.8% (14/44)]. Recovery of liver function or postoperative liver insufficiency was not different between the two groups. However, this study included only patients with low viremia, who have a low probability of developing post-operative liver insufficiency. Thus, the lack of significance likely does not contradict the beneficial effect of preemptive therapy.
Overall, the studies looking at antiviral prophylaxis demonstrate clear evidence that preemptive antiviral therapy prevents HBV reactivation in patients with HBV-related HCC undergoing anti-cancer therapy. The preemptive strategy provides potential additional advantages to reducing overall hepatitis from all causes, discontinuations or disruptions of the anti-cancer treatment, and HBV-related mortality. A potential concern with the preemptive use of lamivudine is the occurrence of drug resistance. However, resistance will likely become uncommon because of the current availability of potent antiviral agents such as entecavir and tenofovir with very low risk of drug resistance. An unresolved issue for prophylactic treatment is when to stop antiviral therapy. Although no study to date has addressed this issue in patients with HCC, given the underlying cirrhosis and shorter survival of HCC patients it seems reasonable to keep patients on antivirals without interruption for a long-term period, probably until HBsAg seroclearance.
POSSIBILITY OF HBV REACTIVATION IN HBSAG-NEGATIVE PATIENTS WITH HCC
Although documented mostly in HBsAg-positive patients, HBV reactivation can also occur in patients with prior resolved hepatitis B, who are identified by the presence of anti-HBc and/or anti-HBs. Occult HBV infection or low-level viremia that persists in the liver and blood for decades after a recovery from acute infection have been implicated as the origin of HBV reactivation[19]. Such de novo hepatitis B or HBsAg sero-reversion is most common in the setting of rituximab-containing chemotherapy or hematopoietic stem cell transplantation, with incidence rates ranging from 2.7% to 45%[3-5]. Given that patients with HCC have a high prevalence of anti-HBc positivity or occult HBV infection, it is speculated that HBV presents in the liver or blood of HBsAg-negative HCC patients and is prone to reactivation when the host immune system is severely compromised by intensive therapy.
Recently, Peng et al[46] investigated HBV reactivation in 43 HBsAg-negative patients undergoing TACE. Four patients (9.3%) developed hepatitis associated with HBV reactivation, but all had resolution of hepatitis after initiation of lamivudine. In our own unpublished data, a similar incidence rate of reactivation was observed following TACE. Although no mortality related to reactivation was found in either study, the results consistently indicate that HBsAg-negative patients, especially those with resolved HBV, are still at risk of developing viral reactivation. As such reactivation potentially results in higher morbidity and mortality[47,48], appropriate management for this particular group needs to be determined in the future.
SPECIAL ISSUES ON HBV REACTIVATION IN PATIENTS WITH HCC
International guidelines recommend prophylactic antiviral therapy for HBV carriers undergoing immunosuppressive or cancer chemotherapy[49-52]. However, emphasis must be placed on the HCC patient where the issue is distinct and much more complex. The degree of ALT elevation following HBV reactivation is more affected by hepatic reserve, so that the absolute ALT level in patients with HCC is often normal or only minimally elevated even if there is severe liver damage. Hepatic decompensation can be more common due to underlying cirrhosis in HCC patients compared with those without cirrhosis. The severity of hepatitis flares is multifactorial, affected by treatment itself, tumor progression, and/or multiple other factors in these patients. Because of the relatively short survival of HCC patients, it is difficult to determine the long-term effect of reactivation. With no generalized practice guidelines, a variety of treatment options with different protocols among institutions are in use for HCC patients at the same stage. All of these remain critical challenges for the estimation of actual risk of reactivation and establishment of consensus on the prophylactic management in patients with HCC.
CONCLUSION
Reactivation of HBV is a common and a life-threatening complication in patients with HBV-related HCC. Patients who are to receive anti-cancer therapy for HCC should be routinely screened for HBsAg and anti-HBc before cytotoxic therapy is performed. Screening for serum HBV DNA should be performed for all HBsAg carriers and is also helpful in the identification of occult HBV infection in HBsAg-negative/anti-HBc positive patients. Since a substantial proportion of HCC patients with reactivation experience morbidity and mortality, which often lead to discontinuation of potentially life-prolonging treatments, preemptive antiviral therapy should be given to all HBsAg carriers with HCC who are to undergo anti-cancer therapy. Reactivation can also occur in HBsAg-negative patients with a history of past HBV on intensive treatment of HCC. Close monitoring and prompt antiviral therapy upon evidence of HBV reactivation should be administered for these patients until an early prophylactic approach can be clearly defined.
