Abstract
Cervical artery dissection (CAD) is one of the most frequent causes (14.5%) of stroke in young adults. Cases with involvement of more than two arteries are rare. Arnold et al described 11 cases (1.5%) with triple CAD of a reported 740 patients and just a single (0.1%) quadruple case in the same population. Simultaneous dissection of the four principal vessels is extremely rare. According to Papagiannaki et al, the incidence of simultaneous three or four CADs is 1–3/million in the general population. To the best of our knowledge, there are only three published cases of spontaneous quadruple CAD.
Background
We report a unique case of simultaneous triple cervicocephalical arterial occlusion due to spontaneous quadruple cervical artery dissection (CAD) with good outcome in a young woman 1 week after uncomplicated elective caesarian section.1–5
Case presentation
A 32-year-old woman presented to the emergency department with 12 h history of mild right-sided hemiparesis and motor aphasia. In our practice, routine acute stroke MRI protocol includes T1, T2, fluid attenuated inversion recovery, diffusion-weighted imaging (DWI) and angiographic regimens. DWI and MR angiography revealed acute focal ischaemia in the left frontoparietal region consistent with decreased blood supply through left carotid artery (figure 1). Further CT angiography (CTA) revealed occlusion of left internal carotid artery (ICA). There were no signs of occlusion, stenosis or dissection in other major vessels. After initial workup, the patient remained stable with Glasgow Coma Scale (GCS) score of 15. Arterial dissection was suspected. Considering more than 12 h history of symptoms, medical management with anticoagulants was initiated. The patient was admitted to the neurological intensive care unit for observation. On second day of hospitalisation, the patient's condition rapidly deteriorated with acute onset of left-sided hemiparesis and GCS score of 8. She was intubated and taken to the intervention radiology operating room within 90 min of symptom onset.
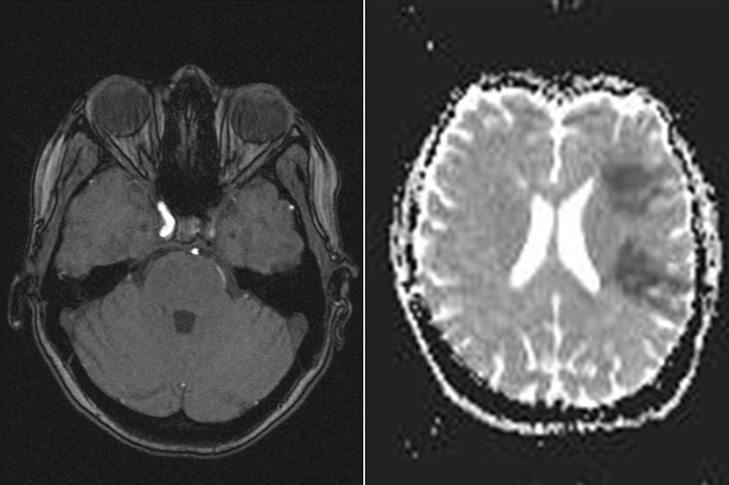
Figure 1.
Initial MRI at admission. Left: T1-weighted gadolinium-enhanced image showing no enhancement from left internal carotid artery. Right: diffusion-weighted image, showing focal acute ischaemia in the left hemisphere.
Treatment
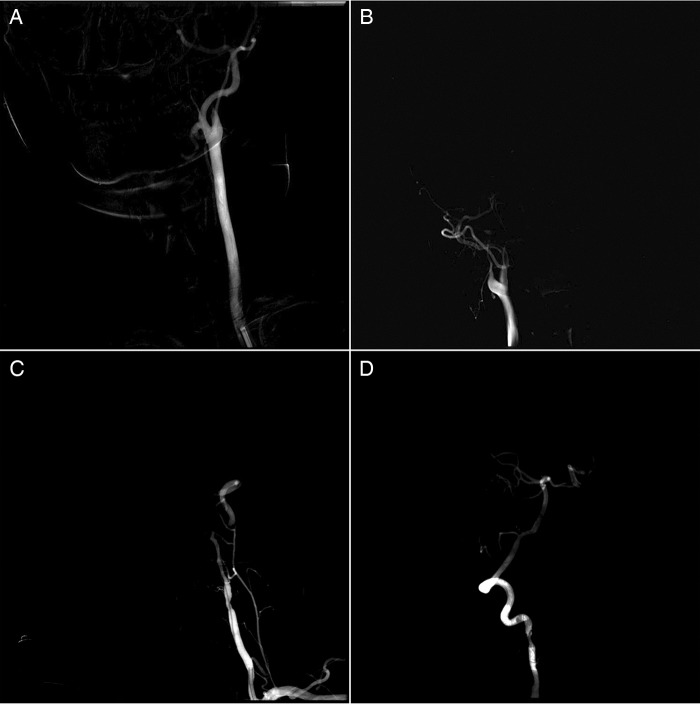
Digital subtracted angiography (DSA) revealed complex pattern of brain blood supply (figure2):
Left ICA was occluded.
