Abstract
Background & objectives:
Although depression is a significant co-morbid condition in chronic illnesses, little is known about the prevalence or risk factors for depressive symptoms in patients with chronic obstructive pulmonary disease (COPD) in India. This study was undertaken to investigate the presence and risk factors of depression in the COPD patients attending a tertiary care health facility in north India.
Methods:
COPD was classified according to GOLD stages based on forced expiratory volume in one second (FEV1) in 126 stable patients. Depression was examined by administering the nine-item Hindi version of Patient Health Questionnaire-9 (PHQ-9). Linear regression model was used to examine association between predictor variables and risk of depression with adjustment of age and sex. Cronbach alpha was calculated to assess internal consistency of PHQ-9.
Results:
In the study population as whole, 33.3 per cent patients showed moderate to severe depressive symptoms whereas 20.6 per cent patients had major depressive disorder on PHQ-9 Scale. Educational and occupational status, body mass index, FEV1, respiratory symptoms, physical impairment and dyspnoea were found to be potential predictors of depression in COPD patients.
Interpretation & conclusions:
One fifth of the patients with COPD had severe symptoms of related to depression, which was especially higher with severity of COPD. Hence, the patients with COPD should focus on management of these two conditions. Further, future studies should be conducted to assess the role of depression management and timely treatment of it in patients with COPD.
Keywords: COPD, depression, GOLD, North India, Tertiary care centre
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) defines chronic obstructive pulmonary disease (COPD) as “a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients”1. It is characterized by airflow obstruction leading to slowly progressive symptoms of persistent cough, exertional dyspnoea, wheezing and eventual functional impairment. Global Burden of Disease and Risk Factors project1 shows that COPD is the leading cause of death and disability-adjusted life years (DALYs) in high-income countries, and in nations of low and middle income2.
Prevalence of COPD in India lies between 6.6 to 7.7 per cent and it contributes significantly to mortality and DALYs3. Previous studies have reported the prevalence of depressive symptoms in COPD patients ranging from 6 to 56 per cent4,5,6,7. The impact of COPD on individuals living with the disease depends upon multiple factors in addition to the medical burden, ranging from patients’ circumstances, expectations to coping skills and psychological wellbeing. In individuals with COPD, depression is significantly associated with decreased functional status, impaired quality of life (QoL)8 and disease progression and mortality9.
Patients with depression may not adhere to their management programmes such as the pulmonary rehabilitation10, and smoking cessation11. Therefore, depression may lead to poor clinical outcomes. It has been shown that depression leads to higher healthcare use with higher admission and relapse rate in emergency department patients12. Ultimately, the presence of depression in patients with COPD leads to higher economic burden.
Given the significant burden associated with presence of depression in patients with COPD, screening and early treatment of depressive symptoms is considered to be important. Therefore, we conducted a study to estimate the presence of depression in patients with COPD visiting a tertiary care centre in north India. Further, the association of depression with demographic and clinical characteristics of COPD patients was also examined.
Material & Methods
Study design: This cross-sectional, non-randomized study was carried out from November 2011 to April 2012 at Indira Gandhi Medical College & Hospital, Shimla, Himachal Pradesh, India. All consecutive patients with COPD attending the Chest Outpatient Clinic, who met the inclusion criteria, were evaluated. A diagnosis of COPD was established based on medical history, current symptoms, suggestive findings from physical examination and available pulmonary function tests, as per the definitions provided by American Thoracic Society and European Respiratory Society13. The main inclusion criteria for the study were (i) clinically stable patients with no exacerbations and change in medication during last four weeks, and (ii) post-bronchodilator ratio of forced expiratory volume in one second to forced vital capacity less than 0.70 (FEV1/FVC<0.70). The exclusion criteria were asthma or any current respiratory disorder other than COPD, and serious, unstable cardiovascular disease, as these affect the QoL of COPD patients. The study protocol was approved by the institutional ethics committee. Written informed consent was obtained from each participant prior to study.
