Abstract
Mutations of the skeletal muscle voltage-gated sodium channel (NaV1.4) are an established cause of several clinically distinct forms of periodic paralysis and myotonia. Focal paresis has sometimes already been described. We report a case with atypical clinical manifestation comprising paramyotonia and cold-induced persistent and focal paralysis. A 27-year-old woman presented with paramyotonia congenita since her childhood. She experienced during her childhood one brief episode of generalised weakness. At the age of 27, she experienced a focal paresis lasting for several months. The known mutation p.Val1293Ile was found in the muscle sodium channel gene (SCN4A). Channel inactivation is involved in most Na+ channelopathies. Fast inactivation is known to be responsible for the myotonia phenotype. We hypothesise that the V1293I mutation may also alter the slow inactivation in specific conditions, for example, prolonged cold exposure or prolonged and intensive exercise. This observation broadens the spectrum of clinical manifestations of this sodium channel mutation.
Background
Hyperkalaemic periodic paralysis, hypokalaemic periodic paralysis type 2 and paramyotonia congenital are sodium channel disorders, clinically heterogeneous. These disorders are due to episodic membrane hypoexcitability or hyperexcitability of skeletal muscles. The phenotypic variability of these allelic disorders is not well understood. Atypical clinical presentations provide an opportunity to gain new insights into these genotype–phenotype associations.
We report the case of a patient presenting with an atypical phenotype of paramyotonia congenita (PMC) and transient paralysis associated with a sodium channel mutation. One palsy attack was specifically particular because of its focal feature and its long duration.
Case presentation
A 27-year-old woman, with an unremarkable medical history, presented with moderate myotonia since her childhood. The myotonia was made worse by exercise and the cold. At the age of 15, she presented generalised weakness (except the face) after a swimming event in cold water. She was unable to walk at that time. The attack persisted over 6 h and was considered as tetany.
During her first pregnancy, she noticed a worsening of muscle stiffness and asked for medical advice for the first time. The clinical examination, performed at room temperature, revealed myotonia in the four limbs, worsened by exercise. Percussion myotonia was also present. There was no lid-lag phenomenon or face myotonia. There was no hypertrophic muscle or weakness and the general clinical examination was normal.
Investigations
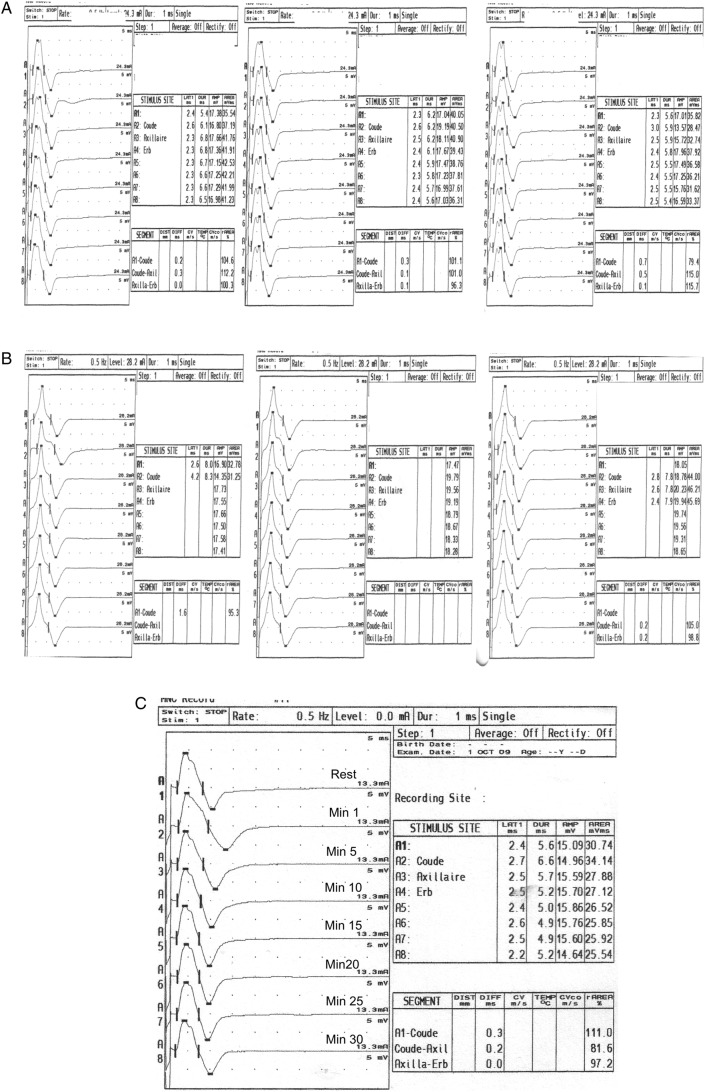
Motor and sensory conduction nerve velocities were normal in all four limbs. Electroneuromyography (ENMG) showed numerous myotonic discharges in limb muscles. Repetitive exercise induced no reduction in the amplitude of the compound motor action potentials (CMAP) and provocative test did not show any change of the CMAP1 (figure 1A–C). The standard biological data, including creatine kinase and potassium levels, were within the normal range. The transthoracic echocardiography and the 24 h ECG recording were normal. Myotonic dystrophies 1 and 2 were ruled out by molecular analysis. The molecular analysis of the muscle sodium channel gene (SCN4A) by nucleotide sequencing found the already described,2 mutation p.Val1293Ile. No mutation was found in CLCN1 gene.