Right ICA was also occluded with typical for dissection flame-like shape.
Left vertebral artery (VA) was occluded at C2 level. Intracranial supply of left VA partially was compensated by anastomosis from muscular cervical arterial branch.
Right VA was functional. However, there was irregularity of contrast filling indicating arterial dissection.
Figure 2.
Digital subtracted angiography of four cervicocerebral vessels. (A) Left common carotid artery (CCA), frontal view. Left internal carotid artery (ICA) occluded immediately after CCA bifurcation, with flame-shaped occlusion. (B) Right CCA, lateral view. Flame-shaped occlusion of right ICA. (C) Left vertebral artery (VA), frontal view. Occlusion at C2–C3 level. Intracranial part of VA has partial supply via small anastomosis with muscular branch of the left subclavian artery. (D) Right VA, lateral view. Irregular dissection-like contour of the vessel with stenosis at C2–C3 level. Good collateral flow to the carotid region via posterior communicant artery.
Thus, brain blood supply was entirely dependant on dissected right VA.
Owing to progressing neurological deterioration, a decision was taken to perform revascularisation. Since symptoms manifested with left-sided hemiparesis, right ICA was intervened on. Catheterisation of right ICA distally to occlusion was performed with Rebar microcatheter, followed by one pass thrombextraction with Solitaire AB stent. Although no thrombotic masses were removed, antegrade flow appeared in right ICA. Self-expanded stent Protégé was placed to complete restoration of right ICA lumen (figure 3).
Figure 3.
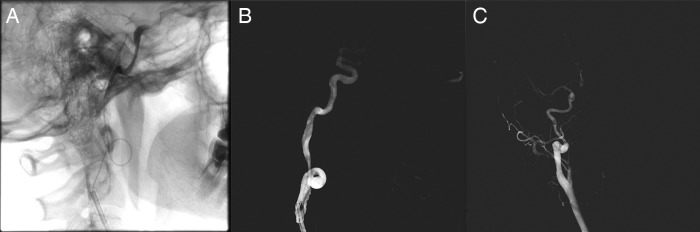
Digital subtracted angiography, stages of right internal carotid artery (ICA) revascularisation. (A) Lateral view: microcatheter passed the occlusion, contrasting the distal part of right ICA. (B) After one pass of stent extraction direct flow appeared, showing irregular dissected vessel wall. (C) After self-expandable nitinol 6×8 × 40 mm, stent implantation lumen of right ICA restored.
Outcome and follow-up
New neurological deficit was resolved in the immediate postoperative period. There were no new signs of right-sided ischaemia on MRI. The patient remained on dual antiplatelet and anticoagulant therapy. She also received a course of neurological rehabilitation.
Two weeks later, DSA of all vessels was performed revealing the following changes (figure 4):
Small antegrade flow in left ICA.
Antegrade flow in left VA.
Normally functioning previously stented right ICA.
Persistent signs of dissection in right VA.
Figure 4.

Digital subtracted angiography, 2 weeks after internal carotid artery (ICA) stenting. All frontal view. (A) Small direct flow of previously occluded left ICA appeared. (B) Direct flow of previously occluded left vertebral artery (VA). (C) Stent implantation to right VA at the site of dissection.
Stenting of right VA with appropriate size Solitaire AB stent was performed at the site of dissection.
During in-hospital neurological rehabilitation, aphasia and right-sided hemiparesis improved gradually and fully resolved at discharge. The patient was sent home neurologically intact and on dual antiplatelet therapy.
At a 3-month follow-up, CTA revealed in-stent thrombosis of right ICA (figure 5). However, other three arteries functioned normally. Left ICA and left VA had adequate blood supply to the brain. The patient remained neurologically intact.
Figure 5.

CT angiography at 3-month follow-up. Left: two-dimensional image showing in-stent thrombosis of right internal carotid artery. Right: three-dimensional image showing no flow at the distal end of stent.
Blood workup showed positive thrombophilic markers: PAI (hom), GP 1a (het), MTGFR (het), MTR (het), MTRR (het), F XIII (het). The patient was referred to a haematologist and received antithrombin-III ×1000ME three times. Since then she has been on clopidogrel 75 mg daily. More than 1 year after her surgery, the patient has continued to do well clinically.