The optimal duration of anti-HBV therapy has not been determined. International guidelines recommend that antivirals be maintained for several months after completion of treatment[49,50]. However, these recommendations may not be applicable to HCC patients with underlying cirrhosis. Long-term use of highly potent antivirals with less resistance (i.e., entecavir or tenofovir) seems logical in patients with HCC, although the efficacy of these drugs has yet to be confirmed. The adequate control of viral replication is of great importance in the management of HCC patients, not only to prevent HBV reactivation, but also to offer additive benefits within the microenvironments of tumors and liver tissues, likely ameliorating the inflammation and cancer-promoting properties of the virus.
Footnotes
P- Reviewers: Saburi A, Sugawara Y S- Editor: Zhai HH L- Editor: A E- Editor: Wang CH
References
- 1.Hoofnagle JH. Reactivation of hepatitis B. Hepatology. 2009;49:S156–S165. doi: 10.1002/hep.22945. [DOI] [PubMed] [Google Scholar]
- 2.Perrillo RP. Acute flares in chronic hepatitis B: the natural and unnatural history of an immunologically mediated liver disease. Gastroenterology. 2001;120:1009–1022. doi: 10.1053/gast.2001.22461. [DOI] [PubMed] [Google Scholar]
- 3.Yeo W, Johnson PJ. Diagnosis, prevention and management of hepatitis B virus reactivation during anticancer therapy. Hepatology. 2006;43:209–220. doi: 10.1002/hep.21051. [DOI] [PubMed] [Google Scholar]
- 4.Kusumoto S, Tanaka Y, Mizokami M, Ueda R. Reactivation of hepatitis B virus following systemic chemotherapy for malignant lymphoma. Int J Hematol. 2009;90:13–23. doi: 10.1007/s12185-009-0359-5. [DOI] [PubMed] [Google Scholar]
- 5.Evens AM, Jovanovic BD, Su YC, Raisch DW, Ganger D, Belknap SM, Dai MS, Chiu BC, Fintel B, Cheng Y, et al. Rituximab-associated hepatitis B virus (HBV) reactivation in lymphoproliferative diseases: meta-analysis and examination of FDA safety reports. Ann Oncol. 2011;22:1170–1180. doi: 10.1093/annonc/mdq583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim JH, Park JW, Kim TH, Koh DW, Lee WJ, Kim CM. Hepatitis B virus reactivation after three-dimensional conformal radiotherapy in patients with hepatitis B virus-related hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2007;69:813–819. doi: 10.1016/j.ijrobp.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Jang JW, Kwon JH, You CR, Kim JD, Woo HY, Bae SH, Choi JY, Yoon SK, Chung KW. Risk of HBV reactivation according to viral status and treatment intensity in patients with hepatocellular carcinoma. Antivir Ther. 2011;16:969–977. doi: 10.3851/IMP1840. [DOI] [PubMed] [Google Scholar]
- 8.Jang JW. Management of patients with hepatitis B virus infection who receive immunosuppressive treatment or chemotherapy. Korean J Med. 2012;82:149–158. [Google Scholar]
- 9.Yeo W, Chan PK, Zhong S, Ho WM, Steinberg JL, Tam JS, Hui P, Leung NW, Zee B, Johnson PJ. Frequency of hepatitis B virus reactivation in cancer patients undergoing cytotoxic chemotherapy: a prospective study of 626 patients with identification of risk factors. J Med Virol. 2000;62:299–307. doi: 10.1002/1096-9071(200011)62:3<299::aid-jmv1>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 10.Nagamatsu H, Itano S, Nagaoka S, Akiyoshi J, Matsugaki S, Kurogi J, Tajiri N, Yamasaki S, Koga H, Torimura T, et al. Prophylactic lamivudine administration prevents exacerbation of liver damage in HBe antigen positive patients with hepatocellular carcinoma undergoing transhepatic arterial infusion chemotherapy. Am J Gastroenterol. 2004;99:2369–2375. doi: 10.1111/j.1572-0241.2004.40069.x. [DOI] [PubMed] [Google Scholar]