Figure 1.
No change in the ulnar CMAP amplitude (<20%) during all provocative repetitive exercises. (A) Repeated short exercises at room temperature. (B) Repeated short exercises at cold. (C) Long exercise during the acute paralysis.
Treatment
This patient was treated by mexiletine (400 mg/day). The improvement was so dramatic that she could again train for swimming. Unfortunately, she suddenly presented a paresis of the left arm (dominant side) after a strong activity of crawl swimming. The clinical examination at day 3 showed a proximal paresis of the left arm. The deltoid muscle was grade 2, the biceps muscle grade 4 and the triceps muscle grade 4 on the MRC (Medical Research Council) scale. There was no pain or hypaesthesia. Serum potassium was normal. Electromyography showed no spontaneous activity except myotonic discharges. Provocative long exercise test1 was normal (figure 1A–C). The spinal and plexus MRIs were normal. Mexiletine was stopped 1 week without effect. One month later, the patient was slightly improved. Her ENMG examination did not show any denervation activity or neuropathic recruitment. The patient slowly recovered over a 2–3-month period and clinical and electrical examinations were normal 6 months after onset (except clinical and electrical myotonia). Her mother presented with a clinical history of stiffness only during her pregnancies suggestive of myotonia. Myotonic discharges were confirmed by the EMMG study and the same p.Val1293Ile mutation was found. Still, she had never presented any similar periodic paralysis.
Discussion
The mutation p.Val1293Ile in the adult skeletal muscle sodium channel α subunit (SCN4A) gene was originally reported to cause PMC.2 In these first cases, the PMC was mild and not associated with cold paralysis like in Eulenbourg paramyotonia. Indeed, these patients never presented with periodic paralysis. Therefore, the clinical phenotype observed in our patient carrying the same mutation raises some questions. This woman presented with paradoxical myotonia and two episodes of transient severe weakness. Based on the clinical features of the myotonia, she was classified as having congenital paramyotonia because of the worsening with exercise and in accordance with the cases already described. However, the myotonia was only moderately worsened by cold and we did not observe the decrease in CMAP after exercise or cooling usually seen in PMC during the ENMG provocative test. Fournier et al1 have already reported pattern III (no change in CMAP) in patients carrying this mutation. They associate this pattern with absence of paresis episodes. Nevertheless, our patient presented two episodes of acute paralysis triggered by exercise. We suggest that the provocative test lacked sensitivity in our case. It may be due to a low intensity of the effort in these tests: both episodes of paralysis arose while practising intensive swim exercise. The paralysis of this woman may be in relation with the weakness encountered in patients with paramyotonia after exercise. Nevertheless, this weakness is usually not so persistent and severe. A focal periodic paralysis could be discussed as some focal paresis has also been described, usually related with an important muscular activity.3 However, the paralysis is usually brief, lasting only for some hours or a few days and happened classically at rest, unlike our patient. In consequence, the phenotype of our patient may be described as a combination of exercise aggravated myotonia and exercise periodic paralysis—with a palsy particular because of its focal feature and its long duration, broadening the clinical spectrum of this SCN4A mutation.
