Dear Editor:
Nipple eczema, considered mostly as a minor manifestation of atopic dermatitis, may have unknown causes. However, its clinical course and pattern often make it difficult to differentiate its underlying causes such as irritation or sensitization. Nevertheless, allergic contact dermatitis must be considered an important cause of nipple eczema.
In the present study, we analyzed the patch test results from pateints of nipple eczema by using the Korean standard series comprising 25 antigens (Chemotechnique Diagnostics, Malmo, Sweden). Antigens were carefully added into an IQ Ultra chamber® (Chemotechnique Diagnostics) which is made of additive-free polyethylene plastic foam with a filter paper incorporated, and stuck to the backs of the patients. Results were recorded 30 minutes after patch removal (as usual), and the patients were re-evaluated 48 hours later. On the basis of the recommendations of the International Contact Dermatitis Research Group, a reading of +1 (patients with erythematous papules and edema but without any vesicles) or higher was deemed a positive response.
Among a total of 12 patients (all women) who were patch tested, 5 were clearly diagnosed with atopic dermatitis on the basis of their medical history and physical examination results. Nine patients showed a positive response to more than 1 antigen. Of 5 patients with a history of atopic dermatitis, 4 patients (80%) showed a positive response. Antigens with a high frequency of positive responses were, in decreasing order of frequency, Cl+Me-isothiazolinone, cobalt chloride, thimerosal, nickel sulfate, and 4-tert-butylphenol-formaldehyde resin (Table 1).
Table 1.
Patch test results for 12 patients with nipple eczema
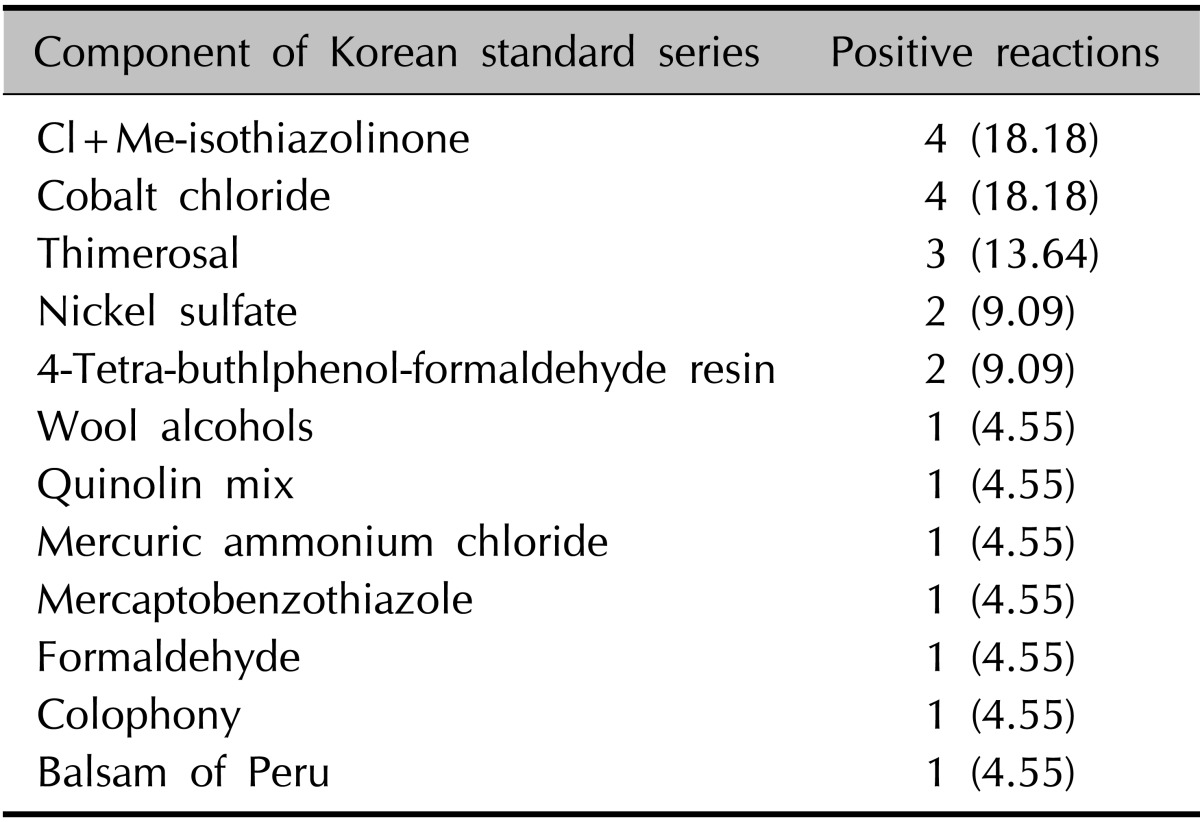
Values are presented as number (%).
Of 9 patients who had positive patch test responses, 7 (77.78%) had a bilateral distribution of lesions, and 8 patients (88.89%) showed spreading of lesions over the periareolar skin. With respect to the progression of eczema, 8 patients (88.89%) had acute lesions. However, 3 patients with negative patch test responses showed only unilateral lesions, which were restricted to the nipple and areola rather than the periareolar skin. Thus, there was a significant difference with respect to the involved area and distribution of the lesions (p<0.05) (Table 2).
Table 2.