Measurement of depression: Depression was evaluated with the validated Hindi version14 of nine item PHQ-9 (a subset of Patient Health Questionnaire). PHQ-9 is a self-report version of Primary care Evaluation of Mental Disorders (PRIME-MD)15. PHQ-9 consists of nine criteria on which the diagnosis of DSM-IV depressive disorders is based16. The PHQ-9 is a dual-purpose instrument that, with the same nine items, can establish provisional depressive disorder diagnosis as well as grade depressive symptom severity. Each of the nine items of PHQ-9 was scored from 0 (not at all) to 3 (nearly every day). Total score ranged from 0 to 27 and depending upon the total score, severity of depression was classified as follows: none (0-4), mild (5-9), moderate (10-14), moderately severe (15-19) and severe (20-27).
Other variables: Lung function impairment was assessed by spirometry after inhalation of 400 μg salbutamol using a computerized spirometer (Model vitalograph 6800; SN.PN-06011 Vitalgraph Ltd., Ireland). In addition, information on the following variables was obtained by using questionnaire: age, sex, highest form of education received (low level: illiterate and primary education; high level: secondary education and graduate), occupational status (working and non working) and anthropometric measurements. International classification of underweight, overweight and obesity was used to define obesity (i.e. BMI for underweight <18.5, normal 18.5 - 24.9, overweight ≥25 and obese ≥30 kg/m2)17. Participants were asked about their smoking habits and exposure to biomass fuel. Smoking index18 was calculated which is a product of average number of cigarettes smoked per day and the total duration of smoking in years.
Based on the response of the patient, the patients breathlessness was scored using Medical Research Council (MRC) Dyspnoea scale19. The MRC Dyspnoea Scale concerns perceived breathlessness and consists of five degrees: 1 - shortness of breath with strenuous exercise; 2 - shortness of breath when hurrying; 3 - walking slower than people of same age; 4 - needing to stop after walking 100 yards on level ground; 5 - too breathless to leave the house20.
The St George's Respiratory Questionnaire (SGRQ) is a disease specific HRQL (health related quality of life) questionnaire21 and in this study validated Hindi version of SGRQ was used22. Symptoms and physical functioning were assessed using the symptoms and activity domains of the SGRQ. The “regeneration” domain relates to the frequency and severity of respiratory symptoms, and the “regeneration” domain focuses on physical activities that either cause or are limited by dyspnoea. Both components were computed using item specific weights assigned to each question. The scores range from 0 to 100 and a higher score indicates a worst HRQL23.
Statistical analysis: Depending on the variable distribution, results were expressed as numbers, percentages and mean ± SEM. Prevalence of depression was determined by calculating the percentage of patients with severity symptoms on PHQ-9. Analysis of the association between depressive symptoms and individual determinants in patients with COPD was carried out using linear regressions analysis controlling for age and sex. The main model consists of PHQ-9 score as dependent variable and all demographic variables (age, gender, body mass index, literacy, socio-economic status, smoking status and biomass exposure) and COPD related variables (FEV1, breathlessness, disease severity, respiratory symptoms, physical functioning) as independent variables. Difference in characteristics between participants were tested with unpaired t test for normally distributed variables, with the Wilcoxon rank sum test for skewed variables, and with the chi-square test or fisher exact test for categorical variables. Cronbach alpha was calculated to assess internal consistency of PHQ-9. All statistical analyses were carried out using Statistical Package for Social Sciences (SSPS) (Version 20.0, USA).
Results
Demographical, clinical and socio-economic characteristics: A total of 126 patients with COPD were included in the study with the mean age of 62.69 ± 0.84 in Table I. Study population included majority of men (93, 73.81%) as compared to women (33, 26.19%), with a low level of education (75.4%) and from rural area (76.2%). A total of 101 (80.14%) patients were either current or past smokers. Mean smoking index of patients with smoking history was 372.94 ± 25.48 with a significant difference (P<0.001) between male and female population. The mean BMI of the sample population was 20.97 ± 0.29 with 24.6 per cent underweight and 14.3 per cent overweight patients. There was no significant difference in BMI status between male and female group (Table I).
Table I.
