Abstract
Urinary bladder ruptures (UBR) typically result from either blunt or penetrating trauma, or from iatrogenic surgical injuries. Patients typically present with symptoms including lower abdominal pain, haematuria, dysuria and anuria. Here, we report on a rare case of spontaneous bladder perforation. A 60-year-old, Caucasian woman initially presented with lower abdominal pain and diarrhoea, and was subsequently found to have an elevated serum creatinine level. A CT cystogram revealed a leak from the bladder. The patient consented to exploratory laparotomy and repair of the non-traumatic bladder perforation. At the time of the last follow-up, given the fact that the patient’s urodynamics were unremarkable and that she was emptying her bladder well (repeat postvoid residual was zero), the patient was informed that she did not require future urological follow-up unless difficulties arise.
Background
Urinary bladder ruptures (UBR) typically occur as a result of either blunt or penetrating trauma, or from iatrogenic surgical injury. Bladder perforations can be extraperitoneal or intraperitoneal, with the latter requiring prompt abdominal exploration and repair. Typically, patients with intraperitoneal bladder perforation present with lower abdominal pain and symptoms including haematuria, dysuria and anuria.1 The abdominal discomfort is generally accompanied by distension, scattered abdominal pain, urinary retention and oliguria following bladder catheterisation.2 However, the presence of urine in the bladder does not necessarily rule out the possibility of a rupture. In 45% of intraperitoneal UBR cases, plasma urea and creatinine levels are elevated within the first 24 h following perforation. After this 24 h window, patients have elevated urea levels due to greater peritoneal absorption.3 4
Several factors including pelvic malignancy and subsequent radiotherapy, pregnancy, previous bladder surgery, trauma, binge alcohol drinking and diabetes have been associated with an increased risk of urinary bladder rupture.5 As a result of these diverse risk factors, a UBR can potentially occur at a range of sites within the bladder. Ruptures at the dome of the urinary bladder are most likely attributed to binge alcohol intake, while those on the posterior wall have been shown to be connected with irradiation therapy. Ruptures at the anterior wall are mainly observed in postpartum women.6
Here, we present a rare case of a spontaneous bladder rupture in a 60-year-old, Caucasian woman in whom no obvious predisposing comorbidity or event could be rationalised as a causative factor.
Case presentation
A 60-year-old, Caucasian woman with prior medical history remarkable for migrane, dyslipidaemia and rheumatoid arthritis initially presented to the emergency room with lower abdominal pain of increasing intensity, diarrhoea and nausea over the prior 5 days. She had initially presented to the emergency room 2 days earlier, but was sent home after a computerised axial tomography scan of the abdomen did not reveal any acute pathology. The patient had no urinary output for approximately 18 h prior to presentation in the emergency room. Surgical history was significant for a total abdominal hysterectomy with bilateral salpingo-oophorectomy secondary to endometriosis 20 years previously. She did not report any recent significant traumatic accident.
Investigations
An abdominal examination revealed marked distension with diffuse tenderness to palpation and no signs of guarding or rebounding. Bowel sounds were diminished and almost absent. The patient underwent a CT of the abdomen and pelvis with contrast, which showed significant amounts of retained stool as well as a large distended bladder. She was given pain medication and discharged but was readmitted shortly afterwards due to worsening pain. The patient also developed loose stools following barium ingestion from her previous contrast and described episodes of nausea. A subsequent CT scan revealed ascites, and the patient had elevated serum creatinine. A CT cystogram revealed a bladder perforation (figure 1A).
Figure 1.
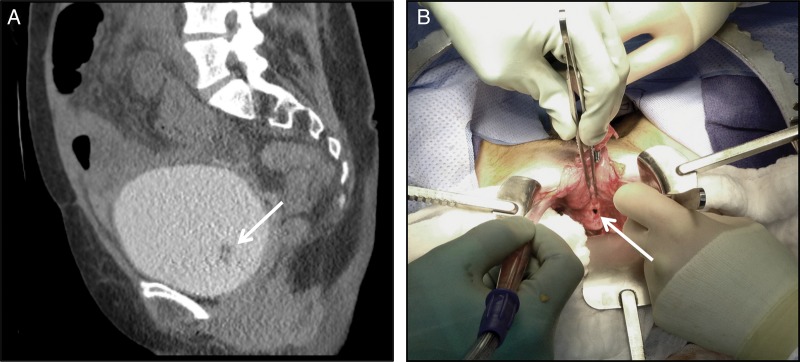
(A) preoperative CT cystogram illustrating perforation of the bladder (arrow). (B) Perioperative image showing the location of the bladder perforation (arrow).
Treatment
The patient consented to exploratory laparotomy and repair of the non-traumatic bladder perforation. Intraoperatively, there was free fluid within the abdomen, and the bladder demonstrated a 1 cm, intraperitoneal perforation at the posterior wall in the right aspect of the midline (figure 1B). The cystotomy was extended and the bladder was inspected and repaired in two layers. The thin-walled interior of the bladder did not show any signs of lesions. Bilateral orifices were noted in the normal anatomic position, and efflux from these orifices was confirmed via injection of intravenous indigo carmine. The patient tolerated the procedure well without any complications and was extubated in the operating room prior to her transfer to the recovery room in stable condition and with minimal blood loss. Foley catheter and Jackson-Pratt drains were positioned in place, and postoperatively, vital signs remained stable and abdominal pain was improved.
Outcome and follow-up
During a subsequent follow-up visit at 2 weeks, a cystogram was obtained and confirmed that the patient's bladder had healed.