Discussion
In most patients with multiple CADs, antithrombotic treatment is effective and the outcome is favourable.2 Moreover, complete recanalisation is expected in 78% of the dissected vessels and medical treatment is sufficient in most cases with multiple CADs.2 Endovascular treatment may be an option in cases with insufficient collaterals and progressive or new ischaemic symptoms despite antithrombotic treatment.2 In all reported cases with quadruple CAD, patients were on medical treatment with anticoagulants and/or antiplatelet drugs. No interventions were performed. At the same time, none of them had simultaneous three-vessel occlusion of principal cerebral arteries. Clinical progression of multiple arterial dissections in the present case appears to be aggressive. New symptoms occurred while the patient had been receiving anticoagulant therapy. DSA revealed three-vessel cervical arterial occlusion with typical signs of dissection. Right VA, the only functioning vessel supplying the brain, had signs of dissection as well. Two weeks later, direct flow appeared in left ICA and left VA. It was unexpected to find in-stent thrombosis of right ICA despite the patient receiving dual antiplatelet therapy. Fortunately, this thrombosis did not result in new symptoms most likely because of restoration of left ICA. Stent thrombosis was further evidence of the aggressive course of this complex pathology. Blood workup revealed that the patient had a number of thrombophilic markers, such as PAI (hom), GP 1a (het), MTGFR (het), MTR (het) and F XIII (het), which possibly contributed to in-stent thrombosis despite dual antiplatelet therapy. Furthermore, same blood alterations could explain progressive arterial occlusion during anticoagulant therapy in the acute phase of disease. However, thrombophilic markers do not clearly explain aetiology of multiple CAD in this patient. Peripartum arterial dissections have been described.6 They mostly occur in coronary vessels and are often associated with Marfan syndrome, affecting different parts of the aorta. In most cases, manifestation of acute symptoms occurs during delivery.6 Risk factors for arterial dissections after C-section include rapid blood pressure elevation with tachycardia.7 There was no medical record of such clinical presentation during C-section in our patient. Postpartum CADs are rare and usually connected with headache and/or neck pain as initial symptoms, developing between 5 and 18 days after delivery.8 Our patient was asymptomatic during delivery and early postpartum, without headache or neck pain, and neurological deficit occurred suddenly 7 days later. Arnold et al2 reported that two-thirds of patients with three or four CADs were women.
Learning points.
Quadruple cervical artery dissections (CADs) are rare. Despite medical treatment being successful in the majority of cases,9 clinical progression of dissection can be aggressive and intervention may be required.
It takes time to distinguish additional risk factors such as thrombophilic markers, so observation of the patient with multiple CAD in the intensive care unit (ICU) for the first days of disease is imperative.
In the present case, observation in the ICU was crucial for a good outcome, as we had little time for revascularisation of right ICA.
We believe that patients with multiple CAD should be managed in tertiary medical centres as they are fully equipped and capable of fast interventional treatment in cases of insufficiency of medical therapy.10
Footnotes
Contributors: MA was involved in conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content. KNK was involved in administrative support. NSS was involved in acquisition of data or analysis and interpretation of data. NAA was involved in analysis and interpretation of data, administrative support, final approval of the version published.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review : Not commissioned; externally peer reviewed.
References
- 1.Larrue V, Berhoune N, Massabuau P, et al. Etiologic investigation of ischemic stroke in young adults. Neurology 2011;76:1983–8 [DOI] [PubMed] [Google Scholar]
- 2.Arnold M, De Marchis GM, Stapf C, et al. Triple and quadruple spontaneous cervical artery dissection: presenting characteristics and long-term outcome. J Neurol Neurosurg Psychiatry 2009;80:171–4 [DOI] [PubMed] [Google Scholar]
- 3.Papagiannaki C, Cottier JP, Barbier C, et al. Quadruple spontaneous cervical artery dissection following aneurysm embolisation: a rare posttreatment complication. AJNR Am J Neuroradiol 2011;32:E3–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leys D, Bandu L, Hénon H, et al. Clinical outcome in 287 consecutive young adults (15 to 45 years) with ischemic stroke. Neurology 2002;59:26–33 [DOI] [PubMed] [Google Scholar]
- 5.Newell CP, Seller C, Vizhi M, et al. Case report: spontaneous coronary artery dissection during elective caessarian section under spinal anaesthesia. Anaesthesia 2011;66:615–19 [DOI] [PubMed] [Google Scholar]
- 6.Higgins GL, Borofsky JS, Irish CB, et al. Spontaneous peripartum coronary artery dissection presentation and outcome. J Am Board Fam Med 2013;26:82–9 [DOI] [PubMed] [Google Scholar]
- 7.Molina-Martinez FJ, Salinas-Inigo ME, Moreno-Rojas AJ, et al. A quadruple spontaneous dissection of cervicocerebral arteries. Eur J Neurol 2006;13:93–102 [DOI] [PubMed] [Google Scholar]
- 8.Arnold M, Camus-Jacqmin M, Stapf C, et al. Postpartum cervicocephalic artery dissection. Stroke 2008;39:2377–9 [DOI] [PubMed] [Google Scholar]
- 9.Redekop GJ. Extracranial carotid and vertebral artery dissection: a review. Can J Neurol Sci 2008;35:146–52 [DOI] [PubMed] [Google Scholar]
- 10.Coric D, Wilson JA, Regan JD, et al. Primary stenting of the extracranial internal carotid artery in a patient with multiple cervical dissections: technical case report. Neurosurgery 1998;43:956–9 [DOI] [PubMed] [Google Scholar]