Dear Editor:
A 49-year-old Korean woman presented to dermatologic department with asymptomatic multiple pustules with surrounding erythema on whole body. Four days ago, the patient developed a high fever (>40℃) with common cold symptoms. Two days later, erythematous patches occurred on whole body. To evaluate the cause of fever and skin rash, she was admitted in the department of internal medicine and started to treat with empirical antibiotics, 3rd cephalosporin. On the 2nd day of admission, more than 100 non-follicular pustules occurred on the previous erythematous patches. Before the skin eruption occurred, there were no history of skin disease.
Physical examination demonstrated multiple small non-follicular pustules with surrounding erythema on whole body (Fig. 1). Laboratory finding showed leukocytosis with neutrophilia (42.52×109/L, 96.1%), elevated erythrocyte sedimentation rate (89 mm/h) and parvovirus B19 immunoglobulin M (IgM) and IgG were both positive. And on the echocardiography and chest computed tomography, dilated cardiomyopathy with myocarditis was observed. A culture of the blood, sputum, urin and pustule did not produce any growth of organisms. The other laboratory studies were unremarkable. A skin biopsy was performed on pustular lesion of trunk. The histopathologic findings showed subcorneal pustules in the epidermis and perivascular, interstitial infiltration of lymphohistiocytes, neutrophils and a few eosinophils in the dermis (Fig. 2).
Fig. 1.

Multiple nonfollicular pustules with surround erythema on the trunk.
Fig. 2.
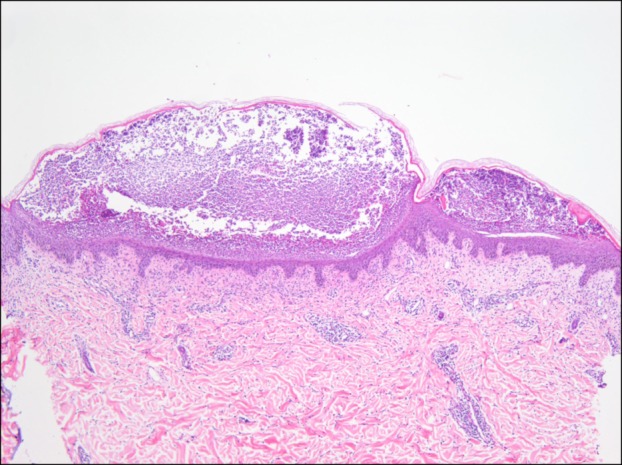
Histopathologic findings shows subcorneal pustules in the epidermis, perivascular and interstitial inflammatory cells infiltration in the dermis. The inflammatory cells are comprised of lymphohistiocytes, neutrophils and a few eosinophils (H&E, ×40).
The patient was dermatologically treated with topical desonide. Despite the ongoing treatment with empirical antibiotics, the pustules resolved within 7 days leaving desquamation and pigmentation.
Acute generalized exanthematous pustulosis (AGEP) is an uncommon cutaneous drug reaction characterized by the acute onset of generalized, non-follicular and sterile pustules on the erythematous background. The eruption can be accompanied by fever and neutrophilc leukocytosis. Although AGEP is induced by drug in over 90% of cases, it can develop without preceding medication history1. Mercury exposure, spider bites, lacquer have been reported to the causes of AGEP, in addition, viral infections may serve as occasional causes.
Parvovirus B19 is a single-stranded nonenveloped DNA virus that can cause several diseases. Its clinical manifestations exist in various forms including arthritis, hematologic disorders, myocarditis and dermatologic involvement such as erythema infectiosum, gloves and socks syndrome2. However, there were only 2 cases of AGEP induced by parvovirus B19 infection in the Englinsh literature3,4. The pathogenesis of AGEP induced by parvovirus B19 is uncertain, it has been thought that viral infection may induce inflammatory cytokines, interleukin 8 or granulocyte-microphage colony stimulating factor and trigger AGEP.
The differential diagnosis of this case is AGEP, generalized pustular psoriasis, subcorneal pustular dermatosis and subcorneal IgA dermatosis. The findings of abscense of psoriasiform acanthosis, tortuous and dilated blood vessels and neutrophils migrate through the epidermis to aggregate beneath the stratum corneum can be differentiated from generalized pustular psoriasis5. Subcorneal pustular dermatosis and subcorneal IgA dermatosis are characterized by the subacute development of larger pustules than present case5. In our patient, the clinical course and histopathologic finding corresponded with AGEP, the cause was parvovirus B19 infection confirmed by serologic test. To our knowledge, AGEP induced parvovirus B19 is a rare entity, we should keep in mind that parvovirus B19 is one of the causative agent of AGEP.
References
- 1.Sidoroff A, Dunant A, Viboud C, Halevy S, Bavinck JN, Naldi L, et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR) Br J Dermatol. 2007;157:989–996. doi: 10.1111/j.1365-2133.2007.08156.x. [DOI] [PubMed] [Google Scholar]
- 2.Vafaie J, Schwartz RA. Parvovirus B19 infections. Int J Dermatol. 2004;43:747–749. doi: 10.1111/j.1365-4632.2004.02413.x. [DOI] [PubMed] [Google Scholar]
- 3.Perceau G, Derancourt C, Salmon-Ehr V, Durlach A, Raclot P, Bredard V, et al. Acute generalized exanthematous pustulosis in hypercalcemia. Ann Dermatol Venereol. 2000;127:1090–1093. [PubMed] [Google Scholar]
- 4.Ofuji S, Yamamoto O. Acute generalized exanthematous pustulosis associated with a human parvovirus B19 infection. J Dermatol. 2007;34:121–123. doi: 10.1111/j.1346-8138.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 5.Fernando SL. Acute generalised exanthematous pustulosis. Australas J Dermatol. 2012;53:87–92. doi: 10.1111/j.1440-0960.2011.00845.x. [DOI] [PubMed] [Google Scholar]