At 1 month following surgery, a urodynamic study was performed. Bladder capacity was 215 mL, and compliance was mildly impaired but within the normal range. No detrusor overactivity was noted and the bladder did not exhibit spasticity. She emptied her bladder well (flow rate 14 mL/s) with a bladder pressure of 29 cm H2O at peak flow. There was no evidence of a remaining perforation, and the patient has continued to be able to void spontaneously with a low postvoid residual volume. She did not subsequently require any future urological follow-up.
Discussion
A spontaneous bladder rupture is an extremely rare clinical scenario that has been shown to have an associated 50% mortality rate.7 Predisposed conditions associated with an increased risk of rupture include previous pelvic radiotherapy or bladder surgery, trauma and pregnancy. There has also been an increase in the number of patients with spontaneous rupture in non-diseased bladders due to binge alcohol consumption.8 While imaging modalities, including retrograde cystography, delayed CT cystography and CT retrograde cystography have been utilised to evaluate patients with suspected bladder injuries,9 it is often challenging to clinically diagnose a bladder perforation.
The clinical management of urinary bladder ruptures varies depending on the location of perforation. Extraperitoneal ruptures are generally treated conservatively, while those occurring intraperitoneally at the bladder dome require surgical intervention and management. Traditionally, intraperitoneal bladder perforations attributed to iatrogenic intervention or trauma have been successfully treated using open or laparoscopic surgery. However, Lima et al10 have also shown the efficacy and safety of endoscopic closure of vesical perforations in a survival porcine pig model, using an endoscopic suturing kit (T-fasteners with a locking cinch). This endoscopic approach may possibly offer quicker recovery times and shorter hospitalisation, as compared with laparotomy or laparoscopy. However, limitations of this approach may include potential for inadvertent bowel injury with full thickness sutures secondary to inability to visualise intraperitoneal organs during suturing. Furthermore, with an endoscopic approach there is potential for further extravasation of bladder irrigant during suturing. Further investigation is required to define the potential for human application. In this situation, laparoscopic approaches may also be appropriate. While there have been a number of well-documented cases of patients who had comorbidities that were likely related to a bladder rupture, there are limited data characterising the general aetiological factors that contribute to bladder wall weakness.11 In men with benign prostatic hyperplasia, the prostate has been suggested to contribute to bladder rupture through creating chronic bladder outlet obstructions that increase postvoidal residual volume. Besides chronic constipation, there was no clear factor that contributed to the spontaneous perforation in this case.
Our case suggests that, to make an accurate and timely diagnosis of UBR, a high degree of clinical vigilance is warranted when a patient presents to the emergency room or clinic with lower abdominal pain, chronic constipation or acute renal failure.
Learning points.
Urinary bladder ruptures typically occur as a result of blunt or penetrative trauma, or during surgery.
However, bladder rupture may also occur spontaneously, in the absence of any apparent comorbidity or event.
When a patient presents with lower abdominal pain, chronic constipation or acute renal failure, a high degree of clinical vigilance is required to make an accurate diagnosis and to define the appropriate course of treatment.
Acknowledgments
The authors would like to acknowledge the assistance of Peter Haddock PhD in the preparation of this report.
Footnotes
Contributors: AM and FA-C conceived the idea of the study and were responsible for the design of the study. AC and FA-C undertook the data analysis. The initial draft of the manuscript was prepared by AC and FAC and then circulated repeatedly among all authors for critical revision.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ahmed J, Mallick IH, Ahmad SM. Rupture of urinary bladder: a case report and review of literature. Cases J 2009;2:7004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Limon O, Unluer EE, Unay FC, et al. An unusual cause of death: spontaneous urinary bladder perforation. Am J Emerg Med 2012;30:2081. [DOI] [PubMed] [Google Scholar]
- 3.Zonca P, Cambal M, Jacobi CA. Laparoscopic management of spontaneous intraperitoneal perforation of urinary bladder. Bratisl Lek Listy 2011;112:282–6 [PubMed] [Google Scholar]
- 4.Mardani M, Shahzadi M, Rakhshani N, et al. Spontaneous perforation of urinary bladder secondary to Candida cystitis: acute abdomen of urologic origin. Surg Infect (Larchmt) 2008;9:525–7 [DOI] [PubMed] [Google Scholar]
- 5.Mitchell T, Al-Hayek S, Patel B, et al. Acute abdomen caused by bladder rupture attributable to neurogenic bladder dysfunction following a stroke: a case report. J Med Case Rep 2011;5:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vohra SB, Kapur S. Diagnosis of bladder rupture by arterial blood gas analysis. Anaesthesia 2007;62:534–5 [DOI] [PubMed] [Google Scholar]
- 7.Basavaraj DR, Zachariah KK, Feggetter JG. Acute abdomen-remember spontaneous perforation of the urinary bladder. J R Coll Surg Edinb 2001; 46:316–17 [PubMed] [Google Scholar]
- 8.Parker H, Hoonpongsimanont W, Vaca F, et al. Spontaneous bladder rupture in association with alcoholic binge: a case report and review of the literature. J Emerg Med 2009;37:386–9 [DOI] [PubMed] [Google Scholar]
- 9.Daignault MC, Saul T, Lewiss RE. Bedside ultrasound diagnosis of atraumatic bladder rupture in an alcohol-intoxicated patient: a case report. Crit Ultrasound J 2012;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lima E, Rolanda C, Osório L, et al. Endoscopic closure of transmural bladder wall perforations. Eur Urol 2009;56:151–7 [DOI] [PubMed] [Google Scholar]
- 11.Haddad FS, Pense S, Christenson S. Spontaneous intraperitoneal rupture of the bladder. J Med Liban 1994;42:149–54 [PubMed] [Google Scholar]