Demographic, clinical and socio-economic characteristics of patients with COPD
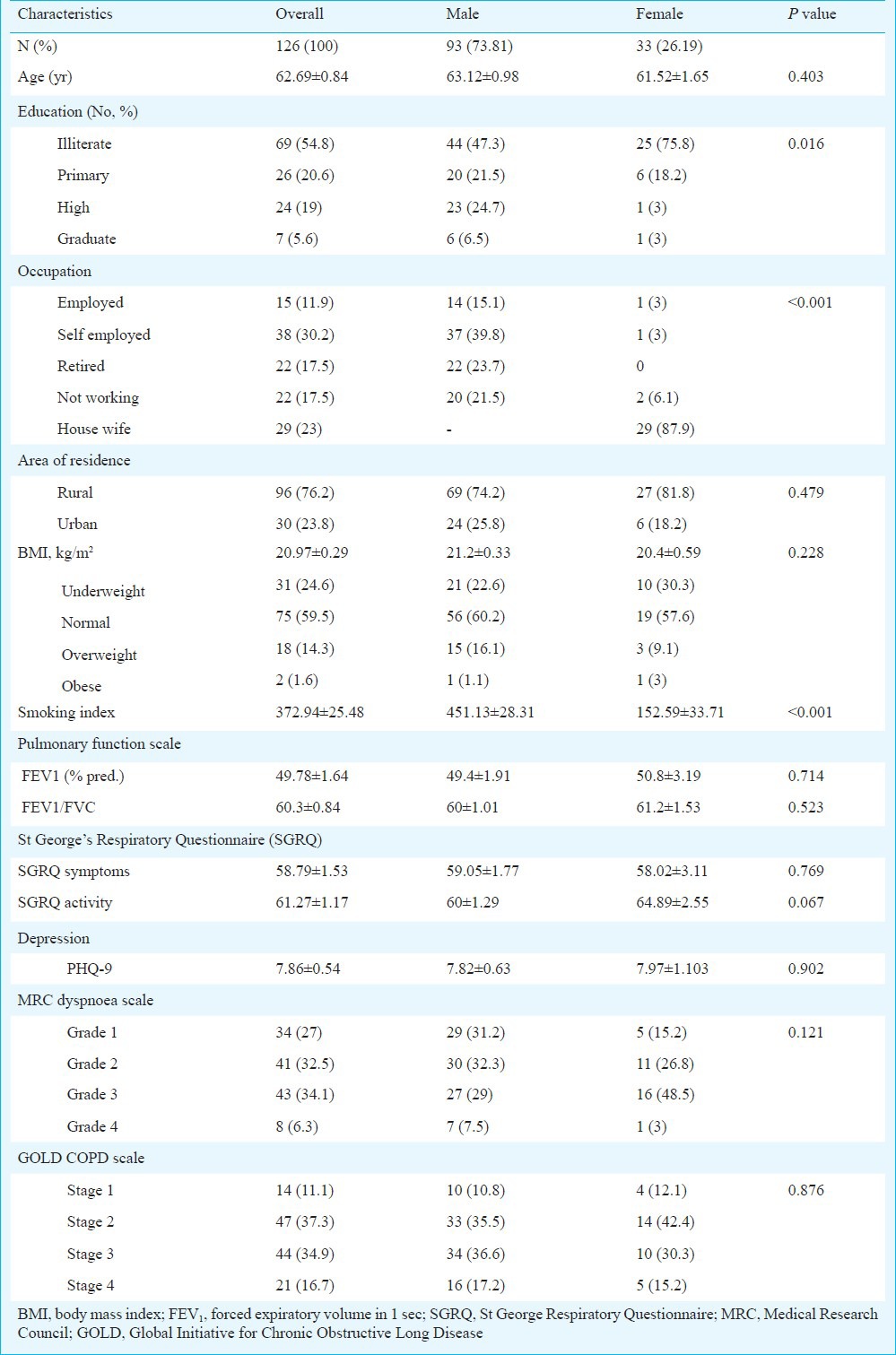
Compared to male, female patients had significantly higher proportion of illiterate patients (75.8 vs. 47.3%). Further, 54.9 per cent of male patients were either employed or self-employed while 87.9 per cent of female patients were housewives. There was no significant difference in area of residence between the male and female group.