Patients carrying SCN4A mutations usually present with periodic paralysis and myotonia, actually showing variable combination of paramyotonia, potassium aggravated myotonia and periodic paralysis (hyperkalaemia or hypokalaemia).4–6 The functional studies of the implicated mutations have already showed impairment in the activation and the slow inactivation of the channel.7 Green et al8 have demonstrated that p.Val1293Ile mutation causes alterations in the activation and the fast inactivation that are likely the direct cause of the myotonia. The V1293I mutation is biochemically a conservative substitution that increases the length of an aliphatic side chain by a methyl group. It is predicted to lie near the cytoplasmic end of S6 in domain III. This site may reside near the intracellular mouth of the ion conducting pore and consequently may affect the fast inactivation mediated by docking of the interdomain III–IV loop or any component of activation that involved rearrangement of the cytoplasmic face of the pore.9 10 However, Green et al did not show any alteration of the slow inactivation whose defect is classically associated with a preferential susceptibility to periodic paralysis. Nevertheless, they studied the slow inactivation only at room temperature. Two studies showed that slow inactivation is affected by cold exposure. Carle et al11 have reported PMC associated with particular weakness at cold exposure. They demonstrated that cooling was able to destabilise slow inactivation. Webb et al12 also showed a temperature sensitivity of slow inactivation in a family with hypokalemic paralysis at cold temperatures and myotonia at warm ones. We could hypothesise that the V1293I mutation led to paresis in our patient because of a combination of some sensitivity of slow inactivation to cold environment (swimming pool) and an increased membrane depolarisation due to prolonged and intense exercise.
Moreover, a pattern is emerging wherein all of the paralysis-associated mutations that disrupt slow inactivation are at the cytoplasmic end of the fifth or sixth transmembrane segments in domains II, III or IV, which are predicted to be the inner vestibule of the ion-conducting pore.
Learning points.
This observation points out that the congenital paramyotonia in relation with the sodium channel might be associated with persistent paralysis, likely through abnormal slow inactivation. The patients should therefore be informed of that risk. In case of frequent periodic paralysis attacks, they could benefit from acetalozamide treatment in association with mexiletine.
Acknowledgments
AM, DS and YP are members of RESOCANAUX, whose contribution to this work is acknowledged.
Footnotes
Contributors: AM followed up with the patient and wrote the manuscript AD had seen the patient for the genetic council. DS carried out the genetic testing. YP followed up with the patient and edited the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fournier E, Arzel M, Sternberg D, et al. Electromyography guides toward subgroups of mutations in muscle channelopathies. Ann Neurol 2004;56:650–61 [DOI] [PubMed] [Google Scholar]
- 2.Koch MC, Baumbach K, George AL, et al. Paramyotonia congenita without paralysis on exposure to cold: a novel mutation in the SCN4A gene (Val1293Ile). Neuroreport 1995;6:2001–4 [DOI] [PubMed] [Google Scholar]
- 3.Plassart E, Eymard B, Maurs L, et al. Paramyotonia congenita: genotype to phenotype correlations in two families and report of a new mutation in the sodium channel gene. J Neurol Sci 1996;142:126–33 [DOI] [PubMed] [Google Scholar]
- 4.Burge JA, Hanna MG. Novel insights into the pathomechanisms of skeletal muscle channelopathies. Curr Neurol Neurosci Rep 2012;12:62–9 [DOI] [PubMed] [Google Scholar]
- 5.Yoshinaga H, Sakoda S, Good JM, et al. A novel mutation in SCN4A causes severe myotonia and school-age-onset paralytic episodes. J Neurol Sci 2012;315:15–19 [DOI] [PubMed] [Google Scholar]
- 6.Lehmann-Horn F, Orth M, Kuhn M, et al. A novel N440K sodium channel mutation causes myotonia with exercise-induced weakness–exclusion of CLCN1 exon deletion/duplication by MLPA. Acta Myol 2011;30:133–7 [PMC free article] [PubMed] [Google Scholar]
- 7.Lossin C, Nam TS, Shahangian S, et al. Altered fast and slow inactivation of the N440K Nav1.4 mutant in a periodic paralysis syndrome. Neurology 2012;79:1033–40 [DOI] [PubMed] [Google Scholar]
- 8.Green DS, George AL, Jr, Cannon SC. Human sodium channel gating defects caused by missense mutations in S6 segments associated with myotonia: S804F and V1293I. J Physiol 1998;510(Pt 3):685–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Catterall WA. Molecular mechanisms of gating and drug block of sodium channels. Novartis Found Symp 2002;241:206–18 [PubMed] [Google Scholar]
- 10.Goldin AL. Mechanisms of sodium channel inactivation. Curr Opin Neurobiol 2003;13:284–90 [DOI] [PubMed] [Google Scholar]
- 11.Carle T, Fournier E, Sternberg D, et al. Cold-induced disruption of Na+ channel slow inactivation underlies paralysis in highly thermosensitive paramyotonia. J Physiol 2009;587:1705–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webb J, Cannon SC. Cold-induced defects of sodium channel gating in atypical periodic paralysis plus myotonia. Neurology 2008;70:755–61 [DOI] [PMC free article] [PubMed] [Google Scholar]