- 11.Thung SN, Gerber MA, Klion F, Gilbert H. Massive hepatic necrosis after chemotherapy withdrawal in a hepatitis B virus carrier. Arch Intern Med. 1985;145:1313–1314. [PubMed] [Google Scholar]
- 12.Mindikoglu AL, Regev A, Schiff ER. Hepatitis B virus reactivation after cytotoxic chemotherapy: the disease and its prevention. Clin Gastroenterol Hepatol. 2006;4:1076–1081. doi: 10.1016/j.cgh.2006.05.027. [DOI] [PubMed] [Google Scholar]
- 13.Rossi G. Prophylaxis with lamivudine of hepatitis B virus reactivation in chronic HbsAg carriers with hemato-oncological neoplasias treated with chemotherapy. Leuk Lymphoma. 2003;44:759–766. doi: 10.1080/104281903100006351. [DOI] [PubMed] [Google Scholar]
- 14.Yeo W, Chan PK, Hui P, Ho WM, Lam KC, Kwan WH, Zhong S, Johnson PJ. Hepatitis B virus reactivation in breast cancer patients receiving cytotoxic chemotherapy: a prospective study. J Med Virol. 2003;70:553–561. doi: 10.1002/jmv.10430. [DOI] [PubMed] [Google Scholar]
- 15.Yeo W, Lam KC, Zee B, Chan PS, Mo FK, Ho WM, Wong WL, Leung TW, Chan AT, Ma B, et al. Hepatitis B reactivation in patients with hepatocellular carcinoma undergoing systemic chemotherapy. Ann Oncol. 2004;15:1661–1666. doi: 10.1093/annonc/mdh430. [DOI] [PubMed] [Google Scholar]
- 16.Huang G, Lai EC, Lau WY, Zhou WP, Shen F, Pan ZY, Fu SY, Wu MC. Posthepatectomy HBV reactivation in hepatitis B-related hepatocellular carcinoma influences postoperative survival in patients with preoperative low HBV-DNA levels. Ann Surg. 2013;257:490–505. doi: 10.1097/SLA.0b013e318262b218. [DOI] [PubMed] [Google Scholar]
- 17.Jang JW, Choi JY, Bae SH, Yoon SK, Chang UI, Kim CW, Cho SH, Han JY, Lee YS. A randomized controlled study of preemptive lamivudine in patients receiving transarterial chemo-lipiodolization. Hepatology. 2006;43:233–240. doi: 10.1002/hep.21024. [DOI] [PubMed] [Google Scholar]
- 18.Lau GK. Hepatitis B reactivation after chemotherapy: two decades of clinical research. Hepatol Int. 2008;2:152–162. doi: 10.1007/s12072-008-9056-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hui CK, Cheung WW, Zhang HY, Au WY, Yueng YH, Leung AY, Leung N, Luk JM, Lie AK, Kwong YL, et al. Kinetics and risk of de novo hepatitis B infection in HBsAg-negative patients undergoing cytotoxic chemotherapy. Gastroenterology. 2006;131:59–68. doi: 10.1053/j.gastro.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 20.Kusumoto S, Tanaka Y, Ueda R, Mizokami M. Reactivation of hepatitis B virus following rituximab-plus-steroid combination chemotherapy. J Gastroenterol. 2011;46:9–16. doi: 10.1007/s00535-010-0331-4. [DOI] [PubMed] [Google Scholar]
- 21.Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73. doi: 10.1001/jama.295.1.65. [DOI] [PubMed] [Google Scholar]
- 22.Lau GK, Leung YH, Fong DY, Au WY, Kwong YL, Lie A, Hou JL, Wen YM, Nanj A, Liang R. High hepatitis B virus (HBV) DNA viral load as the most important risk factor for HBV reactivation in patients positive for HBV surface antigen undergoing autologous hematopoietic cell transplantation. Blood. 2002;99:2324–2330. doi: 10.1182/blood.v99.7.2324. [DOI] [PubMed] [Google Scholar]
- 23.Chou CH, Chen PJ, Lee PH, Cheng AL, Hsu HC, Cheng JC. Radiation-induced hepatitis B virus reactivation in liver mediated by the bystander effect from irradiated endothelial cells. Clin Cancer Res. 2007;13:851–857. doi: 10.1158/1078-0432.CCR-06-2459. [DOI] [PubMed] [Google Scholar]
- 24.Wands JR, Chura CM, Roll FJ, Maddrey WC. Serial studies of hepatitis-associated antigen and antibody in patients receiving antitumor chemotherapy for myeloproliferative and lymphoproliferative disorders. Gastroenterology. 1975;68:105–112. [PubMed] [Google Scholar]