A total of 65 (51.6%) patients were suffering from severe COPD, 61 (48.4%) were suffering from mild to moderate COPD. A total of 51 (40.5%) patients were having severe dyspnoea, while 75 (59.5%) were having mild to moderate dyspnoea. There was no significant difference in severity of COPD or dyspnoea level between male and female groups. The FEV1 to FVC ratio was not significantly different between the groups (Table I).
Presence of depression: In the study population as a whole, 62 (49.2%) patients showed mild to severe depressive symptoms. A total of 26 (20.6%) patients had a moderately severe to severe depression or major depressive disorder, followed by 16 (12.7%) having moderate depression and 20 (15.9%) having mild depression (Table II). Severe depression was found to be higher among patients with severe stages of COPD. Internal consistency of PHQ-9 was evaluated using Cronbach alpha. Cronbach alpha was 0.93 for PHQ-9 showing good consistency of these patient reported outcome tools in present study population.
Table II.
Prevalence of depression in COPD patients visiting a tertiary care center in north India

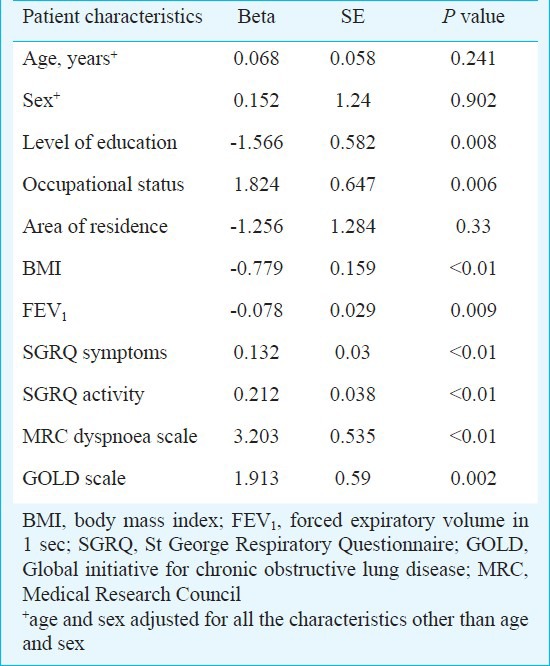
Determinants of depression: Determinants for depression in COPD patients were analysed using linear regression model using score of PHQ-9 as a dependent factor with univariate independent factors such as demographic, clinical and socio-economical factors. Level of education, occupational status, and body mass index, FEV1, dyspnoea, symptoms and activity components of SGRQ, were significantly associated with higher score of PHQ-9 in COPD patients. Lower educational status was associated with higher score of depression severity (beta= -1.566, P<0.01). Higher BMI was associated with lower score of depression in patients with COPD (beta= -0.779, P<0.01). Higher age, gender and area of residence were not associated with higher PHQ-9 score.
Discussion
In the current study, about one third of the patients with COPD were suffering from moderate to severe depression and one in five was suffering from major depressive disorder. The depression was associated with the level of education, occupational status, body mass index, FEV1, respiratory symptoms, physical impairment, dyspnoea and GOLD severity whereas no association was found with age, sex, area of residence and smoking status.
The data regarding the prevalence of depression in patients with COPD from India are scarce. A study has shown 72 per cent cumulative prevalence of depression in Indian COPD patients23. However, studies from other countries reported the prevalence of depression in patients with COPD varying from 6 to 56 per cent9,10,11. This variation in prevalence can be partly attributed to the use of different measures for depression. Studies from Japan and Turkey reported the prevalence of depression in patients with COPD from 40.5 to 46.7 per cent25,26. In our study depression was seen in 33.3 per cent patients which was in accordance with above mentioned studies.
In agreement with a previous study27, our study suggested that age was probably not an important determinant of depression in patients with COPD; gender was also not associated with the depression in COPD patients, which was in accordance with the past studies28. In India, the male patients had higher likelihood of COPD compared to female29; however, in USA the rate is reversed30. One of the major reasons is the high smoking rate in males compared to females in India. Hence, the factors associated with depression could be disease-related factors rather than gender-specific factors. Level of educational has shown strong association with the presence of depressive symptoms similar to a study conducted by Al Shair et al31. Occupational status showed significant association with the presence of depression which could be due to reason that most of the patients with higher disease severity were not working and residing in home only, which in turn could develop mood disorders.