Clinical characteristics of nipple eczema according to distribution of lesion and history where the positive patch test reaction indicated allergic contact dermatitis
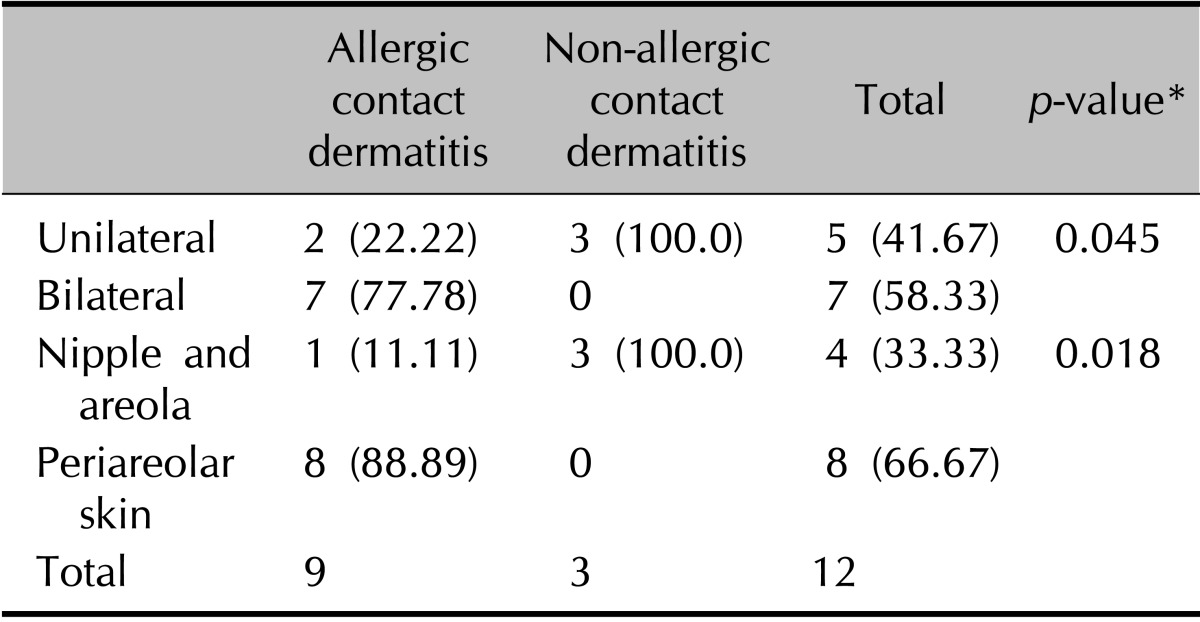
Values are presented as number (%). *Statistical Package for Social Sciences software (SPSS ver.15.0; SPSS Inc., Chicago, IL, USA) was used for data analysis. Categorical data were compared using a Fisher's exact test. Statistically significant differences are indicated by p-values <0.05.
Nine patients with a positive patch test were advised to avoid the use of products containing the positive antigens, after which 5 patients (56%) showed reduced recurrence of nipple eczema.
Nipple eczema is a characteristic minor dermatologic finding indicating atopic dermatitis1. Nevertheless, cases in which nipple eczema was not a characteristic finding of atopic dermatitis have been reported2,3. If nipple eczema does not improve after conventional treatment for atopic dermatitis, or if active symptoms of eczema such as severe erythema and exudation are limited to areas that are frequently affected by atopic dermatitis, allergic contact dermatitis should always be considered first. In this study, positive patch tests to ≥1 antigens were found in 9 of 12 patients (75%). According to an epidemiological survey by the Korean Contact Dermatitis Research Group, Cl+Me-isothiazolinone is not considered a frequent antigen; however, in the present study, this antigen provoked positive responses as frequently as metal ions did. Cl+Me-isothiazolinone is commonly found in preservatives, deterge nts, and fabric softeners; therefore, traceable amounts remaining in undergarments after washing or in personal-care products may act as antigens. Both repeated contact, even at the subclinical threshold, and a weak barrier function in skin affected by atopic dermatitis can contribute to the development of contact sensitization. To prevent chronic recurrent contact dermatitis, the causative antigens should be identified by screening with patch test series, and an avoidance-learning program should be followed4.
We found considerable clinical improvements and reduced recurrence in 5 of the 9 patients who had positive patch tests and followed an avoidance-learning program. In conclusion, allergic contact dermatitis should be considered first in the differential diagnosis of nipple eczema, especially in patients showing bilateral lesions and lesions extending into the periareolar skin.
References
- 1.Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol (Stockh) 1980;60:44–47. [Google Scholar]
- 2.Nagaraja, Kanwar AJ, Dhar S, Singh S. Frequency and significance of minor clinical features in various age-related subgroups of atopic dermatitis in children. Pediatr Dermatol. 1996;13:10–13. doi: 10.1111/j.1525-1470.1996.tb01178.x. [DOI] [PubMed] [Google Scholar]
- 3.Kanwar AJ, Dhar S, Kaur S. Evaluation of minor clinical features of atopic dermatitis. Pediatr Dermatol. 1991;8:114–116. doi: 10.1111/j.1525-1470.1991.tb00297.x. [DOI] [PubMed] [Google Scholar]
- 4.Saint-Mezard P, Rosieres A, Krasteva M, Berard F, Dubois B, Kaiserlian D, et al. Allergic contact dermatitis. Eur J Dermatol. 2004;14:284–295. [PubMed] [Google Scholar]