- 25.Tamori A, Nishiguchi S, Tanaka M, Kurooka H, Fujimoto S, Nakamura K, Shiomi S. Lamivudine therapy for hepatitis B virus reactivation in a patient receiving intra-arterial chemotherapy for advanced hepatocellular carcinoma. Hepatol Res. 2003;26:77–80. doi: 10.1016/s1386-6346(03)00002-0. [DOI] [PubMed] [Google Scholar]
- 26.Vizzini GB, Luca A, Marino IR. Hepatitis B virus reactivation after a single session of transarterial chemoembolization in patients with hepatocellular carcinoma. Ann Intern Med. 2003;138:691–692. doi: 10.7326/0003-4819-138-8-200304150-00036. [DOI] [PubMed] [Google Scholar]
- 27.Jang JW, Choi JY, Bae SH, Kim CW, Yoon SK, Cho SH, Yang JM, Ahn BM, Lee CD, Lee YS, et al. Transarterial chemo-lipiodolization can reactivate hepatitis B virus replication in patients with hepatocellular carcinoma. J Hepatol. 2004;41:427–435. doi: 10.1016/j.jhep.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 28.Hsu CH, Hsu HC, Chen HL, Gao M, Yeh PY, Chen PJ, Cheng AL. Doxorubicin activates hepatitis B virus (HBV) replication in HBV-harboring hepatoblastoma cells. A possible novel mechanism of HBV reactivation in HBV carriers receiving systemic chemotherapy. Anticancer Res. 2004;24:3035–3040. [PubMed] [Google Scholar]
- 29.Nagamatsu H, Kumashiro R, Itano S, Matsugaki S, Sata M. Investigation of associating factors in exacerbation of liver damage after chemotherapy in patients with HBV-related HCC. Hepatol Res. 2003;26:293–301. doi: 10.1016/s1386-6346(03)00158-x. [DOI] [PubMed] [Google Scholar]
- 30.Lao XM, Luo G, Ye LT, Luo C, Shi M, Wang D, Guo R, Chen M, Li S, Lin X, et al. Effects of antiviral therapy on hepatitis B virus reactivation and liver function after resection or chemoembolization for hepatocellular carcinoma. Liver Int. 2013;33:595–604. doi: 10.1111/liv.12112. [DOI] [PubMed] [Google Scholar]
- 31.Park JW, Park KW, Cho SH, Park HS, Lee WJ, Lee DH, Kim CM. Risk of hepatitis B exacerbation is low after transcatheter arterial chemoembolization therapy for patients with HBV-related hepatocellular carcinoma: report of a prospective study. Am J Gastroenterol. 2005;100:2194–2200. doi: 10.1111/j.1572-0241.2005.00232.x. [DOI] [PubMed] [Google Scholar]
- 32.Lao XM, Wang D, Shi M, Liu G, Li S, Guo R, Yuan Y, Chen M, Li J, Zhang Y, et al. Changes in hepatitis B virus DNA levels and liver function after transcatheter arterial chemoembolization of hepatocellular carcinoma. Hepatol Res. 2011;41:553–563. doi: 10.1111/j.1872-034X.2011.00796.x. [DOI] [PubMed] [Google Scholar]
- 33.Ahmad J, Rhee J, Carr BI. The effects of hepatic artery chemotherapy on viral hepatitis in patients with hepatocellular carcinoma. Dig Dis Sci. 2005;50:331–335. doi: 10.1007/s10620-005-1606-0. [DOI] [PubMed] [Google Scholar]
- 34.Burpee SE, Kurian M, Murakame Y, Benevides S, Gagner M. The metabolic and immune response to laparoscopic versus open liver resection. Surg Endosc. 2002;16:899–904. doi: 10.1007/s00464-001-8122-x. [DOI] [PubMed] [Google Scholar]
- 35.Huang L, Li J, Lau WY, Yan J, Zhou F, Liu C, Zhang X, Shen J, Wu M, Yan Y. Perioperative reactivation of hepatitis B virus replication in patients undergoing partial hepatectomy for hepatocellular carcinoma. J Gastroenterol Hepatol. 2012;27:158–164. doi: 10.1111/j.1440-1746.2011.06888.x. [DOI] [PubMed] [Google Scholar]
- 36.Kubo S, Nishiguchi S, Hamba H, Hirohashi K, Tanaka H, Shuto T, Kinoshita H, Kuroki T. Reactivation of viral replication after liver resection in patients infected with hepatitis B virus. Ann Surg. 2001;233:139–145. doi: 10.1097/00000658-200101000-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang L, Li J, Yan J, Sun J, Zhang X, Wu M, Yan Y. Antiviral therapy decreases viral reactivation in patients with hepatitis B virus-related hepatocellular carcinoma undergoing hepatectomy: a randomized controlled trial. J Viral Hepat. 2013;20:336–342. doi: 10.1111/jvh.12036. [DOI] [PubMed] [Google Scholar]