Another important variable, which showed strong association with COPD was body mass index. There was a strong association between BMI and depression as shown by many studies25,31 as presence of depression was significantly higher in patients with low BMI. No association was seen between smoking status and depressive symptoms similar to a study conducted by Hanania et al32 who showed that the depression was more related to COPD itself rather than simply to habits associated with smoking.
Airway obstruction (FEV1) showed strong association with depressive symptoms similar to previous studies25,26. Respiratory symptoms and physical impairment were strongly associated with depressive symptoms, similar to findings reported in the past5,28. Our findings were in accordance with previous studies5,25,31 that dyspnoea was significantly associated with development of depressive symptoms. Reduced physical activity due to dyspnoea is probably the primary factor leading to psychiatric morbidities encountered in our patients. Severity of COPD had strong association with depressive symptoms as shown earlier31.
There were certain limitations in the present study. We were not able to consider sample size for our study population as we did not have previous estimate on prevalence of depression among individuals with COPD and without any extensive co-morbidity in any previous studies. In addition, functional status was not measured in the present study, so relationship of functional status with health related quality of life and psychological health and symptoms was not measured. Table III
Table III.
Linear regression assessing factors associated with higher score of PHQ-9
Future studies should be conducted with large sample size and demographic variation. Depression should be assessed in routine care and factors affecting should be properly monitored in this special group of population. Future studies should be conducted to identify the outcomes of COPD with treatment or screening for depression.
In conclusion, a substantial number of patients with COPD had depression with higher occurrence of depression among less educated, low BMI status, with higher dyspnoea and COPD severity, and with poor quality of life. Therefore, detection of psychological co-morbidities should be emphasized in routine clinical practice in COPD patients.
References
- 1.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Resp Crit Care Med. 2007;176:532–55. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 2.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 3.McKay AJ, Mahesh PA, Fordham JZ, Majeed A. Prevalence of COPD in India: a systematic review. Prim Care Respir J. 2012;21:313–21. doi: 10.4104/pcrj.2012.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Marco F, Verga M, Reggente M, Maria Casanova F, Santus P, Blasi F, et al. Anxiety and depression in COPD patients: the roles of gender and disease severity. Respir Med. 2006;100:1767–74. doi: 10.1016/j.rmed.2006.01.026. [DOI] [PubMed] [Google Scholar]
- 5.Schane RE, Walter LC, Dinno A, Covinsky KE, Woodruff PG. Prevalence and risk factors for depressive symptoms in persons with chronic obstructive pulmonary disease. J Gen Intern Med. 2008;23:1757–62. doi: 10.1007/s11606-008-0749-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tselebis A, Bratis D, Harikiopoulou M, Theodorakopoulou E, Moussas G, Karkanias A, et al. Association between depression and body mass index in patients with chronic obstructive pulmonary disease. Ann Gen Psychiatry. 2010;9(Suppl):S160. [Google Scholar]
- 7.Van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 1999;54:688–92. doi: 10.1136/thx.54.8.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cully JA, Graham DP, Stanley MA, Ferguson CJ, Sharafkhaneh A, Souchek J, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006;47:312–9. doi: 10.1176/appi.psy.47.4.312. [DOI] [PubMed] [Google Scholar]
- 9.Fan VS, Ramsey SD, Giardino ND, Make BJ, Emery CF, Diaz PT, et al. National Emphysema Treatment Trial (NETT) Research Group. Sex, depression, and risk of hospitalization and mortality in chronic obstructive pulmonary disease. Arch Intern Med. 2007;167:2345–53. doi: 10.1001/archinte.167.21.2345. [DOI] [PubMed] [Google Scholar]