- 38.Dan JQ, Zhang YJ, Huang JT, Chen MS, Gao HJ, Peng ZW, Xu L, Lau WY. Hepatitis B virus reactivation after radiofrequency ablation or hepatic resection for HBV-related small hepatocellular carcinoma: a retrospective study. Eur J Surg Oncol. 2013;39:865–872. doi: 10.1016/j.ejso.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 39.Yoshida H, Yoshida H, Goto E, Sato T, Ohki T, Masuzaki R, Tateishi R, Goto T, Shiina S, Kawabe T, et al. Safety and efficacy of lamivudine after radiofrequency ablation in patients with hepatitis B virus-related hepatocellular carcinoma. Hepatol Int. 2008;2:89–94. doi: 10.1007/s12072-007-9020-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fagnoni FF, Zerbini A, Pelosi G, Missale G. Combination of radiofrequency ablation and immunotherapy. Front Biosci. 2008;13:369–381. doi: 10.2741/2686. [DOI] [PubMed] [Google Scholar]
- 41.Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022. doi: 10.1002/hep.24199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cabrera R, Ararat M, Xu Y, Brusko T, Wasserfall C, Atkinson MA, Chang LJ, Liu C, Nelson DR. Immune modulation of effector CD4+ and regulatory T cell function by sorafenib in patients with hepatocellular carcinoma. Cancer Immunol Immunother. 2013;62:737–746. doi: 10.1007/s00262-012-1380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nagai H, Mukozu T, Matsui D, Kanekawa T, Kanayama M, Wakui N, Momiyama K, Shinohara M, Iida K, Ishii K, et al. Sorafenib prevents escape from host immunity in liver cirrhosis patients with advanced hepatocellular carcinoma. Clin Dev Immunol. 2012;2012:607851. doi: 10.1155/2012/607851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tomova R, Antonov K, Ivanova A, Jacobs JJ, Koten JW, Den Otter W, Krastev Z. Low-dose IL-2 therapy reduces HCV RNA and HBV DNA: case report. Anticancer Res. 2009;29:5241–5244. [PubMed] [Google Scholar]
- 45.Tomova R, Pomakov J, Jacobs JJ, Adjarov D, Popova S, Altankova I, Den Otter W, Krastev Z. Changes in cytokine profile during local IL-2 therapy in cancer patients. Anticancer Res. 2006;26:2037–2047. [PubMed] [Google Scholar]
- 46.Peng JW, Lin GN, Xiao JJ, Jiang XM. Hepatitis B virus reactivation in hepatocellular carcinoma patients undergoing transcatheter arterial chemoembolization therapy. Asia Pac J Clin Oncol. 2012;8:356–361. doi: 10.1111/j.1743-7563.2012.01534.x. [DOI] [PubMed] [Google Scholar]
- 47.Roche B, Samuel D, Gigou M, Feray C, Virot V, Schmets L, David MF, Arulnaden JL, Bismuth A, Reynes M, et al. De novo and apparent de novo hepatitis B virus infection after liver transplantation. J Hepatol. 1997;26:517–526. doi: 10.1016/s0168-8278(97)80416-3. [DOI] [PubMed] [Google Scholar]
- 48.Segovia R, Sánchez-Fueyo A, Rimola A, Grande L, Bruguera M, Costa J, Soguero C, Uriz J. Evidence of serious graft damage induced by de novo hepatitis B virus infection after liver transplantation. Liver Transpl. 2001;7:106–112. doi: 10.1053/jlts.2001.21457. [DOI] [PubMed] [Google Scholar]
- 49.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50:661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 50.Liaw YF, Leung N, Kao JH, Piratvisuth T, Gane E, Han KH, Guan R, Lau GK, Locarnini S. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2008 update. Hepatol Int. 2008;2:263–283. doi: 10.1007/s12072-008-9080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.European Association For The Study Of The Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 52.Oketani M, Ido A, Uto H, Tsubouchi H. Prevention of hepatitis B virus reactivation in patients receiving immunosuppressive therapy or chemotherapy. Hepatol Res. 2012;42:627–636. doi: 10.1111/j.1872-034X.2012.00998.x. [DOI] [PubMed] [Google Scholar]