- 10.Garrod R, Marshall J, Barley E, Jones PW. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27:788–94. doi: 10.1183/09031936.06.00130605. [DOI] [PubMed] [Google Scholar]
- 11.Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini LG, et al. The effects of depressed mood on smoking cessation: mediation by post-cessation self-efficacy. J Consult Clin Psychol. 2003;71:292–301. doi: 10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- 12.Dahlen I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122:1633–7. doi: 10.1378/chest.122.5.1633. [DOI] [PubMed] [Google Scholar]
- 13.Celli BR, MacNee W, Agusti A, Anzueto A, Berg B, Buist AS, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–46. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 14.Kochhar PH, Rajadhyaksha SS, Suvarna VR. Translation and validation of brief patient health questionnaire against DSM IV as a tool to diagnose major depressive disorder in Indian patients. J Postgrad Med. 2007;53:102–7. doi: 10.4103/0022-3859.32209. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO expert consultation. Appropriate body mass index for Asian population and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 18.Jindal SK, Malik SK. Smoking Index - a measure to quantify cumulative smoking exposure. Lung India. 1988;6:195–6. [Google Scholar]
- 19.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–6. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peruzza S, Sergi G, Vianello A, Pisent C, Tiozzo F, Manzan A, et al. Chronic obstructive pulmonary disease (COPD) in elderly subjects: impact on functional status and quality of life. Respir Med. 2003;97:612–7. doi: 10.1053/rmed.2003.1488. [DOI] [PubMed] [Google Scholar]
- 21.Jones PW, Quirk FH, Baveystock CM. The St George's respiratory questionnaire. Respir Med. 1991;85(Suppl B):25–31. doi: 10.1016/s0954-6111(06)80166-6. discussion 33-7. [DOI] [PubMed] [Google Scholar]
- 22.Aggarwal AN, Gupta D, Kumar T, Singh N, Jindal SK. Validation of Hindi translation of St. George's respiratory questionnaire in Indian patients with chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2007;49:87–91. [Google Scholar]
- 23.Jones PW. Quality of life measurement for patients with diseases of the airways. Thorax. 1991;46:676–82. doi: 10.1136/thx.46.9.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De S. Prevalence of depression in stable chronic obstructive pulmonary disease. Indian J Chest Dis Allied Sci. 2011;53:35–9. [PubMed] [Google Scholar]
- 25.Hayashi Y, Senjyu H, Iguchi A, Iwai S, Kanada R, Honda S, et al. Prevalence of depressive symptoms in Japanese male patients with chronic obstructive pulmonary disease. Psychiatry Clin Neurosci. 2011;65:82–8. doi: 10.1111/j.1440-1819.2010.02171.x. [DOI] [PubMed] [Google Scholar]
- 26.Tetikkurt C, Ozdemir I, Tetikkurt S, Yilmaz N, Ertan T, Bayar N. Anxiety and depression in COPD patients and correlation with sputum and BAL cytology. Multidiscip Resp Med. 2011;6:226–31. doi: 10.1186/2049-6958-6-4-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ottenheim NR, Giltay EJ, Zitman FG, van der Mast RC, de Craen AJ. Risk of depressive symptoms in the oldest old subjects with chronic obstructive pulmonary disease: the Leiden 85-plus study. Am J Geriatr Psychiatry. 2010;18:388–94. doi: 10.1097/JGP.0b013e3181ca8241. [DOI] [PubMed] [Google Scholar]
- 28.Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24:217–23. doi: 10.1093/fampra/cmm009. [DOI] [PubMed] [Google Scholar]
- 29.Jindal SK. Emergence of chronic obstructive pulmonary disease as an epidemic in India. Indian J Med Res. 2006;124:619–30. [PubMed] [Google Scholar]
- 30.Helms SL, Ni FZ, Darbishire PL. COPD: Investigating the Gender Paradigm Shift. [accessed on July 12, 2012];US Pharmacist. 2011 36 HS-30-HS-34 Available from: http://www.uspharmacist.com/content/d/health%20systems/c/29854 . [Google Scholar]
- 31.Al-shair K, Dockry R, Mallia-Milanes B, Kolsum U, Singh D, Vestbo J. Depression and its relationship with poor exercise capacity, BODE index and muscle wasting in COPD. Respir Med. 2009;103:1572–9. doi: 10.1016/j.rmed.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 32.Hanania NA, Mullerova H, Locantore NW, Vestbo J, Watkins ML, Wouters EF, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respie Crit Care Med. 2011;183:604–11. doi: 10.1164/rccm.201003-0472OC. [DOI] [PubMed] [Google Scholar]